Abstract
Pertussis is an acute and very contagious pulmonary disease, clinically characterized by periods of coughing and paroxysms that may cause death. The disease afflicts mainly the pediatric population and is life threatening to children under the age of 1 year. Since the beginning of the second millennium, the number of cases of pertussis has increased, menacing public health, despite the availability of the pertussis vaccine. The resurgence of the disease among adults and older children creates a reservoir of infection that will afflict the unimmunized or incompletely immunized children. As newborns and infants show the highest mortality rate, immunization during pregnancy is a new strategy to reduce the burden of pertussis. The authors report the case of a newborn that presented respiratory distress accompanied by marked leukocytosis. Bronchiolitis was the initial diagnostic hypothesis, but the clinical picture became typical of pertussis when paroxysmal coughing ensued. Isolation of the Bordetella pertussis and antigenic demonstration by polymerase chain reaction were positive from respiratory secretion. Despite appropriate antibiotic therapy and intensive care management the child died and the autopsy showed characteristic diagnostic findings. The authors call attention to this diagnosis when facing respiratory failure among young children, mainly in the presence of marked leukocytosis. Thorough research on the immunization status of the patient’s social environment is of crucial importance.
Keywords: Bordetella pertussis, Respiratory Insufficiency, Immunization, Leukocytosis, Autopsy
CASE REPORT
A 16-day-old male newborn was brought to the emergency facility with a 3-day history of respiratory distress and cough without fever. He was born at 38 weeks of gestational age, through vaginal delivery with an Apgar score of 9,10,10 at 1,5 and 10 minutes, respectively, weighing 2700 g and 47 cm long. The mother was gesta 4 and para 4, aged 23 years and went through an uneventful prenatal period, which comprised seven medical consultations. The newborn was discharged 2 days after birth and was healthy and exclusively breastfed.
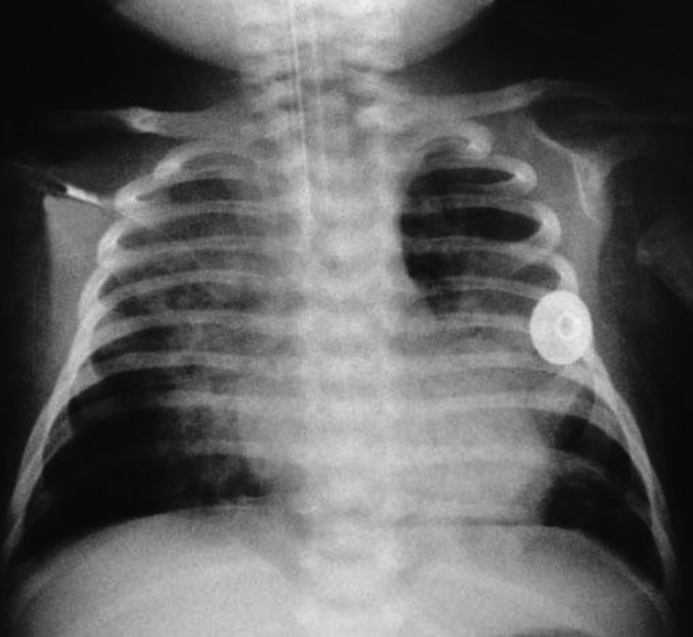
On physical examination, the patient presented signs of respiratory insufficiency with room air oximetry of 86% and the presence of bilateral pulmonary rales. His initial chest radiography showed superior right lobe atelectasis (Figure 1).
Figure 1. Plain chest radiography showing opacity in the upper half of the right lung, delimited by the horizontal fissure, which is upwardly displaced and associated with hyperinflation of the remaining right lung and the entire left lung with deviation of the trachea to the right. The findings consistent with right upper lobe atelectasis.

Bronchiolitis was diagnosed at first glance, and therefore he was hospitalized in the neonatal intensive care unit (NICU) to receive oxygen and enteral feeding.
