Abstract
We aimed to evaluate the Harkavy-Asnis Suicide Scale (HASS), one of the few self-report scales assessing suicidal behavior and ideation, and to identify predictors of suicide attempts with the goal of developing a model that clinicians can use for monitoring suicide-attempt risk. Participants were 131 pediatric Emergency Department patients with suicidal behavior. The HASS and Diagnostic Interview Schedule for Children (DISC-IV) were administered approximately two months after ED presentation. When compared with DISC-IV ratings, sensitivity of the HASS suicide attempt items was excellent (100%), and overall classification accuracy was 72%. Suicide attempt planning was the strongest predictor of suicide attempts.
Evaluating and monitoring suicidality is an essential component of clinical care. By 2020, an estimated 1.5 million people will die by suicide and an estimated 15 to 30 million will make attempts (Collins et al., 2011). Among youths (ages 10–24 years), suicide is the third leading cause of death in the United States, reducing suicide and suicide attempts are two of our national health promotion and disease prevention goals, and recent national estimates indicate that over 4600 youths through age 24 die by suicide each year (Kochanek et al., 2011). Given the magnitude of the problem, the Joint Commission has listed the identification of patients at risk for suicide as a National Patient Safety Goal (Goal 15.01.01) (U.S. Department of Health and Human Services, 2001), a goal that applies to psychiatric hospitals and all patients being treated for behavioral or emotional problems in general hospitals (http://www.jointcommission.org/assets/1/6/NPSG_EPs_Scoring_HAP_20110706.pdf) (The Joint Commission, 2011).
Two robust predictors of suicide attempts are past suicidal behavior and suicidal ideation (Brent et al., 2009; Prinstein et al., 2008; Spirito & Esposito-Smythers, 2006). A number of interviews and scales have been developed for the assessment of suicidal ideation and behavior in youths (Goldston, 2000; Posner et al., 2011). When assessing sensitive topics in adolescents such as suicidality, substance use, or sexual behavior, self-report scales have often shown greater sensitivity and may be more accurate in comparison to face to face interviews (Connor & Rueter, 2009; Prinstein, Nock, Spirito, & Grapentine, 2001). Self-report scales also have the advantage of being easy to administer, with no requirements for trained assessor time. The majority of self-report measures of suicidality in adolescents, however, focus on suicidal ideation and do not include assessments of suicide attempts or other forms of suicidal behavior (e.g. aborted or interrupted attempts) (Goldston, 2000).
This report examines the Harkavy-Asnis Suicide Self-Report Scale (HASS-I, hereafter referred to as HASS), one of the few self-report measures which assesses a broad range of suicidal behavior and ideation (Goldston, 2000; Harkavy Friedman & Asnis, 1989). There are other self-report questionnaires that assess suicidal ideation, such as the widely used Suicidal Ideation Questionnaire, Junior (SIQ) (Reynolds & Mazza, 1999), and other measures that assess suicidal ideation and behavior such as the Suicidal Behaviors Questionnaire (SBQ-14) (Linehan, 1981; Osman et al., 2001). However, the HASS was selected for this study because 1) the items tap passive suicidal ideation, more active suicidal ideation, and active suicide behavior including suicide attempts and aborted attempts, and 2) the measure has been found to be sensitive to early effects of a specialized emergency room (ER, now called emergency department, ED) intervention for youths attempting suicide (Rotheram-Borus, Piacentini, Cantwell, Belin, & Song, 2000; Rotheram-Borus et al., 1996). As originally developed by Harkavy-Friedman et al. (1989), the HASS 21-item self report scale was one part of a three-part instrument designed to assess a broad range of suicide risk factors, including demographics, service use, substance abuse, suicidal behavior in family members and others, as well as suicidal ideation and behavior.
To date, there are limited data on the HASS with youths. The original report on scale development and psychometrics (Harkavy Friedman & Asnis, 1989) supported internal consistency in both clinical and nonclinical samples and concurrent validity in high school students with moderate associations observed between HASS scores and measures of depression, aggression, impulsivity, and negative life stress, but not with positive life stress or social desirability (Harkavy Friedman & Asnis, 1989). More recent work has provided additional support for discriminative and concurrent validity (Harkavy Friedman, 2009; Wetzler et al., 1996), and one study found the scale to be sensitive to early intervention effects in a trial evaluating an ED intervention for youths attempting suicide (Rotheram-Borus et al., 1996). No data on test-retest reliability have been identified for youth populations (Goldston, 2000; Harkavy Friedman, 2009; Harkavy Friedman & Asnis, 1989; Wetzler et al., 1996).The HASS has also been used with adults, particularly to assess suicide-risk and suicidal behavior in individuals suffering from schizophrenia, mood disorders, HIV, and/or substance abuse (Cooperman & Simoni, 2005; Harkavy-Friedman, Nelson, Venarde, & Mann, 2004; Harkavy Friedman, 2009).
This study has two primary aims: 1) to evaluate the psychometric adequacy and validity of the HASS scales in youths in an independent sample of high-risk suicidal youths drawn from two sites independent of the original development site, and 2) to move towards a model that clinicians can use for monitoring suicide attempt risk by using classification and regression tree analysis to examine predictors of suicide attempt behavior from the individual HASS items. Classification and regression tree analysis belongs to a family of decision tree methods that translate easily into a set of decision algorithms that could be used for risk stratification and clinical management. This method has been used increasingly to address medical and behavioral health problems (Zhang & Singer, 1999). The study questions are examined using data from 131 patients participating in a randomized controlled trial evaluating an enhanced mental health intervention, as compared to usual care, in pediatric patients (ages 10–18) presenting to the ED with suicidal behavior (Asarnow et al., 2011). To address the study aims, we emphasize cross-sectional data from the first follow-up assessment after discharge from the ED/hospital.
METHODS
We focus here on the HASS measure and procedures relevant to the assessments of suicidal ideation and behavior on both the HASS and Diagnostic Interview Schedule for Children and Adolescents (DISC-IV) (Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000). The study was reviewed by each site’s local IRB. All subjects gave informed assent/consent (as appropriate) and parents gave informed consent. Readers interested in learning more about the randomized controlled trial, are referred to our other manuscripts (Asarnow et al., 2011; Asarnow et al., 2008; Asarnow, Berk, & Baraff, 2009).
