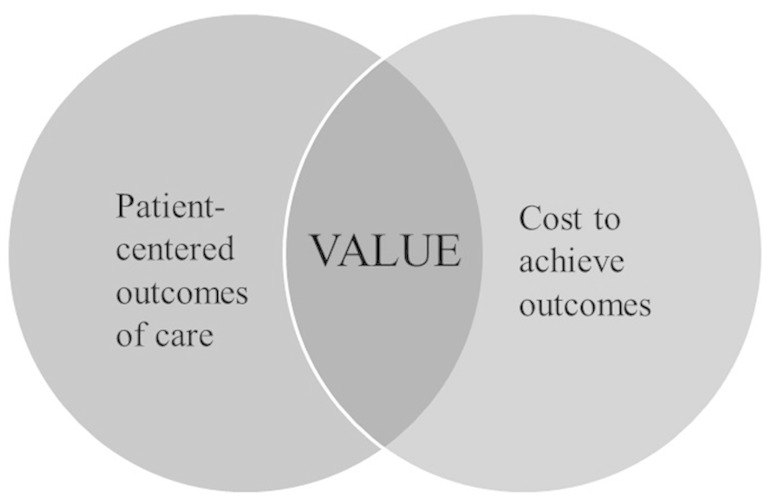
According to renowned strategy experts Michael Porter and Elizabeth Olmstead Teisberg [6], the common bond that unites all healthcare stakeholders is our desire to improve value for patients. Value, defined as health outcomes achieved per healthcare dollar spent, is the center of the Venn diagram between outcomes and costs (Fig. 1), and despite varying perspectives, all stakeholders are focused on this goal. Physicians, including orthopaedic surgeons, are well-positioned to implement strategies to improve value for our patients, given our experience as front-line care providers and our interactions with key healthcare stakeholders, including hospitals, payers, purchasers, and most importantly, patients. We make the case that standardization of care along evidence-based guidelines is the most predictable path to enhancing value in healthcare.
Fig. 1.
Value, defined as health outcomes achieved per healthcare dollar spent, is the center of the Venn diagram between outcomes and costs.
W. Edward Deming’s teachings and training helped revitalize Japan’s economy and development in the wake of WWII. During that period, the Japanese manufacturing sector achieved never-before-seen levels of quality [4]. His work on process improvement is also widely known and accepted in the management science world. Deming emphasized the identification and reduction of variation in any process as the natural basis for improving quality. Understanding a process in detail and differentiating between “normal” and “special cause” variation is the key to eliminating waste and continuing improvement. Deming argued that decreased cost and improved quality follow naturally from this process.
One may ask, “How does this apply to healthcare?” Deming would likely respond that any endeavor can be represented as a process. If our goal is to improve the quality of the system, then it starts with accurate data and statistical process measurement. In order to ensure that all patients having a surgical procedure receive prophylactic antibiotics, the process must be broken down into its component parts, such as writing the order, obtaining the medication, starting the IV, and giving the medication. By studying the process in this way, and gathering data to identify the sources of variation, one’s improvement effort can be applied to the most appropriate aspect of the process.
Of course this is an oversimplified example, but care “pathways” offer many potential benefits of in terms of improved efficiency and greater alignment across physicians and health systems. If your practice or health system is considering participating in a bundled payment program, then reducing variation in both processes and outcomes of care will be crucial to its success. Bosco and colleagues [2] established a standardized care pathway in their drive to implement a bundled payment for spine and total joint arthroplasty procedures at NYU Langone Medical Center. Through standardization of scheduling, preoperative testing, and perioperative coordination, they demonstrated substantial improvements in cancellation rates, on-time operating room starts, and operating room utilization. Other investigators [4] have demonstrated reduced costs and shorter hospital stays for invasive procedures following implementation of standardized care pathways. Common sense suggests that standardized preoperative and postoperative order sets will improve a healthcare delivery team’s ability to comply with evidence-based guidelines for perioperative antibiotic regimens, venous thromboembolism prophylaxis, and Foley catheter removal.
However, while reducing costs and utilization of scarce healthcare resources are important, surgeons are most interested in improving patient outcomes and avoiding complications. Our patients should always come first when making changes to our practices. So the real question is, “Do standardization efforts yield improved patient outcomes?” Rotter et al. [9] published a systematic review using Cochrane methodology in 2008 that combined studies of clinical pathway implementation from 1966 to 2006. A total of 13 randomized controlled trials and four “controlled clinical trials” were included, addressing a variety of conditions and more than 4000 patients. Most of the trials showed a lower length of stay with a stronger effect for invasive procedures. Four out of six trials also demonstrated cost reductions. However, they reported no differences in readmission and in-hospital complication rates between clinical pathways and “usual care.” An updated systematic review on the impact of care pathways on cost and outcomes published by the same group in 2010 [8], which included 27 studies representing 11,398 patients, found reductions in hospitals costs, length of stay, and in-hospital complications associated with clinical pathways. They also reported improved documentation and no difference in mortality or readmissions.
