Abstract
Background
Episode-of-care payments are defined as a single lump-sum payment for all services associated with a single medical event or surgery and are designed to incentivize efficiency and integration among providers and healthcare systems. A TKA is considered an exemplar for an episode-of-care payment model by many policymakers, but data describing variation payments between hospitals for TKA are extremely limited.
Questions/purposes
We asked: (1) How much variation is there between hospitals in episode-of-care payments for primary TKA? (2) Is variation in payment explained by differences in hospital structural characteristics such as teaching status or geographic location, patient factors (age, sex, ethnicity, comorbidities), and discharge disposition during the postoperative period (home versus skilled nursing facility)? (3) After accounting for those factors, what proportion of the observed variation remains unexplained?
Methods
We used Medicare administrative data to identify fee-for-service beneficiaries who underwent a primary elective TKA in 2009. After excluding low-volume hospitals, we created longitudinal records for all patients undergoing TKAs in eligible hospitals encompassing virtually all payments by Medicare for a 120-day window around the TKA (30 days before to 90 days after). We examined payments for the preoperative, perioperative, and postdischarge periods based on the hospital where the TKA was performed. Confounding variables were controlled for using multivariate analyses to determine whether differences in hospital payments could be explained by differences in patient demographics, comorbidity, or hospital structural factors.
Results
There was considerable variation in payments across hospitals. Median (interquartile range) hospital preoperative, perioperative, postdischarge, and 120-day payments for patients who did not experience a complication were USD 623 (USD 516-768), USD 13,119 (USD 12,165-14,668), USD 8020 (USD 6403-9933), and USD 21,870 (USD 19,736-25,041), respectively. Variation cannot be explained by differences in hospital structure. Median (interquartile range) episode payments were greater for hospitals in the Northeast (USD 26,291 [22,377-30,323]) compared with the Midwest, South, and West (USD 20,614, [USD 18,592-22.968]; USD 21,584, [USD 19,663-23,941]; USD 22,421, [USD 20,317-25,860]; p < 0.001) and for teaching compared with nonteaching hospitals (USD 23,152 [USD 20,426-27,127] versus USD 21,336 [USD 19,352-23,846]; p < 0.001). Patient characteristics explained approximately 15% of the variance in hospital payments, hospital characteristics (teaching status, geographic region) explained 30% of variance, and approximately 55% of variance was not explained by either factor.
Conclusions
There is much unexplained variation in episode-of-care payments at the hospital-level, suggesting opportunities for enhanced efficiency. Further research is needed to ensure an appropriate balance between such efficiencies and access to care.
Level of Evidence
Level II, economic analysis.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-015-4445-0) contains supplementary material, which is available to authorized users.
Introduction
In an effort to slow what is viewed as unsustainable spending in the US Medicare program, researchers and policymakers have proposed bundled payments for certain diagnoses and procedures [9, 17]. Bundled payments would involve a single lump sum payment from Medicare (or another payer) to an integrated healthcare delivery system for an entire episode-of-care [24, 26]. The episode-of-care typically would include all preprocedure, periprocedure, and postdischarge services that a patient would receive during treatment for a well-circumscribed disease or condition [26]. There is hope that bundled payments would promote healthcare system integration and align incentives, thereby slowing growth in healthcare spending [4, 11, 12, 20].
However, the complexity of moving from the current fee-for-service payment model to a bundled payment model is enormous for everyone involved in the healthcare sector [30]. Before bundled payments can be implemented, the Centers for Medicare & Medicaid Services (CMS) needs to understand the typical payments (often referred to as “costs”) that Medicare makes for relevant procedures and conditions during an episode of care and then decide how to set a fair and equitable price while taking into account differences in patient complexity. Likewise, healthcare systems and physicians, who will assume “risk” under bundled payment models, need to have access to and understand their internal costs for each condition. Currently, there are few published studies describing episode-of-care payments for specific diagnoses and conditions [1, 3, 8].
Our objective was to describe hospital-level episode-of-care payments for patients who underwent primary elective TKA. In particular, we wanted to understand the range in payments across hospitals and how much of the variation that we observed could be explained by differences in patient factors (age, comorbidity) or hospital factors (teaching status, location). We anticipated that even for a well-circumscribed elective surgical procedure such as a TKA, we would observe much unexplained variability in episode-of-care payments across hospitals.
We asked: (1) How much variation is there between hospitals in episode-of-care payments for a primary TKA? (2) Is variation in payment explained by differences in hospital structural characteristics such as teaching status or geographic location, patient factors (age, sex, ethnicity, comorbidities), and discharge disposition during the postoperative period (home versus skilled nursing facility)? (3) After accounting for those factors, what proportion of the observed variation remains unexplained?
Materials and Methods
We conducted a retrospective analysis of US Medicare administrative data. Our analysis used five separate data files that we obtained from the CMS including: Medicare Part A files for inpatient admissions, hospital payments, and discharge disposition; carrier files for outpatient visits and payments; outpatient files for outpatient hospital-based visits; durable medical equipment files; and home health files. In combination, these files allowed us to construct longitudinal records for all fee-for-service Medicare enrollees who underwent a TKA in 2009 for a 120-day window extending from 30 days before surgery to 90 days after.
We began our analysis by identifying all fee-for-service Medicare beneficiaries who underwent a primary TKA in 2009 using the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) procedure code 81.54 in the Part A (hospital) data files. We verified that all TKAs in the Part A files had a corresponding physician claim in the Medicare Carrier Files using Current Procedural Terminology codes 27437, 27438, 27440, 27441, 27442, 27443, 27445, 27446 and 27447 [19, 32]. TKAs that could not be identified in the hospital and physician files were excluded because lack of both claims precluded us from accurately calculating complete Medicare payments.