Setting & Design
Patients were recruited from two large EDs in Los Angeles County purposely selected to include different geographic areas, populations, and both public and private EDs. ED-A was part of an academic medical center in a largely middle class community, was linked to a psychiatric hospital with youth inpatient services, and served roughly 42,000 patients annually. ED-B, operated by Los Angeles County Department of Health, served roughly 77,000 public-sector patients annually across psychiatric, adult, and pediatric EDs.
Consecutive patients (N=181) were recruited between April 2003 and August 2005. After being informed of the study and eligibility criteria, ED personnel identified possible participants and paged study staff, who verified eligibility and enrolled participants. Inclusion criteria were: presenting to the ED with suicide attempts and/or ideation; age 10 –18 years. Exclusion criteria were: acute psychosis/symptoms that impede consent/assessment; no parent/guardian to consent (youth <18); youth not English-speaking; parents/guardians not English or Spanish-speaking.
After youths and parents completed 20–30 minute baseline questionnaires in the ED (or shortly thereafter), participants were randomly assigned to one of two conditions: the Family Intervention for Suicide Prevention; or ED-treatment as usual. Follow-up assessments were completed at about 2-months after discharge from the ED/hospital (Median = 41 days, Mean = 57 days, SD = 51 days) and asked about the period since the assessment in the ED. These assessments were completed at participants’ homes and supplemented by telephone when needed. Measures were available in Spanish and English for parents. An additional follow-up assessment was conducted at about 3.8 months after the first follow-up assessment (Median = 108 days, Mean = 116 days, SD = 60 days) using the same procedures and measures, and asking about the period since the prior assessment. DISC-IV interviewers were blind to the HASS data. Because the HASS was administered in the follow-up assessments, the analytic sample for this study included only those youths who completed the HASS at a follow-up assessment (N=131). To maintain consistency across measures, the DISC-IV and HASS suicide items were administered using the same time frame: at the first assessment these questions asked about the time period “since your visit to the ER when you were enrolled in the study;” at the second assessment the questions asked about the time period “since the last time you had a study interview.”
Measures
HASS
The Harkavy-Asnis Suicide Scale (HASS) (Harkavy Friedman & Asnis, 1989) was administered to youths at each follow-up assessment. The study version of the HASS included 17 items asking about the frequency of suicidal ideation and behavior on a 5-point Likert scale, with 0 indicating “never” and 4 indicating “most or all of the time” and a total HASS scale range of 0 to 68. The original 21-item HASS included substance abuse items which were excluded in the study scale. In prior research, the HASS suicidality items have been clustered into two subscales: 1) active suicidal behavior and ideation (ASBI, 5 items, e.g. “tried to kill yourself,” “started to do it and then stopped at the last minute”, “talked to someone about killing yourself, besides the people in the clinic or with me”, “had a plan of how you would kill yourself”, “ thought about ways to kill yourself”) and 2) more passive suicidal ideation (Passive SI) 12 items, e.g. “had ideas about killing yourself,” ” thought about killing yourself but did not try to do it”). For the purpose of this study, we also developed a Suicide Attempt subscale (SA) which included 2 items selected from the ASBI scale because they assessed suicide attempt behavior: 1) suicide attempts (“tried to kill yourself”), and 2) aborted suicide attempts (“had a plan to kill yourself, started to do it and then stopped at the last minute”). Recent data indicating that these two items emerged in a factor analysis of data from high school students provides additional support for this SA subscale (Harkavy Friedman, 2009). Because any positive (non-zero) score on these two suicide attempt behavior items is considered significant clinically, we examined dichotomized variables reflecting presence vs. absence of suicide attempt behavior, as well as the overall frequency score for the SA scale (range 0–8). The HASS demonstrated strong internal consistency (coefficient alpha=.897 to .915) in prior research using both clinical and non-clinical samples of adolescents (Harkavy Friedman & Asnis, 1989).
Diagnostic Interview Schedule for Children (DISC-IV)
The NIMH DISC-IV depression module and suicide items were administered at each assessment point. This structured diagnostic interview was administered by interviewers, with the interviewers using a computer assisted format. All interviewers were trained and certified by a member of the DISC development team, and supervised by senior staff. Quality assurance ratings completed on a random subset of 20% of interviews indicated strong interview quality (Mean rating=1.2, SD=0.54, 3-point scale 1=good, 2=fair, 3=poor). The DISC-IV suicidal ideation and attempt items have good test-retest reliability over a 1-week period (kappa=.66–.78) and predictive validity (Goldston, 2000) and the overall DISC-IV interview has shown adequate inter-rater and test-retest reliability (Shaffer et al., 2000). Because all of the youths in this study were identified in the ED due to suicidal ideation or attempts, the time frame for the standard DISC question was modified to ask about the period since discharge from the ED at the first follow-up, and the time since the last study assessment at the second follow-up. The question was: “Now thinking about (time frame), have you tried to kill yourself?”
Statistical Analysis
Standard descriptive statistics were used to describe the sample and distributions of HASS item and scale scores. Some items and scales were strongly positively skewed. When violations of normality were evident, we used Spearman correlation coefficients. To examine the degree to which the individual scale items could predict whether youths endorsed suicide attempt behavior (SA scale), we used a classification tree approach referred to as recursive partitioning. This method has been used increasingly to address medical and behavioral health problems and has advantages over logistic regression or discriminant function analyses when variables are not normally distributed (Zhang & Singer, 1999). Because the approach is not affected by collinearity, multiple variables of similar constructs can be included in the analysis. Another advantage over traditional regression analyses is that recursive partitioning models can identify interactions between variables that best split the sample into more homogeneous subgroups, and therefore, translate easily into a set of decision algorithms that could be used for risk stratification and clinical management.
