Abstract
Objectives
As part of a large randomized controlled trial, we assessed the impact of two early primary care parenting interventions—the Video Interaction Project (VIP) and Building Blocks (BB)—on the use of physical punishment among low-income parents of toddlers. We also determined whether the impact was mediated through increases in responsive parenting and decreases in maternal psychosocial risk.
Methods
Four hundred thirty-eight mother-child dyads (161 VIP, 113 BB, 164 Control) were assessed when children were 14 and/or 24 months. Mothers were asked about their use of physical punishment as well as their responsive parenting behaviors, depressive symptoms, and parenting stress.
Results
VIP was associated with lower physical punishment scores at 24 months, as compared with BB and Controls. In addition, fewer VIP parents reported ever using physical punishment as a discipline strategy. Significant indirect effects were found for both responsive parenting and maternal psychosocial risk, indicating that VIP affects these behaviors and risk factors, and this is an important pathway through which VIP affects parents’ use of physical punishment.
Conclusion
The results support the efficacy of VIP, and the role of pediatric primary care, in reducing the use of physical punishment among low-income families by enhancing parent-child relationships. In this way, the findings support the potential of VIP to improve developmental outcomes for at-risk children.
Keywords: Primary care, Parenting, physical punishment
Recent surveys suggest that physical punishment in the U.S., although declining, is used by approximately two-thirds of parents.1 Rates of physical punishment are higher in families with low education and income, and peak in toddlerhood, when as many as 94 percent of parents use this type of discipline.3 These findings are troubling, given the variety of negative outcomes associated with early physical punishment, including increases in externalizing and internalizing behavior problems in childhood, and increases in depression and substance use in adolescence and adulthood.4,5 Even low levels of spanking at age 5 are associated with more externalizing problems, after controlling for risk and previous behavior problems.6 Because of these effects, and because physical punishment is no more effective than other discipline strategies (e.g., time-out), the American Academy of Pediatrics recommends that pediatricians help parents develop alternative tactics.7 Thus, identifying effective strategies to reduce physical punishment, especially among those at increased risk—namely, low-income parents of toddlers—is critical for ensuring optimal child development.
Several platforms, or avenues, for such intervention have been investigated, including home visiting, community-based, and pediatric healthcare. Home visiting programs, such as Nurse-Family Partnership and Family Check-Up, as well as community interventions, like the Triple P Positive Parenting Program and Chicago Parent Program, have been effective in reducing punitive and coercive parenting.8,9,10,11 However, these programs have several barriers to large-scale dissemination, including cost and logistics of engagement and participation.10,12
Pediatric primary care is a unique platform that can facilitate delivery of preventive interventions related to parenting through frequent, nearly universal access to families in the first five years of a child’s life, due to requirements for screening and vaccinations prior to school entry in the U.S. Additionally, in pediatric primary care, interventions can be delivered early, beginning shortly after birth, and at low cost to families who are already engaged in services with a trusted provider. Despite this potential, there has been limited research in the use of pediatric primary care interventions in reducing physical punishment. Investigation of Healthy Steps, which links pediatric primary care to home visiting, supports the promise of this platform, as participating parents had lower odds of using severe discipline, and were more likely to use non-physical, authoritative parenting strategies—especially if they were near or below the poverty line.13
The current study examined effects on physical punishment of two preventive interventions—the Video Interaction Project (VIP) and Building Blocks (BB)—which, like Healthy Steps, utilize pediatric primary care, but cost approximately 50 to 75% less, respectively. Both VIP and BB have been shown to have beneficial effects on parenting behaviors and psychosocial stressors like maternal depression and VIP has also been associated with reduced parenting stress14,(15) – factors likely to affect physical punishment.16 Indeed, a large body of research has indicated that physical punishment is related parental stress and, inversely, to positive parenting.2, 16 VIP uses videorecordings of the parent and child interacting together, taken at each pediatric well-child visit, to promote self-reflection and thereby encourage positive, responsive parenting behaviors.17 BB utilizes mailed, age-paced parenting newsletters that promote responsive parenting strategies, which can be incorporated into parents' home routines.
In this study, we investigated effects of VIP and BB on rates of physical punishment of toddlers in low-income families. It was hypothesized that (1) physical punishment would be reduced among parents participating in either VIP or BB compared to control families, and that (2) increases in physical punishment into toddlerhood, if existent, would be less pronounced among intervention parents. Further, we predicted that (3) increases in responsive parenting behavior and decreases in maternal psychosocial risk would facilitate these lower rates of physical punishment.