The clinical outcome was troublesome initially requiring non-invasive respiratory support and subsequently orotracheal intubation, and mechanical ventilation coupled with intravenous fentanyl infusion. Pulmonary imaging sequences showed atelectasis of the left upper lobe and signs of bilateral hyperinflation. At this time, nasopharyngeal secretion was collected for Bordetella pertussis research, and azithromycin was started, since the patient had begun paroxysmal coughing.
On the seventh day of hospitalization, a marked leukocytosis (leukocytes = 92,200/mm3 with 1% promyelocytes, 1% myelocytes, 1% metamyelocytes, 8% band cells, 36% neutrophils, 40% lymphocytes, 12% monocytes, 14% eosinophils, with normal platelets and red blood cell count) and C-reactive protein = 73 mg/L (reference value [RV]: < 5 mg/dL) were observed. The chest radiography was repeated and showed bilateral cardiac silhouette blurring besides opacities in the upper two-thirds of the right lung and in the medial third of the left lung, which motivated the association of amikacin and oxacillin to the previous antibiotic regimen (Figure 2). The outcome was unfavorable and hemodynamic instability ensued requiring dobutamine and nitric oxide administration. Unfortunately all efforts were insufficient and the patient died on the seventh day of hospitalization. The polymerase chain reaction (PCR) and nasopharynx culture for B. pertussis were both positive, which were available post mortem.
Figure 2. Plain chest radiography showing bilateral perihilar opacities predominantly of an alveolar pattern with air bronchogram, partially blurring the cardiac silhouette and mediastinum, giving the appearance of a fuzzy heart.
AUTOPSY FINDINGS
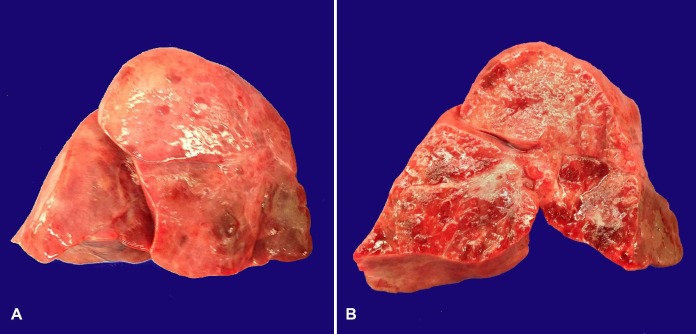
After the opening of cavities, mild bilateral pleural effusion was drained. The lungs were heavy (right lung weighed 54.0 g [RV: 31.0 g]; left lung weighed 42.0 g [RV: 27.0 g]) covered by glossy, smooth pleura with patchy purple areas. The cut surface showed a firm-consistency pulmonary parenchyma with glossy and purple surface, which is consistent with shock lung (Figure 3).
Figure 3. Gross view of the enlarged right lung. A - Glossy pleura and purple patchy areas. B - The cut surface with condensed parenchyma intermingled with purple-colored areas.
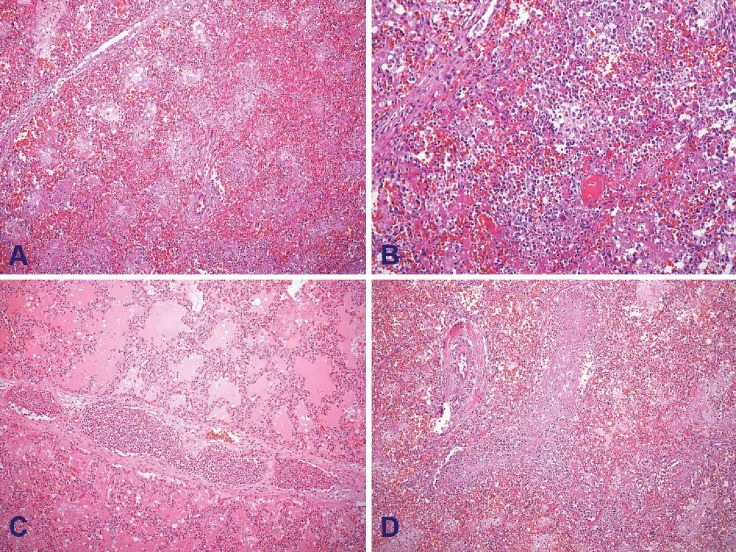
The microscopic examination disclosed extensive diffuse alveolar damaged areas intermingled with edema, alveolar hemorrhage, and pneumonia. Necrotizing bronchiolitis, characterized by respiratory epithelium necrosis, intraluminal desquamated epithelium, cellular debris, and fibrin were also observed. Interlobular septa were slightly thickened by acute inflammatory infiltration and dilated lymphatic vessels with leukostasis (Figure 4).
