Abstract
This report provides a primer for implementing interprofessional education (IPE) within pharmacy and health sciences curricula. In 2013, a panel of administrators and faculty members, whose institutions offered IPE, funded by the Josiah Macy Jr. Foundation, shared best collaborative practice models at the American Association of Colleges of Pharmacy (AACP) Annual Meeting. These presenters subsequently collaborated to write a primer as guidance for other institutions interested in successfully implementing and continuously enhancing the quality of IPE programs. In this article, these IPE faculty members provide a rationale for creating IPE reforms, discuss successful strategies for innovative IPE programs, and share lessons learned for implementing effective assessment tools. A structure and process for determining outcomes of IPE models are presented and strategies for exploring shared education opportunities across health professions and for integrating top-down and bottom-up methods for IPE programs are given.
Keywords: Interprofessional education, pharmacy education, curriculum, interdisciplinary health team, experiential learning
INTRODUCTION
The Institute of Medicine (IOM) released several reports on health care services and the education of professionals in the United States. The reports emphasize the need for substantial change in the delivery of services and education consistent with the needed redesign of the health care system.1,2-In 2010, 2 reports were released that sparked international discussion about needed reforms in health education and a call for producing health professionals who are ready to provide patient-centered, interprofessional, team-based care. The first report, from a global, independent commission on health professional education, called for transformational change in health professions education.3 The commission set forth the case for integrating a systems approach into educational reforms in medicine as well as in health care as a whole. The second report, from the World Health Organization (WHO), presented a framework for implementing IPE and collaborative practice.4 This report defined IPE as students from 2 or more professions learning about, from, and with each other to enable effective collaboration and improve health outcomes. The report also explained how changes in health education can facilitate redesigning the health care system. While efforts to promote IPE have existed for more than 20 years, these reports prompted renewed vigor and motivation for major changes in health professions education worldwide.
In 2011, the Interprofessional Education Collaborative (IPEC) published the Core Competencies for Interprofessional Collaborative Practice, based on work by WHO and sponsored by professional education associations in medicine, nursing, pharmacy, dentistry, and public health.5 The report provided operational definitions for interprofessional collaborative practice, interprofessional teamwork, and interprofessional team-based care. It outlined 4 competency domains: (1) values/ethics of interprofessional practice; (2) roles and responsibilities; (3) interprofessional communication; and (4) teams and teamwork. It also included a set of 38 competency statements describing knowledge, skills, and attitudes necessary for demonstrating interprofessionalism. The IPEC report urged educators to prepare health professions students to work together, with a common goal of building a safer and better patient-centered, population-oriented health care system.
When the Accreditation Council for Pharmacy Education (ACPE) published a draft of the new 2016 Standards,6 the WHO definition for IPE and the 4 IPEC domains were adopted into the mandate for integrating interprofessional collaborative practice into pharmacy curricula. As reform develops, the scope of pharmacy practice changes, and new educational standards are implemented, future pharmacy practice models will likely include interprofessional teams to improve patient outcomes. Consequently, pharmacy programs nationwide are embarking on dynamic changes to integrate IPE throughout the didactic and experiential portions of the curriculum.
Despite this mandate, no published evidence exists of an institution fully implementing a curriculum that builds student competency in interprofessional teamwork and collaborative practice from the first to the last year of education. Many curricula now have experience with IPE activities, simulations, courses, and experiences, but no one has published evidence for success in implementing a well-designed, deliberate, and longitudinal curriculum for IPE that assures all students reach stated outcomes.
The main purpose of this article is to provide colleges and schools of pharmacy with strategies for developing and successfully implementing an IPE curriculum. Through description of practical experiences, this primer emphasizes essential tools for IPE interventions, identifies potential challenges, and discusses effective assessment tools for educational outcomes. Development of this primer resulted from collaboration among members of a panel that presented a platform on innovative IPE curriculum and collaborative practice models to the Curriculum Special Interest Group (SIG) at the 2013 American Association of Colleges of Pharmacy (AACP) Annual Meeting in Chicago. The panel members represented institutions that successfully received external funding in support of IPE programs from the Josiah Macy Jr. Foundation, which seeks to advance education and training of health care professionals through interprofessional education and teamwork, new curriculum content, new models for clinical education, education for the care of underserved populations, and career development in health professions education.
DESIGNING AND IMPLEMENTING AN IPE CURRICULUM
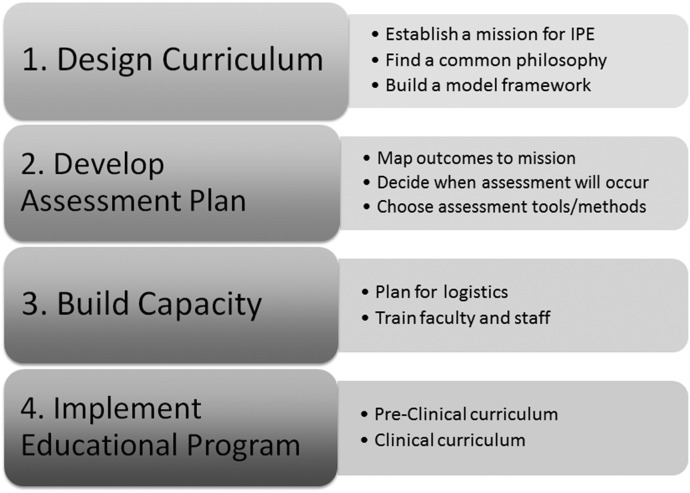
Building an IPE curriculum across multiple professions involves creating common educational outcomes so that the same goals are kept in mind during curriculum development. The ultimate goal is to improve patient-care outcomes, but initial efforts may aim to change attitudes, knowledge, and behaviors as intermediate markers for learning and competency attainment. Blending educational outcomes of multiple health professions programs into a single congruent statement is an exercise in consensus building that can reveal differing agendas each profession brings. An overview of the approach for designing, building, and assessing an IPE curriculum is presented in Figure 1.
