Abstract
Human Metapneumovirus (hMPV) is a leading respiratory viral pathogen associated with bronchiolitis, pneumonia, and asthma exacerbation in young children, the elderly and immunocompromised individuals. The development of a potential vaccine against hMPV requires detailed understanding of the host immune system, which plays a significant role in hMPV pathogenesis, susceptibility and vaccine efficacy. As a result, animal models have been developed to better understand the mechanisms by which hMPV causes disease. Several animal models have been evaluated and established so far to study the host immune responses and pathophysiology of hMPV infection. However, inbred laboratory mouse strains have been one of the most used animal species for experimental modeling and therefore used for the studies of immunity and immunopathogenesis to hMPV. This review summarizes the contributions of the mouse model to our understanding of the immune response against hMPV infection.
Keywords: human metapneumovirus, paramyxovirus, mouse model, immune responses
1. Introduction
Human metapneumovirus (hMPV), belongs to the Paramyxoviridae family and represents the first human member of the genus Metapneumovirus. hMPV is a leading respiratory viral pathogen causing acute respiratory tract infection (ARTI) in young children, the elderly and immunocompromised individuals [1]. hMPV was first isolated in the Netherlands in 2001 from respiratory specimens of young children suffering with acute respiratory tract illness [2] and represents a major respiratory pathogen worldwide. Epidemiological studies show that hMPV is responsible for 5%–15% of pediatric hospitalizations for respiratory tract infections [3,4,5,6,7]. It induces clinical syndromes ranging from mild disease to more severe disease, with high fever, wheezing, severe cough, difficulty in breathing, tachypnea, bronchiolitis and pneumonia [8,9,10].
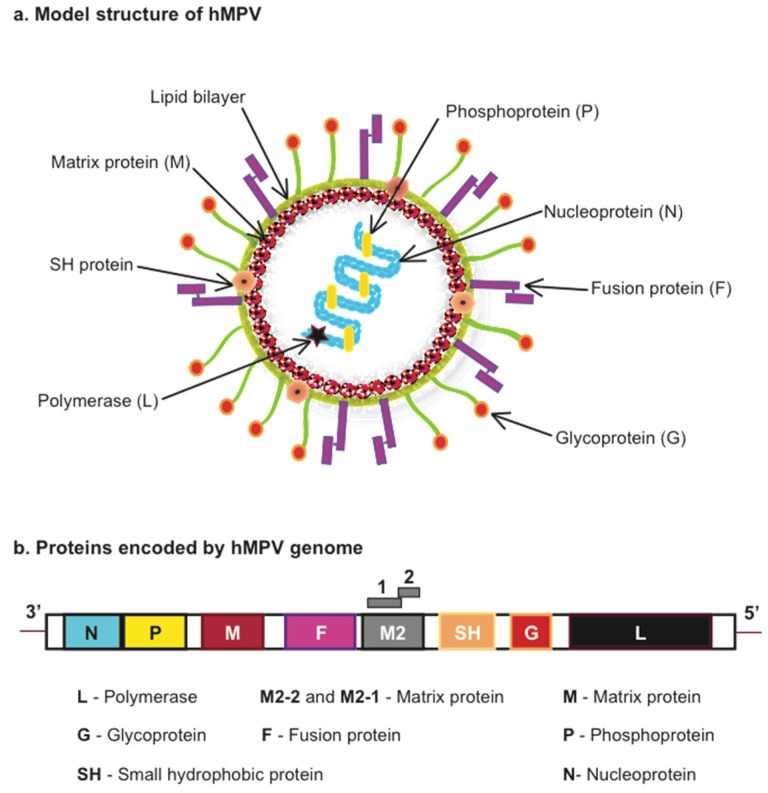
hHMPV is an enveloped, negative sense single-stranded RNA virus (Figure 1). Based on phylogenetic analysis, hMPV is classified into four genetic lineages, named A1, A2, B1 and B2 that divide into the A and B antigenic subgroups that belong to one serotype [11,12]. hMPV genome size is approximately 13,000 nt as it varies depending on the strain. Examples of the subgroup A indicate that the strain CAN97-83 is 13,335 nt and NL/00/1 is 13,350 nt, and for the subgroup B: CAN98-75 is 13,280 nt and NL/1/99 is 13,293 nt [11,13]. The hMPV sequence includes eight genes encoding nine proteins: nucleocapsid (N), phosphoprotein (P), matrix (M), second matrix (M2-1, M2-2), fusion (F), small hydrophobic (SH), attachment (G) and RNA-dependent RNA polymerase (L). The gene order in hMPV is represented as 3′-N-P-M-F-M2-SH-G-L-5′ (Figure 1). The attachment (G) and small hydrophobic (SH) genes are found to be highly variable while a high level of sequence conservation has been observed for the fusion (F) gene [13]. The G protein is a transmembrane surface glycoprotein, which initiates the virus-host cell membrane attachment and so considered as a key player in viral replication. The fusion (F) protein is required for the fusion of virus with host cell membrane and is capable of being accessed by neutralizing antibodies. The nucleocapsid (N), phosphoprotein (P) and RNA-dependent RNA polymerase (L) proteins along with M2 protein are involved in RNA synthesis [11,14,15].
Figure 1.
Model structure and proteins encoded by Human Metapneumovirus (hMPV). (a) hMPV model structure indicating viral proteins encoded by (b) the viral genome.
Several animal models including mouse (see Table 1), cotton rat [16,17,18,19], hamster [20,21,22], ferret [20] and nonhuman primate models [20,23,24] have been established to date to study the immunopathology occurring after hMPV infection. Among them, the mouse model has provided considerable knowledge towards our understanding of the hMPV-host interaction. Thus this review focuses on the current knowledge of the immunity and immunopathology induced by hMPV in the experimental mouse model of infection.
Table 1.