Figure 4. Photomicrography of the lung. A - Exudative phase of the diffuse alveolar damage with alveolar spaces filled by macrophages, cellular debris and fibrin (H&E, 100X). B - Pneumonia. Note the alveolar spaces filled by numerous neutrophils (H&E, 200X). C - Lymphatic vessel in the interlobular septum containing leukostasis. Note pulmonary edema in the adjacent pulmonary parenchyma (H&E, 100X). D - Focal necrotizing bronchiolitis with necrosis of the epithelial lining and intraluminal fibrin and cellular debris (H&E, 200X).
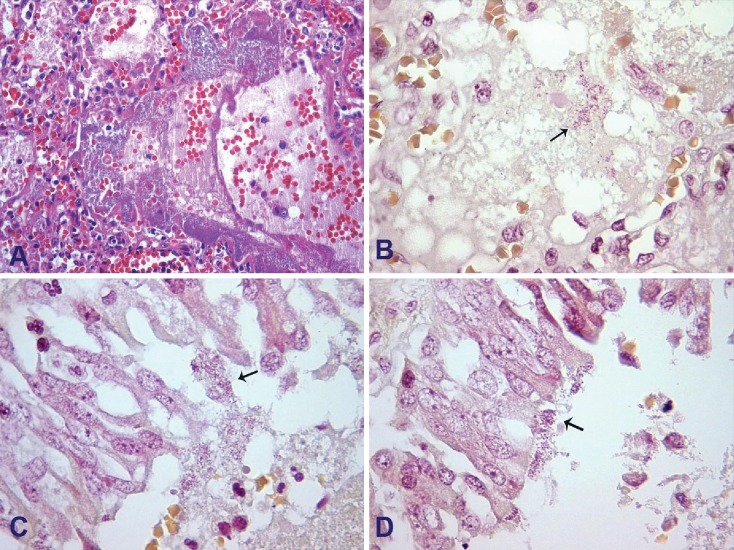
Gram-negative bacilli colonies, identified by Brown-Hopps staining, were found within some alveoli and bronchiole’s respiratory epithelium (Figure 5).
Figure 5. Photomicrography of the lung. A - Bacterial colonies within the alveolar lumen (H&E, 400X). B - Gram-negative bacilli within the alveolar lumen (arrow) (Brown-Hopps, 1000X). C and D – Bacilli rod-shaped bacteria associated with the ciliary respiratory epithelium of the bronchiole (arrows) (Brown-Hopps, 1000X).
The heart weighed 18.8 g (RV: 20.0 g) and still presented patency of the oval foramen, probably due to pulmonary hypertension related to the acute pulmonary disease.
