Abstract
A proper regulation of the innate immune response is fundamental to keep the immune system in check and avoid a chronic status of inflammation. As they act as negative modulators of TLR signaling pathways, miRNAs have been recently involved in the control of the inflammatory response. However, their role in the context of endotoxin tolerance is just beginning to be explored. We here show that miR-146b is upregulated in human monocytes tolerized by LPS, IL-10, or TGFβ priming and demonstrate that its transcription is driven by STAT3 and RUNX3, key factors downstream of IL-10 and TGFβ signaling. Our study also found that IFNγ, known to revert LPS tolerant state, inhibits miR-146b expression. Finally, we provide evidence that miR-146b levels have a profound effect on the tolerant state, thus candidating miR-146b as a molecular mediator of endotoxin tolerance.
1. Introduction
Deregulation of the inflammatory response contributes to tissue damage in several pathological conditions, including autoimmune and infectious diseases [1–3]. To balance inflammation, the innate immune system has developed a regulatory mechanism by which innate immune cells, monocytes, and macrophages in particular display reduced response to subsequent challenges after they have been exposed to low concentrations of endotoxin (e.g., LPS) [4, 5], entering in a so-called “tolerant” state. Although endotoxin tolerance has been considered as a protective mechanism to regulate overexuberant inflammation, the incidence of endotoxin tolerance has been associated with high risk of secondary infections and an endotoxin-tolerant state is considered to be a clinical phenomenon observed not only in sepsis [6, 7] but also in diseases like acute coronary syndrome [8] and cystic fibrosis [9, 10], and in these pathologies the risk of new infections correlates with a refractory state of innate immune cells.
Much of our knowledge on the molecular mechanisms responsible for endotoxin tolerance arises from in vitro studies, where monocytes primed with low doses of LPS or with IL-10 or TGFβ become tolerant to a subsequent LPS challenging and strongly reduce their production of TNFα and other proinflammatory cytokines [11]. IFNγ represents a key negative regulator of LPS tolerance, being able to revert tolerance and restore TNFα production both in in vitro and in vivo models [12]. The molecular basis of endotoxin tolerance has not been completely elucidated, but it is now clear that it is a dynamic process implying a profound gene reprogramming [13, 14]. In particular extensive studies demonstrated the impairment of the Toll-like receptor (TLR) signaling pathway at multiple levels, with the consequent repression of proinflammatory mediators (i.e., TNFα, IL-6, and IL-12), and the concomitant upregulation of anti-inflammatory molecules, such as IL-10 and TGFβ [15]. Functionally, tolerant monocytes also exhibit increased phagocytosis due to increased expression of CD64 and impaired antigen presentation ability due to the downregulation of major histocompatibility class II (MHC II), CD86, and class II transactivator (CIITA) [9, 16, 17].
A growing number of miRNAs have been reported to be involved in the regulation of the inflammatory response [18–27], but only recently studies described the differential expression and effects of miRNA in the context of endotoxin tolerance [28, 29]. MiR-146a was the first miRNA described as upregulated in tolerant THP-1 monocytic cells after priming with low dose of LPS and was shown to partially induce LPS desensitization in monocytes [28, 29]. Evidence suggesting a possible role of miR-155 and miR-125b in tolerance has also been reported [30]. It is still unclear to which degree each miRNA contributes to the development of endotoxin tolerance, but of note all these miRNAs have been shown to modulate TLR4 signaling pathway by targeting different components of its signaling cascade [31]. In the present study we show the involvement of miR-146b in the induction of endotoxin tolerance by showing its upregulation in LPS tolerant monocytes, its induction by the anti-inflammatory stimuli IL-10 and TGFβ, and its negative regulation by IFNγ. We also demonstrate that tuning miR-146b expression results in the induction or reversion of endotoxin tolerance in the THP-1 monocytic cell line.
2. Materials and Methods
2.1. Reagents
LPS was from E. coli (serotype 055:B5). IL-10, IL-4, IL-13, and TGFβ were from R&D system; IFNγ was from Peprotech; dexamethasone was from Sigma Aldrich. Antibodies anti-Pol II (N-20), anti-RUNX3 (H-50), and anti-STAT3 (C-20) for ChIP experiments were purchased from Santa Cruz Biotechnology and anti-Ago2 was purchased from Abcam.
2.2. Cell Purification and Culture
Human monocytes were obtained from healthy donor buffy coats by two-step gradient centrifugation using Ficoll (Biochrom) and Percoll (Amersham) followed by incubation of purified cells in RPMI 1640 (Lonza) without serum for 10 min at 37°C with 5% CO2. Adherent monocytes were washed twice with PBS and then cultured with RPMI medium supplemented with 10% FBS and L-glutamine as fully described below. The purity of the monocytes cultures was tested by CD14 staining and flow cytometry analysis, with an average of 90% CD14+ cells.
Monocytes and THP-1 cells (ATCC) were grown in RPMI supplemented with 10% heat-inactivated fetal bovine serum (FBS; Lonza), 100 U/mL penicillin/streptomycin (Lonza), and 25 mM L-glutamine (Lonza) at 37°C with 5% CO2. HEK-293T cells (ATCC) were grown in D-MEM (Cambrex) supplemented with 10% FBS, 100 U/mL penicillin/streptomycin, and 25 mM L-glutamine at 37°C with 5% CO2.
