In 2010, the top five causes of death in the United States were 1) diseases of the heart, 2) cancer, 3) chronic lower respiratory diseases, 4) cerebrovascular diseases (stroke), and 5) unintentional injuries (1). The rates of death from each cause vary greatly across the 50 states and the District of Columbia (2). An understanding of state differences in death rates for the leading causes might help state health officials establish disease prevention goals, priorities, and strategies. States with lower death rates can be used as benchmarks for setting achievable goals and calculating the number of deaths that might be prevented in states with higher rates. To determine the number of premature annual deaths for the five leading causes of death that potentially could be prevented (“potentially preventable deaths”), CDC analyzed National Vital Statistics System mortality data from 2008–2010. The number of annual potentially preventable deaths per state before age 80 years was determined by comparing the number of expected deaths (based on average death rates for the three states with the lowest rates for each cause) with the number of observed deaths. The results of this analysis indicate that, when considered separately, 91,757 deaths from diseases of the heart, 84,443 from cancer, 28,831 from chronic lower respiratory diseases, 16,973 from cerebrovascular diseases (stroke), and 36,836 from unintentional injuries potentially could be prevented each year. In addition, states in the Southeast had the highest number of potentially preventable deaths for each of the five leading causes. The findings provide disease-specific targets that states can use to measure their progress in preventing the leading causes of deaths in their populations.
Mortality data from the National Vital Statistics System for the period 2008–2010 were analyzed. Population estimates for the period 2008–2010 were produced by the U.S. Census Bureau in collaboration with the National Center for Health Statistics. The calculations of potentially preventable deaths were restricted to U.S. residents and to deaths that occurred to persons aged <80 years. The age restriction is consistent with average life expectancy for the total U.S. population, which was nearly 79 years in 2010 (2). Analysis was restricted to deaths with an underlying cause of death among the five leading causes, based on International Classification of Diseases, 10th Revision (ICD-10) codes: diseases of the heart codes (I00–I09, I11, I13, I20–I51), cancer (C00–C97), chronic lower respiratory diseases (J40–J47), cerebrovascular diseases (stroke) (I60–I69), and unintentional injuries (V01–X59, Y85–Y86). The five leading causes of death represented 63% of all deaths in 2010; the next five most frequent causes accounted for only about 12% of deaths (2).
The annual number of potentially preventable deaths for each of the five leading causes of death by state was calculated in three steps. The first step was to calculate and rank state disease-specific death rates by age group. Ages were initially grouped by 10-year increments, from 0–9 years through 70–79 years. However, these 10-year age groups, especially at the younger ages, frequently did not have enough deaths reported to be statistically reliable. Therefore, adjacent 10 year-age groups with small numbers of deaths were combined until enough deaths were aggregated to achieve reliability. For chronic lower respiratory diseases, for example, the age groupings were 0–49, 50–59, 60–69, and 70–79 years. The three states with the lowest observed death rates for each age group-specific cause of death category were then selected and their death rates averaged to calculate a lowest average age-specific death rate for each cause of death. The average of the lowest three states was chosen to minimize the effect of any extreme outlier and to represent the low end of the distribution of death rates among the states. The second step was to calculate expected deaths for each age group and state by multiplying the age-specific state populations by the lowest three-state average age-specific death rate for each cause. Total expected deaths for each cause per state were then calculated by summing expected deaths over all age groups up to age 79 years. Finally, the potentially preventable deaths were calculated by subtracting expected deaths from observed deaths. In instances where the result would be a negative number of potentially preventable deaths because the existing state rate was lower than the average of the three lowest states, the state’s potentially preventable deaths were set to zero. Results are presented by state and by the 10 U.S. Department of Health and Human Services regions.*
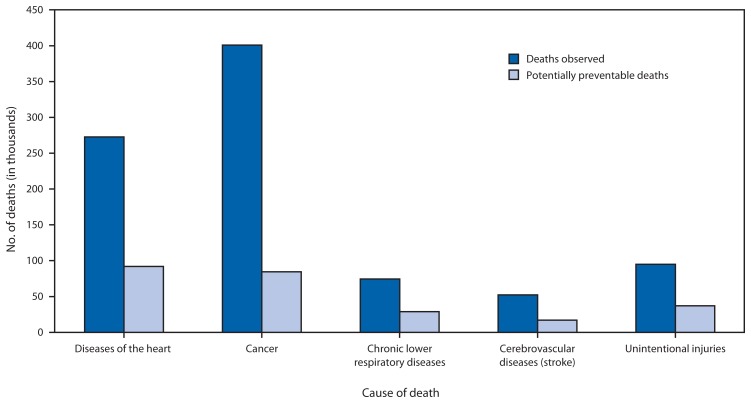
During the period from 2008 to 2010, the average number of annual deaths from the five leading causes of death in persons aged <80 years was 895,317. This number represents 66% of annual deaths from all causes. The estimated average number of potentially preventable deaths for the five leading causes of death in persons aged <80 years were 91,757 for diseases of the heart, 84,443 for cancer, 28,831 for chronic lower respiratory diseases, 16,973 for cerebrovascular diseases (stroke), and 36,836 for unintentional injuries (Table 1). The Southeast (Region IV) had the highest number of potentially preventable deaths for all five leading causes of death (Table 2). The proportion of potentially preventable deaths among observed deaths for each of the five causes of death were 34% for diseases of the heart, 21% for cancer, 39% for chronic lower respiratory diseases, 33% for cerebrovascular diseases (stroke), and 39% for unintentional injuries (Figure).