We excluded several patient populations in an effort to identify a homogeneous population of patients who received a single elective primary TKA (Supplemental Fig. 1). We excluded patients who underwent more than one TKA during the index hospital stay, patients with acute fractures, and patients admitted from the emergency department in accordance with methods used in prior studies of primary TKA [7, 23]. We excluded patients who had not been enrolled continuously in Medicare Part A and Part B programs for 12 months preceding the TKA and 3 months after surgery. The requirement for 12 months of enrollment preceding the index surgery was necessary to allow us to be certain that each procedure represented the first TKA and not a readmission for a complication and/or early revision. The 3-month postprocedure enrollment was needed to allow for a full 90-day window for capturing postprocedure Medicare payments, including hospital readmissions. We excluded patients who qualified for Medicare on the basis of needing dialysis and patients who resided outside the United States because both populations would not be representative of the general population undergoing TKA. We also excluded patients for whom Medicare was not listed as the primary payer because in such cases, the Medicare payments might not fully capture all payments associated with the TKA.
After identifying all eligible patients who had TKAs (n = 167,186 patients treated in 2843 hospitals), we reviewed the number of eligible TKAs in Medicare beneficiaries across hospitals. After reviewing the distribution of cases across hospitals, we made the decision to exclude all hospitals with a volume less than the hospital median (37 eligible TKAs). The decision to exclude low-volume hospitals is consistent with statistical principles used by the CMS and others when evaluating hospital performance—in particular, that small sample sizes of lower-volume hospitals are insufficient for valid estimates of performance [21, 22]. For each patient who received a primary elective TKA in one of our study hospitals, we created a longitudinal record extending from 30 days before admission until 90 days after surgery; thus, the total episode of care for each patient extended for a full 120 days in accordance with current proposals for episode-of-care payments using the five data files described previously [9, 18, 24].
The patient-level Medicare data were augmented by several additional data sources. We obtained socioeconomic measures for each patient by linking each recipient of a TKA in the Medicare files to data available from the 2010 US Census including zip code-level median household income. We obtained hospital-level information including teaching status (membership in the Council of Teaching Hospitals), safety net status, ownership, and bed size by linking each hospital in the Medicare files to data from the American Hospital Association annual survey.
Statistical Analysis
First, we used descriptive statistics (mean, median, percentages) to explore the demographic characteristics (ie, age, sex, race), socioeconomic measures, and comorbidities of our cohort of TKA recipients. Comorbidities were identified by mapping specific ICD-9-CM codes to Chronic Condition Categories using methods developed by the CMS [5]. Comorbidities were identified using inpatient and outpatient files beginning 12 months before the TKA and continuing through hospital discharge. We identified seven discrete complications occurring after TKA during either the initial inpatient stay or subsequent hospitalization using methods developed by the CMS in consultation with contractors at Yale University [31]. Individual complications included myocardial infarction, pneumonia, sepsis, surgical site bleeding, pulmonary embolism, mechanical complication, and infection [2]. Second, we examined the characteristics of the hospitals included in our sample including TKA volume, geographic region, teaching status, hospital ownership, bed size, and nurse staffing ratio (nurse full-time-equivalents divided by adjusted patient days) using similar methods.
Third, we calculated the mean, median, and range in Medicare payments for the preoperative, perioperative, postdischarge, and entire 120-day episode of care for the 1430 hospitals included in our study. Calculations included Medicare transfers for direct and indirect medical education [6]. Analyses initially were conducted for all patients undergoing TKA (those who did and did not experience complications); analyses were repeated focusing exclusively on patients who did not experience a complication because we expected that complications would be a significant cause of variation in hospital-level payment differences (eg, some variation in episode-of-care payments might be explained by differences in complication rates). Fourth, we extended these analyses by evaluating the variation in preoperative, perioperative, and postdischarge payments after stratifying hospitals by geographic region, teaching status, for-profit status, and other hospital categories; these analyses allowed us to examine whether TKAs performed in certain types of hospitals tended to be associated with greater (or lesser) payments from Medicare.
Fifth, we stratified hospitals into quartiles of 120-day episode-of-care TKA payments, focusing only on patients who did not experience complications. We compared patient characteristics (sociodemographics, comorbidity) and hospital characteristics (eg, bed size, teaching status) with low (lowest quartile), high (highest quartile), and intermediate (all others) payments in an effort to understand potential patient- and hospital-level factors associated with greater and lesser payments. We used ANOVA to evaluate differences in continuous measures (eg, age, income) and the chi-square test for differences in categorical variables (eg, hospital teaching status). To examine the robustness of our findings, we repeated our analyses using all patients (ie, patients who did and did not experience complications).
Sixth, we used multilevel models to examine how TKA episode-of-care payments varied across individual hospitals while adjusting for patient- and hospital-level characteristics. For these analyses, log-transformed total episode-of-care TKA payments for each patient were the dependent variable (outcome), whereas predictors included patient sociodemographics, comorbidities, and hospital-level structural factors. Our analyses included seven different models that progressively adjusted for an increasing number of factors. Models 1 to 4 included all patients undergoing TKA: Model 1 = unadjusted model; Model 2 = adjusted for patient demographics and comorbidity; Model 3 = adjusted for patient demographics, comorbidity, and hospital factors; and Model 4 = included all Model 3 factors plus an indicator for whether a given patient did or did not experience a complication. Models 5 to 7 were identical to Models 1 to 3 but included only patients who did not experience a complication. We used a smearing retransformation approach to predict Medicare episode of payment for several hypothetical patient scenarios to illustrate the differences in payment that we identified, while accounting for the skewed distribution of payments [10] (Supplemental Table 1. Supplemental material is available with the online version of CORR®). We examined regression coefficients for individual patient- and hospital-level characteristics to examine factors associated with greater and lesser payments. These models also were used to calculate the mean episode-of-care payments for each hospital; we then used graphic methods to evaluate the distribution of mean hospital episode-of-care payments for each hospital in our sample.
All p values are two-tailed, with p less than 0.05 considered statistically significant. All statistical analyses were performed using SAS® 9.3 (SAS Institute Inc, Cary, NC, USA). This project was approved by the University of Iowa institutional review board.
