Abstract
Background
Constipation is highly prevalent in the United States. The association of dietary fat intake with constipation has not been well studied. We recently reported that mice fed a high-fat diet had higher incidence of constipation than regular diet fed mice. The aim of this study was to assess if increased intake of dietary saturated fat in humans is also associated with higher risk of constipation and reduced stool frequency.
Methods
Analyses were based on data from 6,207 adults (≥20 years) from the 2005–2006 and 2007–2008 cycles of the National Health and Nutrition Examination Surveys (NHANES) who had completed the bowel health questionnaire. Constipation was defined as a stool frequency of less than three times per week. Multivariable logistic regression analysis was used to calculate adjusted prevalence odds ratio estimates. Statistical analyses were performed using R and RStudio softwares.
Key Results
The prevalence of constipation in this sample was 3.1%. After multivariable adjustment high saturated fat remained associated with constipation. The odds ratio for high saturated fat intake associated with constipation was much higher in diabetics above 65 years, especially in non-Hispanic blacks, females, and those with poor glycemic control, compared to the control group.
Conclusions & Inferences
To our knowledge, this is the first report to investigate the association of high saturated fat diet, bowel frequency and diabetes. This study demonstrates that a high dietary saturated fat intake is associated with significant increase in the prevalence of constipation, especially in the uncontrolled diabetic, non-Hispanic black, female patients.
Keywords: stool frequency, diabetes, constipation, NHANES, high-fat diet
Introduction
Constipation is highly prevalent worldwide; it has been shown recently that the rate is as high as 10.2% in women and 4% for men.(1) It is even more prevalent among older adults and those with lower socioeconomic status, significantly reducing quality of life and increasing health-care cost.(2) Chronic constipation is also the most common gastrointestinal symptom of diabetes,(3) and has been linked to low dietary fiber content in human studies. Even though many correlations between constipation and dietary habits have been published, a relationship between fat intake and constipation is still not studied in large population-based surveys. The pattern of dietary fat intake in the Western population reveals that a large fraction of people consumes high-fat diet (HFD) with 33% of calories from fat.(4) This prompted us to study the correlation of HFD consumption and prevalence of constipation in human population.
Dietary fat has detrimental effects on enteric neuronal cells survival and gastrointestinal motility.(5) It is shown that a HFD causes colonic transit delay in mice, partly by inducing apoptosis in enteric neuronal cells.(6) Hence, the aim of this study was to assess the relationship between dietary fat intake and bowel habits after adjusting for dietary intake of fiber, water, gender, and physical activity. To address these questions we used the National Health and Nutrition Examination Survey (NHANES) database.
Materials and Methods
Study Population
The NHANES is a program of cross-sectional surveys of a nationally representative sample of the non-institutionalized population, which is designed to assess the health and nutritional status of adults and children in the United States. The population is sampled using a complex, stratified, multi-stage, and probability cluster design. The protocol was approved by the National Center for Health Statistics (NCHS) Ethics Review Board and all participants provided written informed consent. The NHANES 2005–2006 and 2007–2008 cycles were used in this study because bowel habit and dietary intake data were collected in these cycles only. Subjects with incomplete data collected for bowel habits, water intake, diet, physical activity, diabetes, physical and laboratory examination were excluded from the study. The collection of data on constipation from the survey is pulled from larger sets of questionnaires -e.g. Bowel Health Questionnaire, as the structure of NHANES survey is not primarily designed to study constipation or gastrointestinal (GI) disorders. Survey participants with ostomies and gastrointestinal conditions such as irritable bowel syndrome were not identified in the NHANES data file. Patients with chronic disease (e.g. hypothyroidism or hyperparathyroidism), pregnancy, medical comorbidities and concomitant medication use were excluded from the study.
Physical activity was reported based on a questionnaire developed by the World Health Organization. The survey collected information on physical activity participation in three settings/domains and sedentary behavior. Respondents were asked about the frequency of their physical activity in week days. Duration was asked in terms of minutes or hours. Vigorous-intensity activities were activities that require hard physical effort and cause large increases in breathing or heart rate. Moderate-intensity activities were activities that require moderate physical effort and small increases in breathing or heart rate.(7)
Definition of Constipation
The NHANES surveys record stool frequency and consistency within the last 30 days prior to the data collection time. Similar to previous studies that evaluated constipation in the NHANES surveys, constipation was defined as less than three bowel movements (BMs) per week.(8) We included people from whom bowel movement frequency data was available (Table 1). However, in further analysis the 600 patients with hard stool but more frequent bowel movements (Bristol score 1–2 and >3 BM per week), were excluded from our sample size to ascertain that this population would not be analyzed as non-constipated population. Stool frequency was assessed with the following question, “How many times a week do you usually have a bowel movement in the past 30 days?” Response levels were not specified and the range varied from 1 to 70 BMs/ week. Stool frequency results were dichotomized as <3 BMs/ week (constipated) or ≥3 BMs/ week.
Table 1.