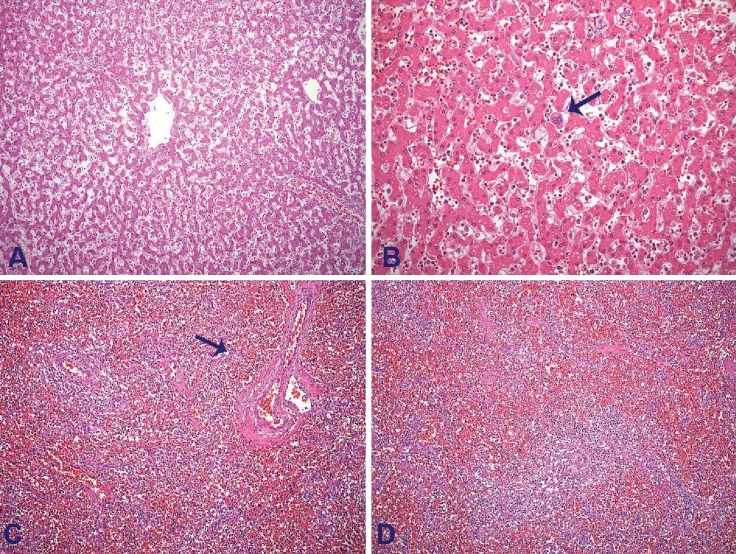
The liver was enlarged (weighed 159.0 g [RV: 127 g]) and showed purple parenchyma at the cut surface. At microscopy, signs of passive congestion with extensive sinusoidal dilatation were present besides the presence of grade-2 microvesicular steatosis and remnant extramedullary hematopoiesis. The spleen weighed 10.1 g (RV: 12 g) and showed red pulp congestion and white pulp lymphocyte depletion (Figure 6).
Figure 6. A - Photomicrography of the liver showing zone three sinusoidal dilatations due to passive congestion (H&E, 100X). B – Photomicrography of the liver with extramedullary hematopoiesis. Note the megakaryocyte within the hepatic sinusoid (arrow) (H&E, 200X). C and D - Photomicrography of the spleen showing red pulp congestion and white pulp lymphocytary depletion (arrow) (H&E, 100X).
DISCUSSION
Pertussis, also called whooping cough, is an acute and very contagious pulmonary disease, with typical manifestation characterized by periods of cough and paroxysms. The etiologic agent is a small, aerobic Gram-negative bacillus, pathogenic only in humans. The transmission is made through the inhalation of respiratory fluids from ill contacts. Symptoms usually develop 5–10 days after contact with the diseased (not exceeding 3 weeks).1,2
Worldwide, an estimated 50 million cases of pertussis take place every year, accompanied by up to 300,000 deaths. During the 1990s, a marked reduction in the incidence was observed, due to the expansion of an efficient immunization policy. However, since 2011, an increasing number of cases have been observed, affecting mostly children in their first year of age. In 2010, a pertussis outbreak hit California, USA, with more than 9000 reported cases and 10 reported infant deaths.3 Such an increase in the incidence of this disease was also seen in Australia, The Netherlands, Canada, Belgium, Germany, UK, and Japan at the same time.4 Since 2011 in Brazil, and in the state of São Paulo, there has been a progressive increase in the incidence of pertussis despite the universal coverage of immunization. In Brazil in 2008, the incidence was 0.71 cases/100,000 inhabitants; however, in 2014, the incidence increased to 37 cases/100,000 inhabitants with nearly 50 cases/100,000 inhabitants in the state of São Paulo—the highest rate compared with other Brazilian states. The mortality rate of pertussis in Brazil increased from 0.7% (23 deaths) in the 1990s to 1.7% (109 deaths) in 2013.5-8 The reasons for the re-emergence of the disease are still unknown, but among the possibilities that some researchers believe, is a cyclical behavior with a re-appearance every 4–5 years, while others believe in bacterial antigenic changes. Recent studies showed a difference in the virulence factors of both the circulating and the vaccine strains of B. pertussis, suggesting an imposed selection pressure on the bacterial strains circulating in the population caused by vaccination. It is also believed that the shift from whole cell pertussis vaccine (DTwP) to acellular pertussis vaccine (DTaP) led to a rise in pertussis cases. DTaP replaced the DTwP in most countries during the 1990s, when the disease became more frequent. DTaP is supposed to produce short-lived immunity, which means that adolescents and adults would not be protected from B. pertussis. Other theories include improved reporting of cases secondary to increased awareness, the use of PCR assays for diagnosis, and pockets of populations with high rates of vaccination refusal.3,4,9-10.