After excluding all low-volume hospitals (1413 hospitals; 21,672 TKAs), our final cohort consisted of 145,514 patients who received TKAs performed in 1430 hospitals in 2009 (Table 1). The mean age of our cohort was approximately 75 years, 65% were female, and 91% were Non-Hispanic white. Among the 1430 hospitals included in our study, the mean annual Medicare TKA volume was nearly 102, 36% were teaching hospitals, and 15% were for profit (Supplemental Fig. 1, Supplemental Table 2. Supplemental materials are available with the online version of CORR®).
Table 1.
Characteristics of patients* and hospitals included in our sample
| Parameter | Number |
|---|---|
| Age (mean years; SD) | 75.3 (5.8) |
| Female, number (%) | 94,788 (65.1) |
| Race, number (%) | |
| Non-Hispanic white | 131,693 (90.5) |
| Black (or African American) | 6676 (4.6) |
| Asian/Pacific Islander | 1415 (1.0) |
| Hispanic | 4628 (3.2) |
| Native American/Alaska native | 499 (0.3) |
| Other | 558 (0.4) |
| Unknown | 45 (0.0) |
| Prevalence of key comorbid conditions, number (%) | |
| Cancer | 34,450 (23.7) |
| Diabetes | 49,331 (33.9) |
| Osteoarthritis | 145,491 (100.0) |
| Dementia | 9137 (6.3) |
| Coronary artery disease | 48,351 (33.2) |
| Chronic obstructive pulmonary disease | 25,570 (17.6) |
| Renal failure | 16,185 (11.1) |
| Median household income (mean USD; SD) | 57,329.80 (22,427.50) |
| Prevalence of key complications, number (%) | |
| One or more complications | 13,501 (9.3) |
| Acute myocardial infarction | 566 (0.4) |
| Pneumonia | 10,354 (7.1) |
| Sepsis/septicemia/shock | 584 (0.4) |
| Surgical site bleeding | 71 (0.1) |
| Pulmonary embolism | 1403 (1.0) |
| Mechanical complications | 585 (0.4) |
| Infection | 872 (0.6) |
| Hospitals with TKAs performed (n = 1430) Medicare TKA volume, mean (SD) |
101.8 (77.5) |
| Geographic census region, number (%) | |
| Northeast | 225 (15.9) |
| Midwest | 403 (28.4) |
| South | 536 (37.8) |
| West | 256 (18.0) |
| Teaching hospital, number (%) | 506 (35.6) |
| Bed size, mean (SD) | 173.0 (124.7) |
| Ownership, number (%) | |
| For profit | 218 (15.4) |
| Not for profit | 1062 (74.8) |
| Government | 140 (9.9) |
| Nurse-staffing ratio, mean (SD) | 3.3 (1.2) |
| Rural/urban, number (%) | |
| Rural | 233 (16.5) |
| Urban | 1183 (83.6) |
* Number of beneficiaries = 145,514; missing information on geographic census region = 10, bed size = 149, ownership status = 10, nurse-staffing ratio = 10, teaching status = 10, and rural/urban status = 14); nurse-staffing ratio = full-time equivalent divided by adjusted patient days.
Results
How Much Variation is There Between Hospitals in Episode-of-care Payments for Primary TKA?
There was large variation in Medicare payments in the preoperative, perioperative, postdischarge, and 120-day periods whether focusing on all patients undergoing TKA or focusing exclusively on patients who did not experience a complication (Table 2). The range between the highest and lowest payment hospitals for the preoperative, perioperative, postdischarge and total payments were USD 2165, 22,100, 24,036, and 38,791.
Table 2.
Variation in Medicare episode-of-care TKA payments|| (USD)
| Patient group | Preoperative* | Perioperative† | Postdischarge‡ | Total§ |
|---|---|---|---|---|
| All patients | ||||
| Mean (SD) | 694.00 (235.30) | 13,921.20 (2543.80) | 9188.60 (3092.10) | 23,797.10 (4918.80) |
| Median (IQR) | 655.20 (540.70–800.70) | 13,255.40 (12,264.50–14,795.60) | 8763.20 (7100.00–10,742.80) | 22,767.60 (20,552.00–26,015.60) |
| Range& | 2165.40 | 22,099.60 | 24,035.50 | 38,798.60 |
| Patients without complications | ||||
| Mean (SD) | 680.80 (230.90) | 13,783.70 (2487.20) | 8725.70 (2986.40) | 23,183.60 (4748.40) |
| Median (IQR) | 642.30 (530.90–789.90) | 13,080.30 (12,162.80–14,626.10) | 8298.90 (6643.60–10,295.10) | 22,186.10 (20,014.00–25,393.00) |
| Range | 2196.40 | 18,909.20 | 22,860.40 | 37,345.90 |
||All payments incurred during 120-day episode of care were attributed to the index admission hospital;*30 days before index admission date (exclusive); †entire duration of the index admission during which TKA was performed (from admission until discharge); ‡period after discharge from the index admission extending to 90 days after TKA. Patients who were hospitalized for 90 days or more during index admission would have no postdischarge costs. Patients who died during the index admission did not incur any postdischarge costs; &difference between hospital with the lowest and highest mean payment for each time; §preoperative + perioperative + postdischarge payment amount; IQR = interquartile range.
Is Variation in Payment Explained by Differences in Hospital Structural Characteristics?
In unadjusted analyses (Table 3), we found substantial differences in Medicare payment by geographic region (hospitals in the Northeast received higher payments), teaching status (teaching hospitals paid more), ownership (for profit paid less), and urban/rural location (rural hospitals paid less). More specifically, the mean total episode payment for hospitals in the Northeast was USD 26,886 compared with 21,139 in the Midwest, 22,184 in the South, and 23,548 in the West (p < 0.001). The mean total payment was lower for rural hospitals (USD 20,103) compared with urban hospitals (USD 22,315) (p < 0.001). The mean total payment also was significantly higher for patients who were discharged to inpatient rehabilitation (USD 31,840) and skilled care (USD 26,980) compared with home (USD 17,112) or home with home health support (USD 19,215) (p < 0.001). Results were similar when looking separately at the preoperative, perioperative, and postdischarge periods (Table 3). Patients who received a TKA at hospitals in the lowest quartile for episode-of-care payments (Table 4) tended to be younger, less often female, more often white, and had fewer comorbidities compared with patients treated in hospitals with higher episode-of-care costs. Hospitals with high episode-of-care payments were located more often in the Northeast and less often in the Midwest, South, or West. Hospitals receiving high payments also were more often major teaching hospitals and less often for profit. Results also were similar when analyses were repeated while including patients who experienced complications (Supplemental Table 2. Supplemental material is available with the online version of CORR®).