The recursive partitioning analyses were conducted using the package rpart (Therneau & Atkinson, 2012) in the software environment R (R Development Core Team 2011). This approach uses binary recursive partitioning to identify the most efficient predictors for splitting the sample into progressively smaller high- and low-risk groups using any combination of categorical or continuous variables (Brieman, Friedman, Stone, & Olshen, 1984). In the first split, the so-called “parent node,” the predictor is identified that best discriminates between high and low risk groups within the full sample (in our case youths with and without SA behavior). For each successive split, the process is repeated to generate a series of “child nodes,” identifying the split at each node yielding the greatest improvement in predictive accuracy. “Terminal nodes” are obtained when predictive accuracy cannot be improved with additional splits. Sensitivity analyses examined whether a similar tree would emerge predicting to the single suicide attempt item vs. the 2-item SA scale (attempts and aborted attempts). The stability of HASS scores over a roughly 3–4 month interval was examined using data for 88 youths who completed the HASS at a second follow-up.
RESULTS
The sample ranged from 10–18 years of age with a mean of 14.87 years (SD = 1.89). Youths were predominantly female (74%, n=97/131), and the sample was ethnically diverse: Hispanic 46.6% (n=61/131); Caucasian 32.8% (n=43/131); African-American 11.5% (n=15/131); Asian/Other 9.2% (n=12/131). Past-year suicide attempts were reported by 65% (n=85/131) of youths, with 25% (n=33/131) reporting multiple (≥ 2) past-year attempts. Mental health/functioning problems were common at baseline: 78% (n=102/131) reported severe depression (CES-D ≥ 24) (Radloff, 1977); 53% (n=65/122) screened positive for post-traumatic stress disorder (Prins et al., 2003); 13% (n=17/129) reported probable substance abuse (Glynn et al., 2003); and 54% (n=62/115), 50% (n=57/115), and 60% (n=69/115) of youths scored in the clinical range on the Child Behavior Checklist (CBCL) internalizing, externalizing, and total problems, respectively (Achenbach, 1991). Most youths were hospitalized after ED evaluation/treatment (66%, n=87/131). Based on retrospective assessments completed at follow-up, 40.5%, n=47/116) of youths met DISC-criteria for depressive disorders (major depression or dysthymic disorder) during the year prior to the ED-visit. Please note that missing data resulted in variations in the denominators across measures. Comparisons of the sample of youths with HASS follow-up data (the analytic sample for this study) with the baseline sample without Hass follow-up data, revealed a significant tendency for youths completing the HASS at follow-up to have significantly lower baseline rates of probable substance abuse (13% vs. 28%, X2(1)=5.53, p=.02) and clinically significant externalizing problems on the CBCL (50% vs. 86%, X2(1)=6.56, p=.01). This is somewhat expected, as youths with substance use and severe out of control behavior were often placed out of the home and unavailable for follow-up assessments.
HASS Scales
Table 1 shows the psychometrics for the HASS Scales. The scale scores were positively skewed with a modal score of 0 for all scales. Cronbach’s Alpha ranged from 0.77 to 0.96. These values fall within the good (.70–.89) to high (≥.90) range (Cicchetti, 1994; Clark & Watson, 1995). Item-total correlations (with the Total HASS Scale) exceeded 0.30 for all items and scales, again supporting the internal consistency of the scales. Item-total correlations ranged from 0.58–0.90 for the Total Hass Scale, 0.49–0.92 for Passive SI Scale, 0.65–0.86 on the ASBI scale, and 0.80–0.92 for the SA scale. Both skewness and kurtosis were within the range of +1.5 to −1.5 for the HASS Total Score and Passive SI Score, but were more extreme for the ASBI and SA scales.
Table 1.
Psychometrics on the HASS Scales
| Scale | Items | N | Alpha | Mean | SD | Median | Mode | Range | Skewness | Kurtosis |
|---|---|---|---|---|---|---|---|---|---|---|
| Total HASS | 17 | 128 | 0.96 | 16.03 | 16.57 | 11.0 | 0 | 0–61 | 0.991 (.214) |
0.001 (.425) |
| Passive Suicidal Ideation (SI) | 12 | 128 | 0.95 | 12.79 | 12.71 | 9.0 | 0 | 0–48 | 0.861 (.214) |
−0.319 (.425) |
| Active Suicidal Behavior/Ideation (ASBI) | 5 | 131 | 0.86 | 3.39 | 4.75 | 1.0 | 0 | 0–20 | 1.61 (.212) |
1.98 (.42) |
| Suicide Attempt (SA) | 2 | 131 | 0.77 | 1.05 | 1.96 | 0 | 0 | 0–8 | 2.194 (.212) |
4.421 (.420) |
2 items on the Passive Suicidal Ideation scale had missing data (Item 6 (been in high places and felt like jumping) missing=2); item 9 (felt like running into traffic), missing=1) resulting in N=128 vs. 131 for the Passive SI and Total HASS scales. Possible range: Total HASS 68; SI 48; ASBI 20; SA 8.
Item Distributions
The distribution of all item scores was positively skewed (Table 2). The modal response was 0 for all items; medians ranged from 0 to 1 across items. Reflecting the higher rate of suicidal ideation vs. attempts, all of the items on the SA scale (Q14, 17) had low endorsement rates (median score=0), as did the remaining items on the ASBI scale (Q 7, 10, 16). Skewness and kurtosis were within the range of +1.5 to −1.5 for 12 of the 17 items. The most highly skewed items included the two SA items (Q 14, 17), the suicide plan item (Q10), and 2 items from the Passive SI Scale that listed specific attempt methods (jumping from high places (Q6), running into traffic(Q9)).
Table 2.
