Abstract
The objective of this research was to describe the slip, trip, and fall injury experience and trends in a population of nursing home workers, identify risk factors for slip, trip, and fall injuries, and develop prevention strategies for slip, trip, and fall hazards. Workers’ compensation injury claims data and payroll data from 1996 through 2003 were obtained from six nursing homes and used to calculate injury incidence rates. Narrative information was used to describe details of slip, trip, and fall events. A total of 86 slip, trip, and fall-related workers’ compensation claims were filed during the 8-year period. Slip, trip, and fall claim rates showed a nonsignificant increase during the 8-year period. Most slips, trips, and falls were attributed to hazards that can be mitigated (e.g., water on the floor or loose cords in a walkway). Nursing home workers experience more slip, trip, and fall-related injury claims than workers in other industries. Preventive programs should be implemented and evaluated in this industry.
Slips, trips, and falls account for the second largest proportion of lost-workday nonfatal injuries (26%) in the nursing care facilities industry subsector (Bureau of Labor Statistics, 2011b). In a ranking of the 268 industry subsectors based on 3-digit North American Industry Classification System (NAICS) codes (Office of Management and Budget, 2007), the nursing care facilities industry subsector ranked fourth overall for same-level slips, trips, and falls (i.e., falls on the same level, and slips or trips without a fall) and tenth for total slips, trips, and falls (i.e., falls from an elevation, falls on the same level, and slips or trips without a fall), with 66.9 and 70.4 lost workdays per 10,000 workers, respectively (Bureau of Labor Statistics, 2011b). The incidence rate for nursing care facilities surpasses that for all industries for same-level and total slips, trips, and falls—19.5 versus 26.4 per 10,000 workers, respectively. Due to the large number of nursing care facility workers, approximately 1.7 million (Bureau of Labor Statistics, 2011a), and a high incidence, 9,060 lost-workday slip, trip, and fall-related injuries occurred in this industry in 2010 (Bureau of Labor Statistics, 2011c).
Overexertion injuries, caused by bodily motions such as pushing, pulling, lifting, or twisting, are the most numerous occupational injuries among nursing care facility workers (Bureau of Labor Statistics, 2011b); consequently, overexertion injuries have received research focus. To address the issue of overexertion injuries, evaluations of patient-handling methods have provided evidence that these interventions can be effective in reducing overexertion injuries in the nursing care facility environment (Alamgir et al., 2008; Collins, Wolf, Bell, & Evanoff, 2004; Miller, Engst, Tate, & Yassi, 2006). In addition to patient-handling injuries, recent research has also focused on violence-related and needlestick injuries in the health care industry, including among nursing care workers (Myers, Kriebel, Karasek, Punnett, & Wegman, 2007; Trinkoff et al., 2008). These types of work-related incidents are postulated to contribute to high turnover rates among long-term care staff (Karsh, Booske, & Sain-fort, 2005). Although slips, trips, and falls are the second most frequent cause of lost-workday injuries among nursing care facilities, research about risk factors and prevention of slip, trip, and fall injuries among nursing care facilities is relatively scarce. In a review of injuries among nursing care facility employees, Castle, Engberg, Mendeloff, and Burns (2009) did not address slip, trip, and fall injuries in detail, despite their prominence in national data. The most recent published research on falls among health care workers reported that long-term care workers had the highest rate of fall injuries in British Columbia's health care sector (Drebit, Sharjari, Alamgir, Yu, & Keen, 2010). Given the paucity of slip, trip, and fall data in the U.S. health care sector, the objective of this research was to describe the slip, trip, and fall injury experience and trends in a population of nursing care facility workers compared to national trends, identify contributing factors, and inform future preventive efforts.
