Abstract
Objective
To test the efficacy of the relationship-focused behavioral coaching intervention Communicating and Relating Effectively (CARE) in increasing maternal-infant relational effectiveness between depressed mothers and their infants during the first nine months postpartum.
Design
Randomized clinical trial (RCT) with three phases.
Methods
In this three-phase study, women were screened for postpartum depression (PPD) in Phase I at 6 weeks postpartum. In Phase II, women were randomly assigned to treatment or control conditions and maternal-infant interaction was video-recorded at four intervals postpartum: 6 weeks, 3 months, 6 months, and 9 months. Phase III involved focus group and individual interviews with study participants.
Setting
Phase I mothers were recruited from obstetric units of two major medical centers. Phase II involved the RCT, a series of nurse-led home visits beginning at 6 weeks and ending at 9 months postpartum. Phase III focus groups were conducted at the university and personal interviews were conducted by telephone or in participants’ homes.
Participants
Postpartum mother-infant dyads (134) representative of southeastern New England, United States participated in the RCT. One hundred and twenty-five mother-infant dyads were fully retained in the 9-month protocol.
Results
Treatment and control groups had significant increases in quality of mother-infant interaction and decreases in depression severity. Qualitative findings indicated presence of the nurse, empathic listening, focused attention and self-reflection during data collection, directions for video-recorded interaction, and assistance with referrals likely contributed to improvements for both groups.
Conclusions
Efficacy of the CARE intervention was only partially supported. Nurse attention given to the control group and the data collection process likely confounded results and constituted an unintentional treatment. Results suggest that nurse-led home visits had a positive effect on outcomes for all participants.
Keywords: postpartum depression, maternal-infant interaction, nursing intervention, behavioral coaching, randomized clinical trial
Depression is a leading cause of disability globally, and women are affected disproportionally (Gaynes et al. 2005; World Health Organization, 2010). Following childbirth harmful effects of depression extend from mother to infant. Postpartum depression (PPD) is a mood disorder that occurs with alarming frequency with documented prevalence of 10–15% and period prevalence of 19.2% during the first three months after delivery, thus making it one of the most common postpartum complications (Gaynes et al., 2005; O’Hara & Swain, 1996; World Health Organization, 2010). Even higher prevalence rates have been reported among some populations with identified demographic risk factors such as very young maternal age, low education, low income, history of depression, and selected race/ethnicity, e.g., possibly being African American (Beck, 2001; Mayberry, Horowitz, & Declercq, 2007; Segre, Losch, & O’Hara, 2006).
Postpartum depression is characterized by loss of interest or pleasure, depressed mood, psychomotor agitation or retardation, fatigue/sleep disturbance, changes in appetite, feelings of inadequacy, worthlessness, or guilt, and decreased concentration, all of which can interfere with effective maternal functioning (Abell, 2007; American Psychiatric Association, 2000; Beck, 2006; Gaynes et al., 2005). Diagnostic criteria specify mood disorder onset within four weeks postpartum (American Psychiatric Association). Notably, even episodes of mild or sub-clinical depression have been associated with difficulties in maternal functioning (Weinberg et al., 2001).
Background and Significance
Effects of PPD on Maternal-infant Interaction and Infant Development
Links between PPD and less affectionate, withdrawn or intrusive hostile maternal behavior, and more avoidant, discontent, and withdrawn infant behavior have been demonstrated by a body of research over the past three decades (Feldman & Edelman, 2007; Field, 2010; Forman, O'Hara, Stuart, Gorman, Larsen, & Coy, 2007; Letourneau, Salmani, & Duffett-Leger et al., 2010; Stein, Malmberg, Sylva, Barnes, & Leach, 2008; Teti, Gelfand, Messinger, & Isabella, 1995). Evidence supports the conclusion that PPD likely has universal negative effects on maternal functioning (Field, 2010) with negative sequelae for children, which have been demonstrated through age 12 (Letourneau et al., 2010).
Interventions to Mitigate Effects of PPD on Infant Development
Interventions for PPD have largely been aimed at treating maternal depression without focused attention on treating the maternal-infant relational disturbance (Field, 2010). Yet treatment of PPD alone may be insufficient to ameliorate disordered maternal-infant interaction. Notably,Forman et al. (2007) showed that even when PPD improved with depression-focused treatment, the quality of maternal–infant interaction did not. In a meta-analysis to examine effectiveness of preventive interventions to enhance depressed mothers’ sensitivity (Kersten-Alvearez et al., 2011), the authors demonstrated that individual therapy for the mother was ineffective in improving maternal sensitivity. However, results confirmed that depressed mothers' sensitivity can be improved by preventive intervention. Thus, interventions for PPD aimed specifically at maternal-infant interaction are needed.
To date, a limited number of intervention studies targeted at improving maternal–infant interaction in the presence of PPD have been reported (Barlow, Davis, McIntosh, Jarrett, Mockford et al., 2006; Horowitz, Bell, Trybulski, Munro, Moser, Hartz et al., 2001; Kalinauskiene, Cekuoliene, van Ijzendoorn, Bakermans-Kranenburg, Juffer, et al., 2009; Van Doesum, Riksen-Walraven, Hosman & Hoefnagels, 2008). The RCTs showed that behaviorally-based home visiting interventions for depressed mothers and their infants had positive effects on maternal-infant interaction. Additionally, Olds, Henderson, & Kitzman (1994) completed groundbreaking research on the use of home visits by nurses during the prenatal and early childhood years and demonstrated long term effects on parental caregiving and child development (Eckenrode et al., 2010; Kitzman et al., 2010; Olds et al., 1994). However, this work was not targeted specifically at mothers with PPD and their infants. In conclusion, these combined results are promising; however, additional intervention research is needed to produce sufficient evidence to influence standard care designed for mothers experiencing PPD that aims to affect the maternal-infant relationship (Field, 2010).
Theoretical Foundations
Intervention design begins with analyzing the nature of the problem (Johnston & Dixon, 2008; Melnyk & Morrison-Beedy, 2012). PPD dysregulates maternal cognitive and affective function and in turn interferes with the mother’s ability to notice and interpret her infant’s cues accurately, contingently, and sensitively (Dawson & Ashman, 2000; Horowitz, Murphy, Gregory, & Wojcik, 2011). Resultant problematic maternal-infant interaction has been linked to impaired infant neurobiological development, specifically psychobiological disruptions associated with reduced activity in the frontal brain region that mediates positive approach, affiliative behavior, and increased autonomic arousal during social encounters (Diego, Field, Jones, & Hernandez-Reif, 2006; Field & Diego, 2008; Parsons, Young, Murray, Stein & Kringelbach, 2010). Postpartum depression is a common childbirth complication that occurs during the critical period of the first few months of the infant's life when the maternal-infant relationship is developing. Problematic maternal-infant interaction patterns threaten the infant's health, behavioral and psychobiological development, and subsequent social behavior and cognitive development.