Figure 1.
Steps for Implementing an Interprofessional Curriculam.
Choice of curriculum design and assessment methods should depend on the stated aims. Ideally, outcomes should be outlined at the outset, inclusive of an assessment plan to measure their achievement. A curriculum can then be built to meet them. However, programs can also experiment with small changes first to determine effectiveness and work out the logistical difficulties encountered when building an interprofessional environment. A staged approach for planning and execution follows, which includes 3 key steps.
Establish a mission for IPE.
Whether a school collaborates within the institution (eg, an academic health center) or identifies partners in the surrounding region, the first step to developing an IPE curriculum is to establish a common mission across the professional schools/programs involved. Achieving consensus about the direction for collaboration and establishing mutual goals are essential.7 Examples of mission statements include this one from the University of Washington Health Sciences: “To advance the health of individuals and communities by integrating and transforming the learning experience across the university’s six health sciences schools – Dentistry, Medicine, Nursing, Pharmacy, Public Health and Social Work.” Another example is from the University of Colorado Anschutz Medical Campus: “To improve population health, quality of care, and reduce health care costs through the creation of a patient-centered, collaborative practice ready work force with competencies in: quality and safety, values and ethics, teamwork and collaboration, in the context of systems and systems-based practice.”
Find a common philosophy.
The underlying motivation for implementing IPE may be different for an individual program vs the partnerships among programs. For example, some programs seek to meet accreditation standards that mandate IPE, while others want to fundamentally change health professions education. Therefore, the scope of changes made could differ based on these different views of the purpose of IPE. As outlined by WHO and IOM, the goal of IPE is to improve patient safety and outcomes through IPE. However, others view IPE as a means of aligning professions in patient-care decision-making and may even use it to advocate for their profession’s scope of practice.8 Competing intentions should be recognized and discussed thoughtfully.
An important starting point is to seek understanding of each participant. Reviewing each program’s curriculum is time well spent. Students in different health profession programs develop clinical competency and professional identity at different rates. Because various programs differ in length and organization, students’ knowledge, skills, and abilities will grow in different areas at different times. Understanding where the overlaps and gaps are between professions is important to understand.
One philosophy for building an IPE curriculum is that interprofessional learning is best situated within the context of uniprofessional content—simply make what the student is already learning an interprofessional activity. However, experience at the University of Washington School of Pharmacy proved that the practical application of this philosophy was not always possible. Integrating IPE into other coursework was challenging because IPE activities were so new that they were often changed, improved, or dropped. This evolving nature of new IPE content became cumbersome to integrate into other courses. Therefore, a separate curriculum thread (course series) was developed.
At Thomas Jefferson University, a 2-year longitudinal IPE endeavor was integrated into existing coursework for pharmacy, medicine, nursing, occupational therapy, and physical therapy. Moreover, the University of Colorado has had more than 15 years of experience with a free-standing interprofessional ethics course upon which to build its interprofessional framework.
Build a model framework.
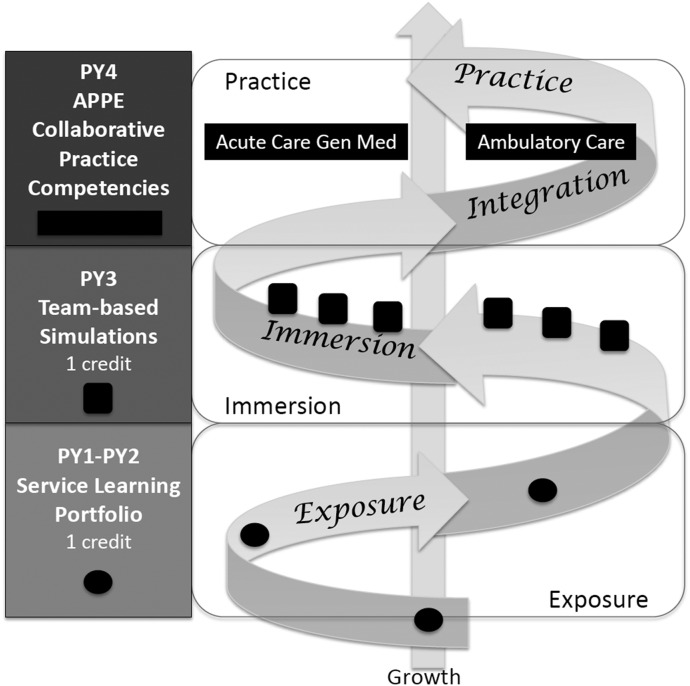
Determining a common philosophy about IPE lays the groundwork for curriculum design. A curricular and theoretical framework that expresses the common philosophy can guide the development of a curricular structure and course offerings. Theories differ among faculty members teaching IPE, which results in the use of different teaching methods. For example, service learning, didactic coursework, simulation, and even clinical practice placements have different purposes and different learning theories that underpin them. Graphics are particularly useful for helping faculty members and students visualize a curricular and theoretical framework.9-14 (Figure 2)
Figure 2.