METHODS
The data used in this study were administrative records (e.g., workers’ compensation claims, first reports of injury, and personnel records) collected for non-research purposes by the partnering health care system. All work-related injury records and employment records were examined for all employees in six nursing care facilities from January 1, 1996, to December 31, 2003. All nursing care facilities belonged to the same non-profit U.S. Midwest health care system, covering a total of 552 licensed beds. The facilities ranged in size from 60 to 120 beds. Injuries, hours worked, and demographic data were supplied by the health care system for all staff employed during the 8-year study period. This research study was reviewed and approved by the National Institute for Occupational Safety and Health (NIOSH) Human Subjects Review Board (Institutional Review Board).
Injury Data
All workers’ compensation claims data from January 1, 1996, to December 31, 2003, for the six nursing care facilities were obtained electronically. Data on worker injuries were gathered from workers’ compensation claims. These records included narrative information on the event leading to the injury. The narrative information for each claim was used to identify specific details about the circumstances of the slip, trip, and fall incident. Causal factors were extracted from the text when possible to determine if the injured worker slipped on water, body fluids, or grease or tripped on an object or cord, for example. The first fall initiating event (Haslam & Bentley, 1999) was identified when possible and categorized as a slip, trip, loss of balance/misstep, or unknown (i.e., not enough information provided in the narrative to describe the fall initiating event).
Employment Data
Human resources records were obtained electronically for all nursing care facility employees and included data on productive hours worked per employee per year, employee date of birth, gender, job title, date of hire, and employment termination date. The job title assigned to every employee in the system was obtained from human resources records. The authors grouped the individual job titles into larger functional groups: care aides (primarily certified nursing assistants and patient care aides), nurses, food services, housekeeping, maintenance, and all other jobs (primarily administrative staff).
Incidence Rate Calculation
Workers’ compensation injury claims were used as the numerator and productive hours were used as the denominator to calculate incidence rates. Rates were reported as the number of injury claims per 100 full-time equivalents (FTEs) per year. One FTE is the equivalent of 2,000 productive work hours per calendar year. This is a method commonly used by the Bureau of Labor Statistics; it assumes a full-time worker works 40 hours a week, 50 weeks each year (2,000 hours).
National Trends
Bureau of Labor Statistics data on nonfatal injuries in the nursing care facilities industry are presented to show the frequency of slips, trips, and falls at the national level. To describe nonfatal lost workday injuries, slip, trip, and fall cases from Bureau of Labor Statistics yearly tables entitled “The number of nonfatal occupational injuries and illnesses involving days away from work by industry and selected events or exposures leading to injury or illness” (Bureau of Labor Statistics, 2011c) were summed for the events “fall to lower level,” “fall to same level,” and “slips or trips without fall.” The number of nonfatal occupational injuries and illnesses involving days away from work by industry and selected events or exposures leading to injury or illness in 2009 (Bureau of Labor Statistics, 2011c) were summed for the events of “fall to lower level,” “fall to same level,” and “slips or trips without fall.” The numbers of workers were estimated using the Bureau of Labor Statistics’ yearly tables for slips, trips, and falls (Bureau of Labor Statistics, 2011a). The analysis included all data currently available for nursing care facilities (NAICS code 6231), 2006 through 2010.
Statistical Analysis
Statistical analyses were performed using SAS, version 9.3 (SAS Institute Inc., 2011). Trends were calculated using Poisson regression (GENMOD procedure) with the number of slip, trip, and fall injury cases as the outcome variable, divided by person-time. For the six nursing care facilities in the study, workers’ compensation claims and productive hours worked per year were used in the trend analysis. In the analysis of national trends, Bureau of Labor Statistics lost-workday injury cases were used, along with the number of workers reported through the current population survey from the U.S. Census Bureau.
RESULTS
Study Nursing Care Facilities
During the 8-year period, January 1996 through December 2003, a dynamic cohort of employees worked a total of 8,865,470 productive hours (~4,433 FTEs). Over-exertion injuries comprised the largest proportion of total injury claims, 47% (223 of 472), during the 8-year period; slips, trips, and falls comprised the second largest proportion of total injury claims, 18% (86 of 472), and struck by/struck against/caught under, on, or in objects comprised the third largest proportion of total injury claims, 12% (56 of 472).