METHODS
Study Design
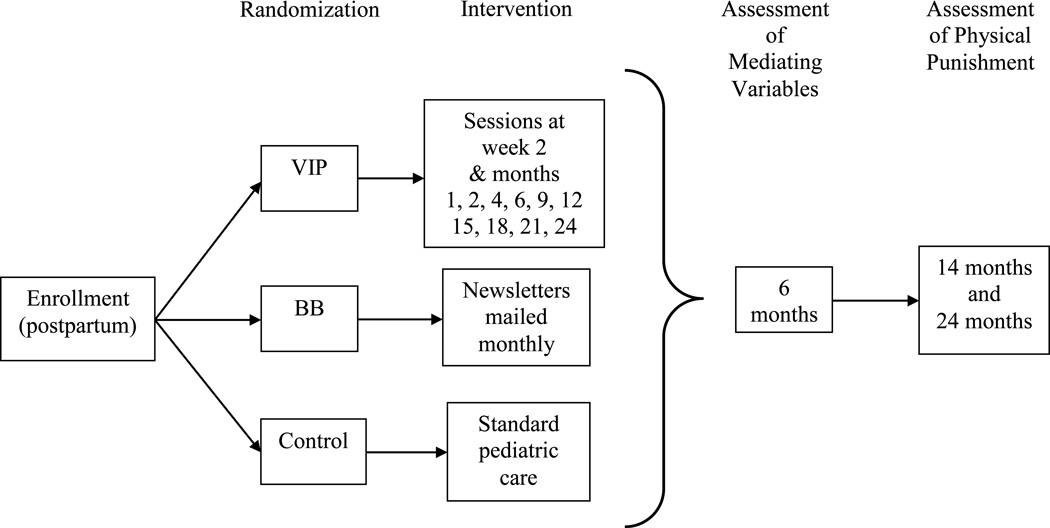
A 3-way randomized controlled trial—the Bellevue Project for Early Language, Literacy and Education Success (BELLE)—was conducted at an urban public hospital serving low-income families. This RCT was single-blind, in that researchers conducting the assessments were blinded to the family's randomization group and did not have access to the database where that information was stored. Mother-child dyads were enrolled consecutively in the postpartum unit, and all patients had the opportunity to take part in the project. Six hundred seventy-five participants were randomized to the VIP intervention, the BB intervention, or a control group. All three groups received Reach Out and Read (ROR) as part of standard pediatric care. Approval was obtained from both the New York University School of Medicine Institutional Review Board and the Bellevue Hospital Center Research Review Committee. The trial was registered with clinicaltrials.gov (NCT00212576).
Randomization Groups
Video Interaction Project
VIP was developed as an enhancement to ROR, which promotes parent-child reading aloud and has had population-level U.S. dissemination.18 In VIP, 11 sessions take place from birth to 2 years, on the same day as scheduled well-child primary care visits. Although VIP is intended to take place before families see their pediatrician, administration is flexible and often takes place following the visit. Sessions employ an interventionist who typically has a Bachelor's degree and experience working with children; VIP training includes both discussing cases and videos as well as ongoing periodic supervision. The interventionist is conceptualized as a member of the healthcare team, but interactions with providers take place primarily by encouraging parents to share information from VIP with their providers. Interventionists also refer parents for additional services if issues arise, and are trained in and follow standard hospital protocols regarding concerns about domestic violence and neglect.
The interventionist meets with families one-on-one for 25–30 minutes and video-records dyads during 5–7 minute episodes that include either play or shared reading. These episodes utilize a developmentally-appropriate toy and/or book that is provided by the program for the parent to take home. The video is reviewed together with the parent to identify and reinforce responsive interactions and thereby promote parent self-reflection. To promote generalization of responsive parenting behaviors in the home, the video is given to the parent with the suggestion to watch at home and/or share with other family members. Messages are further emphasized through the use of pamphlets that are personalized with the mother's observations about the child and goals for interacting with the child. The pamphlets also provide suggestions related to responsive parenting during play, reading and daily routines.17 These pamphlets include limited information about discipline, and do not have a specific focus on physical punishment.
Although providers were not given any specific training in VIP, they did periodically receive information about the role of the interventionist and the goals of VIP. Providers were asked to reinforce the messages put forth in the intervention, but were given no specific talking points (other than the pamphlets, when shared by the parent).