Longitudinal Curricular Framework for Interprofessional Education.
As discussions about a framework occur, important questions can emerge: (1) What health professions are involved or available for inclusion? (2) Will coursework be structured, a core series set aside as IPE, or will learning activities be integrated into other coursework? (3) Will IPE learning activities occur for all students simultaneously, or will students be allowed to gather experiences over time based on choice? (4) Will all students take the course at the same time? (5) Is there adequate space to accommodate all students? (6) Which instructors from which programs will be involved in developing course content? Given these questions, a tremendous diversity of IPE programs among schools of pharmacy can be developed and implemented. Thus, each university or group of universities working together to implement IPE should develop its own mission, philosophy, and framework that fits the students and trainees involved.
For example, the current curricular framework for the University of Washington School of Pharmacy depicts an IPE curricular thread, some of which exists as standalone credits. Plans for exposure to other professionals span the first 2 years via a menu-driven approach. Immersion is conducted in the third year with specially designed activities and simulations that require students to make shared decisions and operate as teams. Collaborative practice occurs in the fourth year in selected advanced pharmacy practice experiences (APPEs) that will be designated as interprofessional experiences.
DEVELOPING AN IPE ASSESSMENT PLAN
A comprehensive IPE assessment plan ensures the mission, goals, and educational outcomes of IPE programming are met. Prior to implementing the IPE models, assessment plans must be implemented as they are critical for guiding continuous quality improvement of current and future programming. The importance of keeping the end product in mind cannot be overstated.
An assessment plan should be developed as the IPE curriculum is being created to help ensure a link between the mission, goals, educational outcomes, and the assessment tools. Including all participating professions in creating the assessment plan is highly desirable so that the common interests are included in the conversations. The assessment outcomes can be applicable in different ways to each program (ie, for accreditation purposes or programmatic continuous quality improvement). An assessment committee, inclusive of all professions, can assist in formalizing the plan and in creating accountability for execution of the plan.
Numerous quantitative instruments are available, as are a growing number of resources from which to select evaluation tools.15-17 Several publications examine the development of assessments with regard to the broad outcomes of IPE programs as students prepare to graduate and enter practice.16,18-23 Examples include the validation of the interprofessional collaborative competency attainment survey (ICCAS) and the exploration of a tool derived from the IPE Core Competencies.18,19 The Student Perceptions of Physician-Pharmacist Interprofessional Clinical Education (SPICE) instrument was developed by physicians and pharmacists to assess students participating in an interprofessional clinic. It was deemed useful for identifying differences in students’ self-perception following interprofessional education experiences and has been compared against other instruments.20,21 The creators of this tool found that the assessment of roles and responsibilities had the lowest reliability for the SPICE instrument, indicating that it remains a challenging domain to assess. The CATS tool was developed to assess knowledge of the professional roles of others as a component of team communication, function, and leadership.24 This instrument is used to assess interprofessional communication, function and performance among student teams in APPEs.25
Overassessment of IPE programs and participants should be avoided. When developing a new IPE programs, a desire to collect a wide range of data is common. Two assessment plan development tips can help educators avoid this. Select only tools that link to the program mission, goals, and educational outcomes, and choose no more than 2 validated instruments. This approach can help teaching teams avoid assessment burnout that could negatively affect reliable data collection.
To date, assessment studies mainly focus on student attitudes toward and readiness for IPE and their achievement of individual IPE activity goals, specifically knowledge and skills. For future research, issues to address for examining additional educational outcomes are what impact IPE has on student performance and ability to deliver collaborative care during experiential education and how students trained in IPE will affect patient care compared to those who did not receive IPE training upon graduation and entry into the work force. Realistically, mixed-method assessment will likely be necessary to provide longitudinal evidence of change in practice and long-term benefits of IPE. Ultimately, assessment tools will need to evaluate whether the students involved in these programs are meeting the IPE Core Competencies and collaborating to redesign the health care system.
Institutions should strive to develop an overall assessment map of their IPE programs to evaluate which IPE competencies are met by each program and to what extent. An example map may include a cross-referencing of the IPE programs, the IPE competencies addressed by each program and the assessment tool(s) used in evaluating the ability of the programs (and the students, individually and/or in aggregate) to achieve the competencies.