Different conditions for mouse infection with hMPV.
| Mice Strain | Mice Age | (Group) Strain | Virus Dose | Refs. |
|---|---|---|---|---|
| BALB/c | F 6–8 week-old | (A) NL 00-01 | 3.3 × 105 PFU | [25] |
| BALB/c | F 4–6-week-old | (A) C-85473 | 1.5 × 105–108 TCID50 | [16,26,27,28,29,30,31,32] |
| BALB/c | F 6–8-week-old | (A) C4-CJP05 | 106 PFU | [33] |
| BALB/c | F 4–6-week-old | (B) CAN98-75 | 0.8–1 × 106 PFU | [29,34,35] |
| BALB/c | F 5–7 week-old | (A) NL/1/00 | 106–107 PFU | [20,36] |
| BALB/c | F 6–7 week-old | (B) NL/1/99 | 107 PFU | [36] |
| BALB/c | F 6–10 week-old | (A) CAN97-83 | 106–107 PFU/TCID50 | [30,37,38,39,40,41] |
| BALB/c | F 5–6 week-old | (A) CZ0107 | 106 PFU | [42] |
| BALB/c | M 19 month-old | (A) CAN97-83 | 2 × 107 geq | [43] |
| BALB/c | F 8–10 week-old | (A) D03-574 | 2 × 105 PFU | [44] |
| C57BL/6 | 6–10 week-old | (A) CAN97-83 | 106–107 PFU | [38,45,46,47,48,49] |
| C57BL/6 | F 6–12 week-old | (A) TN/94-49 | 0.6–1.5 × 106 PFU | [50,51,52,53] |
| DBA/2 | 5–6 week-old | (A) TN/94-49 | 105.9 PFU | [17] |
| SCID | F 6–8 week-old | (A) NL/1/00 | 6.5 × 106 PFU | [54] |
PFU = Plaque Forming Units; geq = genome equivalents; TCID50 = 50% tissue culture infective dose.
2. hMPV Infection in Mice
The experimental mouse model of hMPV infection has been established in several mouse backgrounds using different hMPV strains at diverse inoculum concentrations, as shown in Table 1.
Intranasal inoculation of mice with hMPV induces pulmonary inflammation characterized by interstitial inflammation and/or peribronchiolar and perivascular cellular infiltration [30,35,39,49], body weight loss with a peak of 15%–25% [16,25,32,34,41], altered respiratory function characterized by a significant increase in airway obstruction on day 5 after hMPV infection that could persist until day 21 [30], and lung viral titers that peak between day 3 to day 14 after hMPV infection [16,25,30,41].
However, some variations can be observed depending on the different experimental conditions. For instance, intranasal inoculation of BALB/c mice with hMPV CAN98-75 resulted in a biphasic lung viral replication with peaks at day 7 and day 14 [34,35] while infection of BALB/c mice with any other hMPV strain led to a one-peak only of viral titer on or before day 5 after infection (Table 2). Based on the data from the reports included in Table 2, BALB/c mice appear to be more permissive than C57BL/6 mice. Although, shedding of infectious virus beyond the recovery phase has been rarely reported [34], detection of hMPV transcripts have been found at day 154 [30] and 180 [34] after infection, suggesting that hMPV could persist in the lung of infected animals since hMPV infection has been characterized as a localized infection affecting just the airways but no other organs [35].
Table 2.
Mouse susceptibility and permissibility to hMPV.
| Mice Strain | Virus Strain | Virus Inoculum | Peak Viral Titer | Ref. |
|---|---|---|---|---|
| BALB/c | NL/1/00 | 3.3 × 105 PFU | Day 4 (Log10 2.37 PFU/g) | [25] |
| BALB/c | CAN97-83 | 107 TCID50 | Day 4 (105 TCID50/g) | [41] |
| BALB/c | C85473 | 1.5 × 105 TCID50 | Day 6 (~104 TCID50/lung) | [26] |
| BALB/c | C85473 | 1 × 108 TCID50 | Day 5 (7 × 106 TCID50/lung) | [30] |
| BALB/c | C85473 | 1 × 108 TCID50 | Day 5 (1.92 × 107 TCID50/g) | [16] |
| BALB/c | C85473 | 5.8 × 105 TCID50 | Day 5 (~105 TCID50/g) | [32] |
| BALB/c | NL/1/00 | 1.5 × 105 PFU | Day 5 (5.1 × 105 PFU/g) | [55] |
| BALB/c | D03-574 | 2 × 105 PFU | Day 4 (~103.6 PFU/lung) | [44] |
| C57BL/6 | CAN97-83 | 5 × 106 PFU | Day 5 (104.9 PFU/g) | [46] |
| C57BL/6 | TN/94-49 | 1 × 106 PFU | Day 5 (~4.7 Log10 PFU/g) | [53] |
| C57BL/6 | CAN97-83 | 1 × 107 PFU | Day 5 (~4.1 Log10 PFU/g) | [47] |
| C57BL/6 | TN/94-49 | 6 × 105 PFU | Day 5 (~4.2 Log10 PFU/g) | [51] |
3. Lung Antiviral and Inflammatory Responses
3.1. Innate Immunity
Innate immune responses to viral infections in the lung serve as the first line of defense and it is activated upon recognition of the pathogen by immune cells in the respiratory tract. The cellular barrier constituting neutrophils, macrophages, natural killer (NK) cells and dendritic cells (DC) play a key role in the innate immune responses, which is triggered by the recognition of pathogen associated molecular pattern (PAMP) by cell receptors called pattern recognition receptors (PRRs) expressed in most cells of the respiratory tract. These pattern recognition receptors are broadly classified into membrane bound Toll-like receptors (TLRs), C-type lectin receptors (CLR), cytoplasmic RIG-I-like receptors (RLRs) and nucleotide-binding oligomerization domain (NOD)-like receptors (NLRs) [56]. The recognition of viral PAMPs by the cellular PRRs initiate the activation of signaling pathways leading to the production of cytokines and chemokines by the cells in the respiratory tract, that in turn regulate the inflammatory and immune responses in the infected host.
3.1.1. Pattern Recognition Receptors and Signaling Pathways
We have recently demonstrated the importance of the RLR helicase melanoma differentiation-associated gene 5 (MDA5) in the type I (α/β) and type III (λ) interferon (IFN) production by hMPV infection [45]. In a model of MDA5-deficient mice (C57BL/6J background) infected with hMPV CAN97-83, the lack of MDA5 resulted in a decreased viral clearance, enhanced disease severity and pulmonary inflammation, and was necessary for the production of IFN-α/β and IFN-λ2/3. Moreover, MDA5 regulated the production of cytokines and chemokines in response to hMPV, demonstrating the critical role MDA5 plays in the control of hMPV-induced disease [45]. Downstream of the MDA5 signaling pathway, this helicase interacts with the adaptor molecule IFN-promoter stimulator 1 (IPS-1) at the mitochondrial membrane in order to induce the expression of cytokines [57]. In that regard, studies in neonatal IPS-1 deficient mice (C57BL/6 background) have shown that the absence of IPS-1 led to an increased viral load and decreased production of IFN-β and IFN-λ2/3 at day 1 after hMPV infection [58], indicating that IPS-1 contributes to the antiviral response and hMPV clearance. Moreover, similar IFN response to hMPV infection in the absence of IPS-1 has been reported in adult mice [59]. Thus, these findings confirm the key role for the MDA5 and IPS-1 signaling pathway in the antiviral response against hMPV infection.