Comparison of stool frequency and stool consistency in NHANES, 2005 – 2006 and 2007 – 2008
| Stool frequency (per week) |
Stool consistency | ||
|---|---|---|---|
| Bristol type 1–2 | Bristol type 3–7 | Total | |
| <3 | 0.8% (79) | 2.6% (246) | 3.4 (325); Constipated |
| >3 | 7% (660) | 89.6% (8,485) | 96.6% (9145); Non-constipated |
| Total | 7.8% (739) | 92.2% (8731) | 100% (9470) |
Assessment of Risk Factors for Constipation
Age, gender, race, education, fluid and fiber intake, physical activity, cholesterol, and diabetes were considered in the assessment of risk factors. Age was used as a categorical variable with three categories: young (less than 50 years), middle (between 50 and 65 years), and senior (older than 65 years). The body mass index (BMI, kg/m2) was dichotomized into normal/overweight (less than 30.0 kg/m2) or obese (30.0 kg/m2 or greater). Race/ethnicity was categorized as non-Hispanic black, non-Hispanic white, Hispanic (including Mexican-American), and other (defined as multi-racial groups), which was self-reported. Consistent with prior NHANES surveys, diabetes mellitus was defined as being informed by a doctor or health professional about the diagnosis and/or taking insulin and/or diabetic pills. Uncontrolled diabetes was defined as observed fasting plasma glucose greater than 126 mg/dL.(9)
Dietary Measures
24-hour dietary data was gathered in two days using a multiple-pass dietary (2 dietary periods) recall method. Dietary consumption, including fat, was ascertained in both periods and averaged. Total fat was estimated as the sum of daily fat intake for all foods. The distribution of fiber intake and liquid intake were categorized into tertiles.
Statistical Methods
All statistical analyses were done using the public domain software R, version 2.15.2 and RStudio software version 0.98.977 (Boston, MA).(10) Initially, bivariate data analyses were explored to identify possible associations between constipation and risk factors. The R-function CrossTable and Chi-square tests were used to select the factors that were included in the logistic regression model. A logistic regression model was estimated using the Generalized Linear Model (GLM) function with the binomial family. A preliminary analysis of the estimated residuals for model checking using the plot function identified three influential observations. These are observations that have a disproportionate impact on the values of the model parameters. Cook’s distance was used to identify three influential observations. The sequence numbers of these participants were 37616, 42028 and 45634. These individuals were excluded from the final analysis. Univariate logistic regression analysis was used to calculate prevalence Odds Ratio (OR) estimates and corresponding 95% confidence intervals (CI) for constipation prevalence. Multivariable logistic regression analysis was used to calculate prevalence Odds Ratio estimates and corresponding 95% CI for constipation prevalence with adjustment for other variables associated with constipation. P values < 0.05 were considered statistically significant.
Results
Prevalence of constipation based on stool frequency and consistency
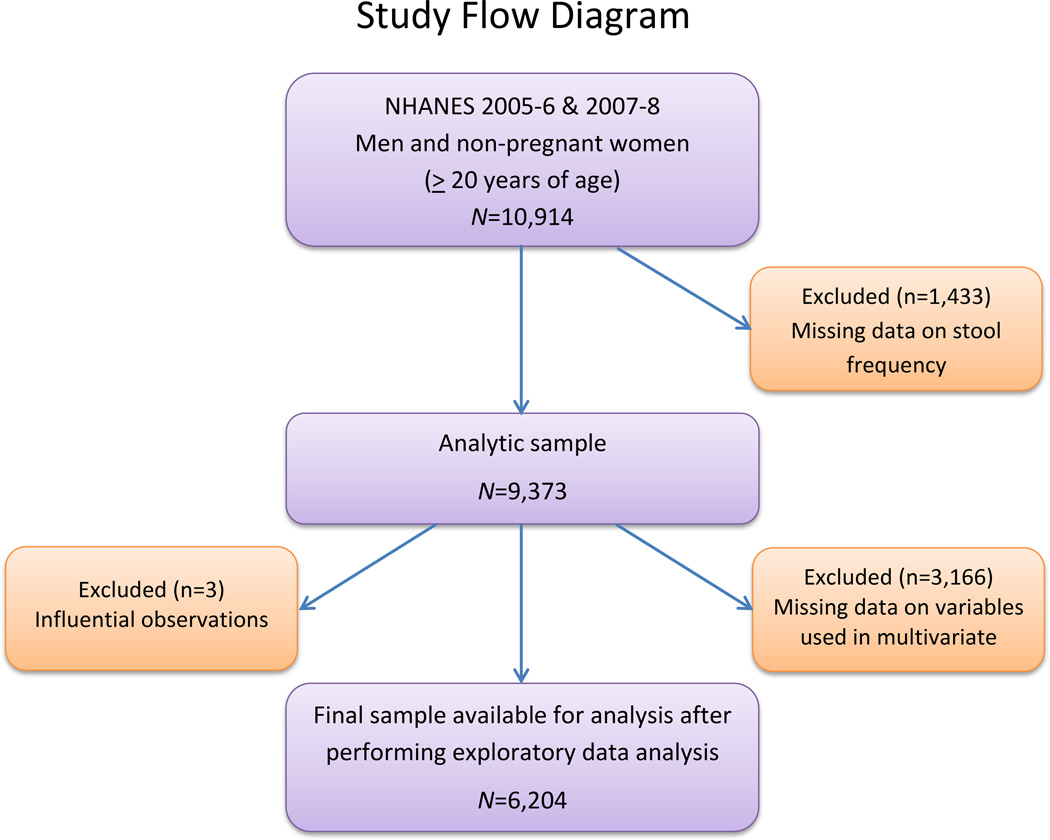
Of the 10,914 people who participated in both these cycles, data on stool frequency and/or consistency was available for 9,373. However, some of the independent variables were missing in multivariate regression analysis in 3,166 observations, reducing the final sample to 6,207 people (2,830 men and 3,377 women) aged 20 years or older in whom all data was available (Figure 1). In this cohort, the prevalence of constipation was 7.2%, (95% CI, 6.7–7.8) when defined by stool consistency alone (i.e., Bristol stool form score of 1 and 2), 3.1% (95% CI, 2.6–3.8) as defined by less than 3 bowel movements per week, and 0.8% (95% CI, 0.6–1.0) when both criteria were used (Table 1). Since data for other variables were missing among participants in whom stool consistency was available, subsequent analyses defined constipation as less than three bowel movements per week.