Table 3.
Payment according to hospital characteristics (patients without complications only)(USD)
| Hospital characteristics | Preoperative | Perioperative | Postdischarge | Total | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Median (IQR) | Mean (SD) | Median (SD) | Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | |
| Geographic census region1 | ||||||||
| Northeast (n = 225) | 787.80 (247.30) | 740.20 (625.60–887.10) | 15,015.70 (2764.30) | 14,485.40 (13,074.20–16,201.30) | 11083.80 (3546.20) | 10,853.90 (8342.20–13,439.50) | 26,886.00 (5794.90) | 26,291.00 (22,376.80–30,322.6) |
| Midwest (n = 403) | 643.00 (177.50) | 618.90 (517.10–742.20) | 13,029.10 (1562.50) | 12,704.30 (11,920.70–13,695.10) | 7471.20 (2388.60) | 7206.10 (5713.10–8987.10) | 21,138.9 (3346.30) | 20,613.90 (18592.00–22,967.90) |
| South (n = 536) | 639.40 (237.50) | 594.80 (487.80–752.30) | 13,235.80 (2381.30) | 12,617.60 (11,892.40–13,596.10) | 8319.90 (2296.40) | 8152.60 (6757.50–9617.60) | 22,184.20 (3813.30) | 21,584.40 (19,662.60–23,940.80) |
| West (n = 256) | 622.20 (194.00) | 593.50 (477.10–746.60) | 15,068.00 (2680.00) | 14,416.60 (13,188.70–16,615.60) | 7864.00 (2774.10) | 7463.70 (6113.50–9444.60) | 23,547.90 (4623.60) | 22,421.40 (20,316.90–25,859.50) |
| Teaching status2 | ||||||||
| Teaching (n = 506) | 675.00 (201.70) | 637.10 (538.20–768.70) | 14,808.60 (28,75.50) | 14,039.10 (12,796.70–16,095.50) | 8977.90 (3154.20) | 8449.10 (6764.50–10,362.50) | 24,456.10 (5358.80) | 23,152.40 (20,426.00–27,126.90) |
| Nonteaching (n = 914) | 653.00 (233.50) | 615.40 (500.40–765.70) | 13,225.30 (2018.70) | 12,730.10 (11,906.90–13,855.70) | 8134.10 (2705.30) | 7804.70 (6251.70–9648.70) | 22,005.00 (3916.20) | 21,336.00 (19,351.70–23,845.70) |
| Ownership3 | ||||||||
| For profit (n = 218) | 634.40 (231.00) | 591.20 (470.30–754.50) | 12,876.70 (1994.50) | 12,488.20 (11,646.70–13,567.90) | 8165.30 (2892.50) | 7804.50 (6349.00–9542.90) | 21,667.10 (4252.60) | 21,090.00 (18,854.00–23,853.50) |
| Not for profit (n = 1062) | 673.80 (224.30) | 637.80 (527.00–774.30) | 13,970.90 (2502.40) | 13,281.10 (12,315.30–14,982.30) | 8532.60 (2962.20) | 8088.80 (6427.10–10,121.10) | 23,171.20 (4745.50) | 22,095.90 (19,882.40–25,443.10) |
| Government (n = 140) | 604.00 (184.90) | 579.00 (487.00–691.60) | 13,834.90 (2666.50) | 12,788.10 (12,117.20–14,494.20) | 8112.40 (2356.40) | 8096.70 (6535.20–9353.90) | 22,543.80 (3993.00) | 21,797.30 (20,098.30–24,342.30) |
| Rural/urban4 | ||||||||
| Rural (n = 233) | 601.10 (220.10) | 576.60 (459.60–686.80) | 12,941.80 (1798.40) | 12,575.10 (11,876.60–13,470.50) | 6896.0 (2169.8) | 6670.70 (5410.30–8121.40) | 20,434.00 (2867.10) | 20,102.5 (18,401.40–21,794.00) |
| Urban (n = 1183) | 672.20 (221.80) | 631.00 (524.30–784.70) | 13,944.70 (2544.00) | 13,256.90 (12,236.10–14,982.30) | 8728.00 (2917.70) | 8280.40 (6711.10–10,269.10) | 23,337.80 (4730.70) | 22,314.50 (20,068.00–25,676.90) |
| Bed size5 | ||||||||
| < Median (n = 637) | 637.90 (204.50) | 610.70 (503.30–734.70) | 13,224.80 (2078.40) | 12,687.80 (11,959.10–13,788.90) | 7720.80 (2507.50) | 7384.50 (5933.40–9092.70) | 21,575.80 (3710.20) | 20,994.00 (19,090.30–23,217.80) |
| ≥ Median (n = 644) | 684.60 (238.30) | 644.60 (527.20–799.00) | 14,416.40 (2712.00) | 13,611.50 (12,561.10–15,654.00) | 9194.90 (3036.30) | 8755.70 (7185.30–10,591.10) | 24,290.80 (5049.70) | 23,132.20 (20,666.80–26,814.40) |
| Nurse-staff ratio6 | ||||||||
| < Median (n = 710) | 673.10 (243.40) | 631.60 (520.50–775.70) | 13,569.20 (2331.80) | 12,941.00 (12,130.10–14,270.50) | 8650.30 (2972.30) | 8221.50 (6555.60–10,274.60) | 22,887.10 (4661.30) | 210875.90 (19,736.40–24,842.10) |
| ≥ Median (n = 710) | 648.60 (199.70) | 614.60 (513.10–759.50) | 14,009.70 (2598.80) | 13,287.30 (12,230.00–15,025.20) | 8219.20 (2812.50) | 7844.50 (6332.00–9634.60) | 22869.70 (4608.10) | 21,861.50 (19,758.80–25,132.10) |
| Patient discharge destination7 | ||||||||
| Home (self-care) | 552.60 (790.40) | 327.00 (186.30–618.30) | 13,404.50 (2683.60) | 12,738.50 (11,778.60–14,133.90) | 3155.20 (4729.50) | 1859.70 (1101.20–3563.10) | 17,112.40 (5913.00) | 15 582.90 (13,940.30–18,292.90) |