On the other hand, data of hMPV infection in C57BL/10ScSnJ Toll-like receptor 4 (TLR4) deficient mice have shown that absence of TLR4 resulted in a decreased inflammatory response, disease severity, as well as IFN-α/β and cytokine production [48]. In line with those data, the lack of myeloid differentiation protein response 88 (MyD88), an essential adaptor molecule for TLR’s (except TLR3), led to a reduced lung inflammation and disease severity compared to wild type mice. The absence of MyD88 also impaired the production of cytokines and chemokines and the recruitment of DC, CD4 and CD8 T cells into the lungs of infected mice [47]. Collectively, these studies indicate that TLR4 and MyD88 are key molecules that regulate the hMPV-induced pulmonary inflammation and disease pathology in mice.
Signaling via PRRs ultimately leads to the activation of the transcription factors interferon (IFN) regulatory factors (IRFs), which induce the expression of the interferons and cytokine responses. Data in C57BL/6 mice have demonstrated that the expression of both IRF3 and IRF7 were necessary for the production of IFN-α/β [45]. In agreement with these results, in hMPV-infected C57BL/6 neonatal mice, both IRF3 and IRF7 were necessary for the expression of IFN-α4 and IFN-β. Moreover, the absence of both IRF3 and IRF7 exacerbated the Th1, Th2, and Th17 lymphocyte responses as well as the recruitment of neutrophils, eosinophils, NK and NK T cells in response to hMPV infection [58]. Similarly, the production of IFN-λ2/3 after hMPV infection was regulated by the expression of IRF-7 in adult [49] and neonatal [58] mice. However, the expression of IRF-3 was necessary for the production of IFN-λ2/3 in neonatal mice [58] but it was dispensable when the IFN-λ2/3 was induced by hMPV in adult mice [49], suggesting that the activation of the IFN-λ response by hMPV in adult and young mice is differentially regulated by IRF-3 and IRF-7 expression. Interestingly, hMPV has also been reported to inhibit the IFN responses [39,49]. Studies in BALB/c mice have demonstrated that hMPV infection inhibits the poly-ICLC- (synthetic dsRNA, TLR3/RIG-I/MDA5 agonist) and CpG-ODN- (TLR9 agonist) induced IFN-α production [39], suggesting that hMPV infection is able to inhibit the activation of RLRs and TLRs in vivo. In addition, recent data have shown that hMPV G protein inhibits the production of IFN-λ2/3 in BALB/c mice after hMPV infection, at least through the interference with the RIG-I/MDA5 pathway [49].
Based on the reported observations described above, hMPV-induced immune response is regulated by the activation of selected PRRs. It appears that hMPV infection activates TLRs to induce an inflammatory response while it subverts RLRs to alter the antiviral responses via the inhibition of interferons. This immune subversion is attributed to the expression of hMPV G protein. Taken together, experimental evidence demonstrates that hMPV is able to activate and subvert antiviral signaling pathways, likely through different mechanisms. However, unresolved pathways involved in activation or subversion of hMPV induced immune response, need further elucidation. A detailed understating of hMPV induced recognition and signaling cascades is crucial to developing effective therapeutics and vaccine strategies.
3.1.2. Cytokine Production
hMPV is known to induce in humans a profile of cytokines distinct to other respiratory viruses such as respiratory syncytial virus (RSV), and influenza virus [60]. Although very scarce, studies comparing hMPV and RSV infection are clinically relevant as RSV is the closest related human paramyxovirus to hMPV [11]. In fact, symptoms between RSV and hMPV are indistinguishable, ranging from mild cold-like symptoms to more severe clinical manifestations like bronchiolitis or severe pneumonia that require hospitalizations [3,7,61]. However, some aspects of the immune response elicited by these two viral pathogens are distinct. This was demonstrated by the analysis of nasal washes from hospitalized infants showing that hMPV infection induced significantly lower amounts of proinflammatory cytokines including IL-12, IL-6, IL-8, TNF-α and IL-1β compared to RSV infection [60], suggesting that hMPV is a poor inducer of inflammatory cytokines compared to RSV in infected infants. In line with these data, research in the mouse model resembled the observation in human studies. Using BALB/c mice infected with hMPV (CAN97-83) and compared to RSV (A2) side-by-side, hMPV induced a weaker response of proinflammatory cytokines (IL-1α, IL-1β, IL-6, TNF-α, G-CSF) and regulatory cytokines (IL-10, IL-12p70, IL-17). However, hMPV induced a stronger response of IFN-α, GM-CSF, IL-18, CXCL1 (KC) and a sustained production of IL-12p40 [37]. In contrast to this work, a study conducted in BALB/c mice using a clinical hMPV isolate (D03-574) induced significantly higher levels of TNF-α, IL-6 and MCP-1 compared to RSV (A2) at day 4 and 7 post infection [44]. The discrepancies between these two studies in mice could be due to the use of different virus strains and virus stock preparations.
The effect of hMPV on the IFN response has been further confirmed since experimental observations indicated that hMPV induced a stronger response of IFN-β and IFN-λ2/3 when compared to RSV infection in BALB/c mice [49]. However, levels of IFN-γ were induced similarly by hMPV and RSV-infected BALB/c mice [44]. Additional data have also demonstrated the capacity of hMPV to induce several cytokines in the lung, where a significant induction of CCL2 (MCP-1) and CXCL1 (KC) on day 1 and IFN-γ, CCL5 (RANTES), CCL3 (MIP1α), and IL-4 on day 5 after hMPV infection has been observed [16,25]. Overall, these findings suggest that hMPV infection induces a unique profile of cytokines and chemokines in the lung of infected mice.
The regulatory effects that lung cytokines and chemokines exert in hMPV-induced disease are still largely unexplored. In that regard, IL-12p40, an induced cytokine during hMPV infection that remains sustained after the resolution of the disease [37] has been shown to be critical to control disease severity by regulating cytokine production, inflammatory response and mucin production in the lung. Using IL-12p40-/- mice infected with hMPV, showed an increased goblet cell formation, increased mucin gene expression in the airways and decreased lung function. IL-12p40 was found to specifically regulate the expression of IFN-γ, IL-6, CXCL10 (IP-10), CCL11 (eotaxin), CXCL1 (KC, IL-8 homolog) and CCL2 (MCP-1) in mice infected with hMPV [46]. Furthermore, the level of expression of inflammatory cytokines after hMPV infection appears to be altered in aged animals. For instance, TNF-α levels were decreased ~7-fold in 19 moth-old hMPV-infected mice when compared to 4–6 week-old animals [43] while IL-6 was increased in 18–19 month-old mice when compared to 6–8 week old mice [62]. Also, hMPV infection alters the cytokine response to opportunistic bacterial infection in the lung. Prior hMPV infection exacerbated the levels of TNF-α, IFN-γ, IL-1α, IL-1β, IL-6, IL-12p40, IL-12 p70, IL-9, IL-10, IL-13, KC, G-CSF, GM-CSF, MCP-1 and MIP-1α in Streptococcus pneumonia-infected mice and predisposed those animals to severe pneumococcal infection [26]. The described cytokine patterns induced by hMPV infection are crucial to understanding the underlying mechanisms in activation of the innate and adaptive immune responses as well as the initiation and resolution of the inflammatory response and lung viral clearance. However, the role of these cytokine pathways in promoting and modulating inflammation and host immune responses in hMPV infection are still largely unknown. The use of genetically modified mice will represent a critical tool to answer these relevant questions.