2.3. Chromatin Immunoprecipitation (ChIP) Assay
ChIP experiments were performed as described elsewhere [32]. 107 human purified monocytes were culture and extracted DNA was used to perform qPCR using promoter-specific primers [21]. 1% of starting chromatin was used as input. Signals obtained from the ChIP samples were normalized on those obtained from the corresponding input samples, according to the formula: 100 × 2∧(input Ct − sample Ct). Results were expressed as fold enrichment relative to untreated cells.
2.4. Quantification of miR-146b Expression
Total RNA was purified using TRIzol Reagent (Ambion) and extracted with “Directzol RNA miniprep” kit (Zymo Research). Q-PCR was conducted using a 7900HT Real-time PCR System. 100 ng of total RNA was reverse transcribed for quantification of miR expression using TaqMan MiRNA Reverse Transcription kit (Applied Biosystems), according to manufacturer's instructions and as previously described [20, 21]. MiRNA expression values were calculated according to the comparative threshold cycle method, using the ubiquitous small nucleolar RNA U6 as endogenous reference.
2.5. Construct Generation
To overexpress miR-146b in THP-1 monocytic cells a lentiviral-based system was used, as described elsewhere [21] Briefly, the miR/lentiviral-based expression vector pRRL-miR-146b was generated by cloning in the pRRLSIN.cPPT.PGK-GFP.WPRE vector (plasmid #12252; Addgene) a 500 bp region encompassing the pre-miR-146b. The lentiviral construct pRRL-ct, encoding for a hairpin yielding a 22-mer RNA with no homology to any human gene, was used as mock construct. THP-1 cells were transduced with pRRL-146b or pRRL-ct vectors and pRRL-146b THP-1 GFP+ cells and pRRL-ct THP1 GFP+ cells were sorted by FACS with a 90–95% of purity. To knockdown miR-146b-5p expression, THP-1 cells were transduced with the miRzip lentivector-based construct anti-miR-146b and the relative control (System Biosciences) [21]. Transduced GFP+miRT-146b and GFP+miRT-ct THP-1 cells were sorted by FACS with over a 95% of purity.
2.6. Immunoprecipitation of Ago2-Bound RNAs
Immunoprecipitation of Ago2-bound RNAs (RIP) was performed as previously described [21]. 30 × 106 stimulated monocytes were used and results were expressed as fold enrichment relative to unstimulated samples.
2.7. ELISA Assay
All antibodies and detection reagents were purchased from R&D Systems. The ELISA was carried out according to the manufacturer's instructions. Samples were diluted so that the optical density fell within the optimal portion of a log standard curve.
2.8. LPS Desensitization and Reversal
MiRT-ct and miRT-146b-5p THP1 cells were cultured in 24-well plates in 500 μL RPMI supplemented with 10% FBS and 1% L-glutamine, incubated or not for 18 h with 50 ng/mL TGFβ or 20 ng/mL IL-10, followed by LPS stimulation with 0.1 ng/mL or 20 ng/mL LPS. Cells were then washed twice and challenged with 10 ng/mL LPS. Supernatants were collected 24 h after stimulation.
2.9. Statistical Analysis
Statistical evaluation was determined using either Student t-test or one-way ANOVA and p values are reported in figures (∗ p < 0.05; ∗∗ p < 0.01).
3. Results
3.1. MiR-146b Expression Is Induced by IL-10 and TGFβ in Human Primary Monocytes
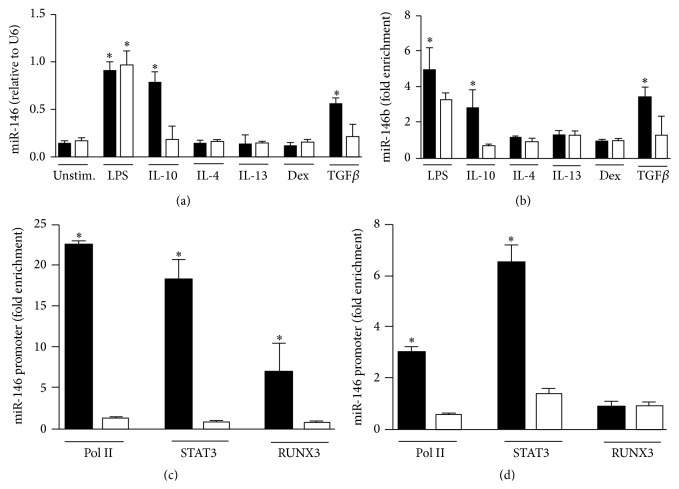
The miR-146 family is composed by miR-146a and miR-146b, both of which are induced during the inflammatory response and target different component of TLR signaling pathway, thus acting as anti-inflammatory regulators [18, 21, 33]. In previous studies we reported that LPS induced the expression of both miR-146a and miR-146b in human monocytes [20] and demonstrated that miR-146b but not miR-146a induction was dependent on the endogenous production of IL-10 subsequent to LPS exposure [21]. We here investigated the regulation of miR-146b and miR-146a by anti-inflammatory mediators known to negatively modulate the activation of monocyte/macrophages. We found that, in addition to IL-10, TGFβ was able to specifically increase the expression of miR-146b but not miR-146a. Glucocorticoids (Dex), IL-4, and IL-13 did not affect miR-146b and miR-146a expression levels (Figure 1(a)).
Figure 1.