At Thomas Jefferson University School of Pharmacy, a process was adopted where members of the IPE curriculum committee, representing all health care professions, identified which specific IPEC competencies to focus on in IPE initiatives. These global competencies related to the overall mission, negating the need to re-evaluate the mission at that time. A grid was developed to highlight which outcomes were being addressed and how they were evaluated for each IPE program. The grid also allowed the institution to identify competencies linked to overassessment or underassessment of students’ performance. According to the grid, in first 2 years of the IPE program, too many tools were used. Therefore, the assessment plan was adjusted to include only 2 validated tools that do not overlap. Also, various assessment tools were distributed to different student cohorts if the total number of participating students was large enough to produce reliable and valid data. The University of Colorado chose the CATME tool, a comprehensive assessment of team member effectiveness and behaviorally anchored rating scale for self- and peer-evaluation.23 This assessment tool set expectations and provided students feedback on their performance during the didactic and clinical interprofessional settings.
IMPLEMENTING IPE INTERVENTIONS
A dynamic and comprehensive curriculum involves multiple interventions and instructional strategies. For example, IPE is suitable for simulation learning, which according to ACPE can account for up to 20% of IPPE hours.6 Students need to understand the relevance of the IPE activities to pharmacy practice rather than merely learning how to “get along” with other professionals. Each school of pharmacy must determine the best approach to take based on its own culture and existing preclinical and clinical curricular structure.
Pre-clinical interventions.
According to the IOM reports, traditional educational models for professional programs trained each member of the health care team in isolation from each other. Once graduated, these professionals entered clinical settings uncertain how each team member contributed to patient care. However, society increasingly expects each team will work together to promote patient welfare.2 When a health care team fails to treat patients with respect, combine knowledge to improve outcomes, or use health care resources wisely, patients can suffer. These messages need to be communicated to students as they begin their preclinical interprofessional education. Providing clinical context exposes students in the didactic environment to the foundational knowledge behind each of the IPEC domains. While the best approach for teaching the IPEC core competencies has yet to be elucidated, a few examples follow of foundational knowledge building for each of the IPEC core domains.
Ethics of interprofessional practice can be an easy place to start because ethics and professional development occur in all curricula and are taught at a basic level, so aligning ethics coursework among professions is not necessary. In addition, ethics is already taught in each curriculum, so extra time is not needed for its instruction.
The University of Colorado provides IPE education early in the PharmD program as a 4-hour IPE orientation to first-year students, during which instructors discuss the importance of interprofessional collaboration for improved health care and explain the rationale of IPE for creating collaborative health care teams. In addition, students are introduced to their interprofessional teammates, who they will work with for the next 15 months. Students are encouraged to stay connected to team members and use each other as resources as they progress through their respective curricula.
Roles and responsibilities can be addressed early in the health professions education.26-28 For example, Van Winkle et al’s IPE study provided medical and pharmacy students an interprofessional workshop in the first years of their respective curricula and assessed student perception of interprofessional collaboration.28 The workshop assessed how the teams reflected upon the roles of each profession in the care of patients. Based on an analysis of preworkshop and postworkshop scores on a collaborative survey instrument, the authors found that the workshop fostered interprofessional collaboration, although the change in the scores varied among students.
Again, at the University of Colorado, an interprofessional course started as a series of small group discussions focused on ethics has evolved into 16 sessions covering the topics of teamwork and collaboration, quality and safety, and ethics and values given over 2 semesters. Prior to orientation, students’ attitudes about each profession’s roles are collected using items from the Role Perception Questionnaire.18 Stereotypes of each profession are then identified and discussed with students during the IPE courses.
Watt-Watson and colleagues developed a 5-day, 20-hour interprofessional pain curriculum for dentistry, medicine, pharmacy, nursing, physical therapy, and occupational therapy students.29 The 20 hours consisted of pretesting and posttesting, lectures, discussions, and work in small groups. Through voluntary daily questionnaires, the authors determined that student learning of the pain topic did occur. Feedback from the students indicated the content of the cases isolated some of the professions (dentistry, occupational and physical therapy) and was taught at a level that was either too easy or too hard for some professions. However, students did ask for more information about the roles and responsibilities of the professions in solving the cases.
Interprofessional communication.
Educators recognize the importance of effective communication for successfully implementing IPE programs.30-34 For example, Dow et al used a quality improvement case to address student ability to work as a team and collaborate interprofessionally.19 Students were provided with specific quality improvement cases in their individual curricula, and given time for interprofessional group work to complete assignments. Students self-reported a significant increase in their ability to communicate and cooperate with others and their ability to identify with their team.30 Marken et al used simulation with 12 students to demonstrate competence while functioning as a member of an interprofessional team engaged in difficult conversations.34 The 2-day, 4-hour events started with a 20-minute discussion of difficult topics, followed by multiple simulated scenarios, debriefs, and discussions on roles. Faculty members used a rubric to assess and debrief students on their ability to engage in difficult conversations. Participants demonstrated skills and gained confidence in dealing with difficult patient situations.
