Abstract
Context
Limited data exist about blood lead levels and potential exposures among children living in Puerto Rico. The Puerto Rico Department of Health has no formal blood lead surveillance program.
Objectives
We assessed the prevalence of elevated BLLs [≥ 5 micrograms (μg) of lead per deciliter (dL) of blood], household environmental lead levels, and risk factors for BLL among children less than 6 years old living in Puerto Rico in 2010.
Methods
We used a population-based cross-sectional sampling strategy to enroll an island-representative sample of Puerto Rican children less than 6 years old. We estimate the island-wide weighted prevalence of elevated BLL, and conducted bivariable and multivariable linear regression analyses to ascertain risk factors for elevated BLLs.
Results
The analytic dataset included 363 households and 439 children less than 6 years old throughout Puerto Rico. The weighted geometric mean BLL of children less than 6 years old was 1.57 μg/dL [95% confidence interval (CI) = 1.27, 1.88). The weighted prevalence of children less than 6 years old with BLLs ≥ 5 μg/dL was 3.18% (95% CI = 0.93, 5.43) and for BLLs ≥ 10 μg/dL was 0.50% (95% CI = 0, 1.31). Higher mean BLLs were significantly associated with data collection during the summer months, a lead-related activity or hobby of anyone in the residence and maternal education less than 12 years. Few environmental lead hazards were identified.
Conclusions
The prevalence of elevated BLLs among Puerto Rican children less than 6 years old is comparable to the most recent (2007 – 2010) U.S. national estimate [BLLs ≥ 5 μg/dL = 2.6% (95% CI = 1.6, 4.0)]. Our findings suggest targeted screening of specific higher-risk groups of children less than 6 years old can replace island-wide or insurance specific policies of mandatory blood lead testing in Puerto Rico.
Introduction
Lead is an environmental neuro-toxicant that affects nearly every system in the body.1 Lead can be found in paint, pottery, toys, traditional medicines, contaminated foods/beverages, batteries and electronics recycling products.2,3,4 Lead poisoning in children has been associated with decreased intelligence, anemia, attention deficit/hyperactivity disorder, increased dental caries, decreased growth, and impaired hearing and in high levels it may cause severe brain damage and death.1,5 Children, especially those who are less than 2 years old, are particularly susceptible to lead poisoning because their central nervous systems are still developing and they absorb more lead from their living and playing environments than adults.6 According to Centers for Disease Control and Prevention (CDC), no safe threshold of blood lead level (BLL) has been identified in children.5 In 2012, the CDC Advisory Committee on Childhood Lead Poisoning Prevention recommended replacing the use of the term “BLL of concern” with a reference range upper value defined as the 97.5th percentile of BLLs among U.S. children aged 1–5 years from two consecutive cycles of NHANES.7
Universal BLL testing is recommended among children 9 – 72 months of age (except in communities with sufficient data to conclude children are not at risk of exposure) as part of the American Academy of Pediatrics’ (AAP) Bright Futures Guidelines for Health Supervision.8 Lead screening in Puerto Rico is not routinely requested in pediatric practices, unless exposure is suspected. The Puerto Rico Department of Health (PRDH) has collected limited BLL screening information from children enrolled in the Head Start Program; however there is no formal BLL surveillance system for children less than 6 years old. A few studies have been conducted in Puerto Rico primarily among population groups considered to be at high risk for lead exposure. Data collected for the Head Start Program by PRDH during 1994-1995 found six out of two hundred children tested had an elevated BLL >10 μg/dL (PRDH, unpublished data). During 2003, an investigation conducted by Sánchez-Nazario and colleagues in Vega Baja-Puerto Rico found among 42 children less than 6 years old, BLLs ranged from 0.97 to 7.79 μg/dL and environmental house dust levels ranged from 0.12 to 98.3 micrograms per square foot (μg/ft2) with 17% of the households being above the Environmental Protection Agency action level of 40 micrograms μg/ft2.9 In contrast, a 2006 study found children between 1-7 years of age living in Puerto Rico were not at high risk for lead toxicity.10 In 2008, a study conducted to determine the association between BLL concentration and intellectual functioning in Vega Baja-Puerto Rico among a group of children aged 6-16 years found a mean BLL of 1.52 μg/dL and a non-significant association (p=0.097) with BLLs above 1.4 μg/dL and a below average score in the verbal subscale test.11 During 2009, the PRDH received unpublished reports of elevated BLLs among Puerto Rican children who were tested while visiting mainland United States. The exposure source of the children was frequently unknown so being from Puerto Rico was a hypothesized risk factor.
Methods
Study Design
This 2010 study included a population-based, cross-sectional, island-representative sample of children less than 6 years old, administration of personal and household risk factor questionnaires to children's parents, and environmental sampling. The study population included children less than 6 years old who lived at the same Puerto Rico address for at least the past 9 months. A population-based cluster survey design was used to select households throughout Puerto Rico. Because the island is approximately 100 × 35 miles, a simple random sample was not logistically feasible. The survey design was based on the Expanded Program on Immunization model, but the accuracy was improved based on the recommendations of Brogan and colleagues12 and Kish.13
The sampling frame for the survey was created by dividing the island into clusters using U.S. census block groups as the clusters. The island consists of 2,453 block groups and 861 census tracts.14 Clusters were stratified by age of housing based on U.S. Census data (2000). The small island municipalities of Vieques and Culebra, former U.S. naval training ranges, were made ineligible for selection due to separate environmental health studies and possible bio-monitoring occurring among residents. Clusters were selected within a stratum with probability proportional to estimated population (children 1-5 years of age) size (PPS) method. Forty clusters were randomly selected using PPS, 20 of these were oversampled (>20% for pre-1950 housing, when the use of lead-based paint may have been more common). These 20 clusters with high proportion of pre-1950 housing were oversampled so areas of potential lead exposure were well represented in the study. Three clusters were replaced due to concerns for the safety of data collection team members by randomly selecting an adjacent cluster with a similar number of estimated children aged 1-5 years. A sample of households was selected within each chosen cluster by using systematic random sampling. All households had equal selection probability within a cluster. All eligible children from each selected household were enrolled into the study.
Using tax assessor data prepared by the Centro de Recaudación de Ingresos Municipales or CRIM (Municipal Internal Revenue Center), an address was randomly selected from the full roster of residential addresses in the cluster as a starting point for each data collection team. After visiting the first address, each data collection team went to the next address on the same side of the street, in descending order, and then up the opposite side until its quota of households was met or until the street ended. The quota of households was 10 per cluster and was conducted using systematic random sampling per cluster. If the quota was not met when the street ended, the team went to another street on its list, which was mapped in a clockwise direction to better ascertain location of teams at all times. To enumerate, the data collection teams noted the outcome of each household visit (i.e., eligible, ineligible, refused, vacant). A household was recorded as “occupied but the residents not at home” only after the team had visited the household at least 3 times over 2 days. To increase participation rates, PRDH note card with a phone number were left at vacant households. Participating families received a $15 gift certificate to a large toy chain store to thank them for their time and effort. A household was defined as the sampling unit (i.e., an area that included at least 1 bedroom, 1 bathroom, and a kitchen) where people could live at a given address, and many addresses visited included multiple families. We enrolled one household from addresses with >1 family.