Figure 1.
The National Health and Nutrition Examination Surveys (NHANES) 2005–2006 and 2007–2008 multivariable analysis study flow diagram.
Age, gender and racial differences in the prevalence of constipation
In the univariate analysis, the prevalence of constipation was higher (P<0.001) in women (4.8%) than men (1.2%), and in non-Hispanic black (5.7%) than non-Hispanic white people (2.7%) (P<0.001). Conversely, participants who finished college had a lower risk of constipation than those who did not complete high school. Those who had a higher income-poverty ratio and greater physical activity were associated with significantly lower prevalence of constipation. The high fiber and water intake were also associated with lower prevalence of constipation (Table 2).
Table 2.
Baseline characteristics and univariate analysis of study sample from NHANES 2005–6 &2007–8
| Variable | Number (n= 6,207, Col.%) |
Constipation (n= 194, (3.1), row %) |
Odd Ratio (95% CI) |
P-value (Chi. Sq.) |
|---|---|---|---|---|
| Age (n,%) | ||||
| Young (<50 yr) | 3362(54.2) | 137 (4.1) | 1(Referent group) | |
| Middle (50–65 yr) | 1481(23.9) | 28 (1.9) | 0.5(0.3–0.7) | |
| Senior (>65yr) | 1364(22.0) | 29(2.1) | 0.5(0.3–0.8) | <0.001 |
| Gender | ||||
| Male | 2,830 (45.6) | 33 (1.2) | 1 (Referent group) | |
| Female | 3,377 (54.4) | 161(4.8) | 4.2 (2.9–6.2) | <0.001 |
| Ethnicity (n, %) | ||||
| Non-Hispanic White | 3,099 (49.9) | 84 (2.7) | 1 (Referent group) | |
| Non-Hispanic Black | 1,316 (21.2) | 75 (5.7) | 2.2(1.6–2.9) | |
| Mexican | 1,116 (18.0) | 15 (1.3) | 0.5(0.3–0.9) | |
| Other Hispanic | 449 (7.2) | 12 (2.7) | 0.98 (0.5–1.8) | |
| Other | 219 (3.7) | 8 (3.7) | 1.4(0.7–2.8) | <.001 |
| Education | ||||
| < High School | 1,558 (25.1) | 55 (3.5) | 1 (Referent group) | |
| High School | 1,480 (23.8) | 54 (3.6) | 1.03 (0.7–1.5) | |
| Some College | 1,781 (28.7) | 67 (3.8) | 1.1(0.7–1.5) | |
| College | 1,388 (22.4) | 18 (1.3) | 0.4(0.2–0.6) | <0.001 |
| Income-Poverty Ratio | ||||
| Low (<2) | 2,621 (42.2) | 109 (4.2) | 1(Referent group) | |
| Medium (2 to 3) | 1,015 (16.4) | 25 (2.5) | 0.6(0.4–0.9) | |
| High (3 to 5) | 2,571 (41.6) | 60 (2.3) | 0.6(0.4–0.8) | <0.001 |
| Waist (cm) | ||||
| Small <75–85 | 2,071 (33.4) | 90 (4.3) | 1(Referent group) | |
| Medium <85–89 or 75–79 | 2,094 (33.7) | 49 (2.3) | 0.5(0.4–0.8) | |
| Large >86–95 | 2,042 (32.9) | 55 (2.7) | 0.6(0.4–0.9) | <0.001 |
| Vigorous Physical Activity | ||||
| No | 4,572 (73.7) | 160 (3.5) | 1(Referent group) | |
| Yes | 1,635 (26.3) | 34 (2.1) | 0.6(0.4–0.9) | 0.006 |
| Fiber (g/day) | ||||
| Low (0–10.8) | 1,986 (32.0) | 91 (4.6) | 1(Referent group) | |
| Medium (10.8–17.6) | 2,043 (32.9) | 70 (3.4) | 0.7(0.5–1) | |
| High (17.6–84.8) | 2,178 (35.1) | 33 (1.5) | 0.3(0.2–0.5) | <0.001 |
| Total Saturated Fat(g/day) | ||||
| Low (<= 15) | 1,647 (26.6) | 48 (2.9) | 1(Referent group) | |
| Medium (>15 &<= 30) | 2,652 (42.7) | 90 (3.4) | 1.2(0.8–1.7) | |
| High (> 30) | 1,908 (30.7) | 56 (2.9) | 1(0.7–1.5) | 0.58 |
| Total Cholesterol | ||||
| < 180 | 2,465 (39.7) | 88 (3.6) | 1(Referent group) | |
| 180 to 399 | 2,342 (37.7) | 71 (3.0) | 0.8(0.6–1.2) | |
| >399 | 1,400 (22.6) | 35 (2.5) | 0.7(0.5–1) | 0.175 |
| Total Water Intake (g/day) | ||||
| Low (0–652) | 892 (14.4) | 33 (3.7) | 1(Referent group) | |
| Medium (652–2200) | 2,620 (42.2) | 95 (3.6) | 1(0.7–1.5) | |
| High (>2200) | 2,695 (43.4) | 66 (2.4) | 0.7(0.4–1) | 0.003 |
| Diabetes |
Number (n= 4,419, Col.%) |
Constipation (n= 136, row %) |
Odd Ratio (95% CI) |
P-value (Chi. Sq.) |
| No Diabetes | 3712(84.0) | 113(3.0) | 1(Referent group) | |
| Undiagnosed diabetes | 188(4.3) | 2 (1.1) | 0.3(0.1–1.4) | |
