Abstract
Objective. To design and assess a horizontally integrated biological sciences course sequence and to determine its effectiveness in imparting the foundational science knowledge necessary to successfully progress through the pharmacy school curriculum and produce competent pharmacy school graduates.
Design. A 2-semester course sequence integrated principles from several basic science disciplines: biochemistry, molecular biology, cellular biology, anatomy, physiology, and pathophysiology. Each is a 5-credit course taught 5 days per week, with 50-minute class periods.
Assessment. Achievement of outcomes was determined with course examinations, student lecture, and an annual skills mastery assessment. The North American Pharmacist Licensure Examination (NAPLEX) results were used as an indicator of competency to practice pharmacy.
Conclusion. Students achieved course objectives and program level outcomes. The biological sciences integrated course sequence was successful in providing students with foundational basic science knowledge required to progress through the pharmacy program and to pass the NAPLEX. The percentage of the school’s students who passed the NAPLEX was not statistically different from the national percentage.
Keywords: biological sciences, pharmacy curriculum, integration
INTRODUCTION
The doctor of pharmacy (PharmD) degree did not become the sole entry level degree for the pharmacy profession until the late 1990s. Prior to that, the baccalaureate degree focused primarily on the biology, chemistry, biochemistry, pharmacology, and medicinal chemistry required to compound, prepare, and distribute medications. It made sense for this heavily basic science-based curriculum to have stand-alone courses in each of these disciplines. The move to a more clinical pharmacy practice began the move away from a topic-driven curriculum to a more outcomes-based education mirroring a similar shift in medical education.1 Given the overlap of basic science disciplines of chemistry, biology, physics, and computation in such fields as epigenetics, genomics, and nanoscale science, it is increasingly difficult to maintain the traditional boundaries between these disciplines.
Two different forms of integrated curriculum have been proposed to address this issue: the vertical integration of basic science and clinical practice throughout the curriculum and horizontal integration of the same concepts from different perspectives.2 Horizontal integration links different subject areas within a scientific discipline while vertical integration blends basic science with clinical science.3 Differing methodologies have been proposed to achieve his integration including case-based, e-learning, and using specialized PhD faculty members to focus on integrated education.4-6 Clinical and basic science faculty members need to work together to ensure that basic science principles are reinforced throughout the PharmD curriculum.7
In 2003, the National Research Council released BIO2010, a report calling for structural changes in the way undergraduate biology education should be delivered.8 The report recognized that biology, chemistry, mathematics, physics, engineering, and computational sciences were increasingly connected. The report noted that the premedical curriculum caused many students to lose interest in medicine and that many students and physicians had come to view premedical education as simply a screening process for admission to medical school. This report issued a strong call for the development of interdisciplinary education that horizontally integrated disciplines across traditional lines to develop better critical-thinking skills in medical students.
To address these issues, the Association of American Medical Colleges and the Howard Hughes Medical Institute formed a committee to evaluate premedical and medical school science curricula. The 2009 report, Scientific Foundations for Future Physicians, suggested that while the move toward evidence-based medicine was necessary, there remained a critical need for physicians to assess each clinical situation and respond appropriately, drawing upon intuitions arising from principles that transcend mere following of examples.9 One goal of this report was to provide greater flexibility in the premedical curriculum that would permit undergraduate institutions to develop more interdisciplinary and integrative science courses.
From its inception in 2003, the Wingate University School of Pharmacy (WUSOP) embraced the concept of integration to create more practice-ready pharmacy graduates. Aside from some vertical integration, the basic sciences were horizontally integrated in a course that spanned the first year of the curriculum. The foundations of biochemistry, cellular biology, molecular biology, anatomy, physiology, and pathophysiology were embedded into a course sequence called Biological Science Integrated, which was designed as two 5-unit courses offered sequentially during the first and second semesters of the curriculum. The basic science curriculum provides a solid foundation on which to build the skills necessary for patient-centered care.10
This paper focuses on the development of this course sequence and the assessment of its effectiveness in imparting the foundational basic science knowledge required for students to successfully progress through the pharmacy curriculum and become competent graduates. The 2013 Center for the Advancement of Pharmacy Education (CAPE) Outcomes released in July 2013 accelerated the drive toward an outcomes-based educational system and defined 4 broad domains to guide the academy in the education of pharmacists. Domain 1 is the foundational knowledge required of a lifelong learner. This standard states students should be able to develop, integrate, and apply knowledge from the foundational sciences.11 This assessment provides other programs with a potential pathway to develop their own horizontally integrated basic science course.
DESIGN
The WUSOP program is a traditional 4-year PharmD program. A horizontally integrated biological sciences course sequence was developed and first offered to the inaugural class of WUSOP in fall 2003 and again in spring 2004. The course sequence has been offered every year since then with only minor changes. The information provided in this manuscript reflects the latest design and assessment of the course sequence. All protocols used to provide data for this study were approved by the institutional Research Review Board and were granted exempt status. The goal of the course sequence is to provide first-year (P1) pharmacy students with the basic biomedical and pharmaceutical sciences foundation on which the processes of applied pharmaceutical care can be built. The course sequence emphasizes the basic principles of biochemistry, molecular biology, cellular biology, anatomy, physiology, and pathophysiology, as well as application to clinical cases and pharmacy-related subjects (eg, such as drug mechanisms). The 2-semester course sequence meets 5 days per week for 15 weeks, with 50-minute class times, making each a 5-credit course. The prerequisite for the first course in the sequence is first-year PharmD standing. The prerequisites for the second course are first-year PharmD standing and completion of the first course with a grade of C or better.