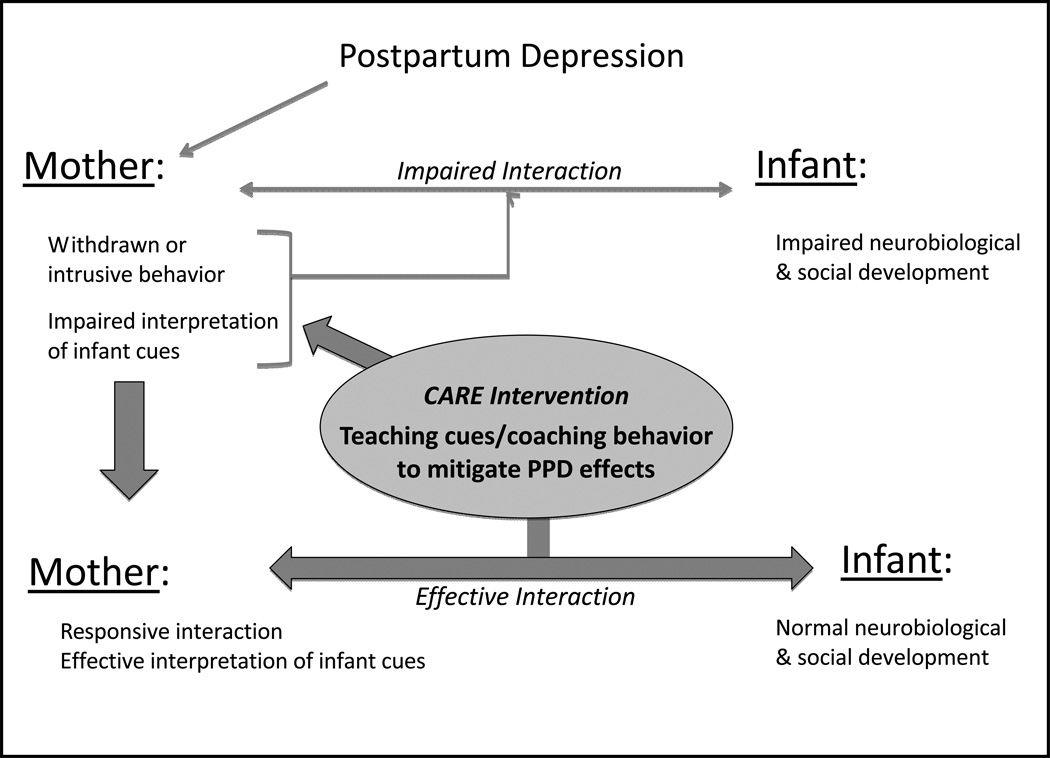
Cognitive-behavioral family therapy theory (Nichols, 2010) provides the theoretical foundation for the Communicating and Realating Effectively (CARE) intervention. In this intervention, the nurse assisted the mother to recognize her infant’s engagement cues and respond appropriately. In doing so she used social reinforcement to promote the infant’s communication. In turn, the mother’s approach behavior was reinforced when the infant responded to her with engagement cues. In response to infant disengagement cues, the nurse encouraged the mother to comfort or avoid further stimulation of the infant. Non-contingent or undesirable maternal responses were extinguished over time by lack of reinforcement and direct teaching and modeling by the nurse. Thus, the nurse interventionist used the principles of cognitive restructuring by teaching interpretation of infant cues and behavioral shaping via modeling, direct instruction, and social reinforcement (including praising successful interaction) with the aim of promoting responsive contingent maternal-infant interaction. Figure 1 illustrates the theoretical foundations of the study.
Figure 1.
Model of Theoretical Foundations For The Study
Purpose
The literature supports the need for continued development of effective, evidenced-based interventions to examine and alter dysfunctional maternal-infant relationship patterns associated with PPD (Field, 2010; Forman et al., 2007; Horowitz, 2011). Moreover, current research outcomes indicate that behaviorally based interventions are the most effective approach in promoting maternal responsiveness (Horowitz, 2011); however, the body of intervention research to date is limited. Therefore, a relationship-focused behavioral intervention, CARE, was developed with the aim of ameliorating the negative effects of PPD on maternal-infant interaction. The CARE intervention is based on previous work but moves the body of knowledge ahead by specifically targeting behavioral coaching to maternal behaviors that characterized mothers with PPD. These behaviors include missing infants’ engagement cues, using limited amounts of voice and touch due to effects of depression, and vocalizing rapidly and failing to wait for infant’s engagement readiness that typify mothers whose PPD includes many anxiety features. This study also followed mothers over a longer timeframe than was done by Horowitz et al. (2001), from early postpartum, 6 weeks, to 9 months. Most importantly, the existing evidence base is too limited to direct standard practice. Thus, this study was needed to build on previous research and move the evidence base forward.
The purpose of this study was to test the efficacy of the relationship-focused behavioral nursing CARE intervention in increasing maternal-infant relational effectiveness between depressed mothers and their infants during the first nine months postpartum.
Hypotheses and Exploratory Research Question
The following hypotheses were tested and one research question was investigated:
After participating in the CARE intervention, the treatment group compared to the control group will have significantly higher maternal-infant relational effectiveness.
After participating in the CARE intervention, the treatment group compared to the control group will have significantly higher infant clarity of cues and responsiveness to parent.
Because PPD severity may change over time and may or may not have been affected by study participation, we also posed the following question: How will maternal depression vary over time for the treatment group and control group?
Methods
Study Design
The study was a repeated measures randomized clinical trial (RCT) with assignment of eligible participants to a treatment or control group. All study procedures were reviewed and approved by the Human Research Subjects Committees of the hospitals and university prior to study initiation. The study had three phases: Phase I involved participant recruitment and postpartum depression prescreening, Phase II involved the clinical trial to test the efficacy of the CARE intervention, and Phase III involved focus groups and individual follow-up interviews. Phase I and II procedures continued concurrently over nearly four years (Phase I continued for 36 months and Phase II continued for another 9 months to complete the RCT) until the desired sample size was reached. Phase III was conducted after Phase II ended and concluded when mothers who agreed to participate had completed follow-up interviews and data saturation was reached.
Study Participants
The sample size required for the planned analyses was 116 mother-infant dyads (i.e., 58 mother-infant dyads per group) as determined by power analysis specifying a moderate effect size (d = .50) to detect meaningful change, power of .80, alpha level of .05, and a minimum correlation between scores of .30. The sample size required for the planned analyses is 116 (58 per group), determined by power analysis specifying a moderately low effect size (d = .50), power of .80, an alpha level of .05, and a minimum correlation between scores at each level of .30 (Maxwell & Delaney, 1990).