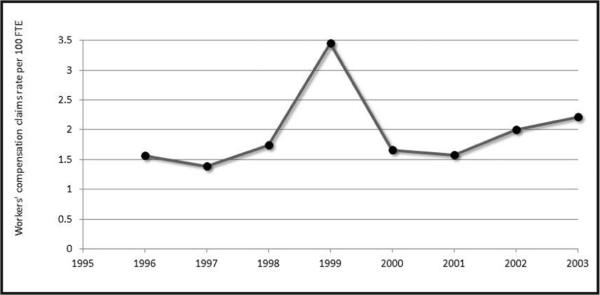
Univariate Poisson regression models were run for gender (male, female) and age group (younger than 50 years, 50 years or older). Although females had slightly higher slip, trip, and fall rates (i.e., 2.0 per 100 FTEs for females vs. 1.3 per 100 FTEs for males), the difference between males and females was not statistically significant (i.e., rate ratio = 1.54, upper and lower 95% confidence intervals = 0.74 and 3.20, respectively). The work force was 86% female overall. Workers 50 years and older experienced a significantly higher rate of work-related slips, trips, and falls (2.8 per 100 FTEs) compared to younger workers (1.6 per 100 FTEs, rate ratio = 1.72, upper and lower 95% confidence intervals = 1.11 and 2.70, respectively). During the 8-year period, the percentage of FTEs in the 50 and older age group increased from 22% in 1996 to 28% in 2003. Slip, trip, and fall claim rates (adjusted for age) showed a nonsignificant increase in trend (slope estimate = 0.0216, p = .6597) during the 8-year period (Fig. 1).
Figure 1.
Slip, trip, and fall workers’ compensation claim injuries in study nursing homes, 1996 to 2003. FTE = full-time equivalent.
The 86 slip, trip, and fall claims were categorized, based on the information in the claims narrative, to identify the causal factors of the event (Table 1). The greatest percentage, 36% (n = 31), was attributed to liquid contamination (e.g., water, body fluid, grease, wax, gel) on the floor. Six of these 31 cases specifically mentioned occurring in a bathroom or shower room. The second largest category (23% of the total incidents) was slips, trips, and falls that were not otherwise classified by contributing factors. An example of the type of claim in this category would be “slip, no fall, back sprain,” where the injury event (slip, no fall) and nature of injury (back sprain) were described but no causative factors (e.g., ice, water, or body fluids) were implicated.
Table 1.
Slip, Trip, and Fall Injury Claims Categorized by Causal Factor
| Causal Factor | n | % |
|---|---|---|
| Liquid contamination (water, wet floor, body fluid, grease, wax, gel) | 31 | 36.0 |
| Slips, trips, and falls not otherwise classifiable | 20 | 23.2 |
| Objects (wheelchairs, boxes, open desk drawers, bedspreads, waste-baskets) | 10 | 11.6 |
| Ice or snow | 9 | 10.5 |
| Cords (electric, phone, and call cords, medical tubing, wires) | 5 | 5.8 |
| Bodily reaction | 4 | 4.7 |
| Outdoor surface irregularities (holes, curbs, drain dips) | 3 | 3.5 |
| Indoor surface irregularities (mats, carpeting, rugs) | 3 | 3.5 |
| Elevations (fall from ladder, step stool, stair, through hole, out of non-moving vehicle) | 1 | 1.2 |
| Total | 86 | 100.0 |
The 86 slip, trip, and fall events were also grouped into four categories by the first fall initiating event: slip, trip, loss of balance/misstep, or unknown (i.e., not mentioned in the injury narrative). In 56% (n = 48) of the slip, trip, and fall claims, the most common initiating event was slipping, followed by tripping in 21% (n = 18) of the cases, not classifiable as to initiating event in 15% (n = 13) of the cases, and loss of balance/misstep in 8% (n = 7) of the cases.