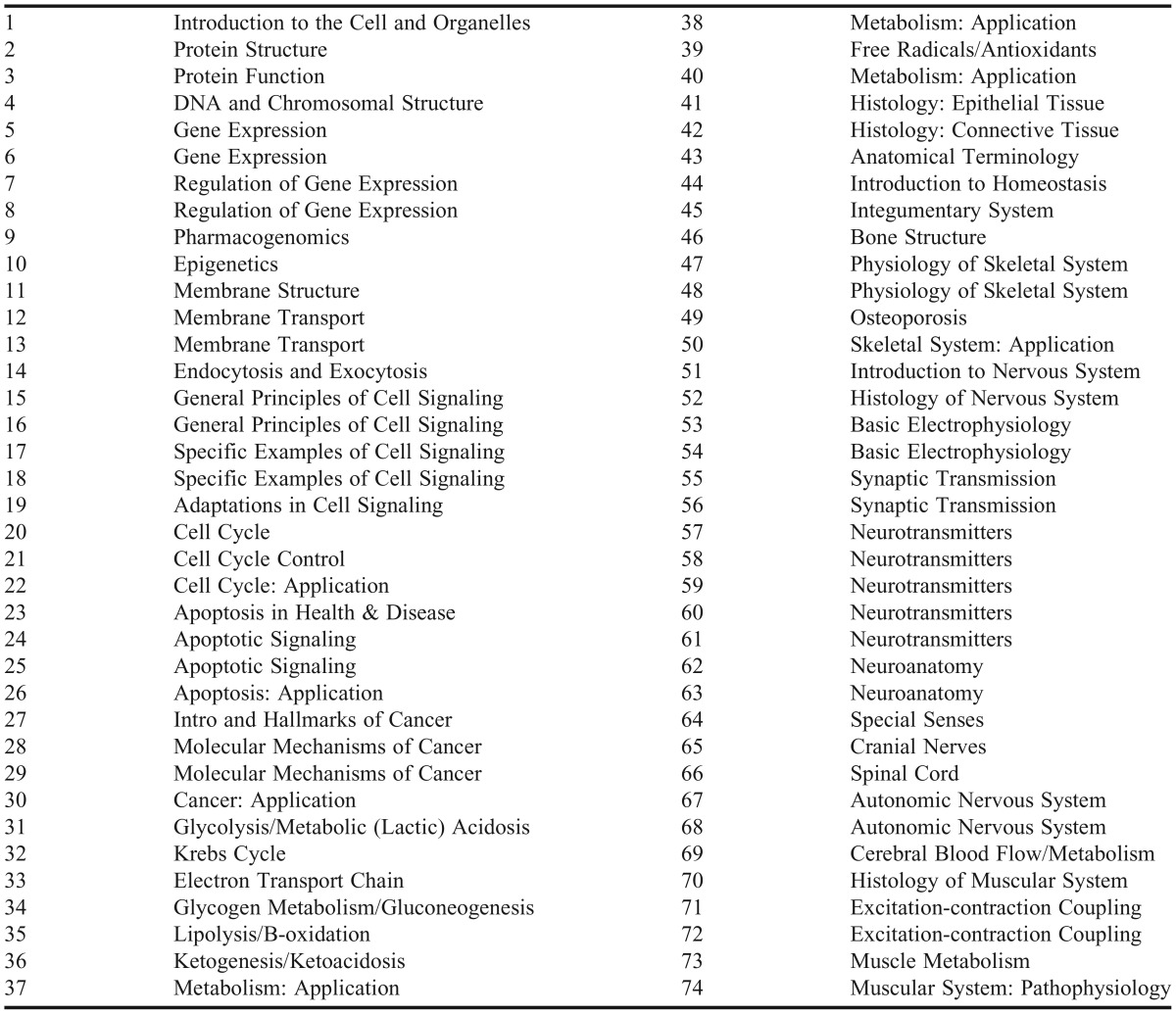
Students are expected to achieve objectives for both courses listed in Tables 1 and 2, respectively. The objectives align with the WUSOP program level outcomes, which include demonstration of a scientific foundation necessary for professional competency. More specific WUSOP outcomes the objectives align with are: (1) describing various cellular processes that are essential for survival; (2) defining the structure, nature, location, and function of a selected component of the human anatomy; (3) describing the physiology of a selected human organ system; and (4) describing how the organs and organ systems function together to maintain homeostatic variables.
Table 1.