MiR-146b is induced in human monocytes by TGFβ signaling pathway. Human purified monocytes were stimulated for 24 h with 100 ng/mL LPS, 20 ng/mL IL-10, 20 ng/mL IL-4, 20 ng/mL IL-13, 20 ng/mL Dex, or 50 ng/mL TGFβ and (a) miR-146b (black columns) and miR-146a (white columns) levels from total RNA were measured by qPCR in triplicate samples. (b) Cell extracts were subjected to RIP assay using anti-Ago2 or IgG control Abs and levels of miR-146b (black columns) and miR-146a (white columns) were measured by qPCR in triplicate samples. Results are expressed as fold change over control (mean ± SEM, n = 3). (c-d) ChIP assays were carried out on human purified monocytes stimulated or not for 4 h with 50 ng/mL TGFβ (c) or 20 ng/mL IL-10 (d) using anti-Pol II, anti-STAT3, or anti-RUNX3 antibodies. Q-PCR was carried out using specific primers for miR-146b (black columns) or miR-146a (white columns) promoters. Results are expressed as fold change over control (mean ± SEM, n = 3).
To investigate the functional activity of miR-146b we evaluated its presence into the Ago2-RISC complex and consistent with the expression data we found an enrichment of miR-146b only when monocytes were treated with LPS, IL-10, or TGFβ (Figure 1(b)). As a control, we measured the relative enrichment of miR-146a and consistent with previous data [21] we detected miR-146a in Ago2-RISC complex only when monocytes were stimulated with LPS (Figure 1(b)).
To elucidate the transcriptional regulation of miR-146b, the cis-regulatory elements in the miR-146b promoter region were characterized. Monocytes exposed to TGFβ or IL-10 showed an enrichment of Pol II onto the miR-146b promoter but not on miR-146a promoter (Figures 1(c) and 1(d)). Bioinformatic analysis performed on the 1 kbp promoter region of miR-146b showed the presence of two consensus sites for STAT3 and one for RUNX3. Since we previously demonstrated the binding of STAT3 to miR-146b promoter in IL-10 stimulated monocytes [21] (Figure 1(d)) we thought to determine whether STAT3 is also recruited to the miR-146b promoter region upon monocytes TGFβ stimulation. We found that recruitment of STAT3 is specific to miR-146b but not to miR-146a promoter (Figure 1(c)). Interestingly, STAT3 has been reported to cooperate with RUNX3 [34], which is also directly induced by TGFβ signaling pathway [35]. Given the proximity of the STAT3 and RUNX3 consensus sites on the miR-146b promoter region, we performed ChIP experiments and found the specific recruitment of RUNX3 transcription factor to the miR-146b promoter region only in monocytes challenged with TGFβ (Figures 1(c) and 1(d)). Taken together, these data identify miR-146b as an IL-10- and TGFβ-responsive gene, whose expression in monocytes is specifically driven by STAT3 in response to IL-10 and by STAT3 and RUNX3 in response to TGFβ.
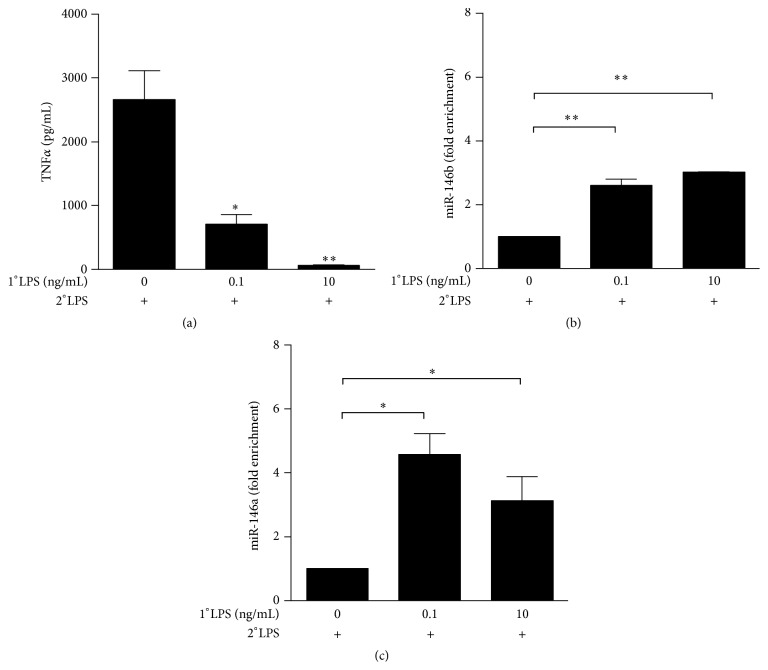
3.2. miR-146b Is Induced in Endotoxin Tolerized Human Monocytes
Since miR-146a was shown to be involved in LPS tolerance [28, 29] and we previously demonstrated that miR-146b is a negative regulator of TLR signaling [21], we investigated the role of miR-146b in the induction of LPS tolerance. We found TNFα strongly downregulated in in vitro tolerized monocytes (Figure 2(a)), in agreement with previous reports [36]. Interestingly, the decrease of TNFα levels was proportional to the dose of LPS used to prime cells: its expression was dramatically impaired in monocytes primed with 0.1 ng/mL LPS and completely abolished with 10 ng/mL LPS (Figure 2(a)). Next we analyzed miR-146b expression levels in tolerized monocytes, using miR-146a as positive control [28]. Strikingly, both miR-146b and miR-146a showed significant higher expression in tolerized monocytes compared to untolerized control cells (Figures 2(b) and 2(c), resp.), thus suggesting miR-146b putative role in LPS tolerance.