| controlled | 181(4.1) | 6(3.3) | 1.1(0.5–2.5) | |
| uncontrolled | 338(7.6) | 15(4.4) | 1.5(0.9–2.6) | 0.19 |
In the multivariate analysis, the odds ratio for constipation was higher in females and the black population in both <65 and >65 age groups (Table 3 and 4). Further, in the multivariate analysis, some of the factors associated with constipation were different in people 65 years and younger compared with those older than 65 years. Among people aged 65 years and younger, physical activity (OR 0.69; 95% CI, 0.46–1.03), high fiber intake (OR 0.49; 95% CI, 0.3–0.78), and high total water intake (OR 0.63; 95% CI, 0.44–1.1) were associated with a lower risk of constipation after controlling for gender, ethnicity and other factors (Table 3). In contrast, after adjusting for gender, ethnicity and other factors, high fiber intake (OR 1.42; 95% CI, 0.28–7.29) and high total water intake (OR 0.41; 95% CI, 0.08–2.11) were not associated with a lower risk of constipation in people older than 65 years (Table 4).
Table3.
Multivariate logistic regression analysis of factors associated with constipation: Age <=65 years
| Odds Ratio (95%CI) | |
|---|---|
| Gender-Female | 4.01*** (2.63–6.33) |
| Ethnicity-Black | 1.64*** (1.13–2.38) |
| Ethnicity-Other Hispanic | 0.62 (0.308–1.19) |
| Physical activity | 0.69* (0.46–1.03) |
| Fiber category-Medium | 0.92 (0.64–1.33) |
| Fiber category-High | 0.49** (0.3–0.78) |
| Total saturated fat-Medium | 1.63* (1.01–2.69) |
| Total saturated fat-High | 1.9* (1.07–3.42) |
| Total water-Medium | 1.01 (0.64–1.64) |
| Total water-High | 0.63* (0.4–1.1) |
| Diabetes-Uncontrolled | 0.98 (0.31–2.6) |
| Diabetes-Controlled | 1.02 (0.23–3.27) |
Referent group: Male, white, non-diabetic, low physical activity and lowest tertile in all other categories
P<0.05
P<0.01
P<0.001
Table 4.
Multivariate logistic regression analysis of factors associated with constipation: Age > 65 years
| Odds Ratio (95%CI) | |
|---|---|
| Gender-Female | 8.1** (2.04–46.01) |
| Ethnicity-Black | 4.15* (1.12–15.64) |
| Ethnicity-Other-Hispanic | 0.55 (0.024–4.53) |
| Ethnicity-Other | 5.11 (0.22–46.25) |
| Fiber category-Medium | 2.56 (0.64–11.56) |
| Fiber category-High | 1.42 (0.28–7.29) |
| Total saturated fat-Medium | 1.16 (0.29–4.87) |
| Total saturated fat-High | 5.0* (0.93–29.08) |
| Total water-Medium | 0.36 (0.085–1.66) |
| Total water-High | 0.41 (0.08–2.11) |
| Diabetes-Uncontrolled# | 7.21* (1.48–34.51) |
| Diabetes-Controlled | 4.7* (0.86–21.82) |
Referent group: Male, white, non-diabetic, low physical activity and lowest tertile in all other categories
Uncontrolled Diabetes: Diabetic patients with fasting BS ≥126 on exam day
P<0.05
P<0.01
Effect of dietary fat intake on constipation
Dietary intake of high saturated fat remained correlated with constipation (P <0.05) after multivariable adjustment (fiber, physical activity, water intake, BMI, total cholesterol, income, education level, ethnicity and gender) in both below 65 years old (OR 1.9; 95% CI, 1.07–3.42, P<0.05) and above 65 years old groups (OR 5.0; 95% CI, 0.93–29.08, P<0.05) (Tables 3 and 4). However, dietary unsaturated fat intake was not associated with increased constipation (P>0.05, data not shown). Moreover, we analyzed this association after the 660 participants with Bristol score 1–2 and >3 BM per week were excluded from our control group. For age category less than 65 years, dietary fat intake maintained significant associations with constipation (OR 1.82; 95% CI, 1.022–3.283, P = 0.044). In participants above 65 years old saturated fat was borderline associated with constipation (OR 4.99, 95% 0.894–30.045, p=0.069).