3.1.3. Dendritic Cells
Dendritic cells (DC) are professional antigen-presenting cells within the immune system. Respiratory tract dendritic cells are present within airway epithelium, submucosa and associated lung parenchymal tissue under resting conditions [63]. Their strategic localization at the site of pathogen entry makes them particularly susceptible to initial viral invasion. After detection, uptake and degradation of viruses, DC initiate immune responses via the secretion of interferon (IFN), chemokines and proinflammatory cytokines, as well as the upregulation of a variety of costimulatory molecules and receptors, a process globally known as cell maturation. After maturation, DC efficiently present antigens and initiate adaptive immune response by migrating into lymph nodes (LN) to activate the virus-specific T cell response [32]. To date, there have been at least three major subsets of murine lung DC described. These include plasmacytoid DC (pDC), the myeloid DC (also known a conventional DC, cDC), and the interferon-producing killer dendritic cells (IKDC). DC have been reported to participate in the innate and adaptive immune response to hMPV infections, indicating their critical role in the antiviral immunity to this virus. Dendritic cells are susceptible to hMPV infection in vitro [64] and in vivo [40,65]. In fact, hMPV activates mouse lung DC, and induces the upregulation of costimulatory molecules and the secretion of several cytokines including IL-6, IFN-α, IFN-β and TNF-α [40]. hMPV infection also induced the recruitment of pDC and IKDC which peaked by day 8 after infection. The predominant subset recruited to the lung corresponded to cDC, and this remained the highest subset for at least 18 days, beyond the acute phase of infection. CD103+ cDC substantially decreased until three weeks after infection and returned to basal levels by week 8. Differential production of cytokines by murine lung pDC and cDC infected with hMPV was also observed. More interestingly, hMPV infection reduced the capacity of lung cDC to stimulate T cell responses [40], which is in line with some reports in vitro using human DC that indicate that hMPV alters their capacity to activate T cells [64,66].
3.1.4. Alveolar Macrophages
Alveolar macrophages (AMs) are known to be the first line of defense against respiratory pathogens [67]. They reside in the pulmonary alveolus and survey the exposed airways to contribute to the innate host defense against inhaled insults [68]. They are essential source of immunomodulatory cytokines for host responses against lung infections and their depletion results in impaired host response [67,69,70]. In fact, recent work has demonstrated that AMs differentially control the antiviral response and airway inflammation in hMPV infection when compared with RSV [69]. Using a BALB/c mouse model, AMs were depleted using clodronate liposomes (L-CL2MBP) prior to hMPV infection. Depletion of AMs altered the hMPV-induced disease since there was a reduced body weight loss, lung viral titer, decreased lung inflammation and airway hyperresponsiveness (AHR). Moreover, the recruitment of CD4+ T lymphocytes was significantly decreased following AM depletion. AMs are sources of pro inflammatory cytokines and chemokines. In line with this, depletion of AMs resulted in significantly lower level of cytokines including IL-1α, IL-1β, TNF-α, IL-6, GM-CSF, G-CSF, CCL4, IFN-α and IFN-β. However, their depletion also induced an increased release of CCL3, CCL5, and IL-12p40 after hMPV infection [69]. Thus, the results of this study indicate that the presence of alveolar macrophages regulate and contribute to the hMPV-induced disease.
3.1.5. Natural Killer Cells
Another component of the innate immune system are the natural killer (NK) cells, which are lymphocytes that respond to malignant tumors and intracellular pathogens including viruses. Studies conducted by Alvarez et al. demonstrated that NK cells have a leading role in controlling hMPV viral clearance [36]. Depletion of NK cells with anti-CD49b/Pan-NK cell monoclonal antibody in BALB/c mice resulted in increased lung viral titers on days 7, 28 and 60 after infection compared to NK cell competent mice. In contrast, work reported by Wen S. et al. in C57BL/6 mice have demonstrated that NK cells do not contribute to hMPV clearance [51]. Lung NK cell numbers in infected mice were, however, increased as early as day 1 after hMPV infection and peaked on day 3 compared to mock infected mice. Moreover, hMPV infection induced activation of lung NK cells, as indicated by the upregulation of CD69. However, depletion of NK cells using the anti-NK1.1 antibody did not result in changes in lung viral titers, lung histopathology, or the numbers of CD4+ and CD8+ T lymphocytes. Suggesting that, NK cells do not play a significant role in the host responses against hMPV, and that the clearance of the viral infection requires different set of immune components in vivo. The discrepancies between these two studies could be attributed to the use of different experimental conditions, as detailed above. Thus, further work to fully define the role of NK cells in hMPV infection is warranted.
3.2. Adaptive Immunity
Cell mediated immunity serves as an important barrier in the multi-step paradigm of immune responses to pathogenic mechanisms. These responses function mainly by activation of cytotoxic T-lymphocytes to induce apoptosis of virus-infected cells or by activating T helper cells to stimulate other immune cells such as macrophages, B cells and NK cells and aid in the production of distinct cytokine profiles to induce intercellular communication. Experimental evidence with clone-specific induction of cytotoxic T cells [38] and experimental models with T cell depletion studies [34,38,41] demonstrate the essential role of T lymphocytes in immune surveillance and protection in hMPV infection.