Specific to hip and knee replacement, Barbieri and colleagues [1] performed a meta-analysis of 22 trials (6316 patients) comparing clinical pathways with standard care. This analysis reported fewer postoperative complications, shorter length of stay, and no difference in rates of discharge to home with clinical pathways. Although costs were lower with pathways, these authors suggested that cost-effectiveness could not be measured because no studies attempted to quantify the cost of creating, implementing, and maintaining those pathways. In a large 2010 study of the Premier Perspective database [3] that used adherence to evidence-based care (appropriate antibiotic prophylaxis, beta-blockade, and venous thromboembolism prophylaxis) to identify process standardization, the investigators found that higher surgeon volume and higher hospital volume were associated with decreased risk of readmission and higher likelihood of being discharged to home. However, process standardization was a more important predictor of outcome than surgeon or hospital volume. After adjusting for patient characteristics, surgeon volume, and hospital volume, maximizing process standardization resulted in improved clinical outcomes (decreased risk of death, readmission, reoperation, or surgical complication) and shorter length of stay.
Although few investigators have evaluated the impact of standardization on patient experience, pain, and functional status, many studies have demonstrated the correlation between standardized care protocols and a reduction in surgical complications, readmissions, reoperations, and length of hospital stay. In that context, the evidence clearly points toward the standardization of care processes as a quality-improvement tool. With implementation of more-sophisticated electronic medical records and data gathering, we likely will have better evidence in the near future to support a strong correlation between implementation of clinical care pathways and higher levels of patient satisfaction and patient-reported outcomes.
Standardized care pathways have been criticized in the past as “cookbook” medicine [1, 2, 5, 7], and are, therefore, considered a threat to physician autonomy. However, we believe that most users eventually find that these tools enhance a provider’s ability to incorporate the important tenets of patient care, and can be modified to meet the specific needs of individual patients as necessary. When these efforts are expanded to include the use of standardized processes in the operating room (including equipment and implants), surgeons may find that their teams are more prepared and more efficient in their ability to care for patients. It seems only sensible that some portion of the association between high-volume surgeons and hospitals and improved patient outcomes is related to repetition of processes. By establishing process measurement and continuous improvement according to Deming’s principles, high-quality care pathways can be established and then disseminated to lower volume providers; thereby extending the “high volume” benefit to a wider group of patients.
We believe that care pathways can minimize unwanted process variation in a complex system, allowing lower-volume providers to achieve improved care quality and value, and helping high-volume providers to refine an already efficient system. Complications should become less common, and costs will decrease. This is a “pathway” we might all benefit from following.
Footnotes
A Note from the Editor-in-Chief: We are pleased to present to readers of Clinical Orthopaedics and Related Research® the latest Orthopaedic Healthcare Worldwide column. This section explores the political, social, and economic issues associated with delivering musculoskeletal care in the many environments in which our specialty is practiced, both in the United States and around the world. We welcome reader feedback on all of our columns and articles; please send your comments to eic@clinorthop.org.
The authors certifies that they, or any members of their immediate families, have no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
The opinions expressed are those of the writers, and do not reflect the opinion or policy of CORR ® or The Association of Bone and Joint Surgeons®.
References
- 1.Barbieri A, Vanhaecht K, Van Herck P, Sermeus W, Faggiano F, Marchisio S, Panella M. Effects of clinical pathways in the joint replacement: A meta-analysis. BMC Med. 2009;7:32. doi: 10.1186/1741-7015-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bosco J, Shah PC, Slover JD, Torrance A. Optimizing the OR for bundled payments: A case study. Bull Am Coll Surg. 2014;99:29–36. [PubMed] [Google Scholar]
- 3.Bozic KJ, Maselli J, Pekow PS, Lindenauer PK, Vail TP, Auerbach AD. The influence of procedure volumes and standardization of care on quality and efficiency in total joint replacement surgery. J Bone Joint Surg Am. 2010;92:2643–2652. doi: 10.2106/JBJS.I.01477. [DOI] [PubMed] [Google Scholar]
- 4.Deming WE. The New Economics for Industry, Government, and Education. 2. Cambridge, MA: The MIT Press; 2000. [Google Scholar]
- 5.Doroshow J. Cookbook medicine is a recipe for disaster. Available at: http://www.huffingtonpost.com/joanne-doroshow/cookbook-medicine_b_2792900.html. Accessed July 30, 2015.
- 6.Porter ME, Teisberg EO. Redefining Health Care: Creating Value-Based Competition on Results. Boston, MA: Harvard Business Review Press; 2006. [Google Scholar]
- 7.Reese S. Will you be pressured to perform “cookbook” medicine? Available at: http://www.medscape.com/viewarticle/808258. Accessed July 30, 2015.
- 8.Rotter T, Kinsman L, James E, Machotta A, Gothe H, Willis J, Snow P, Kugler J. Clinical pathways: Effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev. 2010;3:CD006632. DOI: 10.1002/14651858.CD006632.pub2. [DOI] [PubMed]
- 9.Rotter T, Kugler J, Koch R, Gothe H, Twork S, van Oostrum JM, Steyerberg EW. A systematic review and meta-analysis of the effects of clinical pathways on length of stay, hospital costs and patient outcomes. BMC Health Serv Res. 2008;8:265. doi: 10.1186/1472-6963-8-265. [DOI] [PMC free article] [PubMed] [Google Scholar]