Effect of glycemic control on modulating the high saturated fat diet-induced constipation
In diabetics greater than 65 years old, high saturated fat consumption was associated with a significant increase in the odds ratio for constipation compared with non-diabetics and the odds ratio was the highest in female diabetic patients with poor glycemic control compared with those with good glycemic control. However, this association was not seen in male participants. Constipation prevalence was the greatest in females with uncontrolled diabetes consuming a high saturated fat diet (P<0.05, Table 5). We also performed an analysis to assess the interaction of diabetes and the sub-group of highest fat intake (diabetic non-Hispanic black). This sub group had the highest risk for constipation. Regression coefficients of interaction terms (non-Hispanic black, diabetic and high fat diet) were not statistically significant (P>0.1) indicating the absence of an interaction between these variables.
Table 5.
Multivariate logistic regression analysis of diabetes and dietary fat intake according to age groups in female population.
| Age <=65 years | OR of product(95% CI) |
Number (n=1660*,%) |
| Medium Fat, Controlled Diabetes | 6.66(0.79–56.26) | 25(1.5) |
| Medium Fat, Uncontrolled Diabetes | 6.40(0.79–51.51) | 39(2.3) |
| High Fat, Controlled Diabetes | 7.77(0.87–68.99) | 6(0.3) |
| High Fat, Uncontrolled Diabetes | 7.46(0.87–63.48) | 19(1.1) |
| Age >65 years |
Number (n=450,%) |
|
| Medium Fat, Controlled Diabetes | 44.16(0.76–2542.70) | 19(4.2) |
| Medium Fat Uncontrolled Diabetes | 67.74(1.03–4444.28) | 34(2) |
| High Fat, Controlled Diabetes | 190.35(2.90–12475.04) | 4(0.8) |
| High Fat, Uncontrolled Diabetes | 292.00(4.01–21225.61) | 7(1.5) |
All observations in this table were done in female population excluding undiagnosed diabetes group and were statistically significant compared to referent group in age >65, (P<0.05). Referent group: Male, white, non-diabetic, low physical activity and lowest tertile in all other categories
When assessing the effect of oral hypoglycemic agents, our analysis showed there were only 131 participants that have relevant medications information available. Among this population, we observed no statistically significant impact of oral hypoglycemic agents on bowel habit patterns.
Discussion
These observations show for the first time, that a high intake of saturated fat (greater than 30 grams daily) is associated with a higher prevalence of constipation, even after adjusting for other putative factors for constipation including income and education level, ethnicity and gender, intake of fiber and water, physical activity, and diabetes mellitus. The 30 gm threshold for saturated fat intake is the recommended daily amount of saturated fat intake for individuals consuming a 2500 cal/d diet.(11) It is also the average total dietary saturated fat intake for people more than 20 years of age in the United States.(12) From a public health perspective, these findings are significant because constipation is a very common gastrointestinal symptom and accounts for considerable amount of health-care resources. On the other hand, dietary fat consumption in the United States has increased over time.(13, 14) Thus, constipation is yet another potential hazard of increasing dietary fat consumption in this country.(15)
This study was conducted in a large cohort of participants with an ethnic and socioeconomic distribution comparable to the US population. The NHANES database utilizes a validated methodology for evaluating dietary intake and physical activity. Smaller studies in children and adolescents have suggested that a higher fat intake was associated with constipation.(16, 17) However, those studies did not evaluate fiber intake. It has been proposed that a high-fat diet may have a lower content of dietary fiber.(18) Hence, the ability to adjust for dietary fiber intake in the analysis was a particular strength of our study. Stool frequency is negatively correlated with colonic transit (19), which substantiates its utility as an index of colonic motor function. However, the Bowel Health Questionnaire of NHANES database does not assess for other gastrointestinal symptoms (e.g. bloating, abdominal pain and discomfort, or the sense of incomplete evacuation after defecation).
It has previously been shown in the literature that saturated fatty acids such as palmitic acid can affect systemic and tissue lipid profiles as well as inducing neuronal apoptosis (6), but unsaturated fatty acids such as Oleic acid have shown beneficial properties against free fatty acid-induced neuronal injury. Oleic acid co-incubation prevents palmitate-induced cytotoxicity in a concentration dependent manner.(20) In another study, Kien et al. found that replacing dietary palmitic acid with oleic acid reduces the blood LDL concentration and whole-body fat oxidation by modifying the saturation index of circulating and tissue lipids.(21) Hence, we decided to focus on the impact of saturated fat intake on GI transit and constipation.