TABLE 1.
Annual number of deaths expected,* observed, and potentially preventable† for the five leading cause of death for persons aged <80 years, by state/area — United States, 2008–2010
| Diseases of the heart | Cancer | Chronic lower respiratory diseases | Cerebrovascular diseases (stroke) | Unintentional injuries | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|||||||||||
| State/Area | Deaths observed | Deaths expected | Potentially preventable deaths | Deaths observed | Deaths expected | Potentially preventable deaths | Deaths observed | Deaths expected | Potentially preventable deaths | Deaths observed | Deaths expected | Potentially preventable deaths | Deaths observed | Deaths expected | Potentially preventable deaths |
| Alabama | 6,604 | 2,993 | 3,611 | 7,595 | 5,227 | 2,368 | 1,778 | 765 | 1,013 | 1,277 | 588 | 689 | 2,036 | 910 | 1,126 |
| Alaska | 463 | 331 | 132 | 703 | 588 | 115 | 112 | 77 | 35 | 91 | 62 | 29 | 331 | 131 | 200 |
| Arizona | 4,735 | 3,885 | 850 | 7,460 | 6,775 | 685 | 1,558 | 1,004 | 554 | 848 | 771 | 77 | 2,341 | 1,191 | 1,150 |
| Arkansas | 3,808 | 1,845 | 1,963 | 4,720 | 3,219 | 1,501 | 1,101 | 476 | 625 | 718 | 365 | 353 | 1,221 | 551 | 670 |
| California | 24,707 | 19,742 | 4,965 | 38,226 | 34,454 | 3,772 | 6,047 | 4,904 | 1,143 | 5,366 | 3,839 | 1,527 | 8,627 | 6,886 | 1,741 |
| Colorado | 2,815 | 2,707 | 108 | 4,944 | 4,752 | 192 | 1,141 | 665 | 476 | 604 | 520 | 84 | 1,525 | 940 | 585 |
| Connecticut | 2,569 | 2,176 | 393 | 4,367 | 3,805 | 562 | 509 | 544 | 0 | 425 | 420 | 5 | 905 | 679 | 226 |
| Delaware | 857 | 575 | 282 | 1,352 | 1,006 | 346 | 224 | 147 | 77 | 170 | 113 | 57 | 296 | 172 | 124 |
| DC | 729 | 310 | 419 | 742 | 543 | 199 | 73 | 78 | 0 | 107 | 61 | 46 | 169 | 117 | 52 |
| Florida | 17,586 | 13,352 | 4,234 | 28,249 | 23,195 | 5,054 | 5,327 | 3,501 | 1,826 | 3,481 | 2,655 | 826 | 6,927 | 3,675 | 3,252 |
| Georgia | 9,103 | 5,120 | 3,983 | 11,820 | 8,967 | 2,853 | 2,413 | 1,263 | 1,150 | 1,965 | 989 | 976 | 3,133 | 1,791 | 1,342 |
| Hawaii | 1,007 | 836 | 171 | 1,555 | 1,467 | 88 | 141 | 212 | 0 | 244 | 163 | 81 | 344 | 259 | 85 |
| Idaho | 1,080 | 883 | 197 | 1,753 | 1,546 | 207 | 409 | 224 | 185 | 234 | 174 | 60 | 516 | 285 | 231 |
| Illinois | 11,424 | 7,249 | 4,175 | 16,558 | 12,654 | 3,904 | 2,740 | 1,815 | 925 | 2,047 | 1,412 | 635 | 3,093 | 2,395 | 698 |