The University of Washington Health Sciences is a recognized national training site for TeamSTEPPS, a teamwork system designed for health professionals that improves communication and teamwork to improve patient safety.20 Training in this set of team communication skills is taught and emphasized in simulations as part of the IPE initiatives at the university. This simulation training demonstrated significant changes in team communication, motivation, utility of training, and self-efficacy. Some attitudinal and knowledge shifts also were seen about the TeamSTEPPS skills, which suggests that this team communication training is a useful tool for providing interprofessional education.21
At the University of Colorado, an interprofessional ethics course across multiple professions has been taught for the past decade.27 In the early years of the ethics course, many lessons were learned: (1) conversion of one profession’s ethics course to an interprofessional course left many faculty struggling to make the change; (2) one profession outnumbered the others and, as such, these students felt more comfortable participating in group discussions; and (3) early evaluations indicated that 35% stated the course was too focused on interprofessional health care, but recent evaluations of the course indicated that the interprofessional focus was the students’ favorite aspect of the course.
Teams and teamwork.
In addition to activities conducted by teams, simulation can be used to provide students with opportunities to model appropriate interprofessional team and teamwork behavior. For example, Shrader et al partnered with other programs on their campus to provide a 75-minute simulated interprofessional rounds experience for third-year pharmacy students. Students were provided feedback on their clinical performance, and results revealed that students reported self-perceived improvement in clinical skills and teamwork.35
At the University of Washington Center for Health Sciences Interprofessional Education, Research, and Practice, standardized team members were used as part of an objective clinical structured examination for medicine, pharmacy, dentistry, social work, and nursing to facilitate interprofessional collaboration. Assessment targeted team-oriented behaviors such as managing conflict, advocating for the patient, and speaking up against a power gradient.22,36
At the University of Colorado, during each interprofessional education session, students use knowledge of their own roles and those of other professions to appropriately assess and address the health care needs of patient- and population-centered cases as a team. Because of student concerns that cases did not pertain to all professions, the set-up of the cases changed over time. Care was taken to make issues and themes relevant to all participants, stress positive aspects of teamwork in health care, and make cases interprofessional. Students preferred when several cases were provided, each with a different profession in the featured role vs one case with all professions represented. These types of cases also were more successful when questions asked required consensus or were too broad for any one person to answer. Students commented that working together helped them better understand working in a collaborative environment and the trust that each professional must have for one another.
Clinical interventions.
In addition to exploring preclinical interventions, there is research focused on the impact of clinical interventions on roles and responsibilities, communication, and teamwork.25 Integrating students into practice sites that have embraced the concept of interprofessional health care may have a larger impact than exercises performed in didactic courses on students’ perceptions of team roles and responsibilities. Maldonado et al surveyed pharmacy students before and after practice experiences in multiple settings across the United States to assess student communication and teamwork.37 Working as part of interprofessional transplant teams improved students’ perceptions in all areas. Specifically, understanding each professional’s scope of practice and developing comfort working with other professionals were rated the highest by students. The authors noted that 89% of students completing the survey previously participated in either preclinical or clinical interprofessional experiences, suggesting that the students may already have held an appreciation for interprofessional collaboration. Nevertheless, the survey data demonstrated that participating in this clinical IPE experience positively impacted students’ perceptions. Thistlewait and colleagues published clinical interventions data after surveying nursing students who had participated in interprofessional learning through a student-led hospital ward.26 Themes that emerged included improvement in communicating and collaborating, enhanced team performance, increased understanding of other professions, and knowledge of how nursing fit into the larger team dynamics.26
While these data demonstrate the value of interprofessional clinical training, one cannot assume students will learn to work together simply by practicing in close proximity, and not all interactions with other professionals facilitate shared decision-making and accountability for patient outcomes.27 Small amounts of discussion and team training techniques are useful for enhancing students’ team building skills. Clinicians may already consider their practice interprofessional, but in reality, they are multidisciplinary, defined as several disciplines collaborating in the care of patients or alternatively as different groups within the same profession (e.g. cardiology versus radiology). For interprofessional team-based care to occur, schools of pharmacy must ensure that each practice site demonstrates a health care team that shares patient-care decision-making instead of referring patients to each other for consults. Evaluation of APPE sites may be beneficial in determining where and when interprofessional collaborative practice is actually occurring for pharmacy students. Establishing sites and opportunities specifically aimed at facilitating interprofessional teamwork is paramount for optimizing these types of training experiences.
Based on external funding from the Kaiser Permanente Foundation, the University of Colorado established IPE pairings and collaborations in rural areas. This 3-year grant aimed to create experiential education opportunities where students from various health professions could be paired to provide services to the communities in which they served. Faculty members from each program were identified to meet and overcome logistical challenges to facilitate interprofessional student-delivered care as outreach programs, including educational sessions and health fairs. The 3-year collaboration established more than 700 interprofessional pairings, reaching an estimated 22,000 people across rural Colorado.
BUILDING CAPACITY FOR IPE
Implementing IPE uncovers several logistical challenges (eg, available time, scheduling, faculty development) for fostering collaborations among students and faculty members from multiple professions. Anticipating key questions about logistics and faculty development programs can guide the optimal design and preferred methods for delivering IPE content. Critical capacity questions when developing successful IPE programs can include: (1) How many students must an IPE program accommodate? What are the ratios and mix of students across professions? (2) How many faculty members and staff are available, and how much time can they devote for teaching IPE-related content? (3) Are they comfortable training and/or precepting students in other professions? (4) What facilities are available, including active-learning classrooms, simulation centers, and clinical-training sites? (5) Which practice sites are suitable to provide team-based care? (6) What type of interactions will the students encounter at these sites? To address these questions, 2 key components of building capacity for IPE need to be considered: logistics and faculty development.