There are several possible explanations for the observed association between high dietary saturated fat intake and constipation.(21) Even though gastrocolic reflex in response to fatty food can acutely increase motility of the colon, this response is mainly triggered by stretch in the stomach and byproducts of digestion in the small intestine, which is responsible for the urge to defecate following a meal. However, the findings from our study show that long term HFD consumption can lead to slower GI motility and constipation. We believe that other mechanisms might also affect the GI motility and stool consistency along with gastrocolic reflux. First, it is conceivable that a high-fat diet activates the ileal brake, which delays gastric emptying and small bowel transit, hence slowing overall GI transit and predisposing to constipation.(5, 22) Second, the availability of serotonin in colon enterochromaffin cells is lower in rats fed a high-fat diet compared to control rats.(23) Lastly, a high-fat diet may damage enteric neurons in human in a similar fashion that is shown in mice via a pathway mediated by microRNA375 up-regulation.(6)
The mean intake of 11.1–13.3 g/d of dietary fiber is previously reported in US population from NHANES database. In our analysis, this level of fiber intake was categorized in the medium fiber intake category. United States Department of Agriculture Nationwide Food Consumption Survey recommendation is set at 25 to 50 grams of dietary fiber daily.(24, 25) This level of fiber intake would fall in the high fiber category in our study. In 2005–2006, American adults reported consuming 3.18 liters of total water within the previous 24 hours with plain water and beverages contributing 33% and 48%, respectively.(26) We also observed that high fiber intake and water intake are associated with lower constipation in young and middle-aged group but not for those above 65 years. Although our study provides estimates of various contributors to total water intake adjusted for multiple covariates, the NHANES public release data do not include information on geographic location and season of exam. We expect geographic location and season of exam to be highly correlated with the bowel movements recorded in the NHANES data, yet we acknowledge the possibility that the role of water intake might be underestimated in our study.
Constipation is a common complication of diabetes. Twenty to forty-four percent of patients with diabetes report symptoms of constipation or increased use of laxatives.(27) In our study, we observed a more prominent correlation between high-fat diet consumption and constipation in poorly controlled diabetics. Consistent with previous studies, diabetics had a higher association with constipation.(28) Indeed, the odds of having constipation were greater in both controlled and poorly controlled diabetes. Interestingly, studies show that the children with type 1 diabetes have higher consumption of high-fat, low-fiber diets compared with youth in the general population.(29, 30) Similarly, higher fat intake in diabetic patients in our study may contribute to the increased incidence of constipation seen in diabetics. However, it is necessary to mention that the observed effect of diabetes on constipation was isolated from other contributing factors using statistical models. The best way to eliminate diabetes effect on constipation and assess the high-fat diet and constipation association is to design a randomized clinical trial, which was beyond the scope of the current study, but is necessary for future studies in this field.
The major limitation in our study includes our definition of constipation, which is based on the stool frequency (number of defecations per participants’ report) and is therefore subjective. We included the subjects who had all the relevant data required for analysis. Furthermore, the case group did not include individuals with hard but more frequent stools. Therefore, it is possible that our definition of constipation has resulted in low constipation. However, our constipation prevalence based on frequency was comparable to the other studies done using the NHANES database. (1)
We also considered constipation definition based on both stool form as well as low stool frequency, revealing 79 cases. However, the data did not show any significant association between high saturated dietary fat intake and constipation in this sub-group, which might also be due to the very small sample size. Moreover, as this is a questionnaire based study, there can be some element of recall bias as well. Another limitation is the cross-sectional study design, which allowed us to generate a working hypothesis that increased dietary fat intake is associated with constipation, but is not capable of proving the causality between the two.
Another possible limitation of our study is that constipation is not more prevalent in elderly compared to young people. However, some population based surveys and other studies using NHANES database also failed to report higher prevalence of constipation in the elderly using stool frequency as the definition for constipation. Markland et al. reported that even after dichotomizing age as ≥60 years of age, women and men in the older age groups did not have higher prevalence rates of constipation compared to those <60 years of age (p>0.05). (1) They observed no trends for increased prevalence of constipation by age decade. Similarly, in their study on 62,036 women, Dukas et al. reported that age was inversely associated with constipation, as women aged 60 year and older had a multivariate-adjusted prevalence ratio of constipation of 0.41 (95% CI, 0.32–0.52) compared to 35 to 39-year old women. (31) Also in their population-based study using stool frequency as a definition, Harari et al. studied 42,375 subjects who participated in the National Health Interview Survey on Digestive Disorders and failed to find an increased trend in constipation prevalence by age. (32)
In conclusion, we show for the first time that high saturated fat dietary intake is associated with decreased bowel habit frequency. In our multivariate analysis, we found a strong correlation between high dietary saturated fat intake, diabetes and constipation in the elderly after adjusting for other variables that can contribute to constipation. The odds for constipation are notably higher in uncontrolled diabetic, elderly female patients as well as the non-Hispanic black female population. In recent years, there has been increased consumption of high saturated fat in the westernized population. Our research suggests that dietary high-fat diet intake is correlated with constipation. Further research is needed to confirm whether adjusting the diet can improve the symptoms of constipation. Nevertheless, educating on dietary control in the people consuming high-fat diets particularly the elderly and diabetics, who are at higher risk for constipation, might be worthwhile. Recommendations cannot yet be made concerning the optimal fatty acid composition of the diet for digestive disease system health; however, the present findings provide new evidence supporting dietary recommendations to consume diets low in saturated fat, specifically in those who suffer from constipation. Further work in this area is warranted given the growth of elderly population, prevalence of constipation, and the popularity of low-carbohydrate and high-fat diets in American cuisine.
Key Messages.