Characterization of the T cell response against this virus has indicated that hMPV results in an accumulation of virus-specific cytotoxic CD8+ T cells (CTL) in the lungs 7 days after infection but not in regional lymph nodes or spleen. However, a strong memory response can be recalled from the spleen at 21 days post infection [71]. Though both CD4+ and CD8+ T cells act synergistically and play an indispensable role in both inflammatory responses and anti-viral immunity, they have been found to induce different profile of cytokines after hMPV infection [35]. During primary infection, depletion of either of the two T cell subsets, or in fact both of them, caused reduced inflammation and body weight loss in hMPV-infected mice but were required for viral clearance. These data suggest that primary hMPV infection induces lung disease mediated, in large extent, by T cells while T cells are also necessary for the clearance of primary hMPV infection [41]. Regarding the regulation of the T cell response during hMPV infection, a recent study by Hastings et al., showed that type I IFN signaling is essential for the development of functional hMPV specific CD8 T cells in the lungs using IFN-α receptor deficient C57BL/6 mice [53]. Moreover, in aged mice, CD4+T cells appear to play an important role in the exacerbated hMPV-induced disease. As demonstrated in 18-19 month-old BALB/c mice which showed a significant increased numbers of IL-4-producing CD4+ T cells but no change in the CD8+ T cell numbers when compared with younger mice [62], suggesting a Th2 skewing response in older mice after hMPV infection.
As for the role of T cells in hMPV reinfection, concurrent depletion of both CD4+ and CD8+ T cells led to a decreased airway hyperresponsiveness (AHR) [41]. However, depletion of CD4+ T cells alone during hMPV reinfection, unlike in CD8+ T cell-depleted mice, led to a defective antibody response. Nevertheless, CD4+ T cell-depleted mice had undetectable infectious virus after hMPV challenge and were protected from clinical disease, indicating that protection can be provided by an intact CD8+ T cell response [41]. Interestingly, recent observations indicate that the CD8+ T cell response is impaired during hMPV infection and reinfection and that phenomenon appears to be regulated by the expression of the inhibitor receptor programmed death-1 (PD-1) and programed death ligand-1 (PD-L1) [52,72,73]. These findings indicate that a defective CD8+T cell response contributes to hMPV reinfection. Whether this effect characterizes the commonly observed hMPV reinfection in humans warrants future research.
The understanding of the T cell response induced by hMPV vaccine candidates has found their initial steps using the mouse model. The induction of CD8+ cytotoxic T cells by peptide immunization in mice has proven to be protective against hMPV challenge in reducing viral load and lung histopathology [38]. Likewise, immunization with Bacillus Calmette-Guerin (BCG) strains expressing hMPV-phosphoprotein effectively induced a protective response which was mediated by a Th1 T cell response [42]. Immunization with hMPV F-bearing virus-like particles (VLP) was also able to stimulate an hMPV specific CD8+ T cell response and protected lungs from infection after hMPV challenge [50]. Further experimental studies in non-human primates and/or clinical trials are warranted in order to validate the immunological observations in the mouse model towards vaccine development.
4. Conclusions
The experimental mouse model represents a valuable tool for in vivo research on hMPV infection and has provided important information regarding the hMPV-induced disease and detailed aspects of the immune response induced by hMPV infection. Although, inherent limitations are observed in the mouse model when data are extrapolated to the natural human infection, due to the availability of several gene deficient mice strains and multiple murine specific antibodies, it provides a valued experimental small animal model that allows answering critical questions that are necessary to our better understanding of the immune response and disease pathogenesis of hMPV.
Acknowledgments
Research in Antonieta Guerrero-Plata’s laboratory has been supported by Grants from the National Center for Research Resources (P20RR020159-09), and the National Institute of General Medical Sciences (P20GM103458-09) from the National Institutes of Health, the LSU Competitive Organized Research program (LAV-3489), and the Louisiana Experimental Program from the National Science Foundation and Louisiana Board of Regents (41884).
Author Contributions
Antonieta Guerrero-Plata and Nagarjuna R. Cheemarla performed the literature research and wrote the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Feuillet F., Lina B., Rosa-Calatrava M., Boivin G. Ten years of human metapneumovirus research. J. Clin. Virol. 2012;53:97–105. doi: 10.1016/j.jcv.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Van den Hoogen B.G., de Jong J.C., Groen J., Kuiken T., de Groot R., Fouchier R.A., Osterhaus A.D. A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat. Med. 2001;7:719–724. doi: 10.1038/89098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boivin G., de Serres G., Cote S., Gilca R., Abed Y., Rochette L., Bergeron M.G., Dery P. Human metapneumovirus infections in hospitalized children. Emerg. Infect. Dis. 2003;9:634–640. doi: 10.3201/eid0906.030017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Caracciolo S., Minini C., Colombrita D., Rossi D., Miglietti N., Vettore E., Caruso A., Fiorentini S. Human metapneumovirus infection in young children hospitalized with acute respiratory tract disease: Virologic and clinical features. Pediatr. Infect. Dis. J. 2008;27:406–412. doi: 10.1097/INF.0b013e318162a164. [DOI] [PubMed] [Google Scholar]
- 5.Crowe J.E., Jr. Human metapneumovirus as a major cause of human respiratory tract disease. Pediatr. Infect. Dis. J. 2004;23:S215–S221. doi: 10.1097/01.inf.0000144668.81573.6d. [DOI] [PubMed] [Google Scholar]
- 6.Kahn J.S. Epidemiology of human metapneumovirus. Clin. Microbiol. Rev. 2006;19:546–557. doi: 10.1128/CMR.00014-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mullins J.A., Erdman D.D., Weinberg G.A., Edwards K., Hall C.B., Walker F.J., Iwane M., Anderson L.J. Human metapneumovirus infection among children hospitalized with acute respiratory illness. Emerg. Infect. Dis. 2004;10:700–705. doi: 10.3201/eid1004.030555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Esper F., Boucher D., Weibel C., Martinello R.A., Kahn J.S. Human metapneumovirus infection in the United States: Clinical manifestations associated with a newly emerging respiratory infection in children. Pediatrics. 2003;111:1407–1410. doi: 10.1542/peds.111.6.1407. [DOI] [PubMed] [Google Scholar]