Employees were placed in six functional job groupings based on job title (Table 2). Workers were labeled nursing, care aides, food services, housekeeping, maintenance, and all other. Of all six job groupings, the nursing group and the maintenance group had the lowest slip, trip, and fall claim rates, 1.2 per 100 FTEs and 0.8 per 100 FTEs, respectively. The care aide group had the highest slip, trip, and fall claim rate, 2.6 claims per 100 FTEs.
Table 2.
Slip, Trip, and Fall Workers' Compensation Injury Claims Rate by Job Group
| Job Group | No. of Slip, Trip, and Fall Injury Claims | No. of Hours Worked | Slip, Trip, and Fall Rate per 100 FTEs |
|---|---|---|---|
| Care aides | 41 | 3,162,129 | 2.6 |
| Food service | 9 | 907,716 | 2.0 |
| Other | 17 | 1,896,866 | 1.8 |
| Housekeeping | 7 | 851,955 | 1.6 |
| Nursing | 11 | 1,807,424 | 1.2 |
| Maintenance | 1 | 239,380 | 0.8 |
| Total | 86 | 8,865,470 | 1.9a |
Note. FTEs = full-time equivalents.
Total number of slip, trip, and fall claims for total work force productive hours, expressed as number of claims per 100 FTEs.
National Data on Nursing Care Facilities
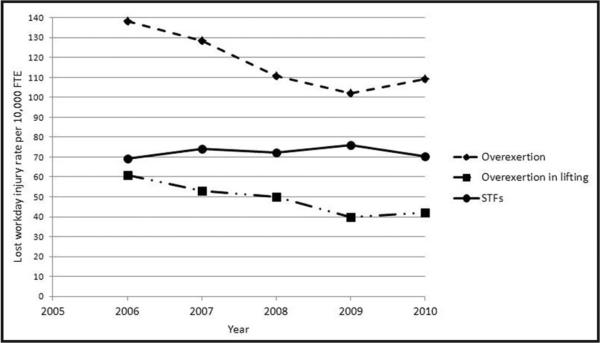
National lost-workday slip, trip, and fall data for nursing care facilities (NAICS 6231) collected by the Bureau of Labor Statistics were analyzed as a reference point (Fig. 2). Unadjusted lost-workday slip, trip, and fall rates showed a non-significant increase in trend (slope estimate = 0.0052, p = .1169) nationally during the 5-year period from 2006 through 2010. Conversely, unadjusted lost-workday overexertion in lifting rates showed a significant decline in trend (slope estimate = −0.1028, p < .0001). The total lost-workday overexertion injury rate (unadjusted) also declined significantly from 2006 through 2010 (slope estimate = −0.0714, p < .0001).
Figure 2.
Nursing care facilities industry lost-workday injuries per 10,000 full-time equivalent (FTE), 2006 to 2010. STFs = slips, trips, and falls. (Data from the Bureau of Labor Statistics, 2011b.)
DISCUSSION
National injury data show that nursing care facility employees are at particularly high risk of a slip, trip, and fall injury resulting in days lost from work when their rates are compared to rates found in all private industry (Bureau of Labor Statistics, 2011b); nursing care facilities’ same-level fall rate is almost 3½ times as great as the all-industry same-level fall rate. It is not fully known why these workers are at such high risk. The workers in this sample population of nursing care facilities were primarily (86%) female, and the percentage of the work force 50 years and older increased from 22% to 28% during the 8-year study period. Previous research in the health care industry has found an increased incidence of injuries caused by slips, trips, and falls among older workers and female workers (Bell et al., 2008; Kemmlert & Lundholm, 1998), and that fractures are common after a fall among older female workers (Verma, Lombardi, Chang, Courtney, & Brennan, 2008).