Logistics.
Scheduling logistics across multiple schools can be challenging. Most programs find scheduling to be the largest and most immediate challenge to implementing IPE. Convincing individual programs to make changes in class and/or practice experience schedules to allow students face-to-face time can be difficult. However, an IPE curriculum is useful even if only some health professions collaborate. Programs that encounter significant scheduling or other logistics problems may want to begin with 2 professions, for example, and expand the program based on their success. Anticipating participation of all students from all disciplines will likely significantly delay IPE implementation.
At the Thomas Jefferson University School of Pharmacy, all of the programs involved selected a specific day and time for IPE activities across various professional programs and used common technologies. This facilitated effective communication among all of the IPE teams.
At the University of Colorado, there were several logistic issues that needed to be addressed. First, while faculty members had appreciation of the value each profession contributed to patient care, they lacked understanding about the different programs on campus. Second, the students’ schedules for clinical experiences varied across programs. Third, the level of students’ expertise differed based on the time of the experiences and the academic year in which the students were within their respective programs. Fourth, pharmacy had specific supervision requirements in order to engage in interprofessional activities, mandating that a licensed pharmacist must be present in order for the students to practice pharmacy. Faculty members at the university level needed to establish a shared mission of the IPE grassroots initiative, identify specific goals and educational outcomes for participating students, and determine each program’s capacity to accommodate pairings to overcome these challenges.
Facilities.
Another challenge is the lack of adequate physical facilities for IPE. Simply putting students from multiple professions together in an auditorium-style lecture hall does not necessarily promote teamwork and shared decision-making. Facilities must allow for small-group discussions, and active learning should be the preferred arrangement for many preclinical interventions. While simulation is an ideal mode of delivering IPE, not all institutions have such facilities. Therefore, careful planning is essential with administration in charge of physical facilities to make sure learning spaces support the IPE curriculum design.
Faculty/preceptor development.
In addition to having students learn about each other, faculty members also must be trained about each other’s scope of practice and the differences in their respective programs. If faculty members do not value each other’s expertise, students will not either. Achieving clear communication across professions, even at the faculty level, can be challenging. Curricular design is time- and labor-intensive, especially when multiple perspectives are included. Not all professions will agree on every educational and clinical intervention. Therefore, time for faculty training is vital for building collegiality and trust. Teaching teams should be given time to get to know one another and to plan for teaching together so that learning is relevant and cohesive for students.
Specialized faculty development also is necessary to anticipate and deal with difficult situations that arise with students across professions. Faculty members must be skilled in facilitating, debriefing, diffusing conflicts, and discussing power gradients—all of which are teaching skills not traditionally taught within professions. Faculty development is necessary to prepare successful teaching teams and to give them confidence in using innovative teaching techniques with students whose perspectives differ from theirs. Preceptor development is also important to make sure that clinical teaching in practice settings is modeling good teamwork and conflict resolution. Programs should perform a needs assessment for faculty and preceptor training, plan development programming, and identify needed resources.28,29
At the University of Washington, a group of pharmacy faculty members formed an IPE learning community to coordinate efforts and share ideas. Later, the university formed an IPE implementation committee that included one faculty and one staff member from each program. The university-level committee worked to remove logistical barriers, assess teaching needs, and secure funding for new facilities to support IPE. A portion of a pharmacy school staff member’s time also was dedicated to assist with logistics and scheduling matters.
At the University of Colorado, capacity was determined despite the fact that all of the programs had students placed in rural sites throughout the academic year; there was no coordination on campus. Each program operated in a silo, finding placements and scheduling students to serve in the rural communities. Consequently, one of the major successes of this initiative was to create collaborations among all faculty members responsible for recruiting and finding new practice sites. For instance, a physician will visit the pharmacy department in rural hospitals to ascertain interest in accommodating medicine and pharmacy students. This increased the efficiency of new sites and allowed faculty members to develop rural “centers of excellence,” where students from various programs are placed at the same health systems for interprofessional trainings.
CONCLUSION
It is vital for administrators and faculty members who are starting new IPE programs to learn from those who have successfully implemented IPE programs. This primer provides tools, guidance, and lessons for pharmacy educators to better understand the process of developing effective IPE activities, implementing successful IPE programs, and assessing students’ educational outcomes.38-41 Collaborative IPE programs can establish a common mission across professional programs, build effective health care teams, develop an assessment plan of students’ competencies, and, ultimately, enhance patient care.
ACKNOWLEDGMENTS
The authors would like to thank the American Association of Colleges of Pharmacy Curriculum Special Interest Group for its support.