- 9.Kahn J.S. Human metapneumovirus, a newly emerging respiratory virus. Pediatr. Infect. Dis. J. 2003;22:923–924. doi: 10.1097/01.inf.0000091347.27554.ff. [DOI] [PubMed] [Google Scholar]
- 10.Williams J.V., Wang C.K., Yang C.F., Tollefson S.J., House F.S., Heck J.M., Chu M., Brown J.B., Lintao L.D., Quinto J.D., et al. The role of human metapneumovirus in upper respiratory tract infections in children: A 20-year experience. J. Infect. Dis. 2006;193:387–395. doi: 10.1086/499274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Collins P.L., Crowe J. Respiratory Syncytial Virus and Metapneumovirus. In: Knipe D.M., Howley P.M., editors. Fileds Virology. 5th ed. Volume 2. Wolters Kluwer; Philadelphia, PA, USA: 2007. pp. 1601–1646. [Google Scholar]
- 12.Van den Hoogen B.G., Herfst S., Sprong L., Cane P.A., Forleo-Neto E., de Swart R.L., Osterhaus A.D., Fouchier R.A. Antigenic and genetic variability of human metapneumoviruses. Emerg. Infect. Dis. 2004;10:658–666. doi: 10.3201/eid1004.030393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Biacchesi S., Skiadopoulos M.H., Boivin G., Hanson C.T., Murphy B.R., Collins P.L., Buchholz U.J. Genetic diversity between human metapneumovirus subgroups. Virology. 2003;315:1–9. doi: 10.1016/S0042-6822(03)00528-2. [DOI] [PubMed] [Google Scholar]
- 14.Mackay I.M., Jacob K.C., Woolhouse D., Waller K., Syrmis M.W., Whiley D.M., Siebert D.J., Nissen M., Sloots T.P. Molecular assays for detection of human metapneumovirus. J. Clin. Microbiol. 2003;41:100–105. doi: 10.1128/JCM.41.1.100-105.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Easton A.J., Domachowske J.B., Rosenberg H.F. Animal pneumoviruses: Molecular genetics and pathogenesis. Clin. Microbiol. Rev. 2004;17:390–412. doi: 10.1128/CMR.17.2.390-412.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamelin M.E., Yim K., Kuhn K.H., Cragin R.P., Boukhvalova M., Blanco J.C., Prince G.A., Boivin G. Pathogenesis of human metapneumovirus lung infection in BALB/c mice and cotton rats. J. Virol. 2005;79:8894–8903. doi: 10.1128/JVI.79.14.8894-8903.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mok H., Tollefson S.J., Podsiad A.B., Shepherd B.E., Polosukhin V.V., Johnston R.E., Williams J.V., Crowe J.E., Jr. An alphavirus replicon-based human metapneumovirus vaccine is immunogenic and protective in mice and cotton rats. J. Virol. 2008;82:11410–11418. doi: 10.1128/JVI.01688-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Green M.G., Huey D., Niewiesk S. The cotton rat (Sigmodon hispidus) as an animal model for respiratory tract infections with human pathogens. Lab Animal. 2013;42:170–176. doi: 10.1038/laban.188. [DOI] [PubMed] [Google Scholar]
- 19.Boukhvalova M.S., Prince G.A., Blanco J.C. The cotton rat model of respiratory viral infections. Biologicals. 2009;37:152–159. doi: 10.1016/j.biologicals.2009.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MacPhail M., Schickli J.H., Tang R.S., Kaur J., Robinson C., Fouchier R.A., Osterhaus A.D., Spaete R.R., Haller A.A. Identification of small-animal and primate models for evaluation of vaccine candidates for human metapneumovirus (hMPV) and implications for hMPV vaccine design. J. Gen. Virol. 2004;85:1655–1663. doi: 10.1099/vir.0.79805-0. [DOI] [PubMed] [Google Scholar]
- 21.Herfst S., de Graaf M., Schrauwen E.J., Sprong L., Hussain K., van den Hoogen B.G., Osterhaus A.D., Fouchier R.A. Generation of temperature-sensitive human metapneumovirus strains that provide protective immunity in hamsters. J. Gen. Virol. 2008;89:1553–1562. doi: 10.1099/vir.0.2008/002022-0. [DOI] [PubMed] [Google Scholar]
- 22.Schickli J.H., Kaur J., Macphail M., Guzzetta J.M., Spaete R.R., Tang R.S. Deletion of human metapneumovirus M2-2 increases mutation frequency and attenuates growth in hamsters. Virol. J. 2008 doi: 10.1186/1743-422X-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Biacchesi S., Pham Q.N., Skiadopoulos M.H., Murphy B.R., Collins P.L., Buchholz U.J. Infection of nonhuman primates with recombinant human metapneumovirus lacking the SH, G, or M2-2 protein categorizes each as a nonessential accessory protein and identifies vaccine candidates. J. Virol. 2005;79:12608–12613. doi: 10.1128/JVI.79.19.12608-12613.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Biacchesi S., Pham Q.N., Skiadopoulos M.H., Murphy B.R., Collins P.L., Buchholz U.J. Modification of the trypsin-dependent cleavage activation site of the human metapneumovirus fusion protein to be trypsin independent does not increase replication or spread in rodents or nonhuman primates. J. Virol. 2006;80:5798–5806. doi: 10.1128/JVI.00294-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Darniot M., Petrella T., Aho S., Pothier P., Manoha C. Immune response and alteration of pulmonary function after primary human metapneumovirus (hMPV) infection of BALB/c mice. Vaccine. 2005;23:4473–4480. doi: 10.1016/j.vaccine.2005.04.027. [DOI] [PubMed] [Google Scholar]
- 26.Kukavica-Ibrulj I., Hamelin M.E., Prince G.A., Gagnon C., Bergeron Y., Bergeron M.G., Boivin G. Infection with human metapneumovirus predisposes mice to severe pneumococcal pneumonia. J. Virol. 2009;83:1341–1349. doi: 10.1128/JVI.01123-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hamelin M.E., Prince G.A., Boivin G. Effect of ribavirin and glucocorticoid treatment in a mouse model of human metapneumovirus infection. Antimicrob. Agents Chemother. 2006;50:774–777. doi: 10.1128/AAC.50.2.774-777.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hamelin M.E., Couture C., Sackett M.K., Boivin G. Enhanced lung disease and Th2 response following human metapneumovirus infection in mice immunized with the inactivated virus. J. Gen. Virol. 2007;88:3391–3400. doi: 10.1099/vir.0.83250-0. [DOI] [PubMed] [Google Scholar]
- 29.Levy C., Aerts L., Hamelin M.E., Granier C., Szecsi J., Lavillette D., Boivin G., Cosset F.L. Virus-like particle vaccine induces cross-protection against human metapneumovirus infections in mice. Vaccine. 2013;31:2778–2785. doi: 10.1016/j.vaccine.2013.03.051. [DOI] [PubMed] [Google Scholar]