Figure 2.
miR-146b and miR-146a are induced in endotoxin tolerized monocytes. Monocytes were first primed with 0, 0.1, or 10 ng/mL LPS (1°LPS) for 18 h and then challenged for 24 h with 10 ng/mL LPS (2°LPS). After 24 h stimulation, TNFα levels (a) were measured by ELISA in cell-free supernatants, and levels of (b) miR-146b and (c) miR-146a were assayed by qPCR in triplicate samples, normalized relative to U6, and expressed as fold enrichment as compared to unstimulated samples. Results are expressed as mean ± SEM of three independent experiments.
3.3. IL-10 and TGFβ Priming Induced Tolerance in Human Monocytes and LPS Responsiveness Can Be Restored by IFNγ Pretreatment
IL-10 and TGFβ act as feedback inhibitors of the LPS-mediated inflammatory response and are part of a more complex network of regulation in which IFNγ operates an opposite function working as a coactivator of the inflammatory pathway triggered by LPS [37]. It has also been reported that IFNγ is able to revert LPS tolerance both in human [11, 38] and murine [39, 40] phagocytes. Accordingly, in human monocytes IFNγ pretreatment strongly enhanced LPS-dependent induction of TNFα and significantly impaired LPS-dependent tolerization effect (Figure 3(e)). Interestingly, IFNγ was able to inhibit the LPS-dependent induction of miR-146b when monocytes were challenged with both LPS and IFNγ (Figure 3(a)), whereas it did not affect the expression of miR-146a (Figure 3(b)). Moreover, pretreatment with IFNγ completely abolished the increased expression of miR-146b observed in LPS-tolerized monocytes, but it had no effect on the overexpression of miR-146a observed in tolerized monocytes (Figures 3(c) and 3(d), resp.).
Figure 3.
IFNγ inhibits the upregulation of miR-146b in tolerized monocytes. (a and b) Monocytes were cultured for the indicated times with 100 ng/mL LPS (circle), 20 ng/mL IFNγ (square), or both stimuli (triangle). (a) MiR-146b and (b) miR-146a were quantified by qPCR. (c to e) Human purified monocytes pretreated or not with 10 ng/mL IFNγ, primed with 0.1 ng/mL LPS (1°LPS) for 18 h, and then challenged with 10 ng/mL LPS (2°LPS). After 24 h stimulation levels of (c) miR-146b and (d) miR-146a were assayed by qPCR in triplicate samples, normalized relative to U6, and expressed as fold enrichment as compared to unstimulated samples. (e) TNFα levels were measured by ELISA in cell-free supernatants. Results are expressed as mean ± SEM of three independent experiments.
Opposite to IFNγ, the anti-inflammatory cytokines IL-10 and TGFβ support LPS desensitization and have been experimentally used to induce hyporesponsiveness to LPS [11]. Both stimuli decreased the expression of TNFα induced by a following stimulation with LPS. IFNγ pretreatment, which strongly enhanced LPS-dependent induction of inflammatory cytokines, was also able to impair the IL-10- and TGFβ-dependent tolerization effect (Figures 4(a) and 4(b)). Since we have observed that both IL-10 and TGFβ induce the expression of miR-146b (Figure 1(c)), altogether these data candidate miR-146b as an effector of LPS tolerance.
Figure 4.
Inhibitory role of IFNγ on IL-10- and TGFβ-dependent endotoxin tolerance. Monocytes were pretreated or not with 10 ng/mL IFNγ and primed with 10 ng/mL IL-10 (a) or 50 ng/mL TGFβ (b) for 18 h and then stimulated with 10 ng/mL LPS. Supernatants were collected 24 h later; TNFα protein levels were quantified by ELISA. Results are expressed as mean ± SEM of three independent experiments.
3.4. Upregulation of miR-146b Mimics LPS Priming to Induce Endotoxin Tolerance
To determine the role of miR-146b in endotoxin tolerance, we used the THP-1 monocytic cell line, a well-established model for in vitro study of endotoxin tolerance. We showed that both miR-146b and miR-146a were significantly induced by LPS (Figure 5(a)). This data were consistent with the expression data of miR-146b and miR-146a in human primary monocytes. In order to discriminate the relative contribution of miR-146b to the establishment of the endotoxin tolerance phenotype, we transduced THP-1 monocytic cells with lentiviral vectors to specifically overexpress (pRRL-146b THP-1 cells) or inhibit miR-146b isoform (miRT-146b THP-1 cells) without affecting miR-146a expression (Figures 5(b)–5(d)). As shown in Figure 5(e), pRRL-146b THP-1 cells stimulated with a single dose of LPS exhibited lower levels of TNFα as compared to pRRL-ct THP-1 cells, thus inducing a state of hyporesponsiveness to LPS similar to that observed by the subsequent LPS stimulation. Accordingly, the induction of endotoxin tolerance by priming monocytes with LPS, IL-10, or TGFβ was completely abolished when the endogenous miR-146b expression was inhibited (Figure 5(f)). Therefore, LPS responsiveness was restored in all the three different in vitro model of endotoxin tolerance, demonstrating that miR-146b is induced during LPS tolerance as part of the inhibitory feedback mechanism that take place in monocytes to render cells refractory to subsequent LPS challenge. Figure 6 depicts the proposal model of miR-146b and miR-146a effect on induction of endotoxin tolerance.
Figure 5.