| Home health agency | 606.90 (905.40) | 345.30 (190.90–693.90) | 13,340.20 (2802.30) | 12,782.20 (11,753.20–14,373.60) | 5268.80 (4438.60) | 4491.50 (3474.40–5822.70) | 19,215.70 (5584.70) | 18,144.10 (16,290.00–20,835.00) |
| Skilled nursing facility | 741.00 (1163.20) | 414.20 (232.40–868.80) | 14,090.00 (3041.90) | 13,234.90 (12,179.40–15,061.10) | 12,149.20 (7480.00) | 10,702.40 (7441.50–14,853.50) | 26,980.30 (8789.50) | 25,257.00 (21,275.20–30,429.90) |
| Inpatient rehabilitation | 826.50 (1276.80) | 463.40 (246.00–999.30) | 14,498.90 (3533.10) | 13,533.50 (12,138.70–15,990.50) | 16,514.20 (8383.50) | 15,009.20 (11,544.90–19,348.10) | 31,839.60 (10,017.70) | 29,846.10 (25,620.70–35,695.60) |
IQR = interquartile range; 1 = p < 0.001 for difference in each cost measure across regions; 2 = p < 0.001 for difference in each cost measure by teaching status, except preoperative costs where p = 0.0758; 3 = p < 0.001 for difference in each cost measure by ownership, except for postdischarge payments where p = 0.0898; 4 = p < 0.001 for each cost measure; 5 = p < 0.001 for each cost measure; 6 = p < 0.001 for difference in perioperative payment, p = 0.005 for difference in postoperative payments, p = 0.039 for difference in preoperative payments, and p = 0.944 for difference in total payments; 7 = p < 0.001 for each cost measure.
Table 4.
Characteristics of patients and hospitals with low, intermediate, and high episode-of-care payments (patients without complications only)
| Factor | Lowest payment (n = 357) | Intermediate payment (n = 716) | High payment (n = 357) | p value |
|---|---|---|---|---|
| Total Medicare payment, USD, mean (SD) | 18,166.20 (1253.10) | 22,012.70 (1431.10) | 29,342.00 (4080.30) | |
| Patient characteristics | ||||
| Age (years) | 75.0 (5.7) | 75.2 (5.7) | 75.6 (5.8) | < 0.001 |
| Sex, female | 23,090 (64.0) | 42,843 (64.8) | 20,378 (68.3) | < 0.001 |
| White | 34,002 (94.2) | 60,492 (91.5) | 25,062 (84.1) | < 0.001 |
| Black | 1145 (3.2) | 2964 (4.5) | 1896 (6.4) | |
| Other | 932 (2.6) | 2661 (4.0) | 2859 (9.6) | |
| Mean number of comorbid conditions | 3.7 (1.9) | 4.0 (2.0) | 4.4 (2.1) | < 0.001 |
| Median household income (USD) | 51,328.20 (17,021.90) | 55,206.10 (20106.00) | 69,668.90 (27,867.90) | < 0.001 |
| Discharge destination (%, SD) | ||||
| Home (self-care) | 37% (27) | 16% (18) | 8% (12) | < 0.0001 |
| Home health agency | 33% (26) | 39% (22) | 27% (20) | < 0.0001 |
| Inpatient rehabilitation | 5% (8) | 10% (14) | 18% (22) | < 0.0001 |
| Skilled nursing facility | 22% (15) | 33% (21) | 45% (27) | < 0.0001 |
| Hospital characteristics | ||||
| Medicare TKA volume, mean (SD) | 110.6 (75.2) | 101.8 (73.6) | 92.8 (86.2) | 0.0089 |
| Geographic census region, number (%) (missing = 10) | ||||
| Northeast | 18 (5.1) | 74 (10.4) | 133 (37.5) | < 0.001 |
| Midwest | 147 (41.6) | 207 (29.1) | 49 (13.8) | |
| South | 139 (39.4) | 302 (42.4) | 95 (26.8) | |
| West | 49 (13.9) | 129 (18.1) | 78 (22.0) | |
| Teaching hospital, number (%) (missing = 10) | 85 (24.1) | 236 (33.2) | 185 (52.1) | < 0.001 |
| Bed size, mean (SD) | 125.5 (90.4) | 167.9 (115.2) | 228.6 (148.2) | < 0.001 |
| Ownership, number (%) (missing = 10) | ||||
| For profit | 75 (21.3) | 107 (15.0) | 36 (10.1) | < 0.001 |
| Not for profit | 250 (70.8) | 525 (73.7) | 287 (80.9) | |
| Government | 28 (7.9) | 80 (11.2) | 32 (9.0) | |
| Nurse staffing ratio, mean (SD) | 3.4 (1.3) | 3.3 (1.0) | 3.3 (1.5) | 0.5052 |
| Rural/urban (missing = 14) | ||||
| Rural | 96 (27.3) | 120 (16.9) | 17 (4.8) | < 0.001 |
| Urban | 256 (72.7) | 591 (83.1) | 336 (95.2) | |
In adjusted regression analyses, patient-level factors associated with statistically significant (p < 0.05) increased episode-of-care payment included age, female sex, black race, and number of comorbid conditions. Hospital-level factors associated with increased payments included location in the Northeast, being a major teaching hospital, and location in an urban area (Supplemental Table 1. Supplemental materials are available with the online version of CORR®). Most of the factors associated with increased episode-of-care payment at the patient and hospital levels were consistent whether models did (Models 1–4) or did not include patients who experienced complications (Models 5–7).