A data collection team comprised at least 1 PRDH staff member, 1 CDC staff member or 1 PRDH-trained field epidemiology fellow, 1 other health professional, and 1 community member. Team members were trained in cultural sensitivity, data collection, capillary and venous blood drawing, environmental sampling, referrals and personal safety. At least two team members were fluent in Spanish language. Approximately 10 teams were used during the 6 week study period (4 weeks during June/July 2010 and 2 weeks during November 2010). Teams conducted field work from late morning to evening, including weekends. Local community leaders and law enforcement officials were notified about the study. The study was announced in several island newspapers, including El Nuevo Día.
Sample size was calculated to provide a sample for a 95% confidence interval of ± 1.5% around an estimated prevalence estimate of 4.8%. The sample size calculation assumed an intra-cluster correlation of 0.04, a design effect of 1.36, and response rate of 80%.
Questionnaire Administration
Study teams administered 3 questionnaires in Spanish to a consenting parent or legal guardian in each eligible household: 1) a child questionnaire to obtain demographic factors and assess lead exposure risk factors, 2) a parental questionnaire, and 3) a household questionnaire. Questionnaire administration averaged 30 minutes in total. A random sample of households also received an environmental questionnaire which included sampling and a visual inspection of the residence and yard.
Environmental Sampling
Two hundred and fifty-seven (257) randomly selected enrolled households received environmental sampling [interior paint X-ray fluorescence (XRF), soil, water, and interior dust]. Environmental sampling consisted of the collection of one composite exterior soil sample from 5 bare soil area locations where resident children less than 6 years old were said to play. A soil-lead hazard for play areas is defined as soil with lead equal to or exceeding 400 parts per million (micrograms per gram).15 A 5 ml water sample was collected from the tap used for drinking/cooking. An unacceptable water lead level was defined as 0.015 parts per million (ppm) or 15 micrograms per liter.16 Two composite dust wipe samples were collected from the floor using a square grid, specifically in the area where the resident child less than 6 years old reportedly played and from the entry way of the house. An elevated dust floor measurement was defined as 40 μg/ft2.17 A second composite dust wipe sample was measured and collected from the bedroom window sill(s) of the resident children less than 6 years old. An elevated dust window measurement was defined as 250 μg/ft2.17 Lastly, a small number of households had interior portable-XRF measurements conducted to determine the presence of lead-based paint inside the residence. A rough schematic sketch of the residence was made and measurements were recorded.
Health Education
At the end of questionnaire administration, teams provided EPA, CDC and PRDH educational material (in Spanish) about lead exposure prevention and referrals to other child and/or housing-related services. At the end of the study, four free BLL screenings (November 2010–May 2011) were provided by CDC and PRDH to children not selected in the study.
Blood Lead Survey
Trained study team members (i.e., physicians or nurses) collected capillary BLL samples because it is convenient and less costly than venous sampling. Previous studies have reported a high correlation between capillary and venous sampling (the preferred diagnostic method).18,19,20 CDC staff with extensive field experience trained nurses and physicians in the appropriate collection of 200 μL samples of capillary blood from each eligible child in the household (National Committee for Clinical Laboratory Standards, 2001). Capillary samples were analyzed within 24 hours of collection using the LeadCare II (Magellan Diagnostics; Billerica, Massachusetts) point of care BLL analyzer. The instrument was modified by the manufacturer for this study to report BLLs less than the limit of detection (3.3 μg/dL), because lower BLLs were expected and population estimates were needed. In 2006, the LeadCare II Blood Lead system was categorized as a waived device under the Clinical Laboratory Improvement Amendment (CLIA).21 This CLIA waiver demonstrates its ease of use and is ideal for use in the field. The instrument was calibrated pre- and post-BLL analyses. A venous blood sample was randomly and exclusively collected from 9% of the participating children by trained PRDH nurses and sent to CDC, National Center for Environmental Health, Division of Laboratory Sciences (DLS) for quality-control. The DLS used the Perkin-Elmer Inductively Coupled Plasma Mass Spectrometer with Dynamic Reaction Cell Technology (ELAN® DRC II) (PerkinElmer Norwalk, CT, www.perkinelmer.com) to test venous blood samples for lead. Children with BLLs ≥ 10 μg/dL had a venous confirmatory test conducted within 3 days.
Results to Study Participants
Child BLL results were provided via U.S. mail to a parent or legal guardian within one week from date of sample collection. Letters explained results to participants and outlined steps to coordinate medical follow-up, if needed. Confirmatory venous testing was conducted for children with a BLL of ≥ 10 μg/dL based on CDC guidelines.22 Environmental sampling results with an interpretation of findings were provided via U.S. mail to parents or legal guardians within 2 months from sample collection date.
Data Analysis
Data were entered into FAST software (Montgomery, AL) and 15% of records were completely reentered to confirm accuracy of data entry. Data were analyzed using complex survey procedures in SAS version 9.3 (SAS Institute Inc., Cary, NC) and SUDAAN version 11.0.0 (Research Triangle Institute, Research Triangle Park, NC) software to account for unequal weighting, clustering and stratification.
The sampling frame for the study was 2000 U.S. census block groups. The survey was a stratified two stage cluster design where the first stage of sampling was block groups and the second stage was a household with at least one child less than 6 years old within a selected block group. The sampling frame of block groups was divided into two strata based on the age of housing: 1) pre-1950 and 2) 1950 and newer. To attempt to capture more children with elevated BLLs, we oversampled block groups with older housing - allocating 20 of the 40 clusters to the pre-1950 housing, when the use of lead paint may have been more common. To calculate prevalence estimates and make inferences about the entire population of children less than 6 years old residing in Puerto Rico, we created sampling weights for both households and children. Sampling weights were adjusted to account for any unequal selection probabilities that occurred to account for non-response and calibrate to the census population.
Descriptive statistics were used to describe household and child characteristics. Linear regression techniques were used to examine risk factors for elevated BLLs that were obtained from the household and child questionnaires. BLL concentrations were markedly right-skewed and were natural log-transformed for linear regression statistical analyses. Geometric mean and ratio of geometric mean estimates were back-transformed. Risk factors included child age and gender, child activities and health conditions, whether the child had ever traveled outside of Puerto Rico > 2 weeks in his/her entire life, previous renovation activity in the household, frequency of painting the residence, presence of household pets, all resident smoking status, mother's education level, lead-related occupation or activities, use of household remedies, herbal remedies or folk medicines, receipt of public or Section 8 housing, receipt of public assistance, house ownership status, and data collection month. On the basis of a previous study, age of the child was selected as a potential confounding variable.23 Age of the residence was not considered as a confounder because of concerns about the quality of reporting of this specific information (90% missing values). Most children (90%) enrolled in the survey were currently on or had received public assistance, thus this variable was also discounted as a confounder.
Bi-variable analyses were conducted to assess each risk factor's association with elevated BLLs; risk factors significantly associated with elevated BLLs were then evaluated separately in multivariable analyses. The initial multivariable analysis assessed each risk factor while the selected confounding variable and interaction terms were assessed. During the second multivariable analysis, we used a forward-selection strategy to add 1 risk factor variable at a time to the most predictive model, including the a priori confounder, until all risk factors in the model were statistically significant. Only statistically significant risk factors (at the p < 0.10 level) identified in the initial multivariable analysis were included in the second multivariable analysis; interactions between risk factors and the confounding variable were assessed during both analyses. The final model only included age and risk factors significant at the p < 0.05 level. Variance inflation factors were used to assess collinearity between variables in the predictive models.