(a) THP-1 wild-type cells were stimulated for the indicated times with 1 μg/mL of LPS. MiR-146b (black circles) and miR-146a (white circles) were measured by qPCR and their levels were normalized relative to U6. (b-d) miRT-ct and miRT-146b THP-1 cells were primed or not with 100 ng/mL LPS (b), 20 ng/mL IL-10 (c), or 50 ng/mL TGFβ (d) for 18 h and then challenged with 1 ug/mL LPS for 24 h. MiR-146b (black columns) and miR-146a (white columns) were measured by qPCR and normalized to U6 levels. (e) TNFα protein levels were measured by ELISA in cell-free supernatants of pRRL-ct (white columns) or pRRL-146b (black columns) THP-1 cells primed or not with 100 ng/ml LPS and stimulated with 1 ug/mL LPS. (f) miRT-ct (white columns) and miRT-146b (black columns) THP-1 cells were primed or not with 100 ng/mL LPS, 20 ng/mL IL-10, or 50 ng/mL TGFβ for 18 h and then challenged with 1 ug/mL LPS for 24 h. TNFα protein levels were quantified by ELISA. Results are expressed as mean ± SEM of three independent experiments.
Figure 6.
MiR-146 a/b effect on induction of endotoxin tolerance. During overt inflammation activation of the TLR4 signaling pathway triggers the induction of proinflammatory cytokines, including TNFα, IL-6, CCL3, and IL-12. In the late phase of the inflammatory response, the induction of anti-inflammatory genes, including IL-10 and TGFβ, drives the expression of miR-146b through STAT3 and RUNX3, which negatively modulate TLR pathway at different steps, thus inducing tolerance.
4. Discussion
Deregulation of the inflammatory response contributes to tissue damage in pathological conditions such as autoimmune diseases and cancer [3, 41, 42]. The innate immune system has developed a number of mechanisms, such as endotoxin tolerance, to balance inflammation. Endotoxin tolerance is a complex, orchestrated counter-regulatory response to inflammation, during which monocytes undergo a global transcriptional and functional reprogramming and enter into a refractory state, unresponsive to a subsequent LPS challenge. A characteristic feature of endotoxin tolerance is the downregulation of several proinflammatory genes and the concomitant upregulation of some anti-inflammatory genes [43]. In particular, the induction of IL-10 and TGFβ in the late phase of the inflammatory response represents a key step for the induction of endotoxin tolerance [16, 21, 44] leading to leukocyte deactivation through the impairment of TLR signaling. Defects of TLR4 signaling have been observed at the level of the receptor, adaptors, transcription factors, and signaling molecules. In this regard, recent studies have focus attention on the differential expression and effects of miRNA in the modulation of TLR4 signaling in monocytes [18–20] and interestingly, new evidence suggests the involvement of miRNA in the regulation of key components of TLR4 pathway during endotoxin tolerance [28, 29].
The miR-146 family, composed by miR-146a and miR-146b, has been implicated in the regulation of immune cell signaling [45, 46] and more interestingly in the modulation of the inflammatory response in monocytes [18, 21, 22]. In particular, miR-146a was shown to be involved in LPS response and in endotoxin tolerance; recent clinical studies showed increased expression of miR-146a in monocytes isolated from CLL patients, challenged with LPS ex vivo [47]. A correlation between miR-146a gene polymorphisms and the risk of severe sepsis has also been described [48]. Despite these first studies highlighting the important role of miR-146a in endotoxin tolerance, the possible contribution of miR-146b in the regulation of the LPS response has not yet been addressed potentially based on the report by Taganov et al. [18], indicating that miR-146a was the major miRNA of the miR-146 family induced by LPS in THP-1 monocytes.
We previously described miR-146b as the other miR-146 family member able to negatively modulate the inflammatory response in phagocytes by targeting multiple components of the TLR signaling pathway [21]. Since defects in TLR signaling and in the consequent release of proinflammatory cytokines are characteristics of endotoxin tolerance, we thought to shed light on the potential role of miR-146b in the induction of the tolerant state. We first demonstrate that both miR-146b and miR-146a are expressed in LPS-stimulated human primary monocytes and in THP-1 monocytic cells. Secondly, their expression is induced in LPS-tolerized monocytes. Since both miRNAs are abundantly expressed in this cellular context and have overlapping target genes, to discriminate the relative contribution of miR-146b to the establishment of the endotoxin tolerance phenotype, we transduced THP-1 cells with a miR-146b lentiviral vector, which specifically inhibits miR-146b isoform without affecting miR-146a expression. We found that inhibition of endogenous miR-146b levels in LPS tolerized cells completely restored the levels of TNFα protein, here used as readout of endotoxin tolerance. Accordingly, the enforced expression of miR-146b in THP-1 monocytes mimicked the effects of LPS priming, inducing a state of tolerance comparable to that observed by the sequential stimulation with LPS in control cells. Remarkably, miR-146b but not miR-146a expression levels were further induced by LPS when monocytes were primed with TGFβ- and IL-10-tolerized monocytes and this is consistent with the specific upregulation of miR-146b in anti-inflammatory conditions. Indeed, characterization of miR-146b transcriptional regulation by bioinformatics analysis and ChIP experiments showed that RUNX3, an important mediator of TGFβ signaling, is specifically recruited to miR-146b promoter in monocytes challenged with TGFβ, while STAT3 drives the expression of miR-146b in both TGFβ and IL-10 stimulated monocytes. It is known that IFNγ can prevent or revert endotoxin tolerance through the inhibition of TGFβ and IL-10 signaling [37], although the precise molecular mechanism responsible for IFNγ-dependent negative feedback loop is still incompletely elucidated. Importantly, the direct induction of miR-146b by IL-10 or TGFβ as well as its indirect induction after LPS challenge was completely abolished by IFNγ.