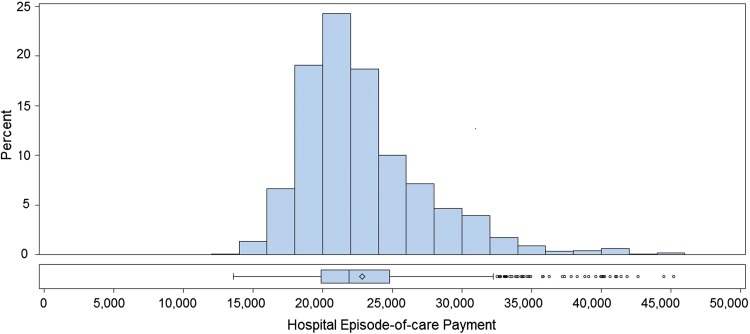
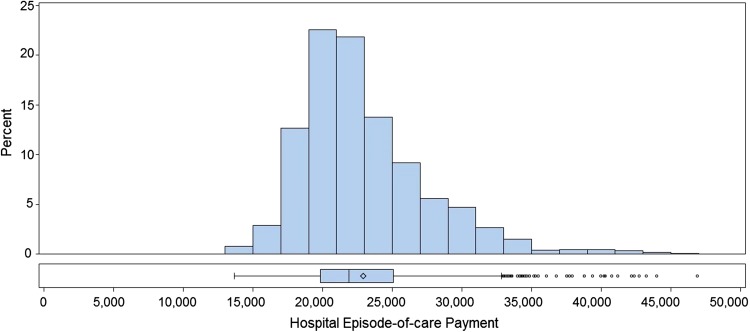
After adjusting for patient- and hospital-level factors (Model 3), median episode-of-care payments and interquartile range were USD 21,901 and USD 19,864 to USD 24,811 (Fig. 1). We repeated our analyses using unadjusted models and models that adjusted for patient demographics and comorbidity but not hospital factors with similar findings (Figs. 1, 2). In aggregate, the histograms show a substantial number of hospitals with extremely high and extremely low episode-of-care payments regardless of the statistical models that were used.
Fig. 1.
The histogram shows the mean hospital 120-day episode-of-care payments (in USD) for primary TKA adjusted for patient demographics, comorbidity, and hospital structural characteristics (teaching status, geographic region). Each hospital (n = 1430) receives one mean episode payment value. Diamond = mean; bar = mean; rectangular box = interquartile range in payments.
Fig. 2.
The histogram shows the mean hospital 120-day episode-of-care payments (in USD) for primary TKA unadjusted for patient demographics and comorbidity. Each hospital (n = 1430) receives one mean episode payment value. Diamond = mean; bar = mean; rectangular box = interquartile range in payments.
What Proportion of Observed Variation Remains Unexplained?
Patient characteristics explained approximately 15% of the variance observed in hospital payment, hospital characteristics explained 30% of variation in payment, and approximately 55% of variation in payment was not explained by either factor even when patients experiencing complications were excluded (Model 7). R2 values (a measure of model fit that ranges from 0–1) for Models 5, 6, and 7 were 0.0671, 0.1734, and 0.2542, respectively, with p values less than 0.001 for each, suggesting that moving from Models 5 to 7, each model offered a significantly greater performance than the prior model [16].
Discussion
The US Medicare program is moving away from a fee-for-service model toward new reimbursement models that encourage efficiency and coordination of care between physicians and health systems across inpatient and outpatient settings. Episode-of-care payment models encourage such efficiency by providing healthcare systems with one lump-sum payment for a group of services required for a circumscribed diagnosis or procedure [9, 27]. Elective primary TKA frequently is cited as an archetype of a procedure amenable to bundled payment [13]. However empirical data describing Medicare payments for TKA using an episode-of-care approach are almost nonexistent. Our objective was to evaluate variation in episode-of-care payments for TKA at the hospital level and to understand the extent to which variation could be explained by hospital factors (teaching status, geographic location). In an analysis of Medicare administrative data from 2009 we found that variation in episode-of-care TKA payments was extremely large across hospitals and not readily explained by differences in hospital structure or patient characteristics.
Our study has numerous limitations. First, our results are based on one calendar year; it is possible that hospitals’ episode-of-care payments might change year to year and that hospitals with high payments in one year might have lower payments in a subsequent year. Analysis of longitudinal performance would be important. Second, it is possible that the differences in payments we found might be reflective of unmeasured differences in patient complexity, although we found no evidence that this was the case. Third, our results were limited to one procedure performed on Medicare beneficiaries on a fee-for-service basis; extrapolation to other populations or procedures must be done with care. Fourth, although we identified primary TKA using previously described methods [7, 32], it is possible that our sample could have been contaminated by a limited number of patients who underwent other procedures (eg, arthroscopy, partial knee replacement). Specifically, approximately 95% of our population had ICD-9CM code 81.54 plus CPT code 27447 included and another 4% had CPT code 27446 (unicompartmental knee arthroplasty), but a small number of patients (approximately 1%) had other CPT codes included (eg, 27437 and 27438). Fifth, while the current analysis is focused mostly on hospital factors associated with variation in episode-of-care payments for TKA, the analysis does not delve deeply into patient factors; a separate study was published that focused entirely on patient factors associated with variation in episode of care payments [8].
We found that mean episode-of-care payments by CMS to hospitals differed by more than 100% between low-cost and high-cost hospitals (USD 15,000 versus USD 30,000); across an average volume of 100 primary TKAs per year, this translates to a substantial difference in cost to the CMS (USD 1,500,000 versus USD 3,000,000 for one hospital). From a different perspective, one healthcare system receives an extra USD 1,500,000 in payments during the course of a year. It is important to consider these findings in the context of prior studies. Birkmeyer et al. [1] and Miller et al. [28] published studies evaluating variations in episode-of-care payments for several common surgical procedures. Key findings included that hospital payments typically were the largest component of total episode payments (60%–80% of the total), payments to physicians typically were 12% to 15% of episode payments, and postacute payments were 5% to 10% of episode payments for most conditions [1]. Alternatively, Bozic et al. [3] focused on total joint arthroplasty performed at a large academic medical center and found that postdischarge payments comprised 36% of total payments and 49% of patients were discharged to postacute care. Our analysis showed that there is substantial variation in episode-of-care payments for primary TKA across hospitals.