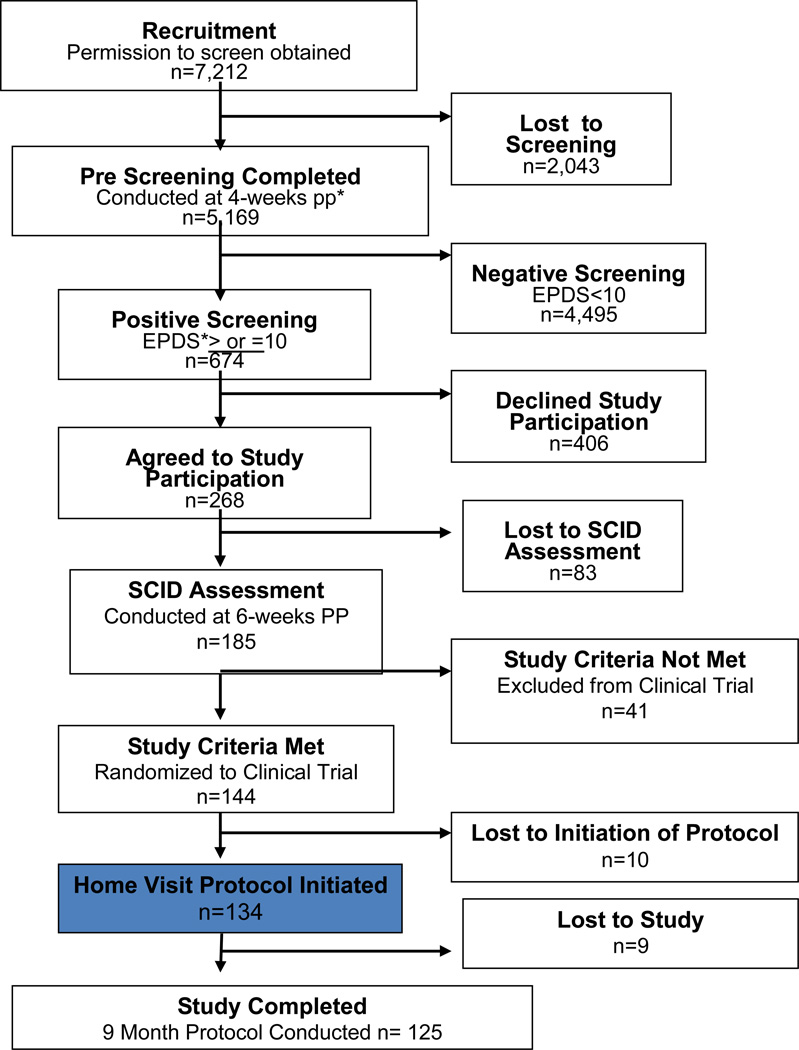
A population of 7,212 postpartum women was recruited for PPD pre-screening, and 5,169 were prescreened for PPD as part of Phase I of this study. Details concerning initial study recruitment and prescreening procedures and results have been reported elsewhere (Horowitz et al., 2011; Horowitz, Murphy, Gregory, & Wojcik, 2009). Preliminary eligibility for Phase II (clinical trial phase) was determined by an Edinburgh Postnatal Depression Scale (EPDS) (Cox, 1986; Cox, Holden, & Sagovsky, 1987) prescreening score ≥ 10. The study sample included in the clinical trial was comprised of 134 postpartum women and their infants. Subject inclusion criteria were (a) an EPDS prescreening score ≥ 10 and subsequent confirmation of depression status by diagnostic interview; (b) birth of a healthy, singleton, term gestation infant at Brigham and Women’s Hospital or Massachusetts General Hospital, Boston; (c) adequate proficiency in English to complete study instruments and converse with research nurses. Mothers were excluded if they had been diagnosed with a major psychiatric disorder (e.g., bipolar disorder, schizophrenia, active postpartum psychosis) or severe medical condition that impaired ability to participate in the study procedures. Women whose diagnostic interview and/or EPDS pre-screening depression scores indicated moderate to severe depression symptom severity (i.e., ≥ 13) (Cox et al., 1987) were retained in the study and their willingness to participate was confirmed. These women were also encouraged to contact their primary care provider (PCP) or delivery hospital psychiatric service for follow-up evaluation.
Once eligibility was confirmed, women were invited to Phase II of the study and then informed consent was obtained and followed immediately by the diagnostic interview (SCID) (First, Spitzer, Gibbon, & Williams, 1997) conducted by an advanced practice psychiatric-mental health nurse (APRN) to confirm depression status. If study criteria were met, and the mother agreed to participate in Phase II after informed consent, then the mother and her infant were randomized and formally enrolled into the RCT. At each contact, participants were asked if they were receiving psychiatric treatment, including medication, via an updated demographic and health information questionnaire.
Demographic characteristics describing the participants included in Phase II of this study are presented in Table 1. The number of participants recruited to the study and those lost to follow up is outlined in Figure 2. To minimize attrition, the researchers employed strategies used successfully in a prior study (Horowitz et al., 2001), including providing stipends and infant gifts for participants, arranging visits at participants’ residences at convenient times, and making reminder calls regarding home visits. As a result, only nine mothers dropped out of the intervention phase of the study through 9 months postpartum. Mothers who dropped out did so for a variety of reasons including returning to work and relocation outside the area.
Table 1.
Characteristics of Study Sample (N = 134 at baseline)
| Characteristic | N | % | X | SD |
|---|---|---|---|---|
| Mother’s Age in Years | 31 | 5.7 | ||
| Mother’s Years Education | 15.6 | 3.4 | ||
| Family Income | $80,132. | $49,070. | ||
| Mother’s Primary Language | ||||
| English | 97 | 72 | ||
| Spanish | 13 | 10 | ||
| Other | 24 | 18 | ||
| Mother’s Marital Status | ||||
| Single | 31 | 23 | ||
| Married | 100 | 75 | ||
| Other | 3 | 2 | ||
| Mother’s Race/Ethnicity | ||||
| African American | 16 | 12 | ||
| Asian | 11 | 8 | ||
| Caucasian | 72 | 54 | ||
| Hispanic | 30 | 22 | ||
| Other | 5 | 5 | ||
| Mother’s Hx Depression | ||||
| Yes | 66 | 49 | ||
| No | 68 | 51 | ||
| Mother’s Hx Substance Abuse | ||||
| No | 133 | 99 | ||
| Yes | 1 | 1 | ||
| Living with Partner | ||||
| Yes | 11 | 83 | ||
| No | 23 | 17 | ||
| Mother’s Employment | ||||
| Not Working | 102 | 76 | ||
| Working | 32 | 24 | ||
| First Baby | ||||
| Yes | 75 | 56 | ||
| No | 59 | 44 | ||
| Gestational Age (wks) | 7.4 | 1.3 | ||
| Birth Weight (gm) | 3432 | 465 |
Figure 2.