- 30.Hamelin M.E., Prince G.A., Gomez A.M., Kinkead R., Boivin G. Human metapneumovirus infection induces long-term pulmonary inflammation associated with airway obstruction and hyperresponsiveness in mice. J. Infect. Dis. 2006;193:1634–1642. doi: 10.1086/504262. [DOI] [PubMed] [Google Scholar]
- 31.Ludewick H.P., Aerts L., Hamelin M.E., Boivin G. Long-term impairment of Streptococcus pneumoniae lung clearance is observed after initial infection with influenza A virus but not human metapneumovirus in mice. J. Gen. Virol. 2011;92:1662–1665. doi: 10.1099/vir.0.030825-0. [DOI] [PubMed] [Google Scholar]
- 32.Aerts L., Hamelin M.E., Rheaume C., Lavigne S., Couture C., Kim W., Susan-Resiga D., Prat A., Seidah N.G., Vergnolle N., et al. Modulation of protease activated receptor 1 influences human metapneumovirus disease severity in a mouse model. PLoS ONE. 2013 doi: 10.1371/journal.pone.0072529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Darniot M., Schildgen V., Schildgen O., Sproat B., Kleines M., Ditt V., Pitoiset C., Pothier P., Manoha C. RNA interference in vitro and in vivo using DsiRNA targeting the nucleocapsid N mRNA of human metapneumovirus. Antiviral Res. 2012;93:364–373. doi: 10.1016/j.antiviral.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 34.Alvarez R., Harrod K.S., Shieh W.J., Zaki S., Tripp R.A. Human metapneumovirus persists in BALB/c mice despite the presence of neutralizing antibodies. J. Virol. 2004;78:14003–14011. doi: 10.1128/JVI.78.24.14003-14011.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alvarez R., Tripp R.A. The immune response to human metapneumovirus is associated with aberrant immunity and impaired virus clearance in BALB/c mice. J. Virol. 2005;79:5971–5978. doi: 10.1128/JVI.79.10.5971-5978.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu P., Shu Z., Qin X., Dou Y., Zhao Y., Zhao X. A live attenuated human metapneumovirus vaccine strain provides complete protection against homologous viral infection and cross-protection against heterologous viral infection in BALB/c mice. Clin. Vaccine Immunol. 2013;20:1246–1254. doi: 10.1128/CVI.00145-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guerrero-Plata A., Casola A., Garofalo R.P. Human metapneumovirus induces a profile of lung cytokines distinct from that of respiratory syncytial virus. J. Virol. 2005;79:14992–14997. doi: 10.1128/JVI.79.23.14992-14997.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Herd K.A., Mahalingam S., Mackay I.M., Nissen M., Sloots T.P., Tindle R.W. Cytotoxic T-lymphocyte epitope vaccination protects against human metapneumovirus infection and disease in mice. J. Virol. 2006;80:2034–2044. doi: 10.1128/JVI.80.4.2034-2044.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Guerrero-Plata A., Baron S., Poast J.S., Adegboyega P.A., Casola A., Garofalo R.P. Activity and regulation of alpha interferon in respiratory syncytial virus and human metapneumovirus experimental infections. J. Virol. 2005;79:10190–10199. doi: 10.1128/JVI.79.16.10190-10199.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guerrero-Plata A., Kolli D., Hong C., Casola A., Garofalo R.P. Subversion of pulmonary dendritic cell function by paramyxovirus infections. J. Immunol. 2009;182:3072–3083. doi: 10.4049/jimmunol.0802262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kolli D., Bataki E.L., Spetch L., Guerrero-Plata A., Jewell A.M., Piedra P.A., Milligan G.N., Garofalo R.P., Casola A. T lymphocytes contribute to antiviral immunity and pathogenesis in experimental human metapneumovirus infection. J. Virol. 2008;82:8560–8569. doi: 10.1128/JVI.00699-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Palavecino C.E., Cespedes P.F., Gomez R.S., Kalergis A.M., Bueno S.M. Immunization with a recombinant bacillus Calmette-Guerin strain confers protective Th1 immunity against the human metapneumovirus. J. Immunol. 2014;192:214–223. doi: 10.4049/jimmunol.1300118. [DOI] [PubMed] [Google Scholar]
- 43.Ditt V., Lusebrink J., Tillmann R.L., Schildgen V., Schildgen O. Respiratory infections by HMPV and RSV are clinically indistinguishable but induce different host response in aged individuals. PLoS ONE. 2011 doi: 10.1371/journal.pone.0016314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Huck B., Neumann-Haefelin D., Schmitt-Graeff A., Weckmann M., Mattes J., Ehl S., Falcone V. Human metapneumovirus induces more severe disease and stronger innate immune response in BALB/c mice as compared with respiratory syncytial virus. Respir. Res. 2007 doi: 10.1186/1465-9921-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Banos-Lara Mdel R., Ghosh A., Guerrero-Plata A. Critical role of MDA5 in the interferon response induced by human metapneumovirus infection in dendritic cells and in vivo. J. Virol. 2013;87:1242–1251. doi: 10.1128/JVI.01213-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chakraborty K., Zhou Z., Wakamatsu N., Guerrero-Plata A. Interleukin-12p40 modulates human metapneumovirus-induced pulmonary disease in an acute mouse model of infection. PLoS ONE. 2012 doi: 10.1371/journal.pone.0037173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ren J., Kolli D., Deng J., Fang R., Gong B., Xue M., Casola A., Garofalo R.P., Wang T., Bao X. MyD88 controls human metapneumovirus-induced pulmonary immune responses and disease pathogenesis. Virus Res. 2013;176:241–250. doi: 10.1016/j.virusres.2013.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Velayutham T.S., Kolli D., Ivanciuc T., Garofalo R.P., Casola A. Critical role of TLR4 in human metapneumovirus mediated innate immune responses and disease pathogenesis. PLoS ONE. 2013 doi: 10.1371/journal.pone.0078849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Banos-Lara Mdel R., Harvey L., Mendoza A., Simms D., Chouljenko V.N., Wakamatsu N., Kousoulas K.G., Guerrero-Plata A. Impact and regulation of lambda interferon response in human metapneumovirus infection. J. Virol. 2015;89:730–742. doi: 10.1128/JVI.02897-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cox R.G., Erickson J.J., Hastings A.K., Becker J.C., Johnson M., Craven R.E., Tollefson S.J., Boyd K.L., Williams J.V. Human metapneumovirus virus-like particles induce protective B and T cell responses in a mouse model. J. Virol. 2014;88:6368–6379. doi: 10.1128/JVI.00332-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wen S.C., Tollefson S.J., Johnson M., Gilchuk P., Boyd K.L., Shepherd B., Joyce S., Williams J.V. Acute clearance of human metapneumovirus occurs independently of natural killer cells. J. Virol. 