Results
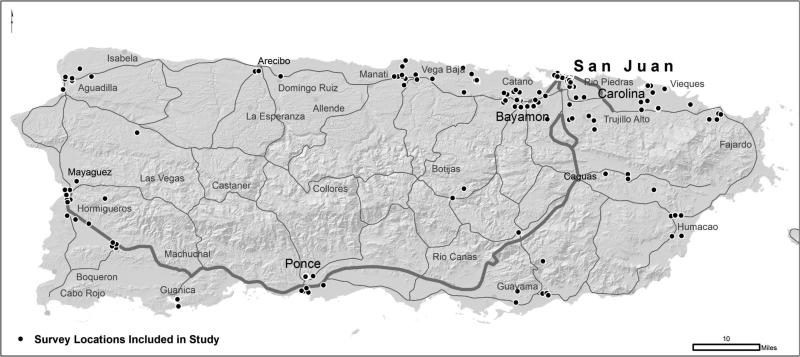
A total of 377 households and 456 children less than 6 years old were enrolled in our population-based survey in Puerto Rico. Of the 1,397 households visited, 855 (61.2%) were ineligible for participation (e.g., no children less than 6 years old lived at the residence, residence was unoccupied, or address was not a residence). The eligible household response rate was 377 (69.6%). The refusal rate was 5.3%. The most common reason for refusal was the inability to get parental or legal guardian permission to join the study. Seventeen children from 14 households were excluded from the analyses because insufficient (n = 15) or no (n = 2) blood was collected. The analytic dataset comprised 363 households and 439 children less than 6 years old (Figure 1).
Figure.
Study sampling locations, Puerto Rico, 2010
Child Characteristics
Gender and age were not recorded for 7 (1.6%) children; attempts to locate families to obtain missing data were unsuccessful. The average age of children was 3.3 years, and among those with available gender information, 234 (53.3%) were male; most children 410 (93.4%) were born in Puerto Rico. The most commonly reported racial groups were multi-racial (n=213 or 48.5%) and white (n=161 or 36.7%). Almost all children were Hispanic (n=423 or 96.4%), with 409 (96.7%) describing their Hispanic ethnicity type as Puerto Rican. One hundred and twenty-five children (28.5%) were reported by a parent or legal guardian to have had a previous BLL test, 117 (26.7%) were reported to have asthma (as told by a health care provider), and 391 (89.0%) were reported to have up-to-date vaccinations. The parent or legal guardian reported 165 (37.6%) children spent more than 20 hours per week other than the primary household. Almost half (47.9%) of these children were reported to spend that time at school. The majority of children (397, 90.4%) were currently receiving or had received public services, the most common form of assistance being government medical insurance (n=348 or 79.3%; Table 1). The parent or legal guardian reported 231 (65%) of the households had a child that played outside the house for an average of 2.9 hours per day (range 1 - 10 hours) (Table 2).
Table 1.
Characteristics and potential risk factors for lead exposure among children enrolled in the blood lead prevalence study, Puerto Rico, 2010
| Child characteristic | Number (%) (N=439) | Median blood lead level (μg/dL) (N=439) | Geometric mean blood lead level (μg/dL) (95% CI) (N=426,718) |
|---|---|---|---|
| Total | 439 (100) | 1.40 | 1.57 (1.27, 1.88) |
| Data collection month (2010) | |||
| June | 170 (38.7) | 1.58 | 1.60 (1.45, 1.79) |
| July | 91 (20.7) | 1.60 | 1.42 (1.30, 1.54) |
| November | 178 (40.6) | 1.05 | 0.88 (0.64, 1.20) |
| Number of residents | |||
| 2 | 20 (4.6) | 1.55 | 1.75 (1.15, 2.69) |
| 3 | 86 (19.6) | 1.40 | 0.91 (0.58, 1.43) |
| 4 | 121 (27.5) | 1.40 | 1.08 (0.78, 1.51) |
| 5 | 111 (25.2) | 1.38 | 1.25 (1.07, 1.45) |
| >5 | 80 (18.2) | 1.30 | 1.36 (1.11, 1.67) |
| Missing | 21 (4.8) | 1.30 | 1.49 (0.96, 2.32) |
| Number of children <6 years of age sampled in household | |||
| 1 | 355 (80.8) | 1.40 | 1.11 (0.88, 1.39) |
| 2 | 72 (16.4) | 1.40 | 1.42 (1.13, 1.79) |
| 3 | 11 (2.5) | 1.93 | 1.77 (0.88, 3.60) |
| 4 | 1 (0.2) | ----- | ----- |
| Gender | |||
| Male | 234 (53.3) | 1.49 | 1.22 (0.98, 1.51) |
| Female | 198 (45.1) | 1.30 | 1.08 (0.84, 1.40) |
| Missing | 7 (1.6) | 2.10 | 1.52 (0.68, 3.39) |
| Age (months) | |||
| <12 | 8 (1.8) | 1.51 | 2.46 (1.22, 5.00) |
| 12-23 | 98 (22.3) | 1.40 | 1.14 (0.75, 1.72) |
| 24-35 | 86 (19.6) | 1.40 | 1.32 (1.04, 1.67) |
| 36-47 | 76 (17.3) | 1.45 | 1.19 (0.91, 1.54) |
| 48-59 | 81 (18.5) | 1.40 | 1.14 (0.93, 1.39) |
| 60-71 | 83 (18.9) | 1.12 | 0.90 (0.62, 1.34) |
| Missing | 7 (1.6) | 2.10 | 1.52 (0.68, 3.39) |
| Race | |||
| Asian | 1 (0.2) | ----- | ----- |
| Black or African American | 43 (9.8) | 1.85 | 1.86 (1.54, 2.25) |
| White | 161 (36.7) | 1.30 | 1.06 (0.75, 1.51) |
| Multi-racial (more than 1 race) | 213 (48.5) | 1.39 | 1.15 (0.93, 1.42) |
| Other | 1 (0.2) | ----- | ----- |
| Refused | 9 (2.0) | 1.50 | 1.12 (0.83, 1.51) |
| Missing | 11 (2.5) | 1.42 | 1.11 (0.54, 2.27) |
| Child Birth Place | |||
| Puerto Rico | 410 (93.4) | 1.40 | 1.15 (0.92, 1.43) |
| Other | 21 (4.8) | 1.80 | 1.16 (0.78, 1.75) |
| Missing | 8 (1.8) | 1.73 | 1.43 (0.73, 2.77) |
| Child has ever traveled outside of Puerto Rico > 2 weeks? | |||
| Yes | 104 (23.7) | 1.40 | 1.08 (0.82, 1.45) |
| No | 323 (73.6) | 1.38 | 1.16 (0.92, 1.48) |
| Missing | 12 (2.7) | 2.40 | 1.70 (1.16, 2.46) |
| Travel outside of Puerto Rico location (multiple answers allowed): | |||
| U.S. Mainland | 65 (62.5) | 1.40 | 1.05 (0.79, 1.38) |
| Dominican Republic | 13 (12.5) | 1.90 | 1.57 (1.19, 2.10) |
| Central/South America | 2 (1.9) | ----- | ----- |
| Other | 2 (1.9) | ----- | ----- |
| Missing | 32 (30.8) | 1.70 | 1.08 (0.84, 1.39) |
| TOTAL | 104 (100) | ----- | ----- |
| Type of Services Child Currently or Ever Received (respondents could choose > 1 answer) | |||
| Government Medical Insurance (Reforma) | 348 (29.8) | 1.48 | 1.28 (1.06, 1.57) |
| Public Housing | 95 (8.1) | 1.50 | 1.46 (1.38, 1.57) |
| Section 8 Voucher | 36 (3.1) | 1.50 | 0.95 (0.50, 1.82) |
| Food Stamps | 313 (26.8) | 1.40 | 1.27 (1.06, 1.54) |
| Women Infant Children Program (WIC) | 325 (27.8) | 1.40 | 1.27 (1.03, 1.58) |
| Other Form of Public Assistance | 9 (0.8) | 2.31 | 1.23 (0.28, 5.47) |
| None/Missing | 42 (3.6) | 1.00 | 0.76 (0.45, 1.28) |
| TOTAL | 1,168 (100) | ----- | ----- |
| Previous Blood Lead Test (parent/guardian reported) | |||
| Yes | 125 (28.5) | 1.55 | 1.34 (1.03, 1.73) |
| No | 304 (69.2) | 1.30 | 1.08 (0.84, 1.40) |
| Missing | 10 (2.3) | 1.73 | 1.72 (1.02, 2.89) |