The clinical manifestation of pertussis depends on the patients’ age, any previous immunization or infection, co-infection with other respiratory infectious agents, the presence of passively acquired antibodies, and perhaps other factors related to the host and organism, such as virulence. The disease is usually characterized by three distinct stages. The first one is called the catarrhal stage, which takes 1–2 weeks and is marked by mild respiratory symptoms (low fever, runny nose, and malaise), progressing towards whooping cough. The second stage, called paroxysmal, has the duration of 2–6 weeks and is characterized by episodes of paroxysmal coughing and high-pitched whoop, which may be accompanied by cyanosis and vomiting. This phase evolves to the convalescent stage, when the patient remains with a persistent cough with no paroxysms for about 2–6 weeks.2,11
Whooping cough can be severe and life-threatening in young children, particularly in children younger than 6 months, and in not fully immunized individuals. Fifty percent of children younger than 1 year old with pertussis are hospitalized and subject to a diverse range of complications. Apnea is the commonest complication in around 60% of hospitalized children under 12 months old, followed by pneumonia, seizures, encephalopathy, and death due to cough or toxins. Infants under the age of the first vaccination dose are substantially prone to a fatal outcome.12-14
Fulminant pertussis, is another clinical presentation of whooping cough, which is defined by a rapidly evolving combination of pneumonia, cardiopulmonary failure, neurologic involvement, and severe pulmonary hypertension, which quite frequently leads to death.12 Such a presentation is more common in infants younger than 1 year old, who usually acquire the infection from housemate adults with an incomplete vaccination calendar. The most accepted pathogenetic hypothesis for this form of pertussis relies on the direct pulmonary damage caused by B. pertussis toxins coupled with the hyperviscosity syndrome due to the peripheral leukocytosis, pulmonary hypertension due to the presence of widespread leukocyte thrombi throughout the pulmonary vascular bed, and consequent hypoxia.15,16 Our case was characterized by severe respiratory insufficiency, pulmonary hypertension and marked leukocytosis.
Paddock et al.16 studied respiratory tissue specimens of 15 autopsy cases of fulminant pertussis in infants aged younger than 4 months. The main histopathological findings were tracheitis, bronchitis and necrotizing bronchiolitis, alveolar edema and hemorrhage, diffuse alveolar damage, neutrophilic pneumonia, interlobular septal edema, and angiolymphatic leukocyte aggregates. Clusters of Gram-negative coccobacilli were also identified within the bronchiolar epithelia and in alveolar lumens. Another retrospective study of 10 autopsy cases also described lymphocytic depletion in lymph nodes, thymus, and spleen. Other findings included hepatic congestion and fatty changes, as well as acute tubular necrosis.17 According to Paddock et al.,16 B. pertussis pneumonia may trigger a cascade of events that includes hypoxia, acidosis, and acute pulmonary vasoconstriction, which, combined with pertussis toxin-mediated leukocytosis, contributes to the restriction of pulmonary blood flow. These compounded effects produce marked pressure elevation in the vasculature of the infant lung that exacerbates hypoxemia and ultimately causes cardiac failure, shock, and acute respiratory distress.16 The autopsy findings of our case are in concordance with the literature, thence representing a typical case of fulminant pertussis.