We found that certain hospital characteristics and certain patient characteristics were associated with greater episode-of-care payments. In particular, hospitals in the Northeast and major teaching hospitals had higher episode payments. In considering the higher payments to teaching hospitals, these hospitals receive supplemental payment under the formula for calculating the diagnosis-related group-based reimbursement [23]; whether such payment is warranted is debatable [6]. Likewise, CMS payments are designed to vary with geography and cost of living, therefore our finding of higher episode-of-care payments in the Northeast may not be surprising [23]. Our finding that major teaching hospitals received higher payments and therefore are more expensive is not surprising and reinforces prior research quantifying excess payments to teaching hospitals [23]. As Chandra et al. reported [6], there is a general lack of clarity in the precise objectives of Medicare payments related to graduate medical education and uncertainty regarding whether these payments are helping to achieve these objectives. Expanding on prior studies [8, 15], we also found that several patient-level factors were associated with higher episode-of-care payments including female sex, black race, older age, and greater number of comorbid conditions. Finally, we found that postdischarge care, specifically discharge to an inpatient rehabilitation facility or skilled nursing facility was a significant driver of greater episode-of-care costs; our finding reinforces a prior report by the Medicare Payment Advisory Committee describing costs in postacute care as an important area of growth in spending [25].
In thinking about our findings, it is important to discuss some of the potential consequences of a move to bundled payments or other efforts to shift financial risk to hospitals or physicians. Current bundled payment projects underway at CMS typically consider an acute care admission as the entry point in the payment model [29]. Bundled payment models currently being tested do not explicitly adjust for patient demographics (age, race, sex) or comorbidity, although the formula used by CMS bases payments on each hospital’s historical performance; thus, in theory, hospitals that serve a population with a high burden of comorbid illness or of lower socioeconomic status would have some degree of financial protection since performance in these hospitals is being compared with their prior performance. Nevertheless, it is reasonable to be concerned that bundled payment models will provide further incentive for health systems to preferentially select patients who are likely to be lower risk, and thus potentially more profitable.
Our analysis suggests that approximately 55% of the variation we observed in episode-of-care payments to hospitals could not be explained by differences at the patient-level (eg, demographics, comorbidity, socioeconomic status) or the hospital level (eg, geographic location, teaching status) factors. What might explain the remaining differences in how much CMS is paying for TKAs across hospitals, and by extension, healthcare systems? One possibility is that there are unmeasured differences in patients receiving a TKA in different hospitals with respect to functional status, comorbidity, or socioeconomic status. For example, we lacked data regarding patients’ preoperative functional status and it is known that preoperative functional status is an important predictor of postoperative recovery [14]. If patient-level factors are a major contributor to differences in payments across hospitals, episode-of-care payment models would have the potential for harming hospitals serving a disproportionately more complex patient population. We also lacked numerous details regarding hospitals including corporate strategies and financial ties between hospitals, physicians, postacute care facilities, and home health agencies (ie, vertical integration). If variation in Medicare payments reflects practices by healthcare systems to maximize reimbursement, a shift to episode-of-care payment models could be extremely successful in improving efficiency and value for CMS, albeit to the detriment of healthcare providers.
In an analysis of Medicare administrative data, we found substantial variations in episode-of-care payments for primary elective TKAs based on the hospitals where patients received their procedures. We found that although some of the variation in payments could be explained by differences in patient demographics, comorbidity, and hospital structural characteristics, much of the variation could not be explained. Policy makers should respond to these data by recognizing that payments should continue to reflect the greater risk and expense inherent in performing TKA in certain subgroups. Hospitals, health systems, and physician leaders must recognize that there is significant unexplained variation in costs of TKA and that unwarranted excessive costs will increasingly be targeted as areas for cost savings.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Footnotes
The institution of one of the authors (PC) has received, during the study period, funding from the National Institutes of Health (K24 AR062133 and R01 AG033035).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that the institutional review board at the University of Iowa approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the University of Iowa, Iowa City, IA.
References
- 1.Birkmeyer JD, Gust C, Baser O, Dimick JB, Sutherland JM, Skinner JS. Medicare payments for common inpatient procedures: implications for episode-based payment bundling. Health Serv Res. 2010;45:1783–1795. doi: 10.1111/j.1475-6773.2010.01150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bozic KJ, Grosso LM, Lin Z, Parzynski CS, Suter LG, Krumholz HM, Lieberman JR, Berry DJ, Bucholz R, Han L, Rapp MT, Bernheim S, Drye EE. Variation in hospital-level risk-standardized complication rates following elective primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2014;96:640–647. doi: 10.2106/JBJS.L.01639. [DOI] [PubMed] [Google Scholar]
- 3.Bozic KJ, Ward L, Vail TP, Maze M. Bundled payments in total joint arthroplasty: targeting opportunities for quality improvement and cost reduction. Clin Orthop Relat Res. 2014;472:188–193. doi: 10.1007/s11999-013-3034-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Medicare and Medicaid Services. 2013 Annual report of the board of trustees of the federal hospital insurance and federal supplementary medical insurance trust funds. 2013. Available at: Available at: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/ReportsTrustFunds/index.html. Accessed June 28, 2014.
- 5.Centers for Medicare & Medicaid Services (CMS). Chronic conditions data warehouse. Available at: https://www.ccwdata.org/web/guest/home. Accessed July 29, 2015.