Course Objectives for Biological Sciences Integrated I
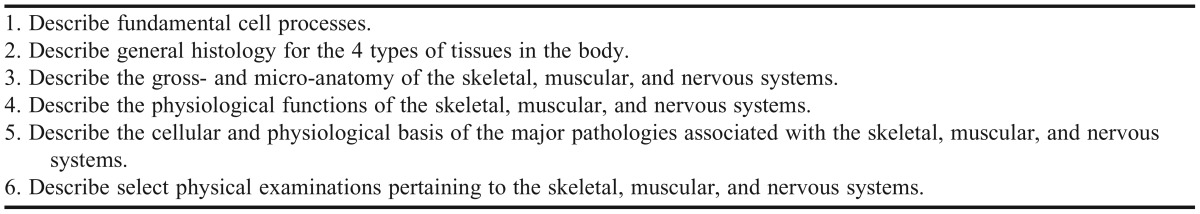
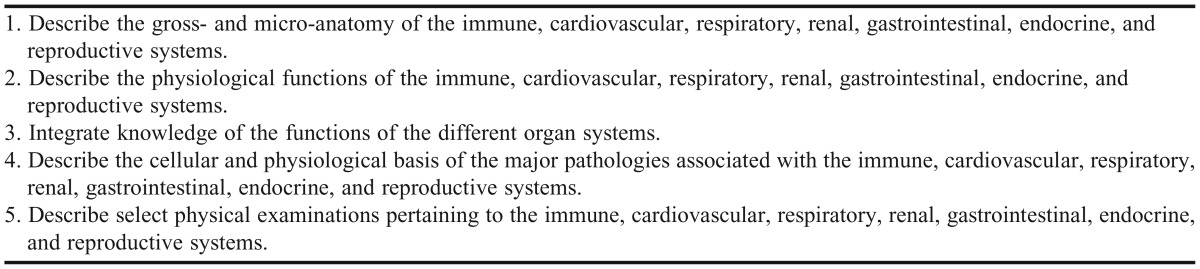
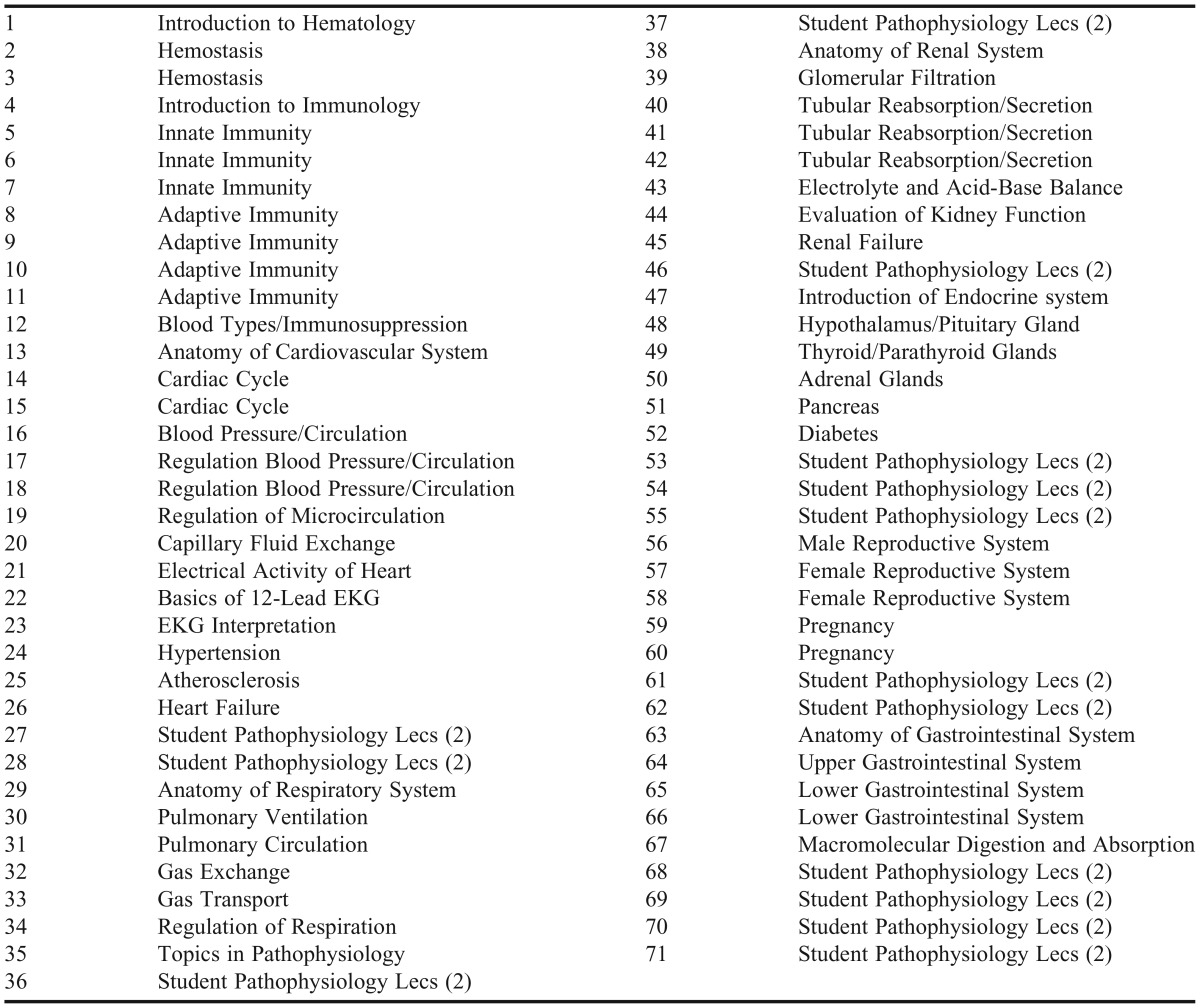
Table 2.
Course Objectives for Biological Sciences Integrated II
The topics covered in each course are listed in Appendix 1 and 2, respectively. Lecture topics in those tables designated as “Application” may include discussion of targeted therapies or of late-breaking research, interpretation of research literature, case studies, and/or other active-learning activities. These activities are not restricted to days designated Application, as most lectures are supplemented with activities and active learning. For example, most lecture class periods include use of TurningPoint clickers (Turning Technologies, Youngstown, OH), think-pair-share activities, videos, interactive physiology software, and other creative teaching techniques to enhance student engagement.
In addition to basic science disciplines being taught in one course sequence, those disciplines are integrated at the lecture level. For example, when teaching on the topic of apoptosis, the physiological and pathophysiological roles in human development, maintenance of health, aging, and disease is discussed. Furthermore, cell signaling pathways that induce apoptosis are taught in the context of physiological stimuli that activate each pathway. Within the discussion of cell biology (cell signaling pathways), some biochemistry is integrated (eg, the topic of protein structure and protein domains is incorporated to explain mechanisms of the formation of the death-inducing signaling complex during receptor-mediated apoptosis). Molecular biology is incorporated when discussing the role of p53 in nuclear-mediated apoptotic signaling in response to DNA damage; it is an example of a transcription factor, which regulates the expression of various genes by binding to gene regulatory sequences that will either repress or activate transcription. Finally, the pathophysiological consequence of altering the expression of various signaling proteins regulating apoptosis is discussed, mainly in the context of cancer. Also discussed are potential targets for drug therapy with the aim of inhibiting or stimulating apoptosis, depending on the disease state.