Building Blocks
BB utilizes mailed information and learning materials in order to improve parent self-efficacy and promote responsive parenting. Each month from birth to 36 months (36 total mailings), parents are mailed an age-specific parenting newsletter that provides suggestions for parent-child interaction around an age-appropriate developmental activity (an accompanying toy or book is also mailed) as well as information on developmental milestones, safety, feeding, and general parenting. Guidance on positive discipline is included approximately every 3–6 months (BB issues at 6, 9, 11, 14, 16, 19, 24, 30, and 32 months). In addition, parents are asked to fill out Ages and Stages developmental questionnaires every four to six months to promote active observation of their child’s development.19 Although BB provides information about discipline in general, like VIP it does not specifically target physical punishment.
Control
Control families received standard pediatric care, including all anticipatory guidance and observation of developmental milestones. Standard pediatric care included ROR for all groups.
Participants
Enrollment took place between November 2005 and October 2008. Consecutive mother-infant dyads who met inclusion criteria and provided informed consent were enrolled in the postpartum unit of Bellevue Hospital Center. Inclusion criteria were plans to receive pediatric care at Bellevue, full-term birth, no significant medical complications or eligibility for Early Intervention at birth as specified by criteria issued by New York State (e.g., Down Syndrome), and a mother who was the primary caregiver, who was over 18 years of age, and who spoke primarily English or Spanish. Mothers also needed to be able to maintain contact with the program (i.e., have a working telephone) in order to schedule assessments and VIP sessions.
Measures
Demographic Characteristics
Information on demographic characteristics was collected during the postpartum period and when infants were 6 months of age through maternal interviews. This included data on maternal age, ethnicity, education, literacy, country of origin, marital status, and primary language. Mothers were also asked to verify their infant's sex and birth order. Socioeconomic status (SES) was calculated based on parental education and employment, using the Hollingshead Four Factor Index.20
Dependent variable
Physical Punishment
Use of physical punishment was assessed at 14 and 24 months using the Socolar Discipline Survey,21 which asks parents about discipline they used during the previous 3 months. The survey has demonstrated adequate internal consistency, with alphas for subscales ranging from .56 to .82.21 Further, rates of physical punishment obtained in developing the measure were similar to those seen in national surveys of parent behavior. For the current study, physical punishment scores were created based on a previously identified corporal punishment factor in the Socolar Survey, which includes two questions regarding the frequency of spanking and of slapping the child’s hand.21 Answers ranged from 1 (never) to 6 (always), providing physical punishment scores from 2 to 12, with 2 representing no physical punishment.
Mediating variables
Maternal Psychosocial Risk
Two aspects of maternal psychosocial risk were assessed when infants were 6 months: maternal depressive symptoms and parenting stress.
Maternal Depressive Symptoms
Maternal depressive symptoms were assessed using the Patient Health Questionnaire 9 (PHQ-9).22 This screening questionnaire has 9 items that gauge mood over the past two weeks, including questions such as “How often have you been bothered by little interest or pleasure in doing things?” or “Feeling down, depressed, or hopeless?” The PHQ-9 has been shown to have a sensitivity and specificity of 88% for major depressive disorder, and has demonstrated good reliability (Cronbach’s α = .89) and validity (correlation to SF-20 mental health scale = .73).22
Parenting Stress
The Dysfunctional Parent-Child Interaction subscale of the Parenting Stress Index-Short Form (PSI-SF) was used to assess parenting stress.23 This scale asks parents about their attitudes and behaviors when interacting with their child, and measures the extent to which parents perceive interactions with their child as rewarding and their child as meeting expectations. The PSI-SF has demonstrated excellent internal consistency (Cronbach’s α = .88–.95) and construct validity, with regression analyses indicating significant associations between the Dysfunctional Parent-Child Interaction scale and maternal self-reported psychological symptoms, as well as family income (R2 = .21).23 Further, this measure has been validated in both the general population and low-income samples.
Responsive Parenting
Responsive parenting, including behaviors that are important for development such as playing and reading with the child, were measured using the StimQ. StimQ is a structured interview that asks parents about their interactions with their child in relation to playing with toys, reading aloud, teaching and daily routines. The StimQ has been validated for use in low SES populations in both English and Spanish (med.nyu.edu/pediatrics/developmental/research/belle-project/stimq-cognitive-home-environment).24 It has demonstrated good internal consistency (Cronbach’s α = .88), test–retest reliability (ICC = 50.93), and criterion validity (correlation with HOME Inventory: r = .55).