Clinical trial enrollment: CONSORT diagram
The CARE Intervention
Communicating And Relating Effectively (CARE), a relationship-focused behavioral nursing intervention, was designed to promote responsive interaction over time between depressed mothers and their infants by coaching mothers to interpret infants’ behavioral cues and to respond sensitively and contingently. Intervention nurses taught and coached depressed mothers to communicate and relate more effectively by altering withdrawn, disengaged patterns and intrusive, irritable styles of interaction. Based on observation, CARE research nurses identified problematic maternal behaviors that were specific to each mother-infant dyad. By teaching the mother how to interpret her infant’s communication cues and by coaching her to try alternate behaviors, the nurses attempted to promote new maternal responses and skills. Specific CARE intervention components for teaching and behavioral coaching are listed in Table 2. Maternal-infant interactions were video-recorded for later blind-coding using the Nursing Child Assessment Teaching Scale (NCATS) (Barnard et al., 1989; Sumner & Spietz, 1994).
Table 2.
CARE Intervention Components for Teaching and Behavioral Coaching
| Teaching How to Interpret Infant’s Cues | Behavioral Coaching | |
|---|---|---|
| Session 1 (4 weeks) |
|
|
|
Sessions 2, 3, 4, & 5 (6 weeks, 2 months, 3months, 4 months, 6 months) |
|
|
The study visits were conducted in participants’ residences (although women had the option to select an alternate site) and lasted for approximately one hour when measurements were also included. These visits occurred at 6 weeks and 3, 6, and 9 months postpartum for all study participants. The treatment group received additional visits at 2 and 4 months postpartum during which only the CARE intervention was administered. These supplemental visits lasted for approximately 30 to 40 minutes. Participants received remuneration of $25 following the diagnostic interview and the 6 week, 3, 6, and 9 month visit, and treatment mothers received a small infant toy following the 2 and 4 month visit.
Measurements
Mother’s Information Tool (MIT), MIT-brief and MIT Update
The Mother’s Information Tool (MIT) was used to elicit demographic and situational information from Phase II participants including: maternal and infant ages; infant gender; ethnicity and race; parity; marital/partner relationship status; education; employment status; income; maternal history of depression; pregnancy, labor and delivery history; and current health status of mother and infant. The MIT was used successfully in the Baby Talk study (Horowitz et al., 2001). The MIT-brief, was used for prescreening in Phase 1 for descriptive purposes to obtain basic data concerning mothers’ age, race and ethnicity, and parity (i.e., first child or not), the complete MIT was administered in Phase II at Time 1, and updated information about maternal and infant health and illness, routine primary care, maternal depression treatment, and others changes, such as returning to work, were obtained at subsequent home visits with the MIT Update.
Edinburgh Postnatal Depression Scale (EPDS)
The EPDS (Cox, 1986; Cox et al., 1987) was designed specifically to identify symptoms of PPD and is the most widely used PPD screening instrument in community-based populations in the United States and internationally (Gibson, McKenzie-McHarg, Shakespere, & Price, 2009). The 10-item version consists of statements describing depressive symptoms with responses ranging from 1 (low) to 4 (high) according to severity or duration. Total scores on the EPDS range from 0–30. Cutoff scores may be set at 9/10 or 12/13. The authors of the EPDS recommended using the score of 9/10 to reduce failed detection to less than 10%, and suggested that mental health referral is indicated for scores 13 or higher. The EPDS was used for pre-screening in Phase 1. In Phase II it was administered in conjunction with the Postpartum Depression Screening Scale (PDSS) (Beck & Gable, 2000; Beck & Gable, 2001a, 2001b, 2001c). Cronbach’s alpha for the EPDS for 134 participants at baseline was .82.
Postpartum Depression Screening Scale (PDSS)
The PDSS (Beck & Gable, 2000; Beck & Gable, 2001a, 2001b, 2001c) is a 35-item self-report instrument to identify women who are at high risk for postpartum depression. Results of psychometric testing indicate that the PDSS is a valid and reliable measure for use in routine screening and research (Beck & Gable, 2001a, 2001b). The PDSS was used to measure PPD symptom severity over time. Cronbach’s alpha for the PDSS for 134 participants at baseline was .94.
Diagnostic Interview
An ARPN conducted diagnostic interviews using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-1) (First et al., 1997) to classify participants as did not meet criteria for depression (i.e., negligible presence of depression symptoms) or met criteria for depression, including Depression NOS (Not Otherwise Specified); Minor Depressive Disorder (i.e., clinically significant depressive symptoms lasting for at least two weeks duration but less than the five symptoms required for Major Depressive Disorder; or Major Depressive Disorder). Women classified as not depressed did not participate in Phase II of the study. The diagnostic interview conducted by a qualified clinician such as an APRN is the gold standard for confirming a depression diagnosis as compared to self-report, which is a major limitation of many studies (Beck & Gable, 2001a). Reliabilty and validity of the SCID when administered by a qualified clinician such as an APRN have been documented across multiple studies (“What Is the Reliability of the SCID?,” 2012; “What Is the Validity of the SCID?,” 2012).
The Nursing Child Assessment Teaching Scale (NCATS)
The Nursing Child Assessment Teaching Scale (NCATS) of the Nursing Child Assessment Satellite Training (NCAST) (Barnard et al., 1989; Sumner & Spietz, 1994) was used as the measure of maternal-infant relational effectiveness (73 items), and responsiveness to parent/caregiver (13 items). Behaviors are observed and binary items are scored as present or absent. Dyadic interactive disturbance is suggested by positive scores for less than 43 items (1–6 months), 46 items (9–12 months), 52 items (13–24 months), or 53 items (25–36 months). Internal consistency reliability was reported as .87 for the Overall Total Scale (Sumner & Spietz, 1994).
In the current study, the NCATS was used to measure mother-infant relational effectiveness. The teaching interaction is designed to be quite brief and provides a novel interaction for the parent and child that places some stress on the interactive system. The NCATS was administered at home visits in Phase II. For 134 participants at baseline, Cronbach’s alpha for all 73 items was .91 and Cronbach’s alpha for the 13 item Responsiveness to Caregiver Subscale was .76. However due to a Cronbach’s alpha < .70 for the Clarity of Cues Subscale in this study, results from this measure were dropped from analyses.
Focus group and Follow-up Interviews
Phase III involved a qualitative descriptive design (Sandelowski, 2000) using individual interviews and focus groups conducted by research nurses and study investigators with 29 willing study participants from both the treatment and control groups to elicit descriptions of their experiences in the study. Groups and individual interviews were audio-recorded and transcribed verbatim. Guiding questions for group and individual interviews included: What was it like to have home visits from a CARE study nurse; what was or was not helpful; what else could have been helpful?
Data Analysis
Descriptive statistics were computed for all study variables at all data collection points to determine the presence of marked skewness, outliers, and systematic missing data. Appropriate adjustments were made for problems. As there were no systematic patterns of missing data, mean substitution based on individuals’ scores was employed for random missing data. Administration of measures during face-to-face home visits and a low attrition rate (6.7%) minimized missing data.