Other examples involve teaching each organ system, which covers anatomy, physiology, and pathophysiology. The regulation of each system by the endocrine and nervous systems typically involves discussion of cellular and molecular biology when explaining the relevant cell signaling. Furthermore, for each organ system, students are assigned 5 to 10 case studies that integrate clinically relevant topics in physiology and pathophysiology and, sometimes, cell biology.
The course sequence is primarily delivered in a lecture format by 2 full-time faculty members with PhDs in a basic science. Each faculty member teaches approximately half of the lectures in each course and alternates by lecture topic. Notes for each lecture are provided to all students electronically at least 48 hours before class. Students use 2 textbooks. The first is Ganong’s Review of Medical Physiology, which is available free online via AccessPharmacy.12 This textbook is an optional resource primarily used for reference, if needed. The second is Physiology Cases and Problems, 4th Edition, by Linda S. Costanzo, which is a required purchase.13 The majority (approximately 55) of the case studies included in the textbook are assigned throughout the 2 semesters to enhance student understanding and clinical application of the lecture topics. Several case studies are included as active-learning activities in class, but students are expected to work through most of the case studies outside of class. The case study textbook includes answers with detailed explanations for each question; thus, students have the opportunity to confirm their answers and thought processes. The case studies are not a graded assignment. However, knowledge of the material covered in the case studies is assessed on the examinations.
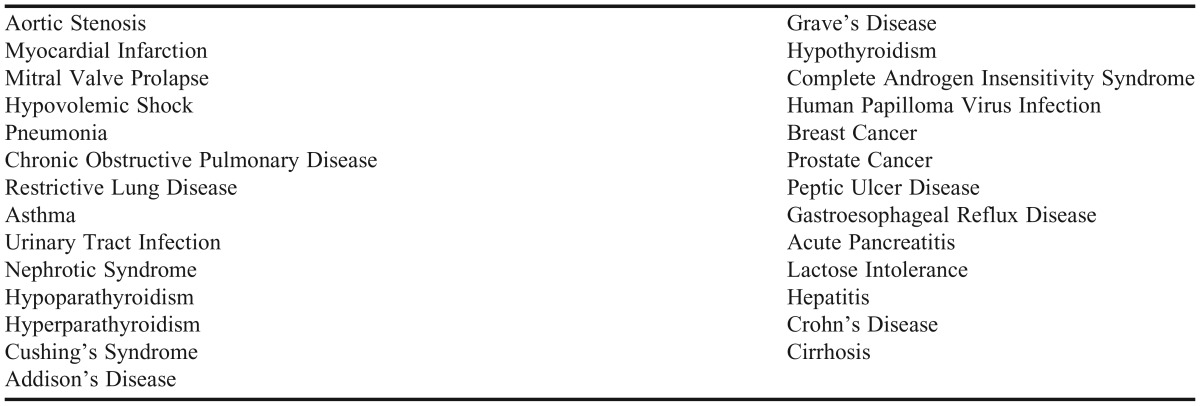
Achievement of course sequence objectives is assessed by 5 multiple-choice examinations in each course. In addition, the assessment of the second course includes student lectures covering selected disease states (Appendix 3). Each selected disease state is presented by a group of 3 to 4 students in a 20-minute lecture format with a 5-minute question and answer period. Two disease states are typically covered in one class period, designated as student pathophysiology lectures (Appendix 2). Student lectures aim to answer the following questions regarding each disease state: (1) who the disease affects; (2) if the disease is common; (3) what the cause/mechanism of the disease is; (4) what the identifying signs and symptoms (and underlying mechanisms) are; (5) how it is treated; and (6) how it is prevented. The presentations emphasize the etiology of each disease state rather than the epidemiology and treatment, since these latter areas are covered in more detail in the pharmacotherapy courses. Knowledge of the material included in the student lectures is assessed on the course examinations. Each student group is required to submit a lecture outline, PowerPoint presentation, and 5 multiple-choice examination questions. In 2011, WUSOP added a distant satellite campus. These students connect to the main campus during class time via a video conferencing system. Addition of this satellite campus has not affected the delivery of the course sequence.
The sequence was designed to integrate into the WSUOP curriculum. The basic concepts from the basic science sequence are expanded on in a separate 3-credit course, Principles of Drug Mechanisms, in the second semester, in which the mechanisms of drug action are described. The foundational principles of biopharmaceutics and pharmacokinetics are introduced in a 3-unit course in semester 3. Clinical Pharmacokinetics is taught as a stand-alone 2-unit course in semester 4. The WUSOP curriculum includes 18 pharmacotherapy courses in the second and third years, which are organized around organ systems and special populations. These courses provide the anatomy, physiology, pathophysiology, genomics, kinetics, and pharmacology relevant to the organ systems and diseases of those systems and, thus, reinforce the foundational principles taught in the basic sciences sequence and the Principles of Drug Mechanisms. Additionally, in each semester of the second and third years, all students participate in a small group, problem-based learning (PBL) sequence that vertically integrates all disciplines into a clinical decision-making course. In PBL activities, students work in teams on cases and must arrive at an evidence-based clinical decision.