Altogether our data propose miR-146b as a key anti-inflammatory miRNA, which acts together with miR-146a in mediating endotoxin tolerance. Notably, we demonstrated a differential regulation of miR-146b and miR-146a expression, suggesting that miR-146b could be one of the molecular tools used by IL-10 and TGFβ to induce an LPS refractoriness state. We also suggest that the two miR-146 family members may represent the components of a relay team in which the two isoforms succeed each other to control expression of proinflammatory genes. Although the observed miR-146b effect in the induction of endotoxin tolerance is consistent with the previously shown regulation of the TLR signaling pathway by miR-146b [21], it is known that endotoxin tolerance is a more complex process, involving a wider cellular regulation. Other biological processes, such as phagocytosis or antigen presentation, should be investigated in in vivo models of endotoxin tolerance to shed light on the effective impact of miR-146b and miR-146a deregulation in the context of endotoxin tolerance. Moreover, due to the large clinical implications of endotoxin tolerance it would be interesting to test the impact of miR-146b deregulation in a clinical context. Further investigations covering all these aspects are needed to candidate miR-146b as a possible therapeutic tool for treating several clinical conditions, such as sepsis and other inflammatory-related disorders.
Acknowledgments
The authors thank Dr. S. Moleirinho for her help in editing and proofreading the paper. This study was supported by research grants from the European Community's Seventh Framework Program [FP7-2007–2013] under grant agreement HEALTH-F4-2011-281608 (TIMER), Ministero dell'Istruzione dell'Università e della Ricerca (PRIN Project 2009JP9WTS_002; FIRB project RBFR08CW8G), the Italian Association for Cancer Research (AIRC), and Fondazione Cariplo.
Conflict of Interests
All authors disclose any commercial affiliations or consultancies, stock or equity interests, or patent-licensing arrangements that could be considered to pose a conflict of interests regarding the submitted paper.
References
- 1.Serhan C. N., Brain S. D., Buckley C. D., et al. Resolution of inflammation: State of the art, definitions and terms. The FASEB Journal. 2007;21(2):325–332. doi: 10.1096/fj.06-7227rev. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Libby P. Inflammation in atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology. 2045;32(9):2045–2051. doi: 10.1161/ATVBAHA.108.179705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lu H., Ouyang W., Huang C. Inflammation, a key event in cancer development. Molecular Cancer Research. 2006;4(4):221–233. doi: 10.1158/1541-7786.MCR-05-0261. [DOI] [PubMed] [Google Scholar]
- 4.López-Collazo E., del Fresno C. Pathophysiology of endotoxin tolerance: mechanisms and clinical consequences. Critical Care. 2013;17(6, article 242) doi: 10.1186/cc13110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schilling D., Thomas K., Nixdorff K., Vogel S. N., Fenton M. J. Toll-like receptor 4 and Toll-IL-1 receptor domain-containing adapter protein (TIRAP)/myeloid differentiation protein 88 adapter-like (Mal) contribute to maximal IL-6 expression in macrophage. The Journal of Immunology. 2002;169(10):5874–5880. doi: 10.4049/jimmunol.169.10.5874. [DOI] [PubMed] [Google Scholar]
- 6.Escoll P., Del Fresno C., García L., et al. Rapid up-regulation of IRAK-M expression following a second endotoxin challenge in human monocytes and in monocytes isolated from septic patients. Biochemical and Biophysical Research Communications. 2003;311(2):465–472. doi: 10.1016/j.bbrc.2003.10.019. [DOI] [PubMed] [Google Scholar]
- 7.Cavaillon J.-M., Adrie C., Fitting C., Adib-Conquy M. Reprogramming of circulatory cells in sepsis and SIRS. Journal of Endotoxin Research. 2005;11(5):311–320. doi: 10.1179/096805105X58733. [DOI] [PubMed] [Google Scholar]
- 8.del Fresno C., Soler-Rangel L., Soares-Schanoski A., et al. Inflammatory responses associated with acute coronary syndrome up-regulate IRAK-M and induce endotoxin tolerance in circulating monocytes. Journal of Endotoxin Research. 2007;13(1):39–52. doi: 10.1177/0968051907078623. [DOI] [PubMed] [Google Scholar]
- 9.del Fresno C., García-Rio F., Gómez-Piña V., et al. Potent phagocytic activity with impaired antigen presentation identifying lipopolysaccharide-tolerant human monocytes: demonstration in isolated monocytes from cystic fibrosis patients. The Journal of Immunology. 2009;182(10):6494–6507. doi: 10.4049/jimmunol.0803350. [DOI] [PubMed] [Google Scholar]
- 10.del Fresno C., Gómez-Piña V., Lores V., et al. Monocytes from cystic fibrosis patients are locked in an LPS tolerance state: down-regulation of TREM-1 as putative underlying mechanism. PLoS ONE. 2008;3(7) doi: 10.1371/journal.pone.0002667.e2667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Randow F., Syrbe U., Meisel C., et al. Mechanism of endotoxin desensitization: involvement of interleukin 10 and transforming growth factor β . The Journal of Experimental Medicine. 1995;181(5):1887–1892. doi: 10.1084/jem.181.5.1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schröder M., Meisel C., Buhl K., et al. Different modes of IL-10 and TGF-beta to inhibit cytokine-dependent IFN-gamma production: consequences for reversal of lipopolysaccharide desensitization. The Journal of Immunology. 2003;170(10):5260–5267. doi: 10.4049/jimmunol.170.10.5260. [DOI] [PubMed] [Google Scholar]