Distribution of scores for HASS items and scales.
| Itema | 0 Never f(%) |
1 Rarely f (%) |
Some of the time F (%) |
Frequently f(%) |
Most of time f(%) |
Median | Mean (SD) | Item-Total Correlationb |
|---|---|---|---|---|---|---|---|---|
| 1. thought you would be better off dead? | 50 (38.2%) | 32 (24.2%) |
24 (18.3%) |
14 (10.7%) |
11 (8.4%) |
1 | 1.27 (1.30) |
.862** |
| 2. dreamed about death? | 73 (55.7%) |
24 (18.3%) |
11 (8.4%) |
11 (8.4%) |
12 (9.2%) |
0 | .9695 (1.34701) |
.785** |
| 3. had ideas about killing yourself? | 65 (49.6%) |
33 (25.2%) |
12 (9.2%) |
7 (5.3%) |
14 (10.7%) |
1 | 1.0229 (1.33281) |
.889** |
| 4. thought that the world would be better off without you? | 48 (36.6%) |
30 (22.9%) |
21 (16.0%) |
15 (11.5%) |
17 (13.0%) |
1 | 1.4122 (1.41351) |
.777** |
| 5. thought about death and dying? | 50 (38.2%) |
28 (21.4%) |
21 (16.0%) |
14 (10.7%) |
18 (13.7%) |
1 | 1.4046 (1.43462) |
.897** |
| 6. been in high places and felt like jumping? | 93 (71.0%) |
17 (13.0%) |
8 (6.1%) |
3 (2.3%) |
8 (6.1%) |
0 | .5736 (1.12344) |
.599** |
| 7. thought about ways to kill yourself? | 79 (60.3%) |
17 (13.0%) |
16 (12.2%) |
7 (5.3%) |
12 (9.2%) |
0 | .9008 (1.32929) |
.833** |
| 8. gotten so discouraged that you thought about ending your life? | 65 (49.6%) |
26 (19.8%) |
14 (10.7%) |
11 (8.4%) |
15 (11.5%) |
1 | 1.1221 (1.40342) |
.902** |
| 9. felt like running into traffic? | 92 (70.2%) |
19 (14.5%) |
10 (7.6%) |
5 (3.8%) |
4 (3.1%) |
0 | .5385 (1.00506) |
.694** |
| 10. had a plan of how you would kill yourself? | 90 (68.7%) |
20 (15.3%) |
7 (5.3%) |
8 (6.1%) |
6 (4.6%) |
0 | .6260 (1.12548) |
.762** |
| 11. wished you were dead? | 53 (40.5%) |
26 (19.8%) |
20 (15.3%) |
16 (12.2%) |
16 (12.2%) |
1 | 1.3588 (1.42542) |
.891** |
| 12. felt that life was not worth living? | 50 (38.2%) |
29 (22.1%) |
17 (13.0%) |
16 (12.2%) |
19 (14.5%) |
1 | 1.4275 (1.46251) |
.835** |
| 13. thought about killing yourself but did not try to do it? | 59 (45.0%) |
29 (22.1%) |
13 (9.9%) |
14 (10.7%) |
16 (12.2%) |
1 | 1.2290 (1.42810) |
.648** |
| 14. tried to kill yourself? | 93 (71.0%) |
20 (15.3%) |
5 (3.8%) |
5 (3.8%) |
8 (6.1%) |
0 | .5878 (1.13592) |
.718** |
| 15. dreamed about killing yourself? | 95 (72.5%) |
13 (9.9%) |
8 (6.1%) |
6 (4.6%) |
9 (6.9%) |
0 | .6336 (1.21025) |
.725** |
| 16. talked to someone about killing yourself, besides the people in the clinic or with me? | 79 (60.3%) |
25 (19.1%) |
9 (6.9%) |
9 (6.9%) |
9 (6.9%) |
0 | .8092 (1.24106) |
.632** |
| 17. had a plan to kill yourself, started to do it and then stopped at the last minute? | 102 (77.9%) |
13 (9.9%) |
6 (4.6%) |
4 (3.1%) |
6 (4.6%) |
0 | .4656 (1.03995) |
.582** |
SA Scale:14,17. ASBI Scale: 14, 17, 7, 10, 16. Passive SI Scale: 1,2,3,4,5,6,8,9,11,12,13,15. In this study, time frame and response options were slightly different. Original HASS I asked about past 2 weeks and used 0–4 scale as follows: 0=none; 1=once; 2=1–2 times a week; 3=3–4 times a week; 4=daily
Item-Total reflects correlation with HASS Total Scale (Items1–17).
Suicide Attempt Scale Items
Because of the importance of suicide attempts as a target variable, we examined the association between the two suicide attempt items (suicide attempts,Q14; aborted suicide attempts,Q17). The Spearman correlation using the full 5-point item range for each item was statistically significant, r=.60, p<.001. Because any positive score on these two suicide attempt behavior items is considered significant clinically, we also examined dichotomized variables reflecting presence vs. absence of the behavior. Results indicated a statistically significant association between these two items, X2(1) = 45.76, p<.001, point biserial correlation r=.59, p<.001. Sixty percent (23/38) of youths reporting suicide attempts also reported aborted attempts, and 79% (23/29) of youths making aborted attempts also reported suicide attempts.
Construct Validity
Comparison of youth report on the HASS SA scale (Q 14 & Q 17) and the DISC-IV suicide attempt item indicated strong construct validity. As shown in Table 3, all of the 9 youths reporting suicide attempts on the DISC-IV also reported SA behavior on the HASS, indicating 100% sensitivity/ true positive rate for the HASS SA scale relative to the DISC-IV SA item. Similarly, when the HASS SA score was negative, none of these youths reported SAs on the DISC-IV, resulting in a negative predictive value for the HASS SA scale of 100%. Specificity was lower, however, with 32 youths reporting SA behavior on the HASS but not on the DISC-IV, resulting in a specificity of 69.8%, and an overall accuracy rate of 72.2% (83/115).
Table 3.
Concurrent Validity: Comparison of HASS SB Scores and Youth Reported Suicide Attempts on the DISC
| DISC Suicide Attempt (SA) | TOTAL | ||
|---|---|---|---|
| HASS SA Scale (Q14 & 17) |
No f (%) |
Yes f (%) |
f (%) |
| No | 74 (69.8%) | 0 | 74 (64.3% |
| Yes | 32 (30.2%) | 9 (100%) | 41 (35.7%) |
| TOTAL | 106 (92.2%) | 9 (7.8%) | 115 (100%) |
Fisher’s Exact Test p<.0001
N=115 due to missing data.