| Asthma (told by a health care provider) | |||
| Yes | 117 (26.6) | 1.33 | 1.12 (0.85, 1.46) |
| No | 309 (70.4) | 1.40 | 1.15 (0.93, 1.42) |
| Don't Know | 2 (0.5) | ----- | ----- |
| Missing | 11 (2.5) | 1.80 | 1.77 (1.17, 2.69) |
| Asthma symptoms such as shortness of breath, coughing, or wheezing | |||
| Yes | 169 (38.5) | 1.40 | 1.19 (0.93, 1.52) |
| No | 261 (59.4) | 1.39 | 1.14 (0.91, 1.42) |
| Missing | 9 (0.8) | 2.10 | 1.20 (0.86, 1.67) |
| Up-to-date vaccinations (parent/guardian reported) | |||
| Yes | 391 (89.1) | 1.40 | 1.16 (0.94, 1.43) |
| No | 27 (6.2) | 1.90 | 0.95 (0.41, 2.18) |
| Missing | 21 (4.8) | 1.20 | 1.31 (0.88, 1.95) |
| Child spends > 20 hours/week anywhere other than household | |||
| Yes | 165 (37.6) | 1.20 | 1.01 (0.73, 1.39) |
| No | 267 (60.8) | 1.48 | 1.30 (1.12, 1.51) |
| Missing | 7 (1.6) | 2.10 | 1.52 (0.68, 3.39) |
| Potential Child Exposures | |||
| Use of household remedies, herbal remedies or folk medicines (e.g., Azarcon and Greta) | |||
| Yes | 53 (12.1) | 1.76 | 1.20 (0.90, 1.60) |
| No | 375 (85.4) | 1.40 | 1.15 (0.92, 1.43) |
| Missing | 11 (2.5) | 1.36 | 1.36 (0.84, 2.23) |
| Observation of child eating or mouthing non-food items | |||
| Yes | 301 (68.6) | 1.37 | 1.20 (0.95, 1.51) |
| No | 127 (28.9) | 1.40 | 1.06 (0.79, 1.42) |
| Missing | 11 (2.5) | 1.36 | 1.28 (0.70, 2.39) |
| Child washes hands before eating | |||
| Yes, often | 279 (63.6) | 1.40 | 1.11 (0.89, 1.39) |
| Yes, sometimes | 105 (23.9) | 1.40 | 1.21 (0.90, 1.63) |
| Rarely | 31 (7.1) | 1.02 | 1.12 (0.88, 1.43) |
| No, never | 7 (1.6) | 1.40 | 1.68 (1.11, 2.59) |
| Missing | 17 (3.9) | 1.40 | 1.72 (1.22, 2.44) |
Table 2.
Selected household characteristics enrolled in the blood lead prevalence study, Puerto Rico, 2010 (N=355)
| Household characteristic |
Number (%) N=355 |
|---|---|
| Ownership Type | |
| Owner occupied | 137 (38.6) |
| Rental | 77 (21.7) |
| Public housing | 62 (17.5) |
| Publicly subsidized (Section 8) | 23 (6.5) |
| Other | 44 (12.3) |
| Missing | 12 (3.3) |
| Dwelling Type | |
| Single family household | 231 (65.1) |
| Multiple family household | 30 (8.5) |
| Two-Unit apartment (duplex) | 24 (6.7) |
| > Two-unit apartment (duplex) | 47 (13.2) |
| Other | 11 (3.1) |
| Missing | 12 (3.3) |
| Year Built (resident reported) | |
| pre-1950 | 2 (0.6) |
| 1950-1969 | 4 (1.1) |
| 1970-1989 | 13 (3.5) |
| Post-1989 | 18 (5.1) |
| Don't know/missing | 319 (89.8) |
| Mother's level of education | |
| None | 3 (0.8) |
| Eighth grade | 61 (17.1) |
| High school graduate or GED | 156 (43.9) |
| Trade school | 17 (4.8) |
| College or higher | 113 (31.8) |
| Missing | 5 (1.4) |
| Father's level of education | |
| None | 10 (2.8) |
| Eighth grade | 78 (22.0) |
| High school graduate or GED | 131 (36.9) |
| Trade school | 16 (4.5) |
| College or higher | 79 (22.2) |
| Missing | 41 (11.5) |
| Potential Household Exposures | |
| Lead occupation of anyone in household (multiple answers allowed) | |
| Smelting | 16 (4.4) |
| Auto repair | 21 (5.8) |
| Work on firing ranges | 2 (0.5) |
| Painting | 8 (2.2) |
| Manufacturing of ceramics | 1 (0.2) |
| Manufacturing of electrical components | 11 (3.0) |
| Manufacturing of batteries | 0 |
| Wire and cable production | 11 (3.0) |
| Pottery making | 0 |
| None of above | 268 (73.6) |
| Missing | 26 (7.1) |
| TOTAL | 364 |
| Lead hobby of anyone in household (multiple answers allowed) | |
| Automobile repair | 31 (8.6) |
| Metal recycling | 4 (1.1) |
| Making fishing sinkers | 5 (1.4) |
| Stained glass | 0 |
| Ceramics/pottery | 1 (0.3) |
| Shooting guns | 0 |
| Jewelry making | 2 (0.5) |
| None of above | 284 (79.3) |
| Missing | 32 (8.9) |
| TOTAL | 358 |
| Any plates, bowls, or food storage containers made of ceramic or earthenware | |
| Yes | 291 (82.0) |
| No | 50 (14.1) |
| Don't know | 2 (0.6) |
| Missing | 12 (3.3) |
| Household renovated during previous 6 months (inside or outside) | |
| Yes | 64 (18.0) |
| No | 271 (76.3) |
| Don't know | 5 (1.4) |
| Missing | 15 (4.2) |
| Frequency household is swept or cleaned | |
| Daily | 252 (71.0) |
| At least weekly | 88 (24.8) |
| At least monthly | 1 (0.3) |
| Less than once a month | 1 (0.3) |
| Never | 0 |
| Don't know | 0 |
| Missing | 13 (3.7) |
| Frequency interior of house is painted | |
| More than once a year | 34 (9.6) |
| Once a year | 173 (48.7) |
| Every two years | 66 (18.6) |
| Every five years | 39 (11.0) |
| Don't remember | 29 (8.2) |
| Missing | 14 (3.9) |
| Source of water used for drinking/cooking | |
| Public water system/piped mun. source (Triple A: Acueductos y Alcantarillados) | 330 (93.0) |
| Non PRASA source | 4 (1.1) |
| From a well | 6 (1.7) |
| Rain water collection | 0 |
| Other | 1 (0.3) |
| Don't know | 3 (0.8) |
| Missing | 11 (3.1) |
| Do(es) child(ren) play outside house | |
| Yes | 231 (65.1) |
| No | 111 (31.2) |
| Don't know | 0 |
| Missing | 13 (3.5) |
| Does anyone smoke tobacco inside the household (includes hanging tobacco products out the window)? | |
| Yes | 47 (13.2) |
| No | 298 (83.9) |
| Don't know | 0 |
| Missing | 10 (2.8) |
| Are there any pets in the household? | |
| Yes | 176 (49.6) |
| No | 166 (46.8) |
| Don't know | 0 |
| Missing | 13 (3.5) |
Household Characteristics
Among participating households, median occupancy was 4 persons (range 2 - 13). Among those who knew the age of housing, 18 (5.1%) housing units were built post-1989; most residents (89.9%) did not know the year their residence was built. Among the 355 households, 137 (38.6%) of the families owned the residence, 231 (65.1%) had a single family dwelling type. Other notable socio-demographic household characteristics reported were 47 (13.2%) had a resident who was a current smoker and 156 (43.9%) children had a mother who completed high school or obtained a general education degree (GED) (Table 2).