- 13.Foster S. L., Medzhitov R. Gene-specific control of the TLR-induced inflammatory response. Clinical Immunology. 2009;130(1):7–15. doi: 10.1016/j.clim.2008.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cavaillon J.-M., Adib-Conquy M. Bench-to-bedside review: endotoxin tolerance as a model of leukocyte reprogramming in sepsis. Critical Care. 2006;10(5, article 233) doi: 10.1186/cc5055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Biswas S. K., Lopez-Collazo E. Endotoxin tolerance: new mechanisms, molecules and clinical significance. Trends in Immunology. 2009;30(10):475–487. doi: 10.1016/j.it.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 16.Monneret G., Finck M.-E., Venet F., et al. The anti-inflammatory response dominates after septic shock: association of low monocyte HLA-DR expression and high interleukin-10 concentration. Immunology Letters. 2004;95(2):193–198. doi: 10.1016/j.imlet.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 17.Manjuck J., Saha D. C., Astiz M., Eales L.-J., Rackow E. C. Decreased response to recall antigens is associated with depressed costimulatory receptor expression in septic critically ill patients. Journal of Laboratory and Clinical Medicine. 2000;135(2):153–160. doi: 10.1067/mlc.2000.104306. [DOI] [PubMed] [Google Scholar]
- 18.Taganov K. D., Boldin M. P., Chang K.-J., Baltimore D. NF-κB-dependent induction of microRNA miR-146, an inhibitor targeted to signaling proteins of innate immune responses. Proceedings of the National Academy of Sciences of the United States of America. 2006;103(33):12481–12486. doi: 10.1073/pnas.0605298103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O'Connell R. M., Taganov K. D., Boldin M. P., Cheng G., Baltimore D. MicroRNA-155 is induced during the macrophage inflammatory response. Proceedings of the National Academy of Sciences of the United States of America. 2007;104(5):1604–1609. doi: 10.1073/pnas.0610731104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rossato M., Curtale G., Tamassia N., et al. IL-10-induced microRNA-187 negatively regulates TNF-alpha, IL-6, and IL-12p40 production in TLR4-stimulated monocytes. Proceedings of the National Academy of Sciences of the United States of America. 2012;109(45):E3101–E3110. doi: 10.1073/pnas.1209100109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Curtale G., Mirolo M., Renzi T. A., Rossato M., Bazzoni F., Locati M. Negative regulation of Toll-like receptor 4 signaling by IL-10-dependent microRNA-146b. Proceedings of the National Academy of Sciences of the United States of America. 2013;110(28):11499–11504. doi: 10.1073/pnas.1219852110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao J. L., Rao D. S., Boldin M. P., Taganov K. D., O'Connell R. M., Baltimore D. NF-kappaB dysregulation in microRNA-146a-deficient mice drives the development of myeloid malignancies. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(22):9184–9189. doi: 10.1073/pnas.1105398108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O'Connell R. M., Chaudhuri A. A., Rao D. S., Baltimore D. Inositol phosphatase SHIP1 is a primary target of miR-155. Proceedings of the National Academy of Sciences of the United States of America. 2009;106(17):7113–7118. doi: 10.1073/pnas.0902636106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hou J., Wang P., Lin L., et al. MicroRNA-146a feedback inhibits RIG-I-dependent type I IFN production in macrophages by targeting TRAF6, IRAK1, and IRAK2. The Journal of Immunology. 2009;183(3):2150–2158. doi: 10.4049/jimmunol.0900707. [DOI] [PubMed] [Google Scholar]
- 25.Huang R.-S., Hu G.-Q., Lin B., Lin Z.-Y., Sun C.-C. Microrna-155 silencing enhances inflammatory response and lipid uptake in oxidized low-density lipoprotein-stimulated human THP-1 macrophages. Journal of Investigative Medicine. 2010;58(8):961–967. doi: 10.231/jim.0b013e3181ff46d7. [DOI] [PubMed] [Google Scholar]
- 26.McCoy C. E., Sheedy F. J., Qualls J. E., et al. IL-10 inhibits miR-155 induction by toll-like receptors. The Journal of Biological Chemistry. 2010;285(27):20492–20498. doi: 10.1074/jbc.m110.102111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu G., Friggeri A., Yang Y., Park Y.-J., Tsuruta Y., Abraham E. miR-147, a microRNA that is induced upon toll-like receptor stimulation, regulates murine macrophage inflammatory responses. Proceedings of the National Academy of Sciences of the United States of America. 2009;106(37):15819–15824. doi: 10.1073/pnas.0901216106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nahid M. A., Pauley K. M., Satoh M., Chan E. K. L. miR-146a is critical for endotoxin-induced tolerance: implication in innate immunity. The Journal of Biological Chemistry. 2009;284(50):34590–34599. doi: 10.1074/jbc.m109.056317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nahid M. A., Satoh M., Chan E. K. L. Mechanistic role of microRNA-146a in endotoxin-induced differential cross-regulation of TLR signaling. Journal of Immunology. 2011;186(3):1723–1734. doi: 10.4049/jimmunol.1002311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tili E., Michaille J.-J., Cimino A., et al. Modulation of miR-155 and miR-125b levels following lipopolysaccharide/TNF-alpha stimulation and their possible roles in regulating the response to endotoxin shock. Journal of Immunology. 2007;179(8):5082–5089. doi: 10.4049/jimmunol.179.8.5082. [DOI] [PubMed] [Google Scholar]