2014;88:10963–10969. doi: 10.1128/JVI.01558-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Erickson J.J., Rogers M.C., Hastings A.K., Tollefson S.J., Williams J.V. Programmed death-1 impairs secondary effector lung CD8(+) T cells during respiratory virus reinfection. J. Immunol. 2014;193:5108–5117. doi: 10.4049/jimmunol.1302208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hastings A.K., Erickson J.J., Schuster J.E., Boyd K.L., Tollefson S.J., Johnson M., Gilchuk P., Joyce S., Williams J.V. Role of type I interferon signaling in human metapneumovirus pathogenesis and control of viral replication. J. Virol. 2015;89:4405–4420. doi: 10.1128/JVI.03275-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yu C.M., Li R.P., Chen X., Liu P., Zhao X.D. Replication and pathogenicity of attenuated human metapneumovirus F mutants in severe combined immunodeficiency mice. Vaccine. 2012;30:231–236. doi: 10.1016/j.vaccine.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 55.Zhang J., Dou Y., Wu J., She W., Luo L., Zhao Y., Liu P., Zhao X. Effects of N-linked glycosylation of the fusion protein on replication of human metapneumovirus in vitro and in mouse lungs. J. Gen. Virol. 2011;92:1666–1675. doi: 10.1099/vir.0.030049-0. [DOI] [PubMed] [Google Scholar]
- 56.Akira S., Uematsu S., Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006;124:783–801. doi: 10.1016/j.cell.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 57.Reikine S., Nguyen J.B., Modis Y. Pattern Recognition and Signaling Mechanisms of RIG-I and MDA5. Front. Immunol. 2014 doi: 10.3389/fimmu.2014.00342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Spann K.M., Loh Z., Lynch J.P., Ullah A., Zhang V., Baturcam E., Werder R.B., Khajornjiraphan N., Rudd P., Loo Y.M., et al. IRF-3, IRF-7, and IPS-1 promote host defense against acute human metapneumovirus infection in neonatal mice. Am. J. Pathol. 2014;184:1795–1806. doi: 10.1016/j.ajpath.2014.02.026. [DOI] [PubMed] [Google Scholar]
- 59.Deng J., Chen Y., Liu G., Ren J., Go C., Ivanciuc T., Deepthi K., Casola A., Garofalo R.P., Bao X. MAVS plays an essential role in host immunity against human metapneumovirus. J. Gen. Virol. 2015 doi: 10.1099/vir.0.000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Laham F.R., Israele V., Casellas J.M., Garcia A.M., Lac Prugent C.M., Hoffman S.J., Hauer D., Thumar B., Name M.I., Pascual A., et al. Differential production of inflammatory cytokines in primary infection with human metapneumovirus and with other common respiratory viruses of infancy. J. Infect. Dis. 2004;189:2047–2056. doi: 10.1086/383350. [DOI] [PubMed] [Google Scholar]
- 61.Aherne W., Bird T., Court S.D., Gardner P.S., McQuillin J. Pathological changes in virus infections of the lower respiratory tract in children. J. Clin. Pathol. 1970;23:7–18. doi: 10.1136/jcp.23.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Darniot M., Pitoiset C., Petrella T., Aho S., Pothier P., Manoha C. Age-associated aggravation of clinical disease after primary metapneumovirus infection of BALB/c mice. J. Virol. 2009;83:3323–3332. doi: 10.1128/JVI.02198-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Stumbles P.A., Upham J.W., Holt P.G. Airway dendritic cells: Co-ordinators of immunological homeostasis and immunity in the respiratory tract. APMIS. 2003;111:741–755. doi: 10.1034/j.1600-0463.2003.11107806.x. [DOI] [PubMed] [Google Scholar]
- 64.Guerrero-Plata A., Casola A., Suarez G., Yu X., Spetch L., Peeples M.E., Garofalo R.P. Differential response of dendritic cells to human metapneumovirus and respiratory syncytial virus. Am. J. Respir. Cell Mol. Biol. 2006;34:320–329. doi: 10.1165/rcmb.2005-0287OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Guerrero-Plata A. Dendritic cells in human Pneumovirus and Metapneumovirus infections. Viruses. 2013;5:1553–1570. doi: 10.3390/v5061553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Le Nouen C., Munir S., Losq S., Winter C.C., McCarty T., Stephany D.A., Holmes K.L., Bukreyev A., Rabin R.L., Collins P.L., et al. Infection and maturation of monocyte-derived human dendritic cells by human respiratory syncytial virus, human metapneumovirus, and human parainfluenza virus type 3. Virology. 2009;385:169–182. doi: 10.1016/j.virol.2008.11.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pribul P.K., Harker J., Wang B., Wang H., Tregoning J.S., Schwarze J., Openshaw P.J. Alveolar macrophages are a major determinant of early responses to viral lung infection but do not influence subsequent disease development. J. Virol. 2008;82:4441–4448. doi: 10.1128/JVI.02541-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lohmann-Matthes M.L., Steinmuller C., Franke-Ullmann G. Pulmonary macrophages. Eur. Respir. J. 1994;7:1678–1689. doi: 10.1183/09031936.94.07091678. [DOI] [PubMed] [Google Scholar]
- 69.Kolli D., Gupta M.R., Sbrana E., Velayutham T.S., Hong C., Casola A., Garofalo R.P. Alveolar Macrophages Contribute to the Pathogenesis of hMPV Infection While Protecting Against RSV Infection. Am. J. Respir. Cell Mol. Biol. 2014;51:502–515. doi: 10.1165/rcmb.2013-0414OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Benoit A., Huang Y., Proctor J., Rowden G., Anderson R. Effects of alveolar macrophage depletion on liposomal vaccine protection against respiratory syncytial virus (RSV) Clin. Exp. Immunol. 2006;145:147–154. doi: 10.1111/j.1365-2249.2006.03114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Herd K.A., Nelson M., Mahalingam S., Tindle R.W. Pulmonary infection of mice with human metapneumovirus induces local cytotoxic T-cell and immunoregulatory cytokine responses similar to those seen with human respiratory syncytial virus. J. Gen. Virol. 2010;91:1302–1310. doi: 10.1099/vir.0.015396-0. [DOI] [PubMed] [Google Scholar]
- 72.Erickson J.J., Gilchuk P., Hastings A.K., Tollefson S.J., Johnson M., Downing M.B., Boyd K.L., Johnson J.E., Kim A.S., Joyce S., et al. Viral acute lower respiratory infections impair CD8+ T cells through PD-1. J. Clin. Investig. 2012;122:2967–2982. doi: 10.1172/JCI62860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wen S.C., Schuster J.E., Gilchuk P., Boyd K.L., Joyce S., Williams J.V. Lung CD8+ T cell impairment occurs during human metapneumovirus infection despite Virus-Like Particle (VLP) induction of functional CD8+ T cells. J. Virol. 2015;89:8713–8726. doi: 10.1128/JVI.00670-15. [DOI] [PMC free article] [PubMed] [Google Scholar]