The Center of Disease Control defines a case of pertussis when the patient presents a cough for 2 or more weeks associated with one of the following symptoms: paroxysms of coughing, inspiratory whoop, post-tussive vomiting, or apnea (with or without cyanosis—for infants aged < 1 year). The final diagnosis is made with the isolation of B. pertussis in culture from nasopharyngeal specimens or with the PCR positivity from respiratory secretion. Marked leukocytosis with lymphocytosis (especially during the paroxysmal stage) is another laboratorial finding in the presence of a radiological image of pneumonia. The average count of leukocytes can reach 30,000–40,000 with 60–80% of lymphocytes.3,14 Marked leukocytosis (white blood counts > 100,000/mm3) in patients aged younger than 2 months represents a poor outcome predictor.15 Despite the typical pattern on presentation and the laboratory studies, pertussis is under-recognized in intensive care, with only 28% of the cases being suspected when admitted in the pediatric intensive care unit (PICU).18
The antibiotic therapy, involving the macrolides (mainly azithromycin) or trimethopim-sulfamethoxazole in case of intolerance, can reduce the intensity of the symptoms and the illness duration.13 In cases of fulminant disease due to hyperviscosity syndrome (due to leukocytosis), treatment modalities that reduce the number of leukocytes, such as exchange transfusion or leukapheresis, may be associated with a better outcome. Extracorporeal membrane oxygenation can be used as a treatment for pulmonary hypertension and hyperviscosity syndrome; however, discouraging outcomes have been reported.15,19
The primary prophylaxis is made with the administration of vaccine against the B. pertussis, which is already included in the Brazilian public immunization calendar. Usually, the basic immunization against pertussis includes three doses of the vaccine in the first year of life, followed by a fourth dose during the preschool years.20 The vaccine has efficacy of around 75–80%, but the protection declines over the years. Following the policy adopted in the USA14, in 2014, the Brazilian Health Ministry also advocated the vaccination of all pregnant women after 27 weeks of gestational age with DtaP (diphtheria, tetanus and pertussis) vaccine.21 This policy foresees a reduction in the incidence of the disease among children younger than 1 year of age, especially those under 6 months, due to the vertical immunization.22
Physicians should be aware of this re-emerging disease, mainly when faced with very young children with respiratory symptoms. Survival may be dependent on the earliest and adequate therapeutic management. An effective immunization program is of paramount importance to reduce the incidence and severity of this disease.
Footnotes
Della Torre JAG, Benevides GN, Melo AMAGP, Ferreira CR. Pertussis: the resurgence of a public health threat. Autopsy Case Rep [Internet]. 2015;5(2):9-16. http://dx.doi.org/10.4322/acr.2015.006
REFERENCES
- 1.Bisgard KM, Pascual FB, Ehresmann KR, et al. Infant pertussis: who was the source? Pediatr Infect Dis J. 2004;23(11):985-9. 10.1097/01.inf.0000145263.37198.2b. [DOI] [PubMed] [Google Scholar]
- 2.Wendelboe AM, Njamkepo E, Bourillon A, et al. Transmission of Bordetella pertussis to young infants. Pediatr Infect Dis J. 2007;26(4):293-9. 10.1097/01.inf.0000258699.64164.6d. [DOI] [PubMed] [Google Scholar]
- 3.Jakinovich A, Sood SK. Pertussis: still a cause of death, seven decades into vaccination. Curr Opin Pediatr. 2014;26(5):597-604. 10.1097/MOP.0000000000000139. [DOI] [PubMed] [Google Scholar]
- 4.Sizaire V, Garrido-Estepa M, Masa-Calles J, Martinez de Aragon MV. Increase of pertussis incidence in 2010 to 2012 after 12 years of low circulation in Spain. Euro Surveill. 2014;19(32):20875. 10.2807/1560-7917.ES2014.19.32.20875. [DOI] [PubMed] [Google Scholar]