Preliminary Analyses
Cronbach’s alpha was computed for all study measures and subscales. Measures used in analyses demonstrated satisfactory evidence of internal consistency reliability ≥ .70 (Cronbach’s alphas: .76–.94 as specified above in measurement description). Appropriate descriptive statistics were computed for all variables across time points. Results are summarized in Table 3.
Table 3.
Means and Standard Deviations for all Care Study Measures from Baseline to 9 Months
| Variable | Baseline (6 weeks) |
3 Month | 6 Months | 9 Months | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| x | sd | n | x | sd | n | x | sd | n | x | sd | n | |
| EPDS | ||||||||||||
| Treatment | 12.15 | 4.7 | 66 | 9.16 | 4.4 | 62 | 8.27 | 5.2 | 62 | 7.19 | 3.8 | 62 |
| Control | 12.53 | 4.8 | 68 | 9.95 | 5.8 | 65 | 7.74 | 4.8 | 65 | 6.40 | 3.8 | 63 |
| PDSS | ||||||||||||
| Treatment | 93.26 | 22.1 | 66 | 75.30 | 24.3 | 63 | 68.39 | 25.1 | 62 | 63.55 | 22.8 | 62 |
| Control | 93.62 | 24.1 | 68 | 78.69 | 27.1 | 65 | 67.45 | 23.0 | 65 | 61.20 | 19.0 | 63 |
| NCATS | ||||||||||||
| Caregiver/Child Total | ||||||||||||
| Treatment | 45.65 | 11.8 | 65 | 49.52 | 11.4 | 61 | 51.15 | 9.1 | 62 | 53.16 | 8.3 | 62 |
| Control | 44.68 | 10.3 | 68 | 49.62 | 10.9 | 64 | 50.78 | 9.2 | 64 | 53.71 | 7.0 | 63 |
| Responsiveness Sub-scale | ||||||||||||
| Treatment | 6.17 | 2.8 | 65 | 6.52 | 2.9 | 61 | 6.66 | 2.9 | 62 | 7.44 | 3.1 | 62 |
| Control | 5.71 | 2.7 | 68 | 6.13 | 2.9 | 64 | 6.2 | 2.9 | 64 | 7.03 | 3.1 | 63 |
Note: EPDS= Edinburgh Postnatal Depression Scale; PDSS= Postpartum Depression Screening Scale; NCATS = Nursing Child Assessment Teaching Scale.
No significant differences were noted between the treatment and control group mothers at baseline on any variable. Therefore, the investigators concluded that the groups were equivalent and that the effects of all variables were randomly distributed. Prior to performing repeated measures analysis of variance (RANOVA) to test the hypotheses, assumptions of normality of sampling distribution, homogeneity of variance-covariance matrices, linearity, multicollinearity and singularity were checked with no significant violations noted. Choice of dependent variables for analyses departed somewhat from the original hypotheses as the obtained reliability for one NCATS subscale, i.e., Infant Clarity of Cues, was < .70. The investigators opted for a univariate, rather than multivariate approach as NCATS subscales were highly correlated (r = .851). Although multivariate analysis of variance (MANOVA) works well with highly negatively correlated dependent variables and acceptably well with moderately correlated dependent variables in either direction, employing MANOVA with very highly correlated dependent variables is wasteful. In addition, the univariate approach is more easily interpreted and presented (Tabachnick & Fidell, 2007). As a result, analysis of variance (ANOVA) and RANOVA with post hoc Bonferroni adjustments were employed to test hypotheses and results are displayed in Table 4. Means and standard deviations for all CARE measures for both treatment and control group mothers, from baseline to nine months are displayed in Table 3.
Table 4.
Results of RANOVA and Post hoc Comparisons* for NCATS, NCATS Responsiveness to Caregiver Sub-scale, and PDSS
| Dependent | Mean | |||
|---|---|---|---|---|
| Variable | F | P | Difference | P |
| NCATS TOTAL | 21.46 | p≤.001 | ||
| 6W-3M | 3.93 | P≤.001 | ||
| 6M-9M | 2.30 | p≤.05 | ||
| 6W-9M | 7.96 | p≤.001 | ||
| Responsiveness | 12.24 | p≤ .001 | ||
| 6W-9M | 1.14 | p≤.001 | ||
| PDSS | 75.85 | p≤ .001 | ||
| 6W-3M | 17.16 | p≤.001 | ||
| 3M-6M | 8.68 | p≤.001 | ||
| 6M-9M | 6.01 | p≤.001 | ||
| 6W-9M | 31.85 | p≤.001 |
Note: RANOVA = Repeated Measures Analysis of Variance; NCATS = Nursing Child Assessment Teaching Scale.; PDSS= Postpartum Depression Screening Scale; W= Weeks; M = months
Bonferroni Adjustment
Results
Hypothesis and Research Question Tests
Hypothesis 1
Hypothesis 1 posited that after participating in the CARE intervention the treatment group would have significantly higher maternal-infant relational effectiveness as measured by NCATS than the control group. To test the hypothesis, RANOVA was performed for treatment and control mothers at four time periods. Hypothesis 1was not supported. There was no significant interaction between time and group. However, both groups improved significantly over specific time periods. Although the largest overall gain was from 6 weeks to 9 months, significant gains were also noted from 6 weeks to 3 months and, to a lesser extent, from 6 months to 9 months (See Table 4).
Hypothesis 2
Hypothesis 2 posited that after participating in the CARE intervention the treatment group would have significantly higher scores than the control group on the Clarity of Cues subscale of the NCATS. This hypothesis was not tested due to the marginal reliability of the sub-scale. The hypothesis that the treatment group would have higher scores than the control group on the Responsiveness to Caregiver scale was tested with RANOVA. This hypothesis was not supported. However, again, both the treatment and control groups improved significantly over time with the most significant improvement observed from 6 weeks to 9 months. No significant interaction was found between group and time (See Table 4).
Research Question 1
Question 1 asked how maternal depression as measured by the PDSS varied over time for the treatment and control groups. RANOVA indicated no significant difference between the treatment and control group while holding time constant. No significant interaction was found between group and time. However, both groups had significant decreases in depression symptom severity from 6 weeks to 3 months, 3 months to 6 months, 6 months to 9 months, and overall from 6 weeks to 9 months (See Table 4).
Results from Focus Group and Individual Follow-up Interviews
Interviews were conducted with participants to understand their experiences while participating in the study. Content analysis (Miles & Huberman, 1994) was used to identify issues that included: concerns with video-recording, anxiety when performing NCATS tasks and increased focus on their interaction with their infants, group assignment questions, and the desire to connect with other mothers for mutual support. Several participants from both the treatment and control groups described how important the CARE study was to them as a source of support during the postpartum period. Control group mothers indicated that they received support and benefit from the nurse home visits. For example, one control group mother stated that she was not sure how she could “have another baby without the CARE study.” Additionally, the following typified responses: Several mothers indicated that completing the depression measures made them aware of their emotional state and validated how they were feeling emotionally. Another mother said that being video-recorded and instructed to “teach” her infant something (re: NCATS’ directions) made her aware that she could affect her infant by how she acted. One control group mother said that she would have liked more positive feedback and support about caring for her infant from her nurse. This response helped to confirm that nurses did not provide the intervention to the control group in terms of specific coaching and reinforcement. Finally, mothers (both treatment and control) agreed that the nurses’ visiting was supportive.