As shown in Table 4, which shows the association between youths response to the SA item on the HASS (Q 14) and reports of SAs on the DISC-IV, one youth who reported an SA on the DISC-IV endorsed an aborted but not an actual attempt on the HASS (yes to Q17, no to Q14), resulting in weaker sensitivity (88.9%, 8/9) of the HASS attempt item (Q 14) vs. the SA scale, and similar specificity, 74.5% (79/106), and overall accuracy 75.6% (87/115).
Table 4.
Concurrent Validity: Comparison of HASS SB Scores and Youth Reported Suicide Attempts on the DISC
| DISC Suicide Attempt (SA) | TOTAL | ||
|---|---|---|---|
| HASS SA (Q 14) | No f (%) |
Yes f (%) |
f (%) |
| No | 84 (73.7%) | 1 (11.1%) | 85 (69.1%) |
| Yes | 30 (26.3%) | 8 (88.9%) | 38 (30.9%) |
| TOTAL | 114 (92.7%) | 9 (7.3%) | 123 (100%) |
Fisher’s Exact Test p<.0001
N=123 due to missing data.
Score Stability/Test-Retest Reliability
We examined the stability of scores over an average of 116 days, SD= 60, range= 46 to 435 (Table 5). Results indicate moderate stability. Results were near identical using the full test-retest sample, and when cases were limited to those where time between assessments was ≤ 120 days (Table 5, columns 2 and 3 vs. columns 4 and 5).
Table 5.
Stability Test-Retest Reliability of HASS Scale Scores Across Two Follow-Up Evaluations
| Full Sample (N=88) | Sample Limited to Follow-Up ≤ 120 Days (N=58) |
|||
|---|---|---|---|---|
| Correlation Coefficient |
P value | Correlation Coefficient |
P Value | |
| HASS Total | .46 | .001 | .54 | .001 |
| HASS PI | .53 | .001 | .54 | .001 |
| HASS ASB | .49 | .001 | .49 | .001 |
| HASS SA | .31 | .004 | .32 | .02 |
Spearman correlations were computed for ASBI and SA scales due to skewed distributions. Others were Pearson correlations.
Because of the importance of SA outcomes, we examined rates of any SA behavior (SA Scale) at the first and second assessments. The association was statistically significant, X2 (1)=7.12, p=.008, Kappa =.24, p=.008: 28.1% (9/32) of youths reporting SA behavior at the first assessment reported SA behavior at the second assessment, whereas 7.1% (4/56) of youths reporting no SA behavior at the first assessment reported SA behavior at the second assessment. Consistent with the expectation that SA behavior would decrease after an acute suicidal episode with ED treatment, there were over twice as many youths reporting SA behavior at the first vs. second assessment (36.3%, n= 32/88 vs. 14.8%, n= 13/88).
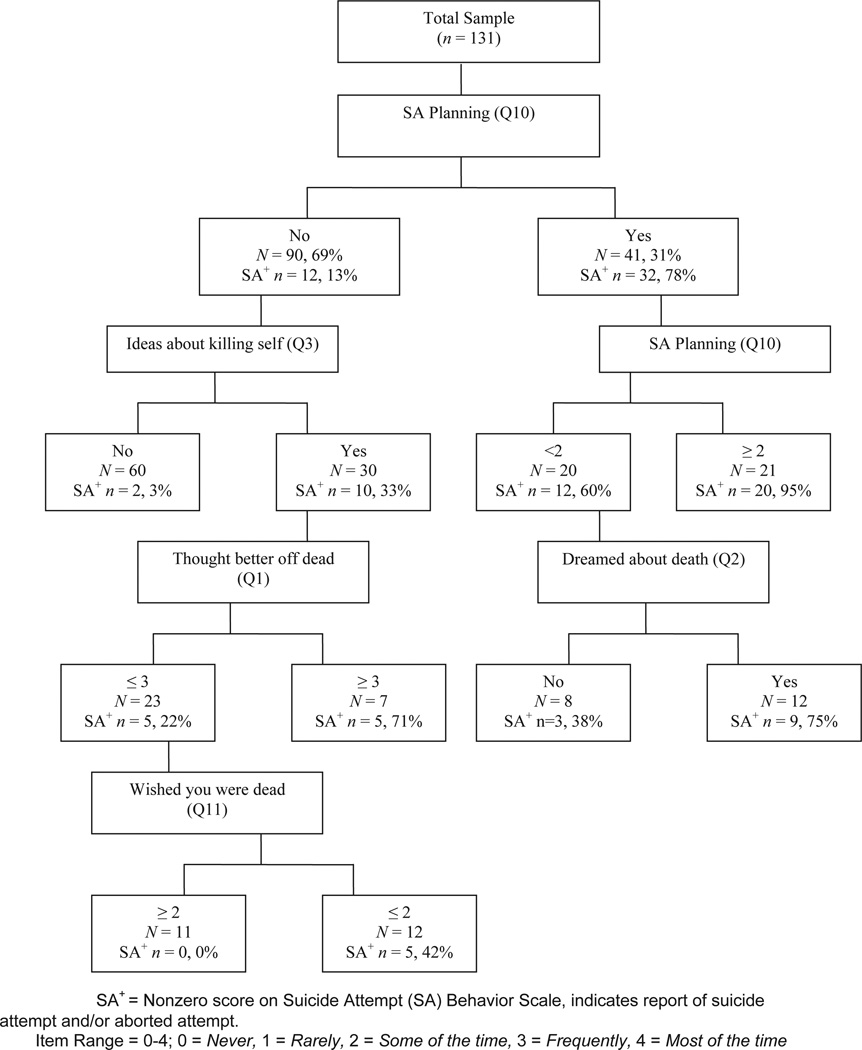
Classification and Regression Tree Analysis: Predicting SA Behavior on HASS
Given our interest in predicting to SA behavior, we conducted regression tree analyses to examine which HASS items best account for the presence vs. absence of reported SA behavior. The model that emerged when all other HASS items were included is shown as Figure 1. This model had 7 nodes, an R2 of 0.61 and an overall correct classification rate of 86.3%. The planning item (Q10) was the first variable to emerge in the classification tree, with an R2 of .40 at this split and a total correct classification rate of 84% based only on the planning item. Whereas the probability of SA behavior was p=.78 (32/41) for youths endorsing SA planning, the probability of SA behavior was p=.13 (12/90) among youths reporting no SA planning. If youths endorsed planning SAs more frequently (at least “some of the time” vs. “rarely” or “never”), the probability of SA behavior was .95 (20/21). Among youths reporting less frequent SA planning (“rarely”), those who endorsed dreams of death (Q2) were more likely to report SA behavior, p=.75 (9/12), while SA behavior was less common among those not reporting dreams of death, p=.375 (3/8).