| Indiana | 6,421 | 3,783 | 2,638 | 9,385 | 6,612 | 2,773 | 2,154 | 954 | 1,200 | 1,240 | 739 | 501 | 2,064 | 1,209 | 855 |
| Iowa | 2,716 | 1,892 | 824 | 4,127 | 3,295 | 832 | 859 | 485 | 374 | 462 | 373 | 89 | 892 | 571 | 321 |
| Kansas | 2,248 | 1,636 | 612 | 3,624 | 2,854 | 770 | 826 | 414 | 412 | 485 | 321 | 164 | 1,010 | 525 | 485 |
| Kentucky | 5,332 | 2,662 | 2,670 | 7,499 | 4,655 | 2,844 | 1,792 | 675 | 1,117 | 934 | 520 | 414 | 2,240 | 826 | 1,414 |
| Louisiana | 5,784 | 2,609 | 3,175 | 6,909 | 4,562 | 2,347 | 1,106 | 658 | 448 | 1,003 | 510 | 493 | 1,771 | 850 | 921 |
| Maine | 1,083 | 928 | 155 | 2,259 | 1,627 | 632 | 443 | 237 | 206 | 229 | 180 | 49 | 390 | 262 | 128 |
| Maryland | 5,321 | 3,303 | 2,018 | 7,218 | 5,788 | 1,430 | 1,035 | 818 | 217 | 935 | 636 | 299 | 1,065 | 1,093 | 0 |
| Massachusetts | 4,416 | 3,926 | 490 | 8,319 | 6,865 | 1,454 | 1,115 | 984 | 131 | 807 | 761 | 46 | 1,507 | 1,252 | 255 |
| Michigan | 10,327 | 6,056 | 4,271 | 14,394 | 10,600 | 3,794 | 2,721 | 1,527 | 1,194 | 1,743 | 1,178 | 565 | 2,923 | 1,869 | 1,054 |
| Minnesota | 2,720 | 3,050 | 0 | 6,273 | 5,328 | 945 | 960 | 762 | 198 | 662 | 592 | 70 | 1,342 | 993 | 349 |
| Mississippi | 4,183 | 1,750 | 2,433 | 4,731 | 3,055 | 1,676 | 1,016 | 446 | 570 | 827 | 344 | 483 | 1,395 | 553 | 842 |
| Missouri | 6,553 | 3,691 | 2,862 | 9,023 | 6,442 | 2,581 | 2,090 | 941 | 1,149 | 1,164 | 724 | 440 | 2,328 | 1,133 | 1,195 |
| Montana | 826 | 650 | 176 | 1,304 | 1,143 | 161 | 341 | 166 | 175 | 162 | 127 | 35 | 416 | 190 | 226 |
| Nebraska | 1,252 | 1,063 | 189 | 2,254 | 1,852 | 402 | 543 | 270 | 273 | 294 | 209 | 85 | 490 | 337 | 153 |
| Nevada | 2,903 | 1,566 | 1,337 | 3,370 | 2,743 | 627 | 701 | 395 | 306 | 446 | 305 | 141 | 952 | 510 | 442 |
| New Hampshire | 916 | 828 | 88 | 1,772 | 1,455 | 317 | 315 | 206 | 109 | 163 | 158 | 5 | 381 | 255 | 126 |
| New Jersey | 7,106 | 5,243 | 1,863 | 10,948 | 9,147 | 1,801 | 1,436 | 1,312 | 124 | 1,319 | 1,015 | 304 | 1,888 | 1,665 | 223 |
| New Mexico | 1,510 | 1,253 | 257 | 2,393 | 2,194 | 199 | 535 | 320 | 215 | 310 | 246 | 64 | 1,013 | 386 | 627 |
| New York | 17,371 | 11,522 | 5,849 | 23,787 | 20,112 | 3,675 | 3,358 | 2,906 | 452 | 2,423 | 2,246 | 177 | 3,804 | 3,692 | 112 |
| North Carolina | 9,021 | 5,679 | 3,342 | 13,297 | 9,931 | 3,366 | 2,698 | 1,436 | 1,262 | 1,894 | 1,108 | 786 | 3,268 | 1,802 | 1,466 |
| North Dakota | 512 | 406 | 106 | 780 | 708 | 72 | 170 | 104 | 66 | 127 | 80 | 47 | 193 | 127 | 66 |