- 6.Chandra A, Khullar D, Wilensky GR. The economics of graduate medical education. N Engl J Med. 2014;370:2357–2360. doi: 10.1056/NEJMp1402468. [DOI] [PubMed] [Google Scholar]
- 7.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA. 2012;308:1227–1236. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cram P, Lu X, Li Y. Bundled payments for elective total knee arthroplasty: an analysis of Medicare administrative data. Geriatr Orthop Rehabil. 2015;6:3–10. doi: 10.1177/2151458514559832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cutler DM, Ghosh K. The potential for cost savings through bundled episode payments. N Engl J Med. 2012;366:1075–1077. doi: 10.1056/NEJMp1113361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duan N. Smearing estimate: a nonparametric retransformation method. J Am Stat Assoc. 1983;78:605–610. doi: 10.1080/01621459.1983.10478017. [DOI] [Google Scholar]
- 11.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138:273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 12.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138:288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- 13.Froimson MI, Rana A, White RE, Jr, Marshall A, Schutzer SF, Healy WL, Naas P, Daubert G, Iorio R, Parsley B. Bundled payments for care improvement initiative: the next evolution of payment formulations: AAHKS Bundled Payment Task Force. J Arthroplasty. 2013;28(8 suppl):157–165. doi: 10.1016/j.arth.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 14.Hawker GA, Badley EM, Borkhoff CM, Croxford R, Davis AM, Dunn S, Gignac MA, Jaglal SB, Kreder HJ, Sale JE. Which patients are most likely to benefit from total joint arthroplasty? Arthritis Rheum. 2013;65:1243–1252. doi: 10.1002/art.37901. [DOI] [PubMed] [Google Scholar]
- 15.Hawker GA, Badley EM, Croxford R, Coyte PC, Glazier RH, Guan J, Harvey BJ, Williams JI, Wright JG. A population-based nested case-control study of the costs of hip and knee replacement surgery. Med Care. 2009;47:732–741. doi: 10.1097/MLR.0b013e3181934553. [DOI] [PubMed] [Google Scholar]
- 16.Hosmer DW, Lemeshow S. Applied Logistic Regression. New York, NY: Wiley Interscience; 2000. [Google Scholar]
- 17.Hussey PS, Eibner C, Ridgely MS, McGlynn EA. Controlling U.S. health care spending–separating promising from unpromising approaches. N Engl J Med. 2009;361:2109–2111. doi: 10.1056/NEJMp0910315. [DOI] [PubMed] [Google Scholar]
- 18.Hussey PS, Ridgely MS, Rosenthal MB. The PROMETHEUS bundled payment experiment: slow start shows problems in implementing new payment models. Health Aff (Millwood). 2011;30:2116–2124. doi: 10.1377/hlthaff.2011.0784. [DOI] [PubMed] [Google Scholar]
- 19.Katz JN, Bierbaum BE, Losina E. Case mix and outcomes of total knee replacement in orthopaedic specialty hospitals. Med Care. 2008;46:476–480. doi: 10.1097/MLR.0b013e31816c43c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ko DT, Tu JV, Austin PC, Wijeysundera HC, Samadashvili Z, Guo H, Cantor WJ, Hannan EL. Prevalence and extent of obstructive coronary artery disease among patients undergoing elective coronary catheterization in New York State and Ontario. JAMA. 2013;310:163–169. doi: 10.1001/jama.2013.7834. [DOI] [PubMed] [Google Scholar]
- 21.Krumholz HM, Wang Y, Mattera JA, Wang Y, Han LF, Ingber MJ, Roman S, Normand SL. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with an acute myocardial infarction. Circulation. 2006;113:1683–1692. doi: 10.1161/CIRCULATIONAHA.105.611186. [DOI] [PubMed] [Google Scholar]
- 22.Krumholz HM, Wang Y, Mattera JA, Wang Y, Han LF, Ingber MJ, Roman S, Normand SL. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with heart failure. Circulation. 2006;113:1693–1701. doi: 10.1161/CIRCULATIONAHA.105.611194. [DOI] [PubMed] [Google Scholar]
- 23.Li Y, Lu X, Wolf BR, Callaghan JJ, Cram P. Variation of Medicare payments for total knee arthroplasty. J Arthroplasty. 2013;28:1513–1520. doi: 10.1016/j.arth.2013.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mechanic R, Tompkins C. Lessons learned preparing for Medicare bundled payments. N Engl J Med. 2012;367:1873–1875. doi: 10.1056/NEJMp1210823. [DOI] [PubMed] [Google Scholar]
- 25.Medicare Payment Advisory Commission (MedPAC). Approaches to bundling payments for post-acute care. Available at: http://www.medpac.gov/documents/reports/jun13_ch03.pdf?sfvrsn=0. Accessed June 8, 2015.
- 26.Medicare Payment Advisory Commission (MedPAC). A path to bundled payments around a hospitalization. Available at: http://67.59.137.244/chapters/Jun08_Ch04.pdf. Accessed June 8, 2015.
- 27.Mehrotra A, Hussey P. Including physicians in bundled hospital care payments: time to revisit an old idea? JAMA. 2015;313:1907–1908. doi: 10.1001/jama.2015.3359. [DOI] [PubMed] [Google Scholar]
- 28.Miller DC, Gust C, Dimick JB, Birkmeyer N, Skinner J, Birkmeyer JD. Large variations in Medicare payments for surgery highlight savings potential from bundled payment programs. Health Aff (Millwood). 2011;30:2107–2115. doi: 10.1377/hlthaff.2011.0783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tsai TC, Joynt KE, Wild RC, Orav EJ, Jha AK. Medicare’s Bundled Payment initiative: most hospitals are focused on a few high-volume conditions. Health Aff (Millwood). 2015;34:371–380. doi: 10.1377/hlthaff.2014.0900. [DOI] [PubMed] [Google Scholar]
- 30.Weeks WB, Rauh SS, Wadsworth EB, Weinstein JN. The unintended consequences of bundled payments. Ann Intern Med. 2013;158:62–64. doi: 10.7326/0003-4819-158-1-201301010-00012. [DOI] [PubMed] [Google Scholar]
- 31.Yale Center for Outcomes Research and Evaluation. Hospital-level risk-standardized complication rate following elective primary total hip arthroplasty (THA) and/or total knee arthroplasty (TKA): measure methdology report. 2012. Available at: Available at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier4&cid=1228772504368.
- 32.Yale Center for Outcomes Research and Evaluation. Hospital-level risk standardized payment associated with 90-day episode of care for elective primary total hip arthroplasty (THA) and knee arthroplasty (TKA). 2014. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/CallforPublicComment.html. Accessed October 27, 2014.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.