High slip, trip, and fall rates in the nursing care facility industry may result when workers provide residents with gait and balance problems who are at high risk of falling with activities of daily living assistance. Activities of daily living include bathing, showering, and toileting; during these activities, care aides are exposed to wet, slippery, and other hazardous floor conditions (Decker, Harris-Kojetin, & Bercovitz, 2009). Some workers in this industry may be less able to shift to light-duty work when injured and have lost-workday claims as opposed to a medical-only or restricted-duty claim (Pompeii, Lipscomb, & Dement, 2008). Research conducted by Galizzi, Miesmaa, Punnett, Slatin, and the Phase in Health-care Research Team (2010) suggests that many injuries are unreported in the health care industry, so it is likely that the injury burden sustained by nursing care facility workers is even greater than it appears.
Drebit et al. (2010) recently performed a large-scale analysis of falls in British Columbia's health care sector. In their study, the long-term care subsector (nursing care facility) workers had the highest rate of falls in the health care sector. Given that care aides were also among the employees at highest risk in long-term care, evaluation of these workers’ specific hazard exposures is warranted so that preventive measures can be better tailored to their work. Bathing and toileting of dependent patients, as an example, may add unique slip, trip, and fall hazards to long-term work. Fifty-six percent of slip, trip, and fall injuries in the current study were attributed to hazards such as liquid contamination on the floor, objects on the floor, or ice/snow in parking areas. Previous research in the health care industry (e.g., acute care hospitals) indicates that these types of hazards can be successfully mitigated through preventive measures such as improved housekeeping procedures, grounds maintenance, and hazard audits (Bell et al., 2008).
Roughly 20% of the slip, trip, and fall incidents in the current study population had an incident narrative lacking sufficient detail to guide specific prevention strategies. For example, an injury event might be described as “slip/ trip/loss of balance—with fall,” but the accompanying incident narrative would only say “right knee contusion.” In these cases, the incident narrative is used to describe the nature of the injury that occurred (e.g., contusion to the knee) rather than the causative factors (i.e., “slipped on icy patch in parking lot”). It would be more useful for developing prevention strategies to have the incident narratives capture these causative factors.
Some health care institutions take a “nature of injury” approach, focusing workplace health and safety efforts on sprains, strains, and musculoskeletal injuries because these are the most common and costly. Although many of these sprain and strain injuries are caused by patient handling, sprains and strains also are the most frequent injuries after a slip, trip, and fall incident (Bell et al., 2008). Back pain is also a common injury outcome; it is estimated that between 19% (Mital, Pennathur, & Kansal, 1999) and 36% (Troup, Martin, & Lloyd, 1981) of occupational back pain cases can be attributed to a slip, trip, and fall event. In a more recent, detailed analysis of the musculoskeletal injuries reported in a population of more than 19,000 medical center workers, it was determined that 30% of these injuries were caused by slips, trips, and falls, almost equal to the 31% caused by patient handling (Pompeii et al., 2008). Therefore, a portion of the total sprain/strain burden in health care is caused by slip, trip, and fall events.
In the national data on injuries to nursing care facility workers, the rates of slip, trip, and fall injuries and injuries due to lifting were similar in 2006; however, the rate of slip, trip, and fall injuries remained static when the overexertion due to lifting injuries, as well as total over-exertion injuries, declined significantly. Evidence within the health care industry suggests that researching and targeting an injury problem can result in declines in injury rates. Over the years, research on safe patient handling has accumulated and safer methods have been promulgated (Alamgir et al., 2008; Collins et al., 2004; Miller et al., 2006). It is plausible that safe patient-handling training and increased use of mechanical lifts (Charney et al., 2010) have contributed to significant declines in national rates. Similar interest in the prevention of health care slip, trip, and fall injuries should also be promoted. The body of research on the effectiveness of occupational slip, trip, and fall prevention measures is growing (Bell et al., 2008; Bentley & Haslam, 2001; Verma et al., 2011) but remains limited. It is hoped that this current research will raise awareness of the high incidence of slip, trip, and fall injuries among the nursing care facility work force. If targeted slip, trip, and fall prevention efforts are encouraged and implemented in nursing care facilities, national declines in slip, trip, and fall injuries (e.g., the declines seen in overexertion and lifting) may eventually be realized.