The basic sciences course sequence has been a part of the WUSOP curriculum since its inception. Therefore, the cost in faculty time and energies in implementing the courses was similar to developing any course. The topics of the course sequence were largely determined using the Medical Physiology Learning Objectives developed by the American Physiological Society and the Association of Chairs of Physiology Departments in 2000.14 Furthermore, topics were refined through reading material (syllabi, course notes, etc) of courses for which the successful completion of the basic sciences sequence are a prerequisite (eg, Drug Mechanisms and all of the pharmacotherapy courses). Topics were also refined through discussions with the clinical faculty members teaching those courses. Continued changes may occur based on results from the university’s Annual Skills Mastery Assessment (ASMA).
EVALUATION AND ASSESSMENT
As an essential component of the WUSOP program’s scientific foundation, we assessed the effectiveness of course sequence in imparting the basic science knowledge appropriate for success in the pharmacy program and for development of a graduate competent to practice pharmacy as deemed by passing the NAPLEX. We assessed the sequence at the course, school, and national levels.
Course Level Assessment
The effectiveness of the sequence in achieving course objectives was assessed with 4x100 question examinations (1 point per question; each examination worth 100 points) and a comprehensive final examination composed of 133 questions (1.5 points per question; examination worth 200 points). Question types included multiple-choice, true or false, and labeling. Course data from 2009 to 2014 were selected for this study as the same 2 faculty members taught the courses those years, making content, grading, etc, subject to less inconsistency. Over this period, the individual student examination scores for the first course ranged from 40% to 100%, and for the second course, from 44% to 98%. These examinations gave 600 points for the first course. However, the second course also included the student lectures on selected disease states (Appendix 3), which were worth 50 points, making a course total 650. Presentations were assessed by both faculty members using a rubric with 10 sections each worth 5 points (50 total, Table 3). The average faculty score was then modified according to the group’s peer evaluations of each other.
Table 3.
Grading Rubric for Student Lecture in Biological Sciences Integrated II
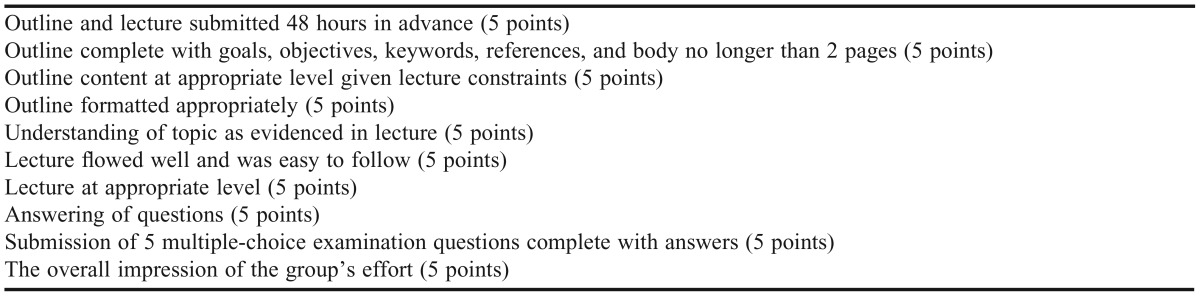
An average peer evaluation score of 5 (out of 5) meant the student would receive 100% of the averaged faculty score whereas an average peer evaluation score of 3 meant the student would only receive 60% of the averaged faculty score. Students were trained in peer assessment in another course (Professional Communications) in the first semester of the curriculum. From 2009 to 2014, individual student lecture scores ranged from 57.6% to 99.0%, with an overall mean score of 92.2%. Letter grade assignments for both courses were initially A ≥ 89.5%, B ≥79.5%, C ≥ 69.5%, D ≥ 64.5%, and F ≤ 64.4%. But in the fall 2011, WUSOP eliminated the D grade option in all courses in the pharmacy curriculum, and any student scoring less than 69.5% received an F.
Mean course scores for the first course were 81.3% in 2009 (out of 75 students, none failed); 82.5% in 2010 (out of 78 students none failed; 3 Ds were given); 79.9% in 2011 (out of 103 students, 5 failed); 84.1% in 2012 (out of 108 students, 3 failed); 82.1% in 2013 (out of 100 students, 3 failed). Mean course scores for the second course were 81.1% in 2009 (out of 71 students, 2 failed); 79.7% in 2010 (out of 77 students, 2 failed); 81.9% in 2011 (out of 77 students, 1 failed); 80.4% in 2012 (out of 100 students, 2 failed); 82.7% in 2013 (out of 106 students, none failed); and 82.3% in 2014 (out of 96 students, 3 failed).
In summary, from 2009 to 2014 (5 semesters), 466 students took the first course, and 14 scored below 69.5%, while over the same period (6 semesters) 527 students took the second course, and 10 scored below 69.5%. Students who failed the course sequence were required to repeat the course the following year, and they progressed through the program on a modified schedule.
School Level Assessment
At the school level, the Annual Skills Mastery Assessment examination (ASMA) was used to assess students’ basic science knowledge independent of the course and its teachers. We reviewed student performance in the ASMA examination from 2009 to 2014 (Table 4). The methodology of the ASMA was described in AJPE in 2009.15 The examination is designed to assess the students’ ability to perform skills as defined by faculty-developed terminal ability outcomes statements (TABO). The mastery score was calculated through a reliable Angoff process.16 Examination questions were written by faculty members other than the 2 who taught the sequence, making this an independent evaluation.
Table 4.