Education on dietary fat control in the people consuming high-fat diets might be worthwhile, particularly in elderly and diabetic patients, who are at higher risk for constipation.
Present findings provide new evidence supporting dietary recommendations to consume diets low in saturated fat, specifically in those who suffer from constipation.
After multivariable adjustment, high saturated fat remained associated with constipation. The odds ratio for high saturated fat intake associated with constipation was much higher in diabetics greater than 65 years old, especially those with poor glycemic control, non-Hispanic blacks and females, compared to the control group.
Acknowledgments
Funding
Financial Support: This work was supported by a grant from the National Institutes of Health, USA (DK080684 and VA-MERIT award to SS)
Footnotes
- SS, VKC, & STV Provided the concept and design of the study
- BGN & VKC helped with the acquisition of data
- SS, VKC, & STV performed analysis and interpretation of data
- SS, STV, & AS performed drafting of the manuscript
- SS & VKC did the critical revision of the manuscript for important intellectual content
- VKC completed statistical analysis
- SS obtained funding and provided administrative support and supervised the study
Disclosures: The authors have no disclosures.
Competing Interests: The authors have no competing interests.
References
- 1.Markland AD, Palsson O, Goode PS, Burgio KL, Busby-Whitehead J, Whitehead WE. Association of low dietary intake of fiber and liquids with constipation: evidence from the National Health and Nutrition Examination Survey. The American journal of gastroenterology. 2013;108(5):796–803. doi: 10.1038/ajg.2013.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bharucha AE, Pemberton JH, Locke GR., 3rd American Gastroenterological Association technical review on constipation. Gastroenterology. 2013;144(1):218–238. doi: 10.1053/j.gastro.2012.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bharucha AE, Low P, Camilleri M, Veil E, Burton D, Kudva Y, et al. A randomised controlled study of the effect of cholinesterase inhibition on colon function in patients with diabetes mellitus and constipation. Gut. 2013;62(5):708–715. doi: 10.1136/gutjnl-2012-302483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Austin GL, Ogden LG, Hill JO. Trends in carbohydrate, fat, and protein intakes and association with energy intake in normal-weight, overweight, and obese individuals: 1971–2006. Am J Clin Nutr. 2011;93(4):836–843. doi: 10.3945/ajcn.110.000141. [DOI] [PubMed] [Google Scholar]
- 5.Mushref MA, Srinivasan S. Effect of high fat-diet and obesity on gastrointestinal motility. Ann Transl Med. 2013;1(2):14. doi: 10.3978/j.issn.2305-5839.2012.11.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nezami BG, Mwangi SM, Lee JE, Jeppsson S, Anitha M, Yarandi SS, et al. MicroRNA 375 mediates palmitate-induced enteric neuronal damage and high-fat diet-induced delayed intestinal transit in mice. Gastroenterology. 2014;146(2):473 e3–483 e3. doi: 10.1053/j.gastro.2013.10.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maher CA, Mire E, Harrington DM, Staiano AE, Katzmarzyk PT. The independent and combined associations of physical activity and sedentary behavior with obesity in adults: NHANES 2003–06. Obesity. 2013;21(12):E730–E737. doi: 10.1002/oby.20430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Everhart JE, Go VL, Johannes RS, Fitzsimmons SC, Roth HP, White LR. A longitudinal survey of self-reported bowel habits in the United States. Dig Dis Sci. 1989;34(8):1153–1162. doi: 10.1007/BF01537261. [DOI] [PubMed] [Google Scholar]
- 9.Muntner P, He J, Chen J, Fonseca V, Whelton PK. Prevalence of non-traditional cardiovascular disease risk factors among persons with impaired fasting glucose, impaired glucose tolerance, diabetes, and the metabolic syndrome: analysis of the Third National Health and Nutrition Examination Survey (NHANES III) Ann Epidemiol. 2004;14(9):686–695. doi: 10.1016/j.annepidem.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 10.R Core Team. R: A language and environment for statistical computing. Austria: R Foundation for Statistical Computing V; 2012. [2012-10-26]. ISBN 3-900051-07-0, URL http://www.R-project.org/. and RStudio Version 0.98.977-2009-2013, RStudio, Inc. [Google Scholar]
- 11.Elbel B. Consumer estimation of recommended and actual calories at fast food restaurants. Obesity. 2011;19(10):1971–1978. doi: 10.1038/oby.2011.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ervin RB, Wright JD, Wang CY, Kennedy-Stephenson J. Dietary intake of fats and fatty acids for the United States population: 1999–2000. Adv Data. 2004;(348):1–6. [PubMed] [Google Scholar]