REFERENCES
- 1.Institute of Medicine. Washington DC: National Academy of Sciences; 2007. Preventing Medication Errors.http://books.nap.edu/openbook.php?record_id=11623# Accessed May 30, 2014. [Google Scholar]
- 2.Committee of Quality Health Care in America, Institute of Medicine. Washington DC: National Academy of Sciences; 2001. Crossing the Quality Chasm: A New Health System for the 21st Century.http://www.nap.edu/openbook.php?isbn=0309072808 Accessed October 10, 2014. [Google Scholar]
- 3.Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376(9756):1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 4.Framework for action on interprofessional education and collaborative practice. World Health Organization; 2010. Health Professions Networks Nursing and Midwifery Office within the Department of Human Resources for Health.http://apps.who.int/iris/bitstream/10665/70185/1/WHO_HRH_HPN_10.3_eng.pdf Accessed August 18, 2015. [Google Scholar]
- 5.Interprofessional Education Collaborative Expert Panel. Washington, DC: Interprofessional Collaborative; 2011. Core competencies for interprofessional collaborative practice: Report of an expert panel.http://www.aacn.nche.edu/education-resources/ipecreport.pdf Accessed August 18, 2015. [Google Scholar]
- 6.Accreditation standards and key elements for the professional program in pharmacy leading to the Doctor of Pharmacy degree. Standards 2016. Accreditation Council for Pharmacy Education; Chicago, IL: 2015. https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf Accessed August 19, 2015. [Google Scholar]
- 7.Smith KM, Doneka RS, Barner JC, DeHart RM, Scott JD, Martin SJ. Interprofessional education at six U.S. colleges of pharmacy. Am J Pharm Educ. 2009;73(4):Article 61. doi: 10.5688/aj730461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haddara W, Lingard L. Are we all on the same page? A discourse analysis of interprofessional collaboration. Acad Med. 2013;88(10):1–7. doi: 10.1097/ACM.0b013e3182a31893. [DOI] [PubMed] [Google Scholar]
- 9.Clark PG. What would a theory of interprofessional education look like? J Interprof Care. 2006;20(6):577–589. doi: 10.1080/13561820600916717. [DOI] [PubMed] [Google Scholar]
- 10.Hean S, Craddock D, O’Halloran C. Learning theories and interprofessional education: a user’s guide. Learning in Health Social Care. 2009;8(4):250–260. [Google Scholar]
- 11.Reeves S, Goldman J, Gilbert J, et al. A scoping review to improve conceptual clarity of interprofessional interventions. J Interprof Care. 2011;25(3):167–174. doi: 10.3109/13561820.2010.529960. [DOI] [PubMed] [Google Scholar]
- 12.Barr H. Toward a theoretical framework for interprofessional education. J Interprof Care. 2012;27(1):4–9. doi: 10.3109/13561820.2012.698328. [DOI] [PubMed] [Google Scholar]
- 13.Hean S., Craddock D, Hammick M. Theoretical insights into interprofessional education: AMEE Guide No. 62. Med Teach. 2012;34(2):e78–e101. doi: 10.3109/0142159X.2012.650740. [DOI] [PubMed] [Google Scholar]
- 14.Suter E, Goldman J, Martimianakis T, Chatalalsingh C, DeMatteo D, Reeves S. The use of systems and organizational theories in the interprofessional field: Findings from a scoping review. J Interprof Care. 2013;27(1):57–64. doi: 10.3109/13561820.2012.739670. [DOI] [PubMed] [Google Scholar]
- 15. The Canadian Interprofessional Health Collaborative (CIHC) Research & Evaluation Committee’s Quantitative Tools Working Group. (2012). An Inventory of Quantitative Tools Measuring Interprofessional Education and Collaborative Practice Outcomes. http://142.103.166.97/files/file/instructor-resources/CIHC_tools_report_Aug26%202012.pdf. Accessed May 21, 2014.
- 16. Measurement Instruments. National Center for Interprofessional Practice and Education. https://nexusipe.org/measurement-instruments. Accessed on August 24, 2014.
- 17.Thannhauser J, Russell-Mayhew S, Scott C. Measures of interprofessional education and collaboration. J Interprof Care. 2010;24(4):336–349. doi: 10.3109/13561820903442903. [DOI] [PubMed] [Google Scholar]
- 18.Archibald D, Trumpower D, MacDonald CJ. Validation of the interprofessional collaborative competency attainment survey (ICCAS) J Interprof Care. 2014;28(6):553–588. doi: 10.3109/13561820.2014.917407. [DOI] [PubMed] [Google Scholar]
- 19.Dow AW, DiazGranados D, Mazmanian PE, Retchin SM. An exploratory study of an assessment tool derived from the competencies of the interprofessional education collaborative. J Interprof Care. 2014;28(4):299–304. doi: 10.3109/13561820.2014.891573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fike DS, Zorek JA, MacLaughlin AA, Samiuddin M, Young RB, MacLaughlin EJ. Devleopment and validation of the student perceptions of physician-pharmacist interprofessional clinical education (SPICE) instrument. Am J Pharm Educ. 2013;77(9):Article 190. doi: 10.5688/ajpe779190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zorek JA, MacLaughlin EJ, Fike DS, MacLaughlin AA, Samiuddin N, Young RB. Measuring changes in perception using the Student Perceptions of Physician-Pharmacist Interprofessional Clinical Educaiton (SPICE) instrument. BMC Med Educ. 2014;14:101. doi: 10.1186/1472-6920-14-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dominguez DG, Fike DS, MacLaughlin EJ, Zorek JA. A comparison of the validity of two instruments assessing health professional student perceptions of interprofessional education and practice. J Interprof Care. 2015;29(2):144–149. doi: 10.3109/13561820.2014.947360. [DOI] [PubMed] [Google Scholar]