Blood Lead Results
Among the 439 children tested, 392 (89.3%) had capillary samples and 47 (10.7%) had venous samples. Mean BLLs did not significantly differ between capillary samples (1.7 μg/dL) and venous samples (1.7 μg/dL) (p=0.965). Overall, 15 (3.6% un-weighted) children in the study had BLLs ≥ 5 μg/dL, and 3 (0.7% un-weighted) children had BLLs ≥ 10 μg/dL. The weighted geometric mean BLL of children less than 6 years old was 1.57 μg/dL (95% CI= 1.27, 1.88). The weighted prevalence of children less than 6 years old with BLLs ≥ 5 μg/dL was 3.2% (95% CI = 0.9, 5.4) and the weighted prevalence of children less than 6 years old with BLLs ≥ 10 μg/dL was 0.5% (95% CI = 0, 1.3). The weighted percent of children less than 6 years old with BLLs ≥ 5 μg/dL residing in pre-1950 housing clusters [4.2% (95% CI= 1.4, 11.8)] differed little compared with percent of children less than 6 years old with BLLs ≥ 5 μg/dL residing in clusters with mostly post-1950 housing [3.1% (95% CI= 1.4, 6.6)].
Environmental Characteristics
Among the 259 (71.3%) households randomly selected for environmental sampling, 19 (7.3%) had XRF paint assessment, 178 (68.7%) had soil assessment, 230 (88.8%) had a dust window assessment, 235 (90.7%) had a dust floor assessment, and 257 (99.2%) had a tap water assessment (Table 3). Environmental sampling results showed water levels above the EPA action level for water in 3 (1.2%) households, 1 household had an elevated floor-dust lead, 1 household had an elevated window-dust lead, 1 household had an elevated XRF measurement, and no households had elevated soil lead levels. Six dust wipe controls were collected. Results of the dust wipe control samples were below limit of detection.
Table 3.
Household (HH) Environmental Sampling Results, Puerto Rico, 2010 (N=259)
| Environmental Sample Type | Number of HHs Sampled (N=259) | Percent of HHs Sampled | Min/Max | Number of HHs Exceeding Elevated Lead Level (%) | Elevated Lead Level Definition |
|---|---|---|---|---|---|
| Interior paint XRF | 19 | 7.3 | 0.0 - 1.05 mg/cm2 | 1 (5.3) | 1.0 mg/cm2 |
| Soil | 178 | 68.7 | 2.2 - 240 ppm (mcg/g) | 0 | 400 ppm (μg/g) |
| Water | 257 | 99.2 | < 3 - 22 mcg/L | 3 (1.2) | 15 mcg/L |
| Dust Floor Composite | 235 | 90.7 | < 0.5 - 180 μg/ft2 | 1 (0.4) | 40 μg/ft2 |
| Dust Window | 230 | 88.8 | < 0.5 - 115.2 μg/ft2 | 0 | 250 μg/ft2 |
Risk Factors
Forty-three (12.0%) households had a resident whose activities or hobbies involved lead, such as automobile repair, metal recycling, fishing sinker making, ceramics/pottery or jewelry making. Seventy-one (19.5%) households had a resident whose occupation involved lead, such as smelting, working on a firing range, battery recycling or manufacturing, painting or construction, and automobile or radiator repair. Two hundred and ninety-one (82.0%) households reported having plates, bowls, or food storage containers made of ceramic or earthenware (these items were not tested for presence of lead), 64 (18.0%) households were renovated (inside or outside) during the previous 6 months, 207 (58.3%) households reported painting once per year or more, and 176 (49.6%) households reported having pets (Table 2).
Fifty-three (12.1%) children were reported to use household/herbal remedies or folk medicines, 301 (68.6%) children were reported to eat or mouth non-food items, and 38 (8.7%) children were reported to rarely or never wash hands before eating (Table 1).
In weighted bi-variable analyses, and after adjusting for child's age the log of the child's BLL was independently significantly associated with June/July data collection months (p=0.0021), lead hobby of a household resident (p=0.005), mother's education achievement less than High School or GED (p=0.047), absence of pets in the household (p=0.0566), and child currently or ever receiving public services (p=0.0725) (Table 4). Based on weighted multivariable analyses, after adjusting for child's age, the log of the child's BLL was significantly associated with June/July data collection months (p=0.0055), lead hobby of a household resident (p=0.0302) and mother's education achievement less than High School or GED (p=0.0088) (Table 5). A co-linearity assessment did not identify significant correlations between variables in any of the models.
Table 4.