- 13.King DE, Xiang J, Brown A. Intake of Key Chronic Disease-Related Nutrients among Baby Boomers. South Med J. 2014;107(6):342–347. doi: 10.14423/01.SMJ.0000450706.44388.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vadiveloo M, Scott M, Quatromoni P, Jacques P, Parekh N. Trends in dietary fat and high-fat food intakes from 1991 to 2008 in the Framingham Heart Study participants. Br J Nutr. 2014;111(4):724–734. doi: 10.1017/S0007114513002924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corwin RL, Hartman TJ, Maczuga SA, Graubard BI. Dietary saturated fat intake is inversely associated with bone density in humans: analysis of NHANES III. J Nutr. 2006;136(1):159–165. doi: 10.1093/jn/136.1.159. [DOI] [PubMed] [Google Scholar]
- 16.Jennings A, Davies GJ, Costarelli V, Dettmar PW. Bowel habit, diet and body weight in preadolescent children. J Hum Nutr Diet. 2010;23(5):511–519. doi: 10.1111/j.1365-277X.2009.01039.x. [DOI] [PubMed] [Google Scholar]
- 17.vd Baan-Slootweg OH, Liem O, Bekkali N, van Aalderen WM, Rijcken TH, Di Lorenzo C, et al. Constipation and colonic transit times in children with morbid obesity. J Pediatr Gastroenterol Nutr. 2011;52(4):442–445. doi: 10.1097/MPG.0b013e3181ef8e3c. [DOI] [PubMed] [Google Scholar]
- 18.Marlett JA, McBurney MI, Slavin JL, American Dietetic A. Position of the American Dietetic Association: health implications of dietary fiber. J Am Diet Assoc. 2002;102(7):993–1000. doi: 10.1016/s0002-8223(02)90228-2. [DOI] [PubMed] [Google Scholar]
- 19.Tornblom H, Van Oudenhove L, Sadik R, Abrahamsson H, Tack J, Simren M. Colonic transit time and IBS symptoms: what's the link? The American journal of gastroenterology. 2012;107(5):754–760. doi: 10.1038/ajg.2012.5. [DOI] [PubMed] [Google Scholar]
- 20.Kwon B, Querfurth HW. Opposite effects of saturated and unsaturated free fatty acids on intracellular signaling and metabolism in neuronal cells. Inflammation & Cell Signaling. 2014;1(e 200) [Google Scholar]
- 21.Kien CL, Bunn JY, Stevens R, Bain J, Ikayeva O, Crain K, et al. Dietary intake of palmitate and oleate has broad impact on systemic and tissue lipid profiles in humans. Am J Clin Nutr. 2014;99(3):436–445. doi: 10.3945/ajcn.113.070557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spiller RC, Trotman IF, Higgins BE, Ghatei MA, Grimble GK, Lee YC, et al. The ileal brake--inhibition of jejunal motility after ileal fat perfusion in man. Gut. 1984;25(4):365–374. doi: 10.1136/gut.25.4.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bertrand RL, Senadheera S, Tanoto A, Tan KL, Howitt L, Chen H, et al. Serotonin availability in rat colon is reduced during a Western diet model of obesity. Am J Physiol Gastrointest Liver Physiol. 2012;303(3):G424–G434. doi: 10.1152/ajpgi.00048.2012. [DOI] [PubMed] [Google Scholar]
- 24.E Lanza DYJ, Block G, Kessler L. Dietary fiber intake in the US population. Am J Clin Nutr. 1987 Nov 5;46:8. doi: 10.1093/ajcn/46.5.790. [DOI] [PubMed] [Google Scholar]
- 25.Slavin JL. Dietary fiber: classification, chemical analyses, and food sources. J Am Diet Assoc. 1987;87(9):1164–1171. [PubMed] [Google Scholar]
- 26.Kant AK, Graubard BI, Atchison EA. Intakes of plain water, moisture in foods and beverages, and total water in the adult US population--nutritional, meal pattern, and body weight correlates: National Health and Nutrition Examination Surveys 1999–2006. Am J Clin Nutr. 2009;90(3):655–663. doi: 10.3945/ajcn.2009.27749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maleki D, Camilleri M, Burton DD, Rath-Harvey DM, Oenning L, Pemberton JH, et al. Pilot study of pathophysiology of constipation among community diabetics. Dig Dis Sci. 1998;43(11):2373–2378. doi: 10.1023/a:1026657426396. [DOI] [PubMed] [Google Scholar]
- 28.Maleki D, Locke GR, 3rd, Camilleri M, Zinsmeister AR, Yawn BP, Leibson C, et al. Gastrointestinal tract symptoms among persons with diabetes mellitus in the community. Archives of internal medicine. 2000;160(18):2808–2816. doi: 10.1001/archinte.160.18.2808. [DOI] [PubMed] [Google Scholar]
- 29.Mehta SN, Volkening LK, Quinn N, Laffel LM. Intensively managed young children with type 1 diabetes consume high-fat, low-fiber diets similar to age-matched controls. Nutr Res. 2014;34(5):428–435. doi: 10.1016/j.nutres.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patton SR, Dolan LM, Chen M, Powers SW. Dietary adherence and mealtime behaviors in young children with type 1 diabetes on intensive insulin therapy. J Acad Nutr Diet. 2013;113(2):258–262. doi: 10.1016/j.jand.2012.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dukas L, Willett WC, Giovannucci EL. Association between physical activity, fiber intake, and other lifestyle variables and constipation in a study of women. The American journal of gastroenterology. 2003;98(8):1790–1796. doi: 10.1111/j.1572-0241.2003.07591.x. [DOI] [PubMed] [Google Scholar]
- 32.Harari D, Gurwitz JH, Avorn J, Bohn R, Minaker KL. Bowel habit in relation to age and gender. Findings from the National Health Interview Survey and clinical implications. Arch Intern Med. 1996;156(3):315–320. [PubMed] [Google Scholar]