| Ohio | 11,875 | 7,164 | 4,711 | 17,413 | 12,514 | 4,899 | 3,729 | 1,818 | 1,911 | 2,271 | 1,400 | 871 | 4,016 | 2,184 | 1,832 |
| Oklahoma | 4,857 | 2,267 | 2,590 | 5,787 | 3,957 | 1,830 | 1,736 | 581 | 1,155 | 889 | 448 | 441 | 1,870 | 703 | 1,167 |
| Oregon | 2,421 | 2,364 | 57 | 5,212 | 4,153 | 1,059 | 1,110 | 599 | 511 | 635 | 461 | 174 | 1,068 | 730 | 338 |
| Pennsylvania | 12,668 | 8,221 | 4,447 | 19,114 | 14,340 | 4,774 | 3,051 | 2,101 | 950 | 2,194 | 1,611 | 583 | 4,319 | 2,435 | 1,884 |
| Rhode Island | 820 | 636 | 184 | 1,423 | 1,112 | 311 | 225 | 160 | 65 | 148 | 123 | 25 | 339 | 200 | 139 |
| South Carolina | 5,413 | 2,896 | 2,517 | 7,063 | 5,079 | 1,984 | 1,391 | 740 | 651 | 1,119 | 567 | 552 | 1,910 | 883 | 1,027 |
| South Dakota | 590 | 491 | 99 | 1,054 | 856 | 198 | 226 | 126 | 100 | 126 | 97 | 29 | 284 | 151 | 133 |
| Tennessee | 7,956 | 3,916 | 4,040 | 10,185 | 6,853 | 3,332 | 2,197 | 995 | 1,202 | 1,463 | 765 | 698 | 2,895 | 1,209 | 1,686 |
| Texas | 19,939 | 12,683 | 7,256 | 27,141 | 22,143 | 4,998 | 5,061 | 3,139 | 1,922 | 4,254 | 2,471 | 1,783 | 7,612 | 4,551 | 3,061 |
| Utah | 1,229 | 1,194 | 35 | 1,931 | 2,080 | 0 | 383 | 298 | 85 | 282 | 238 | 44 | 765 | 470 | 295 |
| Vermont | 482 | 411 | 71 | 921 | 723 | 198 | 167 | 103 | 64 | 91 | 79 | 12 | 181 | 122 | 59 |
| Virginia | 6,588 | 4,609 | 1,979 | 10,162 | 8,073 | 2,089 | 1,647 | 1,148 | 499 | 1,369 | 891 | 478 | 1,889 | 1,521 | 368 |
| Washington | 4,437 | 3,844 | 593 | 8,193 | 6,754 | 1,439 | 1,451 | 956 | 495 | 907 | 743 | 164 | 1,925 | 1,269 | 656 |
| West Virginia | 2,400 | 1,308 | 1,092 | 3,415 | 2,289 | 1,126 | 921 | 338 | 583 | 464 | 257 | 207 | 1,031 | 364 | 667 |
| Wisconsin | 4,513 | 3,424 | 1,089 | 7,530 | 5,978 | 1,552 | 1,190 | 862 | 328 | 869 | 667 | 202 | 1,666 | 1,074 | 592 |
| Wyoming | 492 | 333 | 159 | 695 | 585 | 110 | 186 | 83 | 103 | 73 | 65 | 8 | 296 | 106 | 190 |
| Total | 272,688 | 181,261 | 91,757 | 400,949 | 316,652 | 84,443 | 74,458 | 45,738 | 28,831 | 52,360 | 35,390 | 16,973 | 94,862 | 58,055 | 36,836 |
Abbreviation: DC = District of Columbia.
Expected deaths are the lowest three-state average age-specific death rate times the age-specific state population rounded to the nearest whole number.
Potentially preventable deaths are observed deaths minus expected deaths rounded to the nearest whole number.
TABLE 2.