Annual Skills Mastery Assessment (ASMA) Examination Results 2009-2014
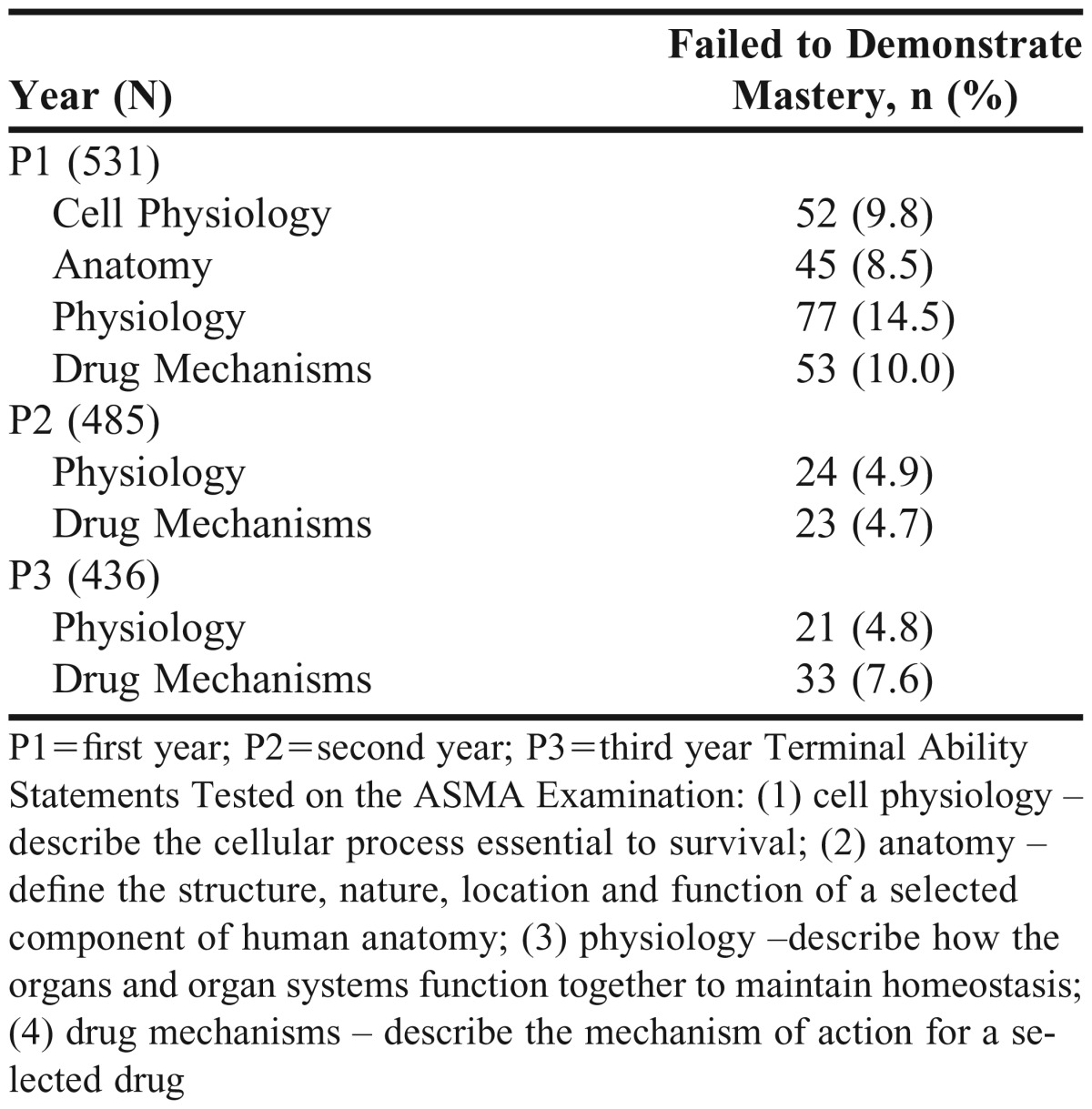
Results were reviewed from 4 TABOs for P1s, and two TABOs for students for the next 2 years (P2s and P3s), which are described in Table 7. Specifically, the TABOs included cellular processes essential to survival, the function of important anatomical structures (terminal abilities 1 and 2), and the interaction of organs and organ systems to maintain homeostasis and mechanisms of action of selected drugs (terminal abilities 3 and 4).
Overall, the percentage of P1s who failed to demonstrate mastery of these abilities between 2009 and 2013 were 9.8% (ability 1), 8.5% (ability 2), 14.5% (ability 3), and 10.0% (ability 4). Over the same time period, the percentage of P2s who failed to demonstrate mastery was 4.9% (ability 3) and 4.7% (ability 4). Similarly, the percentages for P3s were 4.8% (ability 3) and 7.6% (ability 4). The ASMA is not a high-stakes examination for P1s or P2s. However, P3s can be held back from starting P4 clinical practice experiences if they fail to achieve a score of mastery.15 Given the formative nature of the P1 and P2 ASMA examination, students who do not pass, meet with their adviser and discuss a plan to improve their knowledge in relevant subject areas.