IMPLICATIONS FOR PRACTICE
NIOSH and its partners conducted a 10-year longitudinal study in acute care hospitals (Bell et al., 2008) that provided evidence that implementation of broad-scale prevention programs can significantly reduce slip, trip, and fall workers’ compensation injury claims. As a result of the findings from this study, NIOSH published a slip, trip, and fall prevention guide document for health care facility administrators, health and safety professionals, facility managers, food service managers, and workers who are responsible for safety (Bell, Collins, Dalsey, & Sublet, 2010). Although this document was based on research conducted in acute care hospitals, most of the principles and recommendations for prevention apply to long-term care settings. The document identifies the top 10 slip, trip, and fall hazards specific to health care facilities (i.e., contaminants on the floor, poor drainage of pipes and drains, indoor walking surface irregularities, outdoor walking surface irregularities, weather conditions [ice/snow/rain], inadequate lighting, stairs and handrails, tripping hazards such as clutter, cords, and tubing, and improper use of floor mats and runners), provides a checklist to identify hazards in a health care facility, and provides guidance on implementing programs to protect health care workers. In addition to the above, the American National Standards Institute (ANSI) standards such as the provision of slip resistance on walking/working surfaces (ANSI, 2006) and detailed textbooks (Di Pilla, 2010) can guide occupational health and safety professionals in the reduction of slip, trip, and fall hazards.
Occupational slips, trips, and falls are preventable. Evidence suggests that facility-wide programs targeting common slip, trip, and fall hazards can reduce a facility's injury rate. Slippery floors can be addressed through changes such as improvements in housekeeping practices (e.g., correctly using wet floor signs, immediately cleaning up spills, correctly removing grease, aggressively removing ice and snow). Floors that are frequently wet (e.g., bathrooms and kitchens) should be textured so they are not slick when covered with water or other contaminants. Employees assisting residents in these wet environments should consider wearing slip-resistant shoes for additional traction. Employees working in kitchens may benefit from wearing slip-resistant shoes during their entire shift.
Training about recording and coding the initial injury event should be provided to workers to ensure that the specifics of each injury event are properly documented and coded in injury records. Workers should also be trained to recognize common workplace slip, trip, and fall hazards and mitigate these hazards promptly.
It is hoped more institutions will recognize the significant portion of the injury burden among nursing care facility workers caused by slips, trips, and falls and take steps toward prevention.
Applying Research to Practice.
Occupational slip, trip, and fall injuries are preventable. Nursing care facility workers have high rates of lost-workday injuries due to slips, trips, and falls compared to other worker groups. Care aides and food service workers are at highest risk for slip, trip, and fall injuries. Evidence suggests that a facility-wide program targeting common slip, trip, and fall hazards can reduce a facility's injury rate. Examining injury trends within a facility by event type (i.e., slip, trip, or fall, overexertion due to lifting, struck by, needlestick), rather than by nature of injury (i.e., sprain or strain, contusion, laceration), can make tracking the effectiveness of safety interventions over time easier. The initial injury event should be recorded and coded. All employees should be trained to recognize common workplace slip, trip, and fall hazards and to mitigate these hazards promptly.
Footnotes
The authors have disclosed no potential conflicts of interest, financial or otherwise.
Contributor Information
Dr. Jennifer L. Bell, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Division of Safety Research, Morgantown, WV..
Dr. James W. Collins, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Division of Safety Research, Morgantown, WV..
Dr. Hope M. Tiesman, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Division of Safety Research, Morgantown, WV..