- 23.Ohland MW, Loughry ML, Woehr DJ, et al. The comprehensive assessment of team member effectiveness: development of a behaviorally anchored rating scale for self- and peer evaluation. Acad Manag Learn Edu. 2012;11(4):609–630. [Google Scholar]
- 24.MacDonald MB, Bally JM, Ferguson LM, Murray BL, Fowler-Kerry SE, Anonson JMS. Knowledge of the professional role of others: A key interprofessional competency. Nur Educ Pract. 2010;10(4):238–242. doi: 10.1016/j.nepr.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 25.Frankel A, Gardner R, Maynard L, Kelly A. Using the communication and teamwork skills (CATS) assessment to measure health care team performance. Joint Com Journ Qual Patient Safety. 2007;33(9):549–558. doi: 10.1016/s1553-7250(07)33059-6. [DOI] [PubMed] [Google Scholar]
- 26.Thistlewait J, Kumar K, Moran M, Saunders R, Carr S. An exploratory review of pre-qualification interprofessional education evaluations. 2015;29(4):292–297. doi: 10.3109/13561820.2014.985292. [DOI] [PubMed] [Google Scholar]
- 27.Yarborough M, Jones T, Cyr TA, Phillips S, Stelzer D. Interprofessional education in ethics at an academic health sciences center. Acad Med. 2000;75(8):793–800. doi: 10.1097/00001888-200008000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Van Winkle LJ, Bjork BC, Chandar N, et al. Interprofessional workshop to improve mutual understanding between pharmacy and medical students. Am J Pharm Educ. 2012;76(8):Article 150. doi: 10.5688/ajpe768150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Watt-Watson J, Hunter J, Pennefather P, et al. An integrated undergraduate pain curriculum, based on IASP curricula, for six health science faculties. Pain. 2004;110(1-2):140–148. doi: 10.1016/j.pain.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 30.MacKay S. The role perception questionnaire (RPQ): a tool for assessing undergraduate students’ perceptions of the role of other professions. J Interprof Care. 2004;18(3):289–302. doi: 10.1080/13561820410001731331. [DOI] [PubMed] [Google Scholar]
- 31.Dobson RT, Stevenson K, Busch A, Scott DJ, Henry C, Wall PA. A quality improvement activity to promote interprofessional collaboration among health professions students. Am J Pharm Educ. 2009;73(4):Article 64. doi: 10.5688/aj730464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. King HB, Battles J, Baker DP, et al. TeamSTEPPS: team strategies and tools to enhance performance and patient safety. In: Henriksen, Battles JB, Keyes MA, Grady ML, eds. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 3: Performance and Tools). Rockville, MD, 2008.
- 33.Brock D, Abu-Rish E, Chiu CR, et al. Interprofessional education in team communication: working together to improve patient safety. BMJ Qual Saf. 2013;22(5):414–423. doi: 10.1136/bmjqs-2012-000952. [DOI] [PubMed] [Google Scholar]
- 34.Marken PA, Zimmerman C, Kennedy C, Schremmer R, Smith KV. Human simulators and standardized patients to teach difficult conversations to interprofessional health care teams. Am J Pharm Educ. 2010;74(7):Article 120. doi: 10.5688/aj7407120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shrader S, McRae L, King WM, Kern D. A. Simulated interprofessional rounding experience in a clinical assessment course. Am J Pharm Educ. 2011;75(4):Article 61. doi: 10.5688/ajpe75461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Odegard PS, Robins K, Murphy N, et al. Interprofessional initiatives at the University of Washington. Am J Pharm Educ. 2009;73(4):Article 63. doi: 10.5688/aj730463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maldonado AQ, Bray BS, Woodard LJ, et al. Impact of participation on a solid organ transplant team on student pharmacists’ perceptions of interprofessional roles. Am J Pharm Educ. 2013;77(4):Article 74. doi: 10.5688/ajpe77474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hood K, Cant R, Leech M, Baulch J, Gilbee A. Trying on the professional self: nursing students’ perceptions of learning about roles, identity and teamwork in an interprofessional clinical placement. Appl Nurs Res. 2014;27(2):109–114. doi: 10.1016/j.apnr.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 39.Danielson J, Kim A, Bansal A, Weber S.An Interprofessional Education (IPE) Fingerprint for APPEs: Developing Metrics for Collaborative Interactions. American Association of Colleges of Pharmacy Annual Meeting [Poster Abstract]July 2014Grapevine, TX [Google Scholar]
- 40.Buring SM, Bhushan A, Brazeau G, Conway S, Hansen S, Westberg S. Keys to successful implementation of interprofessional education: learning location, faculty development, and curricular themes. Am J Pharm Educ. 2009;73(4):Article 60. doi: 10.5688/aj730460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hall LW, Zierler BK. Interprofessional education and practice Guide No. 1: developing faculty to effectively facilitate interprofessional education. J Interprof Care. 2015;29(1):3–7. doi: 10.3109/13561820.2014.937483. [DOI] [PMC free article] [PubMed] [Google Scholar]