Figure 1.
Classification Tree Predicting Suicide Attempt Behavior.
In contrast, among youths with no endorsed SA planning, those who also reported no ideas of killing themselves (Q3), reported very low rates of SA behavior, p=.03 (2/60). Similarly, youths who reported no SA planning but endorsed some suicidal ideation (Q3) had very low rates of SA behavior if they also had low scores on Q1 (thought you would be better off dead), p=.22 (5/23). Rates of SA behavior were higher, p=.71 (5/7) among youths reporting no SA planning (Q10) if they reported some suicidal thoughts (Q3) and reported thinking they would be better off dead (Q1) “frequently or most of the time”, p=.71 (5/7). Among youths with no planning, some suicidal ideation, and lower Q1 scores (thought better off dead), rates of SA behavior were higher among youths who endorsed low scores on Q11 (wished you were dead), p=.42 (5/12).
We also conducted a sensitivity analysis predicting to suicide attempts (Q14), excluding Q17 (aborted attempts) from the outcome measure. The goal of this analysis was to examine whether the same variables would emerge as predictors, particularly the planning item. All other aspects of the analysis were the same as those in the primary analysis. Results for this tree were similar to those for the SA scale, with planning emerging at the first split (although the split occurred at a higher point in the scale). Three items were common to both trees (Q10, Q3, Q2). The tree predicting to suicide attempts had 6 nodes, an R2 of 0.60, and an 86.3% correct classification rate. After the first split (Q10), items associated with increased likelihood of an SA (Q14) included two suicidal ideation items (Q3, Q7) dreams of death (Q2), and Q16 (talked to someone about killing yourself).
DISCUSSION
The present results support the validity and psychometric adequacy of the HASS for youths with histories of high levels of suicidality. This is a particularly important group for clinical monitoring given their high risk of repeat suicidal behavior. Indeed, 78.6% of our sample of youths evaluated in the ED for suicidality continued to report some suicidal ideation or behavior during the roughly 2-month follow-up period and 33.6% reported suicide attempts or aborted attempts. These data underscore the critical need for systematic evidence-based assessment and monitoring of youth suicidality in high-risk populations.
Consistent with data on the greater sensitivity of self-report versus clinician administered measures when assessing sensitive behaviors, the rate of reported attempts was substantially higher with the HASS as compared to the interviewer-administered DISC-IV. Clinically, this is of critical importance because reporting of suicidal behavior may be particularly sensitive, with youths reluctant to report suicidality given the high likelihood of psychiatric hospitalization and youths’ frequent concerns about being hospitalized (Asarnow et al., 2011; Cohen, Asarnow, Taylor, Do, & Gragossian, 2010). The SA scale developed in this study showed high sensitivity, detecting all of the youths reporting SAs on the DISC-IV. Therefore, the HASS SA scale would appear to be a feasible and effective screener for suicide attempt behavior. Although the HASS SA scale also identified youths who screened negative on the DISC-IV, given the potentially fatal consequences of failure to detect youths exhibiting suicide attempt behavior, sensitivity (accurate detection of youths with attempt behavior) is more critical in this context than specificity (reducing the number of youths being misidentified as “positive”).
The other major objective of this study was to use classification and regression tree analyses to examine predictors of suicide attempt behavior with the ultimate goal of moving towards an algorithm for clinical monitoring and risk stratification. Development of an evidence-based algorithm for risk assessment and monitoring is critical for increasing efficiency and optimizing our ability to identify and triage youths with elevated risk for more intensive evaluation and treatment. This is particularly important given evidence of increasing numbers of youths seeking treatments in settings such as emergency departments (EDs) where risk assessment and triage are key components of care and EDs and hospitals are striving for compliance with Joint Commission safety goals to routinely assess and reduce suicide risk (The Joint Commission, 2011). The present results underscore the significance of planning as a predictor of SAs, with a split based on the presence or absence of SA planning correctly identifying 84% of youths with suicide attempt behavior (R2=.40). The addition of information on frequency of planning, suicidal ideation, and thoughts of death resulted in an overall R2 of .61 with 86.3% of youths with SA behavior correctly identified. These data supporting the clinical significance of attempt planning are consistent with the observation that attempt planning implies some intent to die, and research indicating that high suicide intent is associated with higher lethality among older youths and adults who have accurate expectations of likelihood of death based on attempt methods (Brent, Baugher, Bridge, Chen, & Chiappetta, 1999; Brown, Henriques, Sosdjan, & Beck, 2004).
Our data underscore the value of self-report measures, such as the HASS, as screening and assessment tools for monitoring youth suicidal behavior, and also highlight the importance of additional evaluation after screening to ensure that the clinical response is appropriate to the level of risk. Indeed, the enhanced mental health intervention evaluated in the randomized controlled trial (Asarnow et al., 2011) was originally designed as a behavioral assessment of “imminent risk,” based on behavioral characteristics that are incompatible with suicidal behavior (Rotheram-Borus & Bradley, 1991; Rotheram-Borus et al., 2000; Rotheram-Borus et al., 1996). Using this approach, youths are viewed as lower risk if they are able to work with the therapist to complete the following brief behavioral tasks: 1) to identify and share three positive self-characteristics, 2) to use a “feeling thermometer” to identify triggers for suicidal acts and discriminate varying levels of emotional distress (subjective units of distress) and feeling states, 3) to make a concrete safety plan for dealing with suicidal feelings and suicide-triggering situations, 4) to identify three persons who they could go to for social support at times of distress/risk, and 5) to commit to using the safety plan vs. suicidal behavior in the future and to attend outpatient treatment after discharge. A triage model based on this approach was used successfully to screen runaway and homeless youths for suicide risk, with youths who were unable to complete these tasks triaged to emergency/immediate psychiatric evaluation and those who were able to complete the tasks triaged to outpatient care (Rotheram-Borus & Bradley, 1991). Results indicated that the number of suicide attempts was decreased after implementation of the triage program. Further, whereas screening on statistically based risk factors would have yielded over 80% screener positive youths in this homeless population with multiple problem behaviors, the “imminent risk screening” enhanced feasibility by identifying a smaller number of screener positive youths with elevated risk specifically for suicidal behavior (Rotheram-Borus, 2006). It may be that broad screening using a self-report scale such as the HASS with a high level of sensitivity, followed by additional evaluation and behavioral assessment of imminent risk, may similarly yield an effective approach for ED screening, risk assessment, triage, and linkage to mental health services.