Discussion
Results showed no significant differences between the treatment and control groups for maternal-infant relational effectiveness, responsiveness to caregiver, or PPD symptom severity. Nonetheless, both groups did have significant improvement on all measures over time. Although the findings did not definitively support the efficacy of the CARE intervention, the results indicate that the protocol produced important results. Thus, home visits by the nurse for both treatment and control groups that featured the nurse’s active empathic listening to mothers during data collection, focused attention paid to mothers in the video-recorded sessions, and monitoring provided by completion of depression measures and the diagnostic interview, together likely constituted an unexpected form of treatment for the control group mothers. Self-reflection in completing the measures may have promoted self-monitoring by the mothers and created enough sense of attention to be an unintended intervention. It is also possible that unintentional natural modeling by nurses during data collection with the control group may have influenced results.
In Phase III, mothers validated the positive effects of the nurse home visits. The participants provided insights about how the home visit itself was helpful and supported the investigators’ sense that there were indeed two treatment groups supporting the research byOlds et al. (1994),Eckenrode et al. (2010), andKitzman et al. (2010) of the positive effect of nurse home visiting. Typically postpartum “usual care” care in the United States does not include such monitoring and regular interaction with a nurse. Perhaps, focused attention and support from a trained clinician, i.e., nurse, may be appropriate as a first-line treatment for PPD and maternal-infant interaction difficulties. Such an approach merits future study.
An alternative explanation for the findings is that positive change in maternal-infant relational effectiveness would have occurred over time without the study. However, we reject this explanation because findings from a previous study (Horowitz et al., 2001) showed a significant positive change in maternal-infant interaction for the treatment group that received behavioral mother-infant interactive coaching but not for the control group. The main differences between this previous study (Horowitz et al., 2001) and the study reported here are that the measure of maternal-infant interaction in the previous study did not instruct mothers to teach their babies something, no diagnostic interview was conducted, and the previous study ended at 4–5 months rather than 9 months postpartum. These differences suggest that aspects of the CARE study protocol, specifically confirmation of the mother’s PPD via the diagnostic interview that required disclosure and likely a sense of trust and connection to the nurse who conducted the diagnostic interview along with ongoing monitoring, and NCATS instructions to “teach” the infant, may well have produced positive, albeit inadvertent attention for the control group and resultant effects. Given that between group differences were not detected in the current study at any time, length of the study likely did not play a role in the results, however other differences noted above may have done so. Moreover, improvement over time in PPD severity alone or its treatment likely did not account for improvement in maternal-infant interaction given results of previous research (Forman et al., 2007; Kersten-Alverez, Hosman, Riksen-Walvaren, Van Doesum, & Hoefnagels, 2011).
Finally, maternal-infant relational effectiveness improved significantly from the time of the 6 week visit to the 3 month visit leading researchers to consider future interventions that would be of a shorter duration, but more frequent during early postpartum weeks to achieve a notable effect in a timely fashion. The findings of no between group differences may be due to insufficient intensity of the intervention (Melnyk & Morrison-Beedy, 2012). In addition, Phase III participants stated that more frequent intervention sessions during the first few weeks postpartum would have been helpful. Furthermore, the repeated measures data collection plan likely resulted in enough contact with the control group to produce unanticipated effects. Testing interventions to address specific issues of maternal distress in the context of PPD that were not addressed in this study, such as demands of infant care, also may be needed (Sidor, Kunz, Schweyer, Eickhorst, & Cierpka, 2011).
Strengths and Limitations
Strengths of the study include: recruitment of a large postpartum population for PPD screening, adequate sample size with minimal attrition, random assignment to groups, and the attention paid to internal validity. To ensure treatment fidelity, team meetings and debriefings were held regularly and study procedures were strongly emphasized. Participants readily gave consent to PPD screening, wanted to participate in a study that may help other mothers and consistently set up appointments for follow-up home visits. Lessons learned include the need to attend to possible effects of data collection procedures as an unintended monitoring intervention, as well as data collection instructions that may provide unintended messages that instruct participants about behavior.
Limitations included having NCATS as the sole measure of outcomes regarding maternal-infant interaction that may have limited our ability to distinguish subtle differences in maternal behaviors. Moreover, NCATS likely measures cognitive parenting factors more reliably than affective factors underlying mother-infant interaction and may also have some inherent cultural bias regarding parenting styles (Gross, Conrad, Fogg, Willis, & Garvey, 1993). Based on particpants’ feedback it also is likely that NCATS’ directions to teach your infant something planted the idea that mothers are capable of influencing their infants and thereby became an unintended intervention for both treatment and control groups. Future consideration is warranted of alternative measures of maternal-infant interaction that may more heavily weigh affective factors than NCATS. Additionally, although the sample was representative of the study’s geographic area, it did not match the national population of postpartum mothers. For example, participants in this sample likely had more education, were older, and may have been more likely to have English as a first language than the general population of postpartum women in the United States.
Another limitation was that the same nurses conducted both control and treatment visits, possibly leading to cross-contamination. Even though we attempted to preserve fidelity through ongoing staff training and de-briefing, we cannot insure that some cross-contamination did not occur. Nevertheless, when issues noted regarding the study implementation and findings of Phase II and III are considered, the authors are convinced that the protocol involving nurse home visits produced positive changes in maternal-infant interaction. The intensity of behavioral coaching likely was insufficient to produce a significant difference between the treatment and control groups. Implications for further study include: refining study interventions and testing under varied conditions to overcome the presence of a nurse as a confounding variable for the control condition while still protecting the safety of a vulnerable population, and/or fewer data collection points for the control group. However, inclusion of a control group without nurse home visits to measure the study intervention could be risky with this vulnerable population. Lessons learned include recognizing the possibility of an unintended effect of having nurses collect data and the effect of data collection as unintended monitoring/attention. To reduce effects of having nurses make home visits to collect data, future studies might include: data collection for the control group by non-nurse staff who are supervised by nurses and/or other clinicians to ensure safety monitoring, or delivery via technology that possibly could control for effects of home visits and presence of the nurse.
Implications
Screening for PPD is likely to become the norm in the United States due to mandates of the Patient Protection and Affordable Care Act (Patient Protection and Affordable Care Act, 2010). As screening becomes universal, the need for timely and efficient interventions for mothers with PPD and their infants will increase. This study validates that home visits by nurses can have an effect on outcomes for mothers with PPD and their infants during their first 9 months. This evidence also provides a rationale to refine and test this behavioral coaching intervention under varied conditions. Clinical interventions that extend throughout perinatal care and into general primary and pediatric care are warranted (Beck & Gable, 2001a. 2001b; Glavin, Smith, Sorum, & Ellefsen, 2010). Home visits performed by qualified nurses could provide an important safety net if incorporated into standard clinical practice for vulnerable populations of depressed mothers and their infants.