Weighted bi-variable linear regression age-adjusted estimates of the associations between log of BLL and other study variables, Puerto Rico, 2010 (N=426,718)
| Exposure variable | Geometric Mean* BLL (95% CI) | Beta (SE) | Ratio of geometric means (95% CI) | p Value |
|---|---|---|---|---|
| Data collection month (2010) | 0.54 (0.16) | 1.72 (1.23, 2.39) | 0.0021 | |
| June/July | 1.52 (1.36, 1.70) | |||
| November | 0.89 (0.65, 1.21) | |||
| Observation of child eating or mouthing non-food items | 0.08 (0.13) | 1.09 (0.83, 1.40) | 0.5610 | |
| Yes | 1.19 (0.94, 1.48) | |||
| No | 1.09 (0.84, 1.43) | |||
| Child washes hands before eating | 0.02 (0.14) | 1.02 (0.77, 1.38) | 0.8724 | |
| Rarely or does not | 1.16 (0.90, 1.51) | |||
| Sometimes or often | 1.14 (0.90, 1.43) | |||
| Child plays outside house | 0.12 (0.14) | 1.13 (0.85, 1.49) | 0.4065 | |
| Yes | 1.19 (0.96, 1.46) | |||
| No | 1.05 (0.76, 1.45) | |||
| Pets present in household | −0.18 (0.09) | 0.84 (0.69, 1.01) | 0.0566 | |
| Yes | 1.06 (0.88, 1.30) | |||
| No | 1.28 (1.01, 1.62) | |||
| Interior of house painted | −0.05 (0.12) | 0.95 (0.74, 1.22) | 0.7027 | |
| Once per year or more | 1.15 (0.90, 1.49) | |||
| Every two years or less | 1.21 (0.99, 1.48) | |||
| Household renovated during previous six months | 0.21 (0.13) | 1.23 (0.94, 1.62) | 0.1292 | |
| Yes | 1.34 (1.03, 1.75) | |||
| No | 1.09 (0.86, 1.38) | |||
| Presence of a smoker in the residence | −0.02 (0.12) | 0.98 (0.76, 1.26) | 0.8880 | |
| Yes | 1.13 (0.81, 1.57) | |||
| No | 1.15 (0.93, 1.41) | |||
| Lead hobby of anyone in household | 0.53 (0.18) | 1.70 (1.19, 2.46) | 0.0050 | |
| Yes | 1.79 (1.27, 2.51) | |||
| No | 1.05 (0.84, 1.30) | |||
| Lead occupation of anyone in household | 0.12 (0.17) | 1.13 (0.80, 1.58) | 0.4904 | |
| Yes | 1.25 (0.93, 1.65) | |||
| No | 1.11 (0.86, 1.42) | |||
| Use of household remedies, herbal remedies or folk medicines | 0.01 (0.15) | 1.01 (0.75, 1.36) | 0.9413 | |
| Yes | 1.16 (0.86, 1.57) | |||
| No | 1.15 (0.92, 1.43) | |||
| Any plates, bowls, or food storage containers made of ceramic or earthenware | −0.14 (0.19) | 0.87 (0.59, 1.27) | 0.4543 | |
| Yes | 1.12 (0.90, 1.39) | |||
| No | 1.28 (0.86, 1.93) | |||
| Mother's education | 0.31 (0.15) | 1.36 (1.00, 1.86) | 0.0469 | |
| < high school diploma/GED | 1.51 (1.15, 1.97) | |||
| ≥ high school | 1.09 (0.88, 1.38) | |||
| Child's gender | 0.11 (0.11) | 1.12 (0.90, 1.38) | 0.3059 | |
| Male | 1.21 (0.98, 1.51) | |||
| Female | 1.09 (0.84, 1.40) | |||
| Age, years (continuous) | N/A | −0.07 (0.05) | 0.93 (0.84, 1.03) | 0.1696 |
| Receipt of public housing or Section 8 housing | 0.08 (0.16) | 1.08 (0.79, 1.49) | 0.6243 | |
| Yes | 1.21 (0.90, 1.62) | |||
| No | 1.12 (0.89, 1.43) | |||
| Child currently or ever received public services | 0.54 (0.29) | 1.72 (0.95, 3.10) | 0.0725 | |
| Yes | 1.21 (1.00, 1.49) | |||
| No | 0.71 (0.40, 1.25) | |||
| Living in rental housing | 0 (0.17) | 1.00 (0.70, 1.42) | 0.9928 | |
| Yes | 1.14 (0.80, 1.60) | |||
| No | 1.14 (0.90, 1.43) | |||
| Child has asthma | 0.02 (0.09) | 1.02 (0.86, 1.21) | 0.8195 | |
| Yes | 1.16 (0.88, 1.54) | |||
| No | 1.14 (0.93, 1.39) | |||
| Child has ever traveled outside of Puerto Rico > 2 weeks | −0.03 (0.21) | 0.97 (0.64, 1.46) | 0.8769 | |
| Yes | 1.11 (0.72, 1.68) | |||
| No | 1.14 (0.91, 1.42) | |||
Least Squares Mean (Conditional Marginal)
Table 5.
Weighted multi-variable linear regression age-adjusted estimates of the associations between log of BLL and other study variables, (N=426,718)
| Exposure variable | Geometric Mean* BLL (95% CI) | Beta (SE) | Ratio of geometric means (95% CI) | p Value |
|---|---|---|---|---|
| Lead hobby of anyone in household | 0.34 (0.16) | 1.40 (1.03, 1.90) | 0.0302 | |
| Yes | 1.49 (1.08, 2.05) | |||
| No | 1.06 (0.90, 1.27) | |||
| Mother's education | 0.38 (0.14) | 1.46 (1.11, 1.92) | 0.0088 | |
| < high school diploma/GED | 1.54 (1.21, 1.93) | |||
| ≥ high school | 1.05 (0.87, 1.27) | |||
| Data collection month (2010) | 0.49 (0.17) | 1.63 (1.16, 2.27) | 0.0055 | |
| June/July | 1.43 (1.34, 1.55) | |||
| November | 0.88 (0.64, 1.22) | |||
| Age, years (continuous) | N/A | −0.07 (0.04) | N/A | 0.1443 |
Discussion
The prevalence of elevated BLLs among Puerto Rican children less than 6 years old is comparable to the most recent U.S. national estimate. Our findings suggest that targeted screening of specific higher-risk groups of children less than 6 years old can replace island-wide or insurance specific policies of mandatory blood lead testing in Puerto Rico.
The prevalence of BLLs ≥ 5 μg/dL among Puerto Rican children less than 6 years old is consistent with estimates for the U.S. mainland during 2007-2010. The U.S. mainland estimated percent of children less than 6 years old with BLLs ≥ 5 μg/dL is 2.6% (95% CI = 1.6, 4.0) compared to 3.2% (95% CI = 1.3, 1.9) among Puerto Rican children. The geometric mean BLL among Puerto Rican children less than 6 years old [1.6 μg/dL (95% CI = 1.3, 1.9)] is also very comparable to the U.S. estimate during the 2007-2010 time period [1.3 μg/dL (95% CI = 1.3, 1.4)].24 We found environmental lead levels in our survey population to be well below current regulatory standards among the vast majority of the 259 households assessed for environmental lead, with only 5 samples [representing 4 (1.5%) unique households] being above regulatory thresholds. As a U.S. commonwealth, Puerto Rico is subject to the same policies and regulations about lead concentrations in paint, gasoline, consumer products, etc. It is clear from our study that residential lead paint was not commonly used in housing and given the low soil lead levels we found, even when lead in gasoline was the primary fuel for vehicles, it is quite possible that fewer vehicles per capita resulted in less ambient contamination.
Routine BLL testing of Medicaid-eligible children at specific ages is currently mandatory in Puerto Rico. However, a recent study determined a child's Medicaid status was not predictive of having an elevated BLL,25 and recent recommendations have been established to allow public health officials flexibility in developing BLL screening strategies to reflect local risk for elevated BLLs.26 Our study demonstrates the risk for high BLLs in Puerto Rico is low. This type of finding may serve as a model for other jurisdictions developing waivers for universal BLL testing.