It is important to consider study limitations. Our sample was selected for high risk for suicidal behavior because of the importance of monitoring such high-risk youths. However, results may not generalize to other samples, particularly those with lower risk levels. The classification and regression tree analyses require replication as trees can be unstable because any change in upper levels of the tree is propagated down the tree to affect other splits. Although this report focuses on a self-report measure of suicidal behavior and ideation, assessment and management of suicide risk clearly requires a comprehensive evaluation and monitoring strategy which integrates information from multiple informants, measures, a broad range of risk and protective factors, and then triages youths to optimal intervention strategies. Our analyses focused on classification of SA risk based on cross-sectional information, different patterns may emerge when examining longitudinal prediction or combining a more diverse set of predictor variables. Despite the fact that this is one of the largest clinical samples to date of pediatric suicidal ED patients and the sample was drawn from two diverse EDs that varied in patient population and location, results may not generalize across other ED patient populations. The study sample also included a subset of the baseline sample, for whom HASS self-report data were available, resulting in exclusion of more out of control youths with substance use problems who were in placements out of the home. The DISC is a highly structured interview administered using a computer assisted format by a trained interviewer. Results might have differed had we used a clinical interview or semi-structured interview such as the Schedule for Affective Disorders and Schizophrenia for School-Age Children- Present and Lifetime (K-SADS-PL) (Kaufman et al., 1997). Finally, because we were interested in evaluating intervention effects in the overall study, we modified the time frame of the HASS to ask about the period since ED/hospital discharge. This may have made our dichotomous scoring system for the SA scale (presence vs. absence of SA behavior) most appropriate. As originally developed, the HASS-I asked about the past 2 weeks, and the HASS-II used the same questions to ask about “your whole life, except for the past 2 weeks,” the response options were also slightly different. Further research is needed to clarify how adjustments to time frame and response options like those made in this study may influence results.
In conclusion, there is broad recognition of the urgent need for enhanced evaluation and clinical management strategies for suicidal youths, particularly those with histories of suicidal behavior who as a group have elevated risk for suicide attempts and death by suicide (Spirito & Esposito-Smythers, 2006). Our findings support the value of self-report measures, and the HASS specifically, as a risk evaluation and monitoring tool for youth suicidality. Moreover, our results support the significance of planning behavior, suggesting that planning will be an important variable to consider in the development of risk stratification and management guidelines. Future work is needed to expand this work and develop a comprehensive approach for screening, triage, and linkage to optimal interventions.
Acknowledgments
This work was supported by grant CCR921708 from the Centers for Disease Control and Prevention. Additional support for data analysis was provided by grant R01 MH078082 from the National Institute of Mental Health. We thank the youths, families, staff, and colleagues who made this project possible. Additionally, we thank Donald Guthrie PhD, Gabrielle Carlson MD, and Lisa Jaycox PhD for serving on our Data Safety and Management Board. The HASS is in the public domain and can be obtained from: Jill Harkavy-Friedman, PhD, 205 West 89th Street, 1G, New York, NY 10024, JillHFPhDverizon.net.
REFERENCES
- Achenbach TM. Manual for the child behavior checklist / 4–18 and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Asarnow JR, Baraff LJ, Berk M, Grob C, Devich-Navarro M, Suddath R, et al. Effects of an emergency department mental health intervention for linking pediatric suicidal patients to follow-up mental health treatment: A randomized controlled trial. Psychiatric Services. 2011;62(11):1303–1309. doi: 10.1176/appi.ps.62.11.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow JR, Baraff LJ, Berk M, Grob C, Devich-Navarro M, Suddath R, et al. Pediatric emergency department suicidal patients: Two-site evaluation of suicide ideators, single attempters, and repeat attempters. J Am Acad Child Adolesc Psychiatry. 2008;47(8):958–966. doi: 10.1097/CHI.0b013e3181799ee8. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Berk M, Baraff LJ. Family Intervention for Suicide Prevention: A specialized emergency department intervention for suicidal youth. Professional Psychology: Research & Practice. 2009;40(2):118–125. [Google Scholar]
- Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L. Age- and sex-related risk factors for adolescent suicide. J Am Acad Child Adolesc Psychiatry. 1999;38(12):1497–1505. doi: 10.1097/00004583-199912000-00010. [DOI] [PubMed] [Google Scholar]
- Brent DA, Greenhill LL, Compton S, Emslie G, Wells K, Walkup JT, et al. The Treatment of Adolescent Suicide Attempters study (TASA): Predictors of suicidal events in an open treatment trial. J Am Acad Child Adolesc Psychiatry. 2009;48(10):987–996. doi: 10.1097/CHI.0b013e3181b5dbe4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brieman L, Friedman J, Stone CJ, Olshen RA. Classification and regression trees. Chapman and Hall; 1984. [Google Scholar]
- Brown GK, Henriques GR, Sosdjan D, Beck AT. Suicide intent and accurate expectations of lethality: Predictors of medical lethality of suicide attempts. J Consult Clin Psychol. 2004;72(6):1170–1174. doi: 10.1037/0022-006X.72.6.1170. [DOI] [PubMed] [Google Scholar]
- Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment. 1994;6:284–290. [Google Scholar]
- Clark LA, Watson D. Constructing validity: Basic issues in objective scale development. Psychological Assessment. 1995;7:309–319. doi: 10.1037/pas0000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen DR, Asarnow JR, Taylor H, Do MT, Gragossian A. Treatment for suicide attempts in adolescents: Youth and family perspectives; Paper presented at the annual meetings of the American Psychological Association; 2010. [Google Scholar]
- Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS, et al. Grand challenges in global mental health. Nature. 2011;475(7354):27–30. doi: 10.1038/475027a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor J, Rueter M. Predicting adolescent suicidality: Comparing multiple informants and assessment techniques. J Adolesc. 2009;32(3):619–631. doi: 10.1016/j.adolescence.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooperman NA, Simoni JM. Suicidal ideation and attempted suicide among women living with HIV/AIDS. J Behav Med. 2005;28(2):149–156. doi: 10.1007/s10865-005-3664-3. [DOI] [PubMed] [Google Scholar]
- Glynn SM, Asarnow JR, Asarnow R, Shetty V, Elliot-Brown K, Black E, et al. The development of acute post-traumatic stress disorder after orofacial injury: A prospective study in a large urban hospital. J Oral Maxillofac Surg. 2003;61(7):785–792. doi: 10.1016/s0278-2391(03)00239-8. [DOI] [PubMed] [Google Scholar]
- Goldston D. Assessment of suicidal behaviors and risk among children and adolescents: Technical report submitted to NIMH under Contract No. 263-MD-009995. 2000
- Harkavy-Friedman JM, Nelson EA, Venarde DF, Mann JJ. Suicidal behavior in schizophrenia and schizoaffective disorder: examining the role of depression. Suicide Life Threat Behav. 2004;34(1):66–76. doi: 10.1521/suli.34.1.66.27770. [DOI] [PubMed] [Google Scholar]
- Harkavy Friedman J. Assessing suicidal behavior in schizophrenia: Psychometric properties of a brief self-report measure (Abstract) Schizophrenia Bulletin. 2009;35(8) Suppl.1 [Google Scholar]
- Harkavy Friedman JM, Asnis GM. Assessment of suicidal behavior: A new instrument. Psychiatric Annals. 1989;19(7):382–387. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kochanek KD, Xu J, Murphy SL, Murphy BS, Minino AM, Kung HC. Deaths: Preliminary Data for 2009. Vol. 59. National Vital Statistics Reports; 2011. [PubMed] [Google Scholar]
- Linehan MM. Suicidal Behavior Questionnaire. Seattle: University of Washington; 1981. Unpublished manuscript. [Google Scholar]
- Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): Validation with clinical and nonclinical samples. Assessment. 2001;8(4):443–454. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia-Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168(12):1266–1277. doi: 10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Ouimette P, Kimerling R, Camerond RP, Hugelshofer DS, Shaw-Hegwer J, et al. The primary care PTSD screen (PC–PTSD): Development and operating characteristics. Primary Care Psychiatry. 2003;9(1):9–14. [Google Scholar]
- Prinstein MJ, Nock MK, Simon V, Aikins JW, Cheah CS, Spirito A. Longitudinal trajectories and predictors of adolescent suicidal ideation and attempts following inpatient hospitalization. J Consult Clin Psychol. 2008;76(1):92–103. doi: 10.1037/0022-006X.76.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prinstein MJ, Nock MK, Spirito A, Grapentine WL. Multimethod assessment of suicidality in adolescent psychiatric inpatients: Preliminary results. J Am Acad Child Adolesc Psychiatry. 2001;40(9):1053–1061. doi: 10.1097/00004583-200109000-00014. [DOI] [PubMed] [Google Scholar]
- R Development Core Team. R: A language and environment for statistical computing. 2011 (Publication., from R Foundation for Statistical Computing http://www.R-project.org/ [Google Scholar]
- Radloff LS. The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reynolds WM, Mazza JJ. Assessment of suicidal ideation in inner-city children and young adolescents: Reliability and validity of the Suicidal Ideation Questionnaire-JR. School Psychology Review. 1999;28(1):17–30. [Google Scholar]
- Rotheram-Borus MJ. Screening for suicide risk. Am J Public Health. 2006;96(8):1339–1340. doi: 10.2105/AJPH.2006.090597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Bradley J. Triage model for suicidal runaways. Am J Orthopsychiatry. 1991;61(1):122–127. doi: 10.1037/h0079228. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Piacentini J, Cantwell C, Belin TR, Song J. The 18-month impact of an emergency room intervention for adolescent female suicide attempters. J Consult Clin Psychol. 2000;68(6):1081–1093. doi: 10.1037//0022-006x.68.6.1081. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Piacentini J, Van Rossem R, Graae F, Cantwell C, Castro-Blanco D, et al. Enhancing treatment adherence with a specialized emergency room program for adolescent suicide attempters. J Am Acad Child Adolesc Psychiatry. 1996;35(5):654–663. doi: 10.1097/00004583-199605000-00021. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Spirito A, Esposito-Smythers C. Attempted and completed suicide in adolescence. Annu Rev Clin Psychol. 2006;2:237–266. doi: 10.1146/annurev.clinpsy.2.022305.095323. [DOI] [PubMed] [Google Scholar]
- The Joint Commission. National Patient Safety Goals. 2011 Retrieved. from http://www.jointcommission.org/assets/1/6/NPSG_EPs_Scoring_HAP_20110706.pdf. [Google Scholar]
- Therneau TM, Atkinson B. rpart: Recursive Partitioning. R package (3.1-50 ed.) 2012 [Google Scholar]
- U.S. Department of Health and Human Services. [Retrieved Jan 4, 2012];National strategy for suicide prevention. 2001 from http://www.sprc.org/library/nssp.pdf. [Google Scholar]
- Wetzler S, Asnis GM, Hyman RB, Virtue C, Zimmerman J, Rathus JH. Characteristics of suicidality among adolescents. Suicide Life Threat Behav. 1996;26(1):37–45. [PubMed] [Google Scholar]
- Zhang H, Singer B. Recursive partitioning in the health sciences. New York: Springer-Verlag; 1999. [Google Scholar]