Annual number of deaths expected,* observed, and potentially preventable† for the five leading cause of death for persons aged <80 years, by U.S. Department of Health and Human Services region§ — United States, 2008–2010
| Diseases of the heart | Cancer | Chronic lower respiratory diseases | Cerebrovascular diseases (stroke) | Unintentional injuries | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|||||||||||
| Region | Deaths observed | Deaths expected | Potentially preventable deaths | Deaths observed | Deaths expected | Potentially preventable deaths | Deaths observed | Deaths expected | Potentially preventable deaths | Deaths observed | Deaths expected | Potentially preventable deaths | Deaths observed | Deaths expected | Potentially preventable deaths |
| 1 | 10,286 | 8,904 | 1,382 | 19,061 | 15,587 | 3,474 | 2,774 | 2,234 | 540 | 1,863 | 1,722 | 141 | 3,703 | 2,771 | 932 |
| 2 | 24,477 | 16,765 | 7,712 | 34,735 | 29,259 | 5,476 | 4,794 | 4,218 | 576 | 3,742 | 3,261 | 481 | 5,692 | 5,357 | 335 |
| 3 | 28,563 | 18,327 | 10,236 | 42,003 | 32,039 | 9,964 | 6,951 | 4,630 | 2,321 | 5,239 | 3,568 | 1,671 | 8,769 | 5,703 | 3,066 |
| 4 | 65,198 | 38,367 | 26,831 | 90,439 | 66,962 | 23,477 | 18,612 | 9,820 | 8,792 | 12,960 | 7,538 | 5,422 | 23,804 | 11,650 | 12,154 |
| 5 | 47,280 | 30,726 | 16,554 | 71,553 | 53,686 | 17,867 | 13,494 | 7,740 | 5,754 | 8,832 | 5,988 | 2,844 | 15,104 | 9,724 | 5,380 |
| 6 | 35,898 | 20,656 | 15,242 | 46,950 | 36,074 | 10,876 | 9,539 | 5,174 | 4,365 | 7,174 | 4,040 | 3,134 | 13,487 | 7,040 | 6,447 |
| 7 | 12,769 | 8,281 | 4,488 | 19,028 | 14,443 | 4,585 | 4,318 | 2,111 | 2,207 | 2,405 | 1,628 | 777 | 4,720 | 2,566 | 2,154 |
| 8 | 6,464 | 5,782 | 682 | 10,708 | 10,123 | 585 | 2,447 | 1,442 | 1,005 | 1,374 | 1,128 | 246 | 3,479 | 1,985 | 1,494 |
| 9 | 33,352 | 26,030 | 7,322 | 50,611 | 45,439 | 5,172 | 8,447 | 6,514 | 1,933 | 6,904 | 5,078 | 1,826 | 12,264 | 8,845 | 3,419 |
| 10 | 8,401 | 7,422 | 979 | 15,861 | 13,041 | 2,820 | 3,082 | 1,857 | 1,225 | 1,867 | 1,439 | 428 | 3,840 | 2,414 | 1,426 |
| Total | 272,688 | 181,261 | 91,428 | 400,949 | 316,652 | 84,296 | 74,458 | 45,738 | 28,718 | 52,360 | 35,390 | 16,970 | 94,862 | 58,055 | 36,807 |
Expected deaths are the lowest three-state average age-specific death rate times the age-specific state population rounded to the nearest whole number. Differences between Table 1 and Table 2 are the result of rounding error when calculating states individually or by region.
Potentially preventable deaths are observed deaths minus expected deaths rounded to the nearest whole number.
Region 1: Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont. Region 2: New Jersey, New York, Puerto Rico, and the U.S. Virgin Islands. Region 3: Delaware, the District of Columbia, Maryland, Pennsylvania, Virginia, and West Virginia. Region 4: Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, and Tennessee. Region 5: Illinois, Indiana, Michigan, Minnesota, Ohio, and Wisconsin. Region 6: Arkansas, Louisiana, New Mexico, Oklahoma, and Texas. Region 7: Iowa, Kansas, Missouri, and Nebraska. Region 8: Colorado, Montana, North Dakota, South Dakota, Utah, and Wyoming. Region 9: Arizona, California, Hawaii, Nevada, American Samoa, Commonwealth of the Northern Mariana Islands, Federated States of Micronesia, Guam, Marshall Islands, and Republic of Palau. Region 10: Alaska, Idaho, Oregon, and Washington. Additional information available at http://www.hhs.gov/about/regionmap.html.