We identified three factors in multivariable analyses which predicted an association with higher mean BLLs among children: June/July data collection months, a household hobby or activity involving lead and maternal education less than 12 years. Although these differences are not clinically significant (i.e., BLL ≥ 5 μg/dL), a household lead hobby and maternal education less than 12 months may be useful risk assessment questions. Pediatric health care providers may ask Puerto Rican families if they have a hobby using lead, to determine which children to test. Household hobbies involving lead have been associated with childhood lead poisoning in other Caribbean countries,27,28 although sources of lead exposure can differ by island and country.29 Bernard and McGeehin (2003) reported education (High School graduate or not) of the reference adult was associated with being in the 5-10 μg/dL BLL group (OR: 1.5 [95% CI: 1.0, 2.2]) and the 10-20 μg/dL BLL group (OR: 2.2 [95% CI: 1.3, 3.8]) among children sampled in the Third NHANES, 1988–1994.23 Another study reported on the inverse relationship between child BLL and parental education attainment.30 Our findings demonstrating higher child mean BLLs during the summer months compared to November are consistent with numerous studies describing maximum BLLs during the summer months.31,32,33
In this study we did not find household occupations which can result in exposure to lead (i.e. pottery making, auto repair, battery manufacturing, etc.) significantly predicted higher mean BLLs in children less than 6 years old. This may be due to misclassification if the generalized category includes materials that may or may not contain lead or because lead-related occupations were identified in less than 20% of cases and small numbers may have limited our ability to identify a significant difference. There is a compelling body of literature describing the importance of ‘take home’ lead as an exposure source for children with high BLLs including lead dust contamination of family vehicles and child safety seats,34 automobile repair worker ‘take home’ lead exposure,35 construction worker ‘take home’ lead exposure,36 and a recent study of workers at a battery recycling facility in Puerto Rico.37
Clinical and public health practitioners can take measures to ensure children at risk for elevated BLLs are identified by continued collection of BLL testing data, review of these data to identify common risk factors, and systematic collection of data such as toxic release data that may indicate a new source of exposure. Resources previously used to screen low risk children can be targeted to this ongoing evaluation of exposure and strategies that control or eliminate sources of lead before children have high BLLs.
Our study had limitations. First, we were not able to assess possible differences between children who did and did not participate in the study. Second, using 2000 census data to construct our cluster sample sometimes led field teams to areas with few children less than 6 years old. Additionally, use of 2000 census data to weight our sample may not reflect current population estimates and age distribution. It is known that demographics in Puerto Rico have changed in recent years.14 Elevated BLLs among children is a rare event and they may be clustered in certain areas. In our study we did not find many children with elevated BLLs. To find potentially more children with elevated BLLs, we would need to oversample potential exposure areas (other than older housing) such as communities where occupational take home lead exposure occurs. Lastly, our results are not generalizable to children residing in Vieques and Culebra, areas of former U.S. Naval training ranges.
Nevertheless, this was a comprehensive prevalence study that included a face-to-face survey, BLL testing, environmental sampling and visual housing inspection, conducted during two different seasons (i.e., summer and fall during 2010) which allowed us to observe possible differences among children's behaviors and lead exposure risk factors. One of the main reasons we conducted this study was to investigate results from unpublished reports of Puerto Rican children with elevated BLLs while visiting mainland United States. Nonetheless, our survey did not find that a child ever traveling outside of Puerto Rico for more than 2 weeks was predictive of elevated BLLs.
Our findings support reports of comparable elevated BLLs among children living in Puerto Rico compared to other jurisdictions such as New York (NY) State (excluding NY City), with 1.1% of children less than 6 years old having BLLs ≥ 10 μg/dL during 2004-2007.38 However, it appears risk factors for elevated BLLs might be different compared to those reported stateside, where lead-based paint chips and dust are the major contributors to elevated BLLs. To better understand where population risks lie, continued surveillance and case investigations are required. Our findings suggest targeted screening of specific higher-risk groups of children less than 6 years old can replace costly island-wide or insurance specific policies of mandatory BLL testing in Puerto Rico. The PRDH is collecting and reviewing child BLL lab record data in its effort toward development of a child BLL surveillance system.
Acknowledgments
We thank these individuals for their dedication and hard work making this project successful: Darielys Cordero, Catherine Chacin, Ahmad Baghal, Margie Walling, Encijar Hassan Ríos, Jeff Jarrett, Charles Dodson, Carrie Dooyema, Sharunda Buchanan, W. Dana Flanders, Concepción Q. Longo, Ginger Chew, Elizabeth Hunsperger, Kathy Seikel, Luz B. Mojica, Norma Díaz, Edna Díaz, Julio Cadiz, Sandra Claudio Luciano, Mildred Rivera Luna, Magaly Escalera, Rachel Avchen, Payal Shah, Jennifer Cruz (CRIM) Ulises Feliciano Troche (CRIM) and Olga Cruz.
Funding: The project was funded by the U.S. Environmental Protection Agency (Interagency Agreement Number CE-10-010) and the Centers for Disease Control and Prevention.
Footnotes
Human Subjects Review: The study protocol 5934.0 received approval from Centers for Disease Control and Prevention IRB.
OMB Control Number: 0920-0008
Financial Interests Declaration: None of the authors have any potential competing financial interests regarding this submitted article.
References
- 1.Agency for Toxic Substances and Disease Registry . Toxicological profile for lead. US Department of Health and Human Services; Atlanta, GA: 2007. http://www.atsdr.cdc.gov/toxprofiles/tp.asp?id=96&tid=22. [PubMed] [Google Scholar]
- 2.U.S. Consumer Product Safety Commission . Staff Report on Lead and Cadmium in Children's Polyvinyl Chloride (PVC) Products. Washington, D.C.: 1997. [Google Scholar]
- 3.Centers for Disease Control and Prevention Lead poisoning associated with ayurvedic medications—five states, 2000–2003. MMWR. 2004;9,53(26):582–584. [PMC free article] [PubMed] [Google Scholar]
- 4.Environmental Protection Agency . Air Quality Criteria for Lead Final Report. Washington, DC: 2006. EPA/600/R-05/144aF-bF http://cfpub.epa.gov/ncea/cfm/recordisplay.cfm?deid=158823#Download. [Google Scholar]
- 5.Centers for Disease Control and Prevention . Preventing lead poisoning in young children. U.S. Department of Health and Human Services; Atlanta, GA: 2005. http://www.cdc.gov/nceh/lead/publications/prevleadpoisoning.pdf. [Google Scholar]
- 6.O'Flaherty E. A physiologically based kinetic model for lead in children and adults. Environ Health Perspect. 1998;106(suppl 6):1495–1503. doi: 10.1289/ehp.98106s61495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention . Low level lead exposure harms children: a renewed call for primary prevention. U.S. Department of Health and Human Services; Atlanta, GA: 2012. http://www.cdc.gov/nceh/lead/acclpp/final_document_030712.pdf. [Google Scholar]
- 8.Hagan JF, Shaw JS, Duncan P, editors. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents, Third Edition. Pocket Guide. American Academy of Pediatrics; Elk Grove Village, IL: 2008. [Google Scholar]
- 9.Sanchez-Nazario E, Mansilla-Rivera I, Deriux-Cortes J, Perez C, Rodriguez-Sierra C. The association of lead-contaminated house dust and blood lead levels of children living on a former landfill in Puerto Rico. Puerto Rico Health Sci J. 2003;22:153–159. [PubMed] [Google Scholar]
- 10.Centeno J, Collery P, Ernet G, Finkelman R, Gibb H, Etienne J. Comparison of blood lead levels in urban and rural Puerto Rican Children. Metal and Ions in Biology and Medicine. 2006;6:328–330. [Google Scholar]
- 11.Hassan-Rios E. Low Blood Lead Levels and Intelligence in Children residents of a former landfill, Puerto Rico.. Poster presentation, Council of State and Territorial Epidemiologists; Denver, CO. 2008. [Google Scholar]
- 12.Brogan D, Flagg EW, Deming M, Waldman R. Increasing the accuracy of the expanded programme on immunization's cluster survey design. Ann Epidemiol. 1994;4:302–311. doi: 10.1016/1047-2797(94)90086-8. [DOI] [PubMed] [Google Scholar]
- 13.Kish Leslie. Survey Sampling. Wiley; New York: 1965. p. 43. [Google Scholar]
- 14.U.S. Census 2013 https://www.census.gov/compendia/statab/2012/tables/12s1313.pdf.