The assistant dean for assessment at WUSOP compiled a database of student performance to identify early predictors of failure to complete the PharmD program.17 The database was used to correlate performance in the first course of the basic sciences sequence and performance on the ASMA to student’s scaled score on the NAPLEX. Pearson correlations for each comparison were: 0.32 (basic sciences sequence), 0.52 (ASMA1), 0.63 (ASMA2), 0.66 (ASMA3), and 0.76 (ASMA4). Thus, performance on the ASMA was highly predictive of performance on the NAPLEX. Furthermore, students who scored below 70% in the first course of the sequence were 18 times more likely (odds ratio 18.8) to fail to complete the program on time or to be dismissed from the program for academic failure (n=398, p<0.01). Because students who failed to complete the program typically withdrew before the fourth year, a comparison of performance in the course sequence to performance on ASMA3 seemed to be most appropriate. Students who scored 70% or below in the first course of the sequence were 5 times more likely (odds ratio 4.9) to fail to demonstrate mastery on the ASMA3 examination (n=250, p<0.01).17
National Level Assessment
The third level of assessment involved comparing the WUSOP graduates’ performance on the NAPLEX, (Table 5) to the national performance average to determine if the WUSOP curriculum disadvantaged students.18 A student t test was performed, comparing the national passing rates to WUSOP passing rates using KaleidaGraph (Synergy Software, Reading, PA). Between 2007 and 2013, the cumulative first-time taker pass rate was 96.8% compared to 95.3% nationally. There was no significant difference between the percentage of WUSOP students who passed the NAPLEX and the national average (p>0.05).
Table 5.
NAPLEX Examination Results from All WUSOP Graduates from 2007-2013
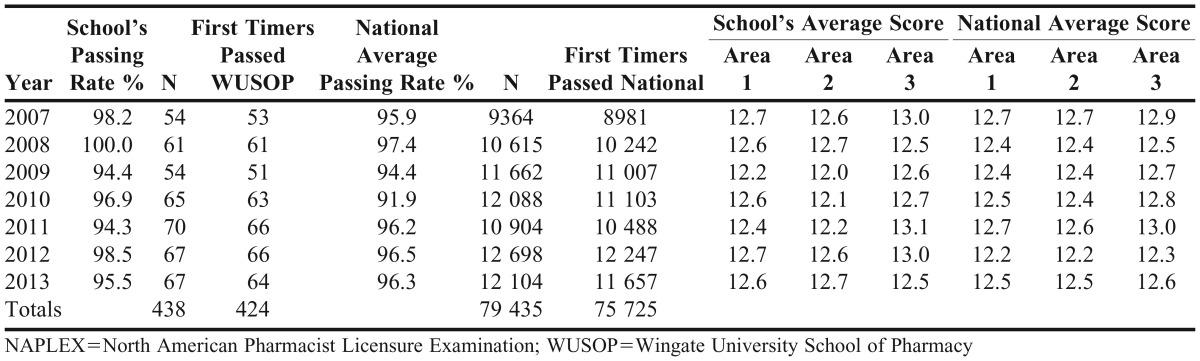
The WUSOP founding class graduated in 2007, thus this data encompassed all graduates from the university to date. Comparing WUSOP with national scores in areas 1 to 3, WUSOP students appeared to closely mirror national trends. The comparative NAPLEX results suggested the basic sciences course sequence, as a component of the curriculum, effectively imparted the basic science knowledge necessary to produce pharmacy school graduates competent to practice pharmacy. The horizontally integrated biological science curriculum provided sufficient preparation for students to pass their board examinations.
DISCUSSION
The basic sciences course sequence was developed to provide P1 pharmacy students with scientific knowledge of disease and treatment through a horizontally integrated approach, from the biochemical and cellular level to organism level. Based on results from course examinations and student lectures, students achieved the course objectives with an average mean course grade of 82.0% for the first course and 81.4% for the second course. Over the time period evaluated, only 3% of P1 students scored below 69.5% in the first course and 1.9% in the second course, demonstrating that the majority of students who completed the course sequence had the necessary basic science knowledge, as deemed by WUSOP, to successfully progress through the curriculum.
Based on the results from the ASMA, the majority of students mastered the terminal basic science abilities tested. In the P1 year, this information is primarily taught in the basic sciences course sequence, with reinforcement in the Principles of Drug Mechanisms course taught in the spring semester in conjunction with the second course of the sequence. In the P2 and P3 years, basic science concepts are reviewed and reinforced in the pharmacotherapy and PBL courses.
The results for the drug mechanism terminal ability is included in Table 4 because many of the basic science concepts to understand drug mechanisms are primarily taught in the basic sciences course sequence. In the P2 and P3 years, the only basic science terminal abilities consistently tested are physiology and drug mechanisms. In the P4 year, no basic science terminal abilities were consistently tested on the ASMA from 2009 to 2014; thus, we did not have sufficient data to include. The percent of P1 students who did not master each of the 4 basic science terminal abilities ranged between 8.5% and 14.5%. Furthermore, 4.7% and 4.9% of P2 students and 4.8% and 7.6% of P3 students did not master physiology and drug mechanisms abilities, respectively.
The data suggest that the course sequence is successful in instilling the basic science concepts necessary to master the related program terminal abilities, and that reinforcement of these concepts in the P2 and P3 years of the curriculum enhances their understanding. Because the ASMA is given in March, before the end of the semester, some material tested on it may have not been taught yet in the second course or Principles of Drug Mechanisms. This factor may contributed to the higher failing rates on these terminal abilities in the P1 year compared to P2 and P3 years.
Because the percentage of WUSOP graduates who pass the NAPLEX is similar to the national average, it can be inferred that the pharmacy program at the university has an effective basic science curriculum; albeit, the link is indirect. We included NAPLEX examination results comparing WUSOP’s percentage of students passing to the national average to demonstrate that our basic science curriculum, primarily the horizontally integrated course sequence, appears to be successful in instilling the foundational basic science knowledge necessary to pass the NAPLEX.
The course sequence has been well-received by students, as determined by the course evaluations and focus group interviews (conducted by the assistant dean of assessment) each year. However, the response rate of the course evaluations is consistently low; thus, the data are not included in the manuscript. In brief, the majority of students who complete the course evaluations rate the design and implementation of the course sequence with the highest rating (mode of 5 out of 5 on all questions) and report that the courses are excellent overall. The high ratings are consistent from year to year.