- 31.O'Neill L. A., Sheedy F. J., McCoy C. E. MicroRNAs: the fine-tuners of Toll-like receptor signalling. Nature Reviews Immunology. 2011;11(3):163–175. doi: 10.1038/nri2957. [DOI] [PubMed] [Google Scholar]
- 32.Tamassia N., Castellucci M., Rossato M., et al. Uncovering an IL-10-dependent NF-κB recruitment to the IL-1ra promoter that is impaired in STAT3 functionally defective patients. The FASEB Journal. 2010;24(5):1365–1375. doi: 10.1096/fj.09-145573. [DOI] [PubMed] [Google Scholar]
- 33.Yang L., Boldin M. P., Yu Y., et al. miR-146a controls the resolution of T cell responses in mice. Journal of Experimental Medicine. 2012;209(9):1655–1670. doi: 10.1084/jem.20112218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ito Y., Bae S.-C., Chuang L. S. H. The RUNX family: developmental regulators in cancer. Nature Reviews Cancer. 2015;15(2):81–95. doi: 10.1038/nrc3877. [DOI] [PubMed] [Google Scholar]
- 35.Ito Y., Miyazono K. RUNX transcription factors as key targets of TGF-beta superfamily signaling. Current Opinion in Genetics and Development. 2003;13(1):43–47. doi: 10.1016/s0959-437x(03)00007-8. [DOI] [PubMed] [Google Scholar]
- 36.Heagy W., Hansen C., Nieman K., West M. A. Evidence for a CD14- and serum-independent pathway in the induction of endotoxin-tolerance in human monocytes and THP-1 monocytic cells. Shock. 2003;19(4):321–327. doi: 10.1097/00024382-200304000-00005. [DOI] [PubMed] [Google Scholar]
- 37.Herrero C., Hu X., Li W. P., et al. Reprogramming of IL-10 activity and signaling by IFN-γ 1 . Journal of Immunology. 2003;171(10):5034–5041. doi: 10.4049/jimmunol.171.10.5034. [DOI] [PubMed] [Google Scholar]
- 38.Randow F., Döcke W.-D., Bundschuh D. S., Hartung T., Wendel A., Volk H.-D. In vitro prevention and reversal of lipopolysaccharide desensitization by IFN-γ, IL-12, and granulocyte-macrophage colony-stimulating factor. Journal of Immunology. 1997;158(6):2911–2918. [PubMed] [Google Scholar]
- 39.Varma T. K., Toliver-Kinsky T. E., Lin C. Y., Koutrouvelis A. P., Nichols J. E., Sherwood E. R. Cellular mechanisms that cause suppressed gamma interferon secretion in endotoxin-tolerant mice. Infection and Immunity. 2001;69(9):5249–5263. doi: 10.1128/IAI.69.9.5249-5263.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bundschuh D. S., Barsig J., Hartung T., et al. Granulocyte-macrophage colony-stimulating factor and IFN-γ restore the systemic TNF-α response to endotoxin in lipopolysaccharide-desensitized mice. Journal of Immunology. 1997;158(6):2862–2871. [PubMed] [Google Scholar]
- 41.Sica A., Allavena P., Mantovani A. Cancer related inflammation: the macrophage connection. Cancer Letters. 2008;267(2):204–215. doi: 10.1016/j.canlet.2008.03.028. [DOI] [PubMed] [Google Scholar]
- 42.Sica A., Mantovani A. Macrophage plasticity and polarization: in vivo veritas. The Journal of Clinical Investigation. 2012;122(3):787–795. doi: 10.1172/jci59643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Melo E. S., Barbeiro D. F., Gorjão R., et al. Gene expression reprogramming protects macrophage from septic-induced cell death. Molecular Immunology. 2010;47(16):2587–2593. doi: 10.1016/j.molimm.2010.06.011. [DOI] [PubMed] [Google Scholar]
- 44.Pan H., Ding E., Hu M., Lagoo A. S., Datto M. B., Lagoo-Deenadayalan S. A. SMAD4 is required for development of maximal endotoxin tolerance. The Journal of Immunology. 2010;184(10):5502–5509. doi: 10.4049/jimmunol.0901601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Curtale G., Citarella F., Carissimi C., et al. An emerging player in the adaptive immune response: microRNA-146a is a modulator of IL-2 expression and activation-induced cell death in T lymphocytes. Blood. 2010;115(2):265–273. doi: 10.1182/blood-2009-06-225987. [DOI] [PubMed] [Google Scholar]
- 46.Fallah P., Arefian E., Naderi M., et al. MiR-146a and miR-150 promote the differentiation of CD133+ cells into T-lymphoid lineage. Molecular Biology Reports. 2013;40(8):4713–4719. doi: 10.1007/s11033-013-2567-6. [DOI] [PubMed] [Google Scholar]
- 47.Jurado-Camino T., Córdoba R., Esteban-Burgos L., et al. Chronic lymphocytic leukemia: a paradigm of innate immune cross-tolerance. Journal of Immunology. 2015;194(2):719–727. doi: 10.4049/jimmunol.1402272. [DOI] [PubMed] [Google Scholar]
- 48.Shao Y., Li J., Cai Y., et al. The functional polymorphisms of miR-146a are associated with susceptibility to severe sepsis in the Chinese population. Mediators of Inflammation. 2014;2014:10. doi: 10.1155/2014/916202.916202 [DOI] [PMC free article] [PubMed] [Google Scholar]