Ms. Marilyn Ridenour, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Division of Safety Research, Morgantown, WV..
Mr. Srinivas Konda, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Division of Safety Research, Morgantown, WV..
Ms. Laurie Wolf, Barnes Jewish Hospital, St. Louis, MO..
Dr. Bradley Evanoff, Occupational and Environmental Medicine, Washington University School of Medicine, St. Louis, MO..
REFERENCES
- Alamgir H, Yu S, Fast C, Hennessy S, Kidd C, Yassi A. Efficiency of overhead ceiling lifts in reducing musculoskeletal injury among careers working in long-term care institutions. International Journal of the Care of the Injured. 2008;39(5):570–577. doi: 10.1016/j.injury.2007.11.420. [DOI] [PubMed] [Google Scholar]
- American National Standards Institute . American national standard: Standard for the provision of slip resistance on walking/working surfaces. Author; New York, NY: 2006. [Google Scholar]
- Bell JL, Collins JW, Dalsey E, Sublet V. Slip, trip, and fall prevention for healthcare workers (DHHS [NIOSH] Publication no. 2011-123) 2010 Retrieved from www.cdc.gov/niosh/docs/2011-123.
- Bell JL, Collins JW, Wolf L, Gronqvist RA, Chiou S, Chang W-R, Evanoff B. Evaluation of a comprehensive STF prevention programme for hospital employees. Ergonomics. 2008;51(12):1906–1925. doi: 10.1080/00140130802248092. [DOI] [PubMed] [Google Scholar]
- Bentley TA, Haslam RA. A comparison of safety practices used by managers of high and low accident rate postal delivery offices. Safety Science. 2001;37(1):19–37. [Google Scholar]
- Bureau of Labor Statistics Employment, hours, and earnings from the current employment statistics survey (national), current employment statistics (national) analytical tables. 2011a Retrieved from www.bls.gov/ces/#data.
- Bureau of Labor Statistics Incidence rates for nonfatal occupational injuries and illnesses involving days away from work per 10,000 full-time workers by industry and selected events or exposures leading to injury or illness, 2010. 2011b Retrieved from www.bls.gov/iif/oshwc/osh/case/ostb2832.pdf.
- Bureau of Labor Statistics Number of nonfatal occupational injuries and illnesses involving days away from work by industry and selected events or exposures leading to injury or illness, 2010. 2011c Retrieved from www.bls.gov/iif/oshwc/osh/case/ostb2828.pdf.
- Castle NG, Engberg J, Mendeloff J, Burns R. A national view of workplace injuries in nursing homes. Health Care Management Review. 2009;34(1):92–103. doi: 10.1097/01.HMR.0000342981.37673.74. [DOI] [PubMed] [Google Scholar]
- Charney W, Hudson A, Gallagher S, Lloyd JD, Baptiste A, Nelson A, Villeneuve J. Back injury prevention in health care. In: Charney W, editor. Handbook of modern hospital safety. 2nd ed. CRC Press; Boca Raton, FL: 2010. [Google Scholar]
- Collins JW, Wolf L, Bell J, Evanoff B. An evaluation of a “best practices” back injury prevention program in nursing homes. Injury Prevention. 2004;10(4):206–211. doi: 10.1136/ip.2004.005595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker FH, Harris-Kojetin LD, Bercovitz A. Intrinsic job satisfaction, overall satisfaction, and intention to leave the job among nursing assistants in nursing homes. The Gerontologist. 2009;49(5):596–610. doi: 10.1093/geront/gnp051. [DOI] [PubMed] [Google Scholar]
- Di Pilla S. Slip, trip, and fall prevention: A practical handbook. 2nd ed. CRC Press; Boca Raton, FL: 2010. [Google Scholar]