FIGURE.
Annual number of deaths observed and potentially preventable* for the five leading cause of death for persons aged <80 years — United States, 2008–2010
* Potentially preventable deaths are observed deaths minus expected deaths (the lowest three-state average age-specific death rate times the age-specific state population) rounded to the nearest whole number.
Discussion
Death rates are population health outcome measures that reflect the combined influences of multiple biological and social health determinants, public health efforts, and medical care. Examining which diseases and injuries result in the greatest number of deaths in populations, particularly for deaths that occur earlier than expected, allows health officials to establish disease prevention goals, priorities, and strategies. In the United States, the largest number of deaths during 2008–2010 occurred from diseases of the heart, cancer, chronic lower respiratory diseases, cerebrovascular diseases (stroke), and unintentional injuries (1). The results of this study demonstrate that if all states achieved the lowest observed mortality levels for the five leading causes, when considered separately, as many as 91,757 premature heart disease deaths, 84,443 cancer deaths, 28,831 chronic lower respiratory disease deaths, 16,973 stroke deaths, and 36,836 unintentional injury deaths might be prevented each year. These calculations translate to approximately one in three premature heart disease deaths, one in five premature cancer deaths, two out of five chronic lower respiratory disease deaths, one out of every three stroke deaths, and two out of every five unintentional injury deaths that could be prevented.
Reducing the number of earlier than expected deaths from the leading causes of death requires risk factor reduction, screening, early intervention, and successful treatment of the disease or injury. For the five leading causes of death, the major modifiable risk factors include 1) diseases of the heart: tobacco use, high blood pressure, high blood cholesterol, type 2 diabetes, poor diet, being overweight, and lack of physical activity (3); 2) cancer: tobacco use, poor diet, lack of physical activity, being overweight, sun exposure, certain hormones, alcohol, some viruses and bacteria, ionizing radiation, and certain chemicals and other substances (4); 3) chronic lower respiratory diseases: tobacco smoke, second hand smoke exposure, other indoor air pollutants, outdoor air pollutants, allergens, and occupational agents (5); 4) cerebrovascular diseases (stroke): high blood pressure, high blood cholesterol, heart disease, diabetes, being overweight, tobacco use, alcohol use, and lack of physical activity (6); and 5) unintentional injuries: lack of vehicle restraint use, lack of motorcycle helmet use, unsafe consumer products, drug and alcohol use (including prescription drug misuse), exposure to occupational hazards, and unsafe home and community environments (7).
The majority of these risk factors do not occur randomly in populations; they are closely aligned with the social, demographic, environmental, economic, and geographic attributes of the neighborhoods in which people live and work (8). However, the calculation of potentially preventable deaths in this study did not account for differences in the attributes of states that might influence risk factors and ultimately death rates, such as proportion of the population below the poverty level. If health disparities were eliminated, as is called for by Healthy People 2020 (9), all states should be closer to achieving the lowest possible death rates for the five leading causes of death.
The findings in this report are subject to at least four limitations. First, uncertainty and error in the diagnosis and reporting of cause of death might result in errors in death rate estimations for some causes of death. Second, state affiliation is based on the person’s residency at the time of death. With the exception of unintentional injuries, the factors that led to the resulting cause of death for some persons might have accumulated over a lifetime spent in different geographic locations. Third, the potentially preventable deaths are based on existing levels of state performance for the three states with the lowest death rates for each condition and might underestimate the benefit if these three states made full use of optimal health promotion and disease prevention strategies. Finally, to the extent that natural (i.e., random) variability in state death rates from year to year is responsible for the selection of the three states with the lowest death rates, there will be a tendency to regress to the mean. The method used tends to slightly overestimate the number of potentially preventable deaths. Nevertheless, the random component of the variation in state death rates is minimal and any bias is also minimal.
What is already known on this topic?
The top five causes of death in the United States are diseases of the heart, cancer, chronic lower respiratory diseases, cerebrovascular diseases (stroke), and unintentional injuries. Death rates for these diseases vary widely across the states because of the distribution of health determinants, access and use of health services, and public health efforts.
What is added by this report?