- 15.Environmental Protection Agency Lead-Based Paint Poisoning Prevention in Certain Residential Structures. 40 CFR§745.65(c) 2001 http://www.access.gpo.gov/nara/cfr/waisidx_01/40cfr745_01.html.
- 16.Environmental Protection Agency 40 CFR Parts 141 and 142. Drinking water regulations: maximum contaminant level goals and national primary drinking water regulations for lead and copper. 56 FR 26460. 1991 http://water.epa.gov/drink/contaminants/basicinformation/lead.cfm.
- 17.Housing and Urban Development Subpart R—Methods and Standards for Lead-Paint Hazard Evaluation and Hazard Reduction Activities. 1999 http://www.hud.gov/offices/lead/library/enforcement/LSHR_Sub_R.pdf.
- 18.Parsons P, Reilly A, Esernio-Jenssen D. Screening children exposed to lead: an assessment of the capillary blood lead fingerstick test. Clin Chem. 1997;43(2):302–11. [PubMed] [Google Scholar]
- 19.Schlenker T, Fritz C, Mark D, et al. Screening for lead poisoning: comparability of simultaneously drawn capillary and venous blood samples. JAMA. 1994;271:1346–8. doi: 10.1001/jama.271.17.1346. [DOI] [PubMed] [Google Scholar]
- 20.Schonfeld D, Cullen M, Rainey P, Berg A, Brown D, Hogan J, et al. Screening for lead poisoning in an urban pediatric clinic using samples obtained by fingerstick. Pediatrics. 1994;94(2):174–9. [PubMed] [Google Scholar]
- 21.Magellan Biosciences Subsidiary Receives CLIA wavier from FDA for LeadCare II Machine. 2006 http://www.waivedleadcare.com/get-a-clia-certificate-of-waiver.html.
- 22.Centers for Disease Control and Prevention . Managing Elevated Blood Lead Levels Among Young Children: Recommendations from the Advisory Committee on Childhood Lead Poisoning Prevention. Atlanta: 2002. http://www.cdc.gov/nceh/lead/casemanagement/casemanage_main.htm. [Google Scholar]
- 23.Bernard SM, McGeehin MA. Prevalence of blood lead levels ≥ 5 μg/dL among US children 1 to 5 years of age and socioeconomic and demographic factors associated with BLLs 5 to 10 μg/dL, Third National Health and Nutrition Examination Survey, 1988-1994. Pediatrics. 2003;112:1308–13. doi: 10.1542/peds.112.6.1308. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention Blood lead levels in children aged 1-5 years — United States, 1999-2010. MMWR. 2013;62(13):245–248. [PMC free article] [PubMed] [Google Scholar]
- 25.Jones R, Homa D, Meyer P, et al. Trends in blood lead levels and blood lead testing among U. S. children aged 1 to 5 years: 1998-2004. Pediatrics. 2009;123:e376–e385. doi: 10.1542/peds.2007-3608. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention Recommendations for blood lead screening of Medicaid-eligible children aged 1-5 years: an updated approach to targeting a group at high risk. MMWR. 2009;58(RR09):1–11. [PubMed] [Google Scholar]
- 27.Matte T, Figueroa J, Ostrowski S, Burr G, Jackson-Hunt L, Keenlyside R. Lead poisoning among household members exposed to lead-acid battery repair shops in Kingston, Jamaica. Int J Epidemiol. 1989;18:874–81. doi: 10.1093/ije/18.4.874. [DOI] [PubMed] [Google Scholar]
- 28.Koplan J, Wells A, Diggory H, Baker E, Liddle J. Lead absorption in a community of potters in Barbados. Int J Epidemiol. 1977;6:225–9. doi: 10.1093/ije/6.3.225. [DOI] [PubMed] [Google Scholar]
- 29.Trepka M, Pekovic V, Santana J, Zhang G. Risk Factors for Lead Poisoning Among Cuban Refugee Children. Pub Hlth Rep. 2005;120:179–185. doi: 10.1177/003335490512000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee M, Chun O, Song W. Determinants of the blood lead level of US women of reproductive age. J Am Coll Nutr. 2005;24(1):1–9. doi: 10.1080/07315724.2005.10719436. [DOI] [PubMed] [Google Scholar]
- 31.Hunter JM. The summer disease: an integrative model of the seasonality aspects of childhood lead poisoning. Soc Sci Med. 1977;11:691–703. doi: 10.1016/0037-7856(77)90155-x. [DOI] [PubMed] [Google Scholar]
- 32.Havlena J, Kanarek M, Coons M. Factors associated with the seasonality of blood lead levels among preschool Wisconsin children. Wis Med J. 2009;108(3):151–5. [PubMed] [Google Scholar]
- 33.Yiin L, Rhoads G, Lioy P. Seasonal influences on childhood lead exposure. Environ Health Perspect. 2000;108(2):177–82. doi: 10.1289/ehp.00108177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention Childhood Lead Poisoning Associated with Lead Dust Contamination of Family Vehicles and Child Safety Seats --- Maine, 2008. MMWR. 2009;58(32):890–893. [PubMed] [Google Scholar]
- 35.Nunez C, Klitzman S, Goodman A. Lead exposure among automobile radiator repair workers and their children in New York City. Am J Ind Med. 1993;23:763–77. doi: 10.1002/ajim.4700230510. [DOI] [PubMed] [Google Scholar]
- 36.Whelan E, Piacitelli G, Gerwel B, et al. Elevated blood lead levels in children of construction workers. Am J Public Health. 1997;87:1352–5. doi: 10.2105/ajph.87.8.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention Take-Home Lead Exposure Among Children with Relatives Employed at a Battery Recycling Facility — Puerto Rico, 2011. MMWR. 2012;61(47):967–970. [PubMed] [Google Scholar]
- 38.New York State Department of Health Children with Elevated Blood Levels Among Children Tested Before Age 6 in New York State Excluding New York City, 2004-2007. 2014 https://apps.health.ny.gov/statistics/environmental/public_health_tracking/tracker/mapaction.map?activeTool=showLeadTabularBlood.