Acknowledgement
Funded by the National Institutes of Health, grant number R01 NR 008033.
Footnotes
Callout #1: Interventions for postpartum depression (PPD) have largely been aimed at treating maternal depression without focused attention on the disordered maternal-infant interaction often associated with PPD.
Callout #2: Participants had improved quality of interaction and decreased depression severity. Nurse home visits, self-reflection, and attention from participation likely contributed to improvements.
Callout #3: Results showed that nurse-led home visits were beneficial for all study participants and had a therapeutic effect for mothers with postpartum depression and their infants during the first 9 months postpartum.
Contributor Information
June Andrews Horowitz, A professor in the William F. Connell School of Nursing, Boston College, Chestnut Hill, MA.
Christine A. Murphy, An independent research analyst, Chestnut Hill, MA.
Katherine Gregory, An associate professor in the William F. Connell School of Nursing, Boston College, Chestnut Hill, MA.
Joanne Wojcik, An associate director for the Commonwealth Research Center and an instructor in psychiatry in the Department of Psychiatry, Harvard Medical School, Beth Israel Deaconess Medical Center, and The Massachusetts Mental Health Center, Boston, MA.
Joyce Pulcini, A professor in the School of Nursing, George Washington University, Washington, DC.
Lori Solon, A clinical instructor in the William F. Connell School of Nursing, Boston College, Chestnut Hill, MA.
References
- Abell S. Postpartum depression. Clinical Pediatrics. 2007;46:290–291. doi: 10.1177/0009922806290724. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. text rev. Washington, DC: Author; 2000. [Google Scholar]
- Barnard KE, Hammond MA, Boothe CL, Bee HL, Mitchell SK, Spieker SJ. Measurement and meaning of parent-child interaction. In: Morrison F, Lord C, Keating D, editors. Applied Developmental psychology. Vol. 3. San Diego, CA: Academic Press; 1989. [Google Scholar]
- Beck CT. Predictors of postpartum depression: An update. Nursing Research. 2001;50(5):275–285. doi: 10.1097/00006199-200109000-00004. [DOI] [PubMed] [Google Scholar]
- Beck CT, Gable RK. Postpartum depression screening scale: Development and psychometric testing. Nursing Research. 2000;49(5):272–282. doi: 10.1097/00006199-200009000-00006. [DOI] [PubMed] [Google Scholar]
- Beck CT, Gable RK. Comparative analysis of the performance of the postpartum depression screening scale with two other depression instruments. Nursing Research. 2001a;50:242–250. doi: 10.1097/00006199-200107000-00008. [DOI] [PubMed] [Google Scholar]
- Beck CT, Gable RK. Further validation of the postpartum depression screening scale. Nursing Research. 2001b;50(3):155–164. doi: 10.1097/00006199-200105000-00005. [DOI] [PubMed] [Google Scholar]
- Beck CT, Gable RK. Postpartum depression screening scale. Los Angeles, CA: Western Psychological Services; 2001c. [Google Scholar]
- Beck CT. Postpartum depression: It isn't just the blues. American Journal of Nursing. 2006;106(5):41–50. doi: 10.1097/00000446-200605000-00020. ISSN: 0002-936X-0002-936X. [DOI] [PubMed] [Google Scholar]
- Cox JL. Postnatal depression. Edinburgh, Scotland: Churchill Livingston Publishing Co.; 1986. [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: Development of the 10 item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Dawson G, Ashman SB. On the origins of a vulnerability to depression: The influence of the early social environment on the development of psychobiological systems related to risk for affective disorder. In: Nelson CA, editor. The effects of early adversity on neurobehavioral development: The Minnesota symposia on child psychology. Vol. 31. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. pp. 245–279. [Google Scholar]
- Diego MA, Field T, Jones NA, Hernandez-Reif M. Withdrawn and intrusive maternal interaction style and infant frontal EEG asymmetry shifts in infants of depressed and non-depressed mothers. Infant Behavior Development. 2006;29:220–229. doi: 10.1016/j.infbeh.2005.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckenrode J, Campa M, Luckey DW, Henderson CR, Cole R, Kitzman H, Olds DL. Long-term Effects of Prenatal and Infancy Nurse Home Visitation on the Life Course of Youths 19-Year Follow-up of a Randomized Trial. Archives of Pediatrics and Adolescent Medicine. 2010;164:9–15. doi: 10.1001/archpediatrics.2009.240. [DOI] [PubMed] [Google Scholar]
- Feldman R, Eidelmen A. Maternal postpartum behavior and the emergence of infant-mother and infant-father synchrony in preterm and full-term infants: The role of neonatal vagal tone. Development Psychology. 2007;49(3):90–302. doi: 10.1002/dev.20220. [DOI] [PubMed] [Google Scholar]
- Field T. Postpartum depression effects on early interactions, parenting and safety practices; A review. Infant Behavior and Development. 2010;33:1. doi: 10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T, Diego M. Maternal depressive effects on infant frontal EEG asymmetry. International Journal of Neuroscience. 2008;118:1081–108. doi: 10.1080/00207450701769067. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV axis disorders (SCID-1): Clinician version administration booklet. New York, NY: Biometrics Research Department, Columbia University; 1997. [Google Scholar]
- Forman DR, O'Hara MW, Stuart S, Gorman L, Larsen KE, Coy KC. Effective treatment for postpartum depression is not sufficient to improve the developing mother-child relationship. Development and Psychopathology. 2007;19(2):585–602. doi: 10.1017/S0954579407070289. [DOI] [PubMed] [Google Scholar]
- Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, Miller WC. Perinatal depression: Prevalence, screening accuracy, and screening outcomes. Agency for Healthcare Research and Quality. 2005;119:1–8. doi: 10.1037/e439372005-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson J, McKenzie-McHarg K, Shakespere J, Price J. A systemic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatrica Scandinavica. 2009;119:350–364. doi: 10.1111/j.1600-0447.2009.01363.x. [DOI] [PubMed] [Google Scholar]
- Glavin K, Smith L, Sorum R, Ellefsen B. Redesigned community postpartum care to prevent and treat postpartum depression in women - a one-year follow-up study. Journal of Clinical Nursing. 2010;19(21–22):3051–3062. doi: 10.1111/j.1365-2702.2010.03332.x. [DOI] [PubMed] [Google Scholar]