- 5.Brasil Ministério da Saúde. Portal da Saúde Coqueluche [Internet]. Brasília; 2014. [cited 2015 Apr 12]. Available from: http://portalsaude.saude.gov.br/index.php/o-ministerio/principal/secretarias/svs/coqueluche [Google Scholar]
- 6.Torres RSLA, Santos TZ, Torres RAA, et al. Resurgence of pertussis at the age of vaccination: clinical, epidemiological, and molecular aspects. J Pediatr. 2015;S0021-7557(15)00006-6. [DOI] [PubMed] [Google Scholar]
- 7.Centro de Vigilância Epidemiológica Prof. Alexandre Vranjac (CVE) Informe técnico Coqueluche-2011: atualizacão da situacão epidemiológica. São Paulo: Divisão de Doenças de Transmissão Respiratória; 2011. [cited 14 Dec 2013]. Available from: http://www.cve.saude.sp.gov.br/htm/resp/pdf/IF11_COQUELUCHE.pdf [Google Scholar]
- 8.Brasil Ministerio da Saúde Sistema de Informação de Agravos de Notificação (Sinan Net) Coqueluche [Internet]. Brasília; 2014. [cited 2015 May 2]. Available from http://dtr2004.saude.gov.br/sinanweb/tabnet/dh?sinannet/coqueluche/bases/coquebrnet.def [Google Scholar]
- 9.Syed MA, Bana NF. Pertussis. A reemerging and an underreported infectious disease. Saudi Med J. 2014;35(10):1181-7. [PMC free article] [PubMed] [Google Scholar]
- 10.Chiappini E, Stival A, Galli L, de Martino M. Pertussis re-emergence in the post-vaccination era. BMC Infect Dis. 2013;13(1):151. 10.1186/1471-2334-13-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saffar MJ, Hashemi A, Ghorbani GR, Rezai MS, Shahmohammadi S, Shojaei J. Clinical and laboratory features of pertussis in hospitalized infants with confirmed versus probable pertussis cases. Ann Med Health Sci Res. 2014;4(6):910-4. 10.4103/2141-9248.144911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC) Pertusis [Internet]. Atlanta; 2014. [cited 2015 Apr 12]. Available from: http://www.cdc.gov/pertussis/surv-reporting.html [Google Scholar]
- 13.Namachivayam P, Shimizu K, Butt W. Pertussis: severe clinical presentation in pediatric intensive care and its relation to outcome. Pediatr Crit Care Med. 2007;8(3):207-11. 10.1097/01.PCC.0000265499.50592.37. [DOI] [PubMed] [Google Scholar]
- 14.Mikelova LK, Halperin SA, Scheifele D, et al. Predictors of death in infants hospitalized with pertussis: a case-control study of 16 pertussis deaths in Canada. J Pediatr. 2003;143(5):576-81. 10.1067/S0022-3476(03)00365-2. [DOI] [PubMed] [Google Scholar]
- 15.Paksu MŞ, Akgün M, Karadağ A, Aşılıoğlu N, Belet N, Şensoy G. Fulminant pertussis in very young infants: two cases and review of the literature. Turk J Pediatr. 2013;55(4):426-9. [PubMed] [Google Scholar]
- 16.Paddock CD, Sanden GN, Cherry JD, et al. Pathology and pathogenesis of fatal Bordetella pertussis infection in infants. Clin Infect Dis. 2008;47(3):328-38. 10.1086/589753. [DOI] [PubMed] [Google Scholar]
- 17.Sawal M, Cohen M, Irazuzta JE, et al. Fulminant pertussis: a multi-center study with new insights into the clinico-pathological mechanisms. Pediatr Pulmonol. 2009;44(10):970-80. 10.1002/ppul.21082. [DOI] [PubMed] [Google Scholar]
- 18.Crowcroft NS, Booy R, Harrison T, et al. Severe and unrecognised: pertussis in UK infants. Arch Dis Child. 2003;88(9):802-6. 10.1136/adc.88.9.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Forsyth K, Nagai M, Lepetic A, Trindade E. Pertussis immunization in the global pertussis initiative international region: recommended strategies and implementation considerations. Pediatr Infect Dis J. 2005;24(5, Suppl):S93-7. 10.1097/01.inf.0000160921.74004.12. [DOI] [PubMed] [Google Scholar]
- 20.Kline JM, Lewis WD, Smith EA, Tracy LR, Moerschel SK. Pertussis: a reemerging infection. Am Fam Physician. 2013;88(8):507-14. [PubMed] [Google Scholar]
- 21.Centro de Vigilância Epidemiológica (CVE) Informe Técnico dTp-a [Internet]. São Paulo; 2014. [cited 2015 Mar 12]. Available from: http://www.cve.saude.sp.gov.br/htm/imuni/pdf/IF14_VAC_DTpa.pdf [Google Scholar]
- 22.Laenen J, Roelants M, Devlieger R, Vandermeulen C. Influenza and pertussis vaccination coverage in pregnant women. Vaccine. 2015;33(18):2125-31. 10.1016/j.vaccine.2015.03.020. [DOI] [PubMed] [Google Scholar]