Possible limitations to the implementation of the course sequence exist. First, the amount of information from each basic science discipline that is taught is limited when compared with a traditional basic science curriculum. For example, the amount of biochemistry taught in the course sequence is far less than what is taught in a separate semester-long course dedicated to biochemistry, which is often included in a traditional pharmacy program. Thus, it may limit students’ basic science foundation. However, NAPLEX results suggest that WUSOP students obtain an adequate foundation necessary for competency as a practicing pharmacist. Others may view the limitation of the amount of material taught in the course sequence as a positive trait because students are not overwhelmed by perceived extraneous information not directly related to competency in pharmacy practice.
A second potential limitation to the course sequence is the 5-day-per-week schedule. Although students master the material, it is difficult for some to keep up with studying and learning the material on a day-to-day basis. In this case, we speculate that these students may find themselves “cramming” before each examination. A third limitation expressed by some students in the course evaluations is that each course is taught by 2 professors, instead of one. Although the teaching evaluations for each professor (data not included) are excellent, some students find it difficult to adjust to 2 different teaching styles.
SUMMARY
A horizontally integrated biological sciences course sequence was developed to provide first-year pharmacy students the scientific foundation necessary to succeed in the pharmacy program and to develop into a competent pharmacist. The course sequence was effective at imparting the basic science knowledge required to successfully progress through the WUSOP curriculum and to pass the NAPLEX. Student achievement of course objectives and program outcomes was demonstrated by positive results of course examinations, student lectures, ASMA, and NAPLEX.
Appendix 1.
Lecture No. and Topics for Biological Sciences Integrated I
Appendix 2.
Lecture Number and Topics for Biological Sciences Integrated II
Appendix 3.
Topics for Student Lectures in Biological Sciences Integrated II
REFERENCES
- 1.Nemire RE, Meyer SM. Educating students for practice: educational outcomes and community experience. Am J Pharm Educ. 2006;70(1):Article 20. doi: 10.5688/aj700120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kerr RA. Curricular integration to enhance educational outcomes. Pharmacotherapy. 2000;20(10Pt2):292S–296S. doi: 10.1592/phco.20.16.292s.35007. [DOI] [PubMed] [Google Scholar]
- 3.Ratka A. Integration as a paramount educational strategy in academic pharmacy. Am J Pharm Educ. 2012;76(2):Article 19. doi: 10.5688/ajpe76219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woster PM. Maintaining basic science content throughout the PharmD curriculum. Am J Pharm Educ. 2003;67(3):Article 99. [Google Scholar]
- 5.National Research Council (US) Committee on Undergraduate Biology Education to Prepare Research Scientists for the 21st Century. 2003. BIO2010: Transforming undergraduate education for future research biologists. http://www.ncbi.nlm.nih.gov/pubmed/20669482. Accessed June 9, 2014.
- 6.Hrubey TW. An integrated case-based curricular model for the entry-level doctor of pharmacy degree. Am J Pharm Educ. 1996;60(FAll):265–274. [Google Scholar]
- 7.Dubois EA, Franson KL. Key steps for integrating a basic science throughout a medical school curriculum using an e-learning approach. Med Teach. 2009;31(9):822–828. doi: 10.1080/01421590903147584. [DOI] [PubMed] [Google Scholar]
- 8.Smith JJ, Koethe SM, Forster HV. A new PhD training track: a proposal to improve basic science training. Am J Physiol. 1997;272(6Pt3):S36–S46. doi: 10.1152/advances.1997.272.6.S36. [DOI] [PubMed] [Google Scholar]
- 9.Association of American Medical Colleges-Howard Hughes Medical Institute. 2009 scientific foundations for future physicians. www.aamc.org/scientificfoundations. Accessed June 9, 2014.
- 10.Brown B, Skau K, Wall A. Learning across the curriculum: connecting the pharmaceutical sciences to practice in the first professional year. Am J Pharm Educ. 2009;(2):73. Article 36. doi: 10.5688/aj730236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Medina MS, Plaza CM, Stowe CD, et al. Report of the 2012-2013 Academic Affairs Standing Committee: Revising the Center for the Advancement of Pharmacy Education (CAPE) Educational Outcomes 2013. Am J Pharm Educ. 2013;77(8):Article 162. doi: 10.5688/ajpe778162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barrett KE, Barman SM, Boitano S, Brooks HL. Ganong’s Review of Medical Physiology. 24rd ed. New York, NY: Lange Medical Books/McGraw-Hill; 2012. [Google Scholar]
- 13.Costanzo LS. Physiology Cases and Problems. 4th ed. Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins; 2012. [Google Scholar]
- 14.American Physiological Society. 2012 Medical Physiology Learning Objectives. www.the-aps.org/medphysobj. Accessed May 24, 2014.
- 15.Alston GL, Love BL. Development of a reliable, valid annual skills mastery assessment examination. Am J Pharm Educ. 2010;74(5):Article 80. doi: 10.5688/aj740580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alston GL, Haltom WR. Reliability of a Cut Score for an Annual Skills Mastery Assessment. Am J Pharm Educ. 2013;77(10):Article 211. doi: 10.5688/ajpe7710211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alston GL, Lane D, Wright NJD. The methodology for the early identification of students at risk for failure in a professional degree program. Curr Pharm Teach Learn. 2014;6(6):798–806. [Google Scholar]
- 18. North American Pharmacist Licensure Examination School Summary Reports for 1st, 2nd and 3rd trimesters for 2010 through 2014. [Accessed at secure score report location provided by NABP.net]. Sample results for 2012 and 2013: http://www.nabp.net/programs/examination/naplex/school-pass-rate. Accessed November 11, 2014.