- Drebit S, Sharjari S, Alamgir H, Yu S, Keen D. Occupational and environmental risk factors for falls among workers in the healthcare sector. Ergonomics. 2010;53(4):525–536. doi: 10.1080/00140130903528178. [DOI] [PubMed] [Google Scholar]
- Galizzi M, Miesmaa P, Punnett L, Slatin C, the Phase in Health-care Research Team Injured workers’ underreporting in the health care industry: An analysis using quantitative, qualitative, and observational data. Industrial Relations. 2010;49:22–43. doi: 10.1111/j.1468-232X.2009.00585.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslam RA, Bentley TA. Follow-up investigations of slip, trip and fall accidents among postal delivery workers. Safety Science. 1999;32(1):33–47. [Google Scholar]
- Karsh B, Booske BC, Sainfort F. Job and organizational determinants of nursing home employee commitment, job satisfaction and intent to turnover. Ergonomics. 2005;48(10):1260–1281. doi: 10.1080/00140130500197195. [DOI] [PubMed] [Google Scholar]
- Kemmlert K, Lundholm L. Slips, trips and falls in different work groups with reference to age. Safety Science. 1998;28(1):59–75. doi: 10.1016/s0003-6870(00)00051-x. [DOI] [PubMed] [Google Scholar]
- Miller A, Engst C, Tate RB, Yassi A. Evaluation of the effectiveness of portable lifts in a new long-term care facility. Applied Ergonomics. 2006;37(3):377–385. doi: 10.1016/j.apergo.2005.05.012. [DOI] [PubMed] [Google Scholar]
- Mital A, Pennathur A, Kansal A. Nonfatal occupation injuries in the United States: Part I. Back injuries. International Journal of Industrial Ergonomics. 1999;25:131–150. [Google Scholar]
- Myers DJ, Kriebel D, Karasek R, Punnett L, Wegman DH. The social distribution of risk at work: Acute injuries and physical assaults among healthcare workers working in a long-term care facility. Social Science and Medicine. 2007;64(4):794–806. doi: 10.1016/j.socscimed.2006.10.027. [DOI] [PubMed] [Google Scholar]
- Office of Management and Budget 2007 NAICS (North American Industry Classification System) United States manual. 2007 Retrieved from www.census.gov/eos/naics.
- Pompeii LA, Lipscomb H, Dement JM. Surveillance of musculoskeletal injuries and disorders in a diverse cohort of workers at a tertiary care medical center. American Journal of Industrial Medicine. 2008;51(5):344–356. doi: 10.1002/ajim.20572. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS/STAT® 9.3 user's guide. Author; Cary, NC: 2011. [Google Scholar]
- Trinkoff AM, Geiger-Brown JM, Caruso CC, Lipscomb JA, Johantgen M, Nelson AL, Selby VL. Personal safety for nurses. In: Hughes RG, editor. Patient safety and quality: An evidence-based handbook for nurses. Agency for Healthcare Research and Quality; Rockville, MD: 2008. [PubMed] [Google Scholar]
- Troup DG, Martin JW, Lloyd DCEF. Back pain in industry: A prospective survey. Spine. 1981;6(1):61–69. doi: 10.1097/00007632-198101000-00014. [DOI] [PubMed] [Google Scholar]
- Verma SK, Chang W-R, Courtney TK, Lombardi DA, Huang Y-H, Brennan MJ, Perry MJ. A prospective study of floor surface, shoes, floor cleaning and slipping in US limited-service restaurant workers. Occupational and Environmental Medicine. 2011;68(4):279–285. doi: 10.1136/oem.2010.056218. [DOI] [PubMed] [Google Scholar]
- Verma SK, Lombardi DA, Chang W-R, Courtney TK, Brennan MJ. A matched case-control study of circumstances of occupational same-level falls and risk of wrist, ankle and hip fracture in women over 45 years of age. Ergonomics. 2008;51(12):1960–1972. doi: 10.1080/00140130802558987. [DOI] [PubMed] [Google Scholar]