This report demonstrates that if all states could achieve the lowest observed death rates for the five leading causes, when considered separately, as many as 91,757 premature heart disease deaths, 84,443 cancer deaths, 28,831 chronic lower respiratory disease deaths, 16,973 stroke deaths, and 36,836 unintentional injury deaths might be prevented in the United States each year.
What are the implications for public health practice?
State health officials can use the lower death rates as benchmarks to establish disease prevention goals, priorities, and strategies. Reducing the number of earlier than expected deaths from the leading causes of death requires the joint effort of public health and heath-care organizations and personnel to support risk factor prevention and reduction, screening, early intervention, and successful treatment of diseases or injuries.
As a further note of caution, potentially preventable deaths cannot be added across causes of death by state or for the nation as a whole because of competing risks. For example, for a state that has been able to reduce its heart disease mortality, some premature deaths will be prevented altogether, but others will be pushed to different causes of death. A person who avoids death from heart disease might then be exposed to a higher risk for dying from injury or cancer. The result is that there is less variation by state in the death rate for all causes combined than for any particular cause of death.
States can use the disease-specific aspirational goals for potentially preventable deaths presented in this report in several ways. They can identify other states with similar populations but better outcomes and examine what those are doing differently to address the leading causes of death. Although each state has a unique set of factors that determine health outcomes, states might find neighboring states or states within their region as good sources of information on effective policies, programs, and services. The goals can also be used to educate state policymakers and leaders about what is achievable if they were able to match the best state outcomes.
Footnotes
Region 1: Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, and Vermont. Region 2: New Jersey, New York, Puerto Rico, and the U.S. Virgin Islands. Region 3: Delaware, the District of Columbia, Maryland, Pennsylvania, Virginia, and West Virginia. Region 4: Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, and Tennessee. Region 5: Illinois, Indiana, Michigan, Minnesota, Ohio, and Wisconsin. Region 6: Arkansas, Louisiana, New Mexico, Oklahoma, and Texas. Region 7: Iowa, Kansas, Missouri, and Nebraska. Region 8: Colorado, Montana, North Dakota, South Dakota, Utah, and Wyoming. Region 9: Arizona, California, Hawaii, Nevada, American Samoa, Commonwealth of the Northern Mariana Islands, Federated States of Micronesia, Guam, Marshall Islands, and Republic of Palau. Region 10: Alaska, Idaho, Oregon, and Washington. Additional information available at http://www.hhs.gov/about/regionmap.html.
References
- 1.Hoyert DL, Xu JQ. Deaths: preliminary data for 2011. Natl Vital Stat Rep. 2012;61(6) [PubMed] [Google Scholar]
- 2.Murphy SL, Xu JQ, Kochanek KD. Deaths: final data for 2010. Natl Vital Stat Rep. 2013;61(4) [PubMed] [Google Scholar]
- 3.National Heart Lung and Blood Institute. What are the risk factors for heart disease? Washington, DC: National Institutes of Health; 2012. Available at http://www.nhlbi.nih.gov/educational/hearttruth/lower-risk/risk-factors.htm. [Google Scholar]
- 4.National Cancer Institute. Prevention, genetics, causes. Washington, DC: National Institutes of Health; 2013. Available at http://www.cancer.gov/cancertopics/prevention-genetics-causes. [Google Scholar]
- 5.World Health Organization. Global surveillance, prevention and control of chronic respiratory diseases: a comprehensive approach. Geneva, Switzerland: World Health Organization; 2007. Risk factors for chronic respiratory diseases; pp. 37–55. Available at http://www.who.int/gard/publications/GARD%20Book%202007.pdf. [Google Scholar]
- 6.CDC. Stroke risk factors. Atlanta, GA: US Department of Health and Human Services, CDC; 2010. Available at http://www.cdc.gov/stroke/risk_factors.htm. [Google Scholar]
- 7.Doll LS, Bonzo SE, Mercy JA, Sleet DA, editors. Handbook of injury and violence prevention. New York, NY: Springer; 2007. [Google Scholar]
- 8.CDC. CDC health disparities and inequalities report—United States, 2013. MMWR. 2013;62(Suppl 3) [PubMed] [Google Scholar]
- 9.US Department of Health and Human Services. Healthy people 2020. Washington, DC: US Department of Health and Human Service; 2013. Available at http://www.healthypeople.gov/2020. [Google Scholar]