- Gross D, Conrad B, Fogg L, Willis L, Garvey C. What does the NCATS measure? Nursing Research. 1993;42:260–265. [PubMed] [Google Scholar]
- Horowitz JA. Interventions to promote maternal responsiveness and sensitivity. In: David DW, Logsdon MC, editors. Maternal sensitivity: A scientific foundation for practice. Hauppauge, NY: Nova Science Publishers, Inc.; 2011. pp. 285–296. [Google Scholar]
- Horowitz JA, Bell M, Trybulski JA, Munro BH, Moser D, Hartz SA, Sokol ES. Promoting responsiveness between mothers with depressive symptoms and their infants. Journal of Nursing Scholarship. 2001;33:323–329. doi: 10.1111/j.1547-5069.2001.00323.x. [DOI] [PubMed] [Google Scholar]
- Horowitz JA, Murphy CA, Gregory KE, Wojcik J. Community-based Postpartum Depression Screening: Results from the CARE Project. Psychiatric Services. 2009;60:432–434. doi: 10.1176/appi.ps.60.11.1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz JA, Murphy CA, Gregory KE, Wojcik J. A community-based screening initiative to identify mothers at risk for postpartum depression. Journal of Obstetric Gynecologic Neonatal Nursing. 2011;40:52–61. doi: 10.1111/j.1552-6909.2010.01199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber CJ. Documenting quality of parent-child interaction: Use of the NCAST scales. Infant and Young Children. 1991;4(1):63–75. [Google Scholar]
- Kersten-Alverez LE, Hosman CMH, Riksen-Walvaren JM, Van Doesum KTM, Hoefnagels C. Which preventive interventions effectively enhance depressed mothers’ sensitivity? A meta-analysis. Infant Mental Health. 2011;32:362–376. doi: 10.1002/imhj.20301. [DOI] [PubMed] [Google Scholar]
- Johnston M, Dixon D. Current issues and new directions in psychology and health: What happened to behavior in the decade of behavior? Psychology and Health. 2008;23:509–513. doi: 10.1080/08870440701816728. [DOI] [PubMed] [Google Scholar]
- Kitzman H, Olds DL, Cole RE, Hanks CA, Anson EA, Arcoleo K, Holmberg JR. Enduring effects of prenatal and infancy home visiting by nurses on children. Archives of Pediatric Adolescent Medicine. 2010;164:412–418. doi: 10.1001/archpediatrics.2010.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letourneau N, Salmani M, Duffett-Leger L. Maternal depressive symptoms and parenting of children from birth to 12 years. Western Journal of Nursing Research. 2010;33(7):662–685. doi: 10.1177/0193945909359409. [DOI] [PubMed] [Google Scholar]
- Mayberry LJ, Horowitz JA, Declercq E. Depression symptom prevalence and demographic risk factors among U.S. women during the first 2 years postpartum. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2007;36(6):542–548. doi: 10.1111/j.1552-6909.2007.00191.x. [DOI] [PubMed] [Google Scholar]
- Maxwell SE, Delaney HD. Designing experiments and analyzing data: A model comparison perspective. Belmont, CA: Wadsworth Publishers; 1990. [Google Scholar]
- Melnyk BM, Morrison-Beedy D. Intervention Research: Designing, conducting, analyzing, and funding. New York, NY: Springer Publishing Co; 2012. [Google Scholar]
- Miles M, Huberman M. Qualitative data analysis: An expanded sourcebook. 2nd ed. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- Nichols MP. Family therapy: Concepts and methods. Boston, MA: Allyn & Bacon; 2010. [Google Scholar]
- O'Hara M, Swain A. Rates and risk of postpartum depression: A meta-analysis. International Review of Psychiatry. 1996;8(1):37–54. [Google Scholar]
- Olds DL, Henderson CR, Kitzman H. Does prenatal and infancy nurse home visitation have enduring effects on qualities of parental caregiving and child health at 25 to 50 months of life? Pediatrics. 1994;93:89–98. [PubMed] [Google Scholar]
- Parsons CE, Young KS, Murray L, Stein A, Kringelbach ML. The functional neuroanatomy of the evolving parent-infant relationship. Progress in Neurobiology. 2010;91(3):220–241. doi: 10.1016/j.pneurobio.2010.03.001. [DOI] [PubMed] [Google Scholar]
- Patient Protection and Affordable Care Act, 2010. Congressional Budget Office (CBO) Patient Protection and Affordable Care Act, 2010. 2010 Retrieved from http://democrats.senate.gov/pdfs/reform/patient-protection-affordable-care-act-aspassed.pdf.
- Sandelowski M. Whatever happened to qualitative description? Research in Nursing & Health. 2000;23:334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Segre LS, Losch ME, O'Hara M. Race/ethnicity and perinatal depressed mood. Journal of Reproductive and Infant Psychology. 2006;24(2):99–106. [Google Scholar]
- Sidor A, Kunz E, Schweyer D, Eickhorst A, Cierpka M. Links between maternal postpartum depression symptoms, maternal distress, infant gender and sensitivity in a high-risk population. Child and Adolescent Psychiatry. 2011;5(7):1–7. doi: 10.1186/1753-2000-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein A, Malmberg LE, Sylva K, Barnes J, Leach P. The influence of maternal depression caregiving and socioeconomic status in the post-natal year on children's language development. Child: Care, Health, and Development. 2008;34(5):603–612. doi: 10.1111/j.1365-2214.2008.00837.x. [DOI] [PubMed] [Google Scholar]
- Summer G, Spietz A. Caregiver/parent-child interaction. Seattle, WA: NCAST-ANEVUW Pub; 1994. [Google Scholar]
- Tabachnick BG, Fidell LS. Use of multivariable statistics. 5th ed. Boston, MA: Pearson; 2007. [Google Scholar]
- Teti DM, Gelfand DM, Messinger D, Isabella R. Maternal depression and the quality of early attachment: An examination of infants, preschoolers, and their mothers. Development and Psychopathology. 1995;31(3):364–376. [Google Scholar]
- Van Doesum KTM, Riksen-Walraven JM, Hosman CMH, Hoefnagels C. A randomized controlled trial of home-visiting intervention aimed at preventing relationship problems in depressed mothers and their infants. Child Development. 2008;79(3):547–561. doi: 10.1111/j.1467-8624.2008.01142.x. [DOI] [PubMed] [Google Scholar]
- Weinberg MK, Tronick E, Beeghly M, Olson KL, Kernan H, Riley JM. Subsyndromal depressive symptoms and major depression in postpartum women. American Journal of Orthopsychiatry. 2001;7:87–97. doi: 10.1037/0002-9432.71.1.87. PMID: 11271721. [DOI] [PubMed] [Google Scholar]
- What Is the Reliability of the SCID? 2012 Retrieved from http://www.scid4.org/psychometric/scidI_reliability.html.
- What Is the Validity of the SCID? 2012 Retrieved from http://www.scid4.org/psychometric/scidI_validity.html.
- World Health Organization. Women's health. 2010 Retrieved from http://www.who.int.proxy.bc.edu/mental_health/management/depression/definition/en/