Statistical Analysis
Statistical analyses were performed using SPSS 20 on intent-to-treat groups. First, ANOVA and Chi-Square tests were used to compare sociodemographic characteristics across the 3 randomization groups for families completing one or more assessments, and between those who completed at least one assessment and those who did not.
At each age, we used ANOVA, followed by Tukey post-hoc testing and calculations of Cohen’s d, to compare physical punishment scores between randomization groups for complete cases only. We used chi-Square analyses, with calculations of odds ratios to compare the proportion of parents in each group who used any physical punishment to those who did not. Next, we compared rates of physical punishment over time for all participants across groups, using linear multilevel modeling (MLM). Using the MIXED command and maximum likelihood estimation, an individual MLM was estimated. Standardized coefficients are reported in the current analyses to provide estimates of effect size.
To determine whether maternal psychosocial risk or responsive parenting behaviors mediated the relation between intervention group and reductions in physical punishment, we used bias-corrected bootstrap mediation analysis. This method employs bootstrap simulations calculated from random samples that are pulled from the original data to inform and correct the confidence intervals around the effects in a path analysis. In the current analyses, 5000 bootstrap samples were taken, and 95% CI were used. Bootstrap mediation is particularly suited to modest sample sizes (<500). Further, bias-correction adjusts for skew in the population, a problem common in human subjects research. First, a simple regression model was used to examine the direct effects of the primary predictor variable—participation in intervention—on physical punishment at 24 months. Then, the potential mediating variable(s) was added to the model in order to determine if there was a reduction in the direct effect of the predictor, as well as if there was a significant indirect effect of the predictor on the outcome through the mediating variable. For models assessing maternal psychosocial risk as a mediator of program impacts, we utilized a maternal psychosocial risk factor score derived from principal components analysis with Varimax (orthogonal) rotation, based on mothers’ depressive symptoms and parenting stress scores.
RESULTS
Four hundred thirty-eight families (64.9% of the initial sample) were assessed at one or both time points and were included in the current analyses. Demographic characteristics of the sample can be found in Table 1. The majority of the sample was Hispanic, born outside the U.S., and low-income. There were no significant differences in demographic characteristics between the randomization groups at enrollment or at follow-up. Follow-up included 71.6% of VIP participants and 72.9% of control participants. Due to financial constraints within the BELLE trial, follow-up in the BB group was lower, 50.2%. However, there were no demographic differences between families in any of the randomization groups who were lost to follow-up and those who continued in the study through 24 months.
Table 1.
Demographic Characteristics of Families Completing One or More Follow-Up Assessments (Analytic Sample).
| Baseline | 24M Follow-up | |||||||
|---|---|---|---|---|---|---|---|---|
| VIP (N = 161) |
BB (N = 113) |
C (N = 164) |
p† | VIP (N = 152) |
BB (N = 62) |
C (N = 144) |
p† | |
| Mother <Age 21 | 9% | 12% | 9% | .57 | 9% | 10% | 8% | .94 |
| Married/partner | 86% | 88% | 85% | .87 | 87% | 89% | 85% | .81 |
| Hispanic | 94% | 95% | 92% | .43 | 93% | 95% | 92% | .76 |
| Spanish speaking | 87% | 81% | 84% | .33 | 88% | 79% | 84% | .20 |
| Born outside US | 93% | 88% | 88% | .20 | 95% | 92% | 89% | .18 |
| Non High School Grad | 63% | 55% | 62% | .19 | 64% | 65% | 64% | .34 |
| Low SES | 92% | 91% | 93% | .92 | 91% | 92% | 94% | .63 |
| Male child | 45% | 52% | 46% | .26 | 45% | 53% | 54% | .33 |
| First born child | 42% | 37% | 37% | .61 | 42% | 34% | 36% | .42 |
p-value based on Chi-Square tests.
Overall, 67.0% of parents used physical punishment when their children were 14 months, and 79.9% did so at 24 months. At 14 months, fewer parents in VIP (61.7%) had used any physical punishment in the previous 3 months as compared to Control (70.0%) and BB (69.2%); however, these differences were not significant. One-way ANOVA indicated that mean differences in physical punishment scores between groups, found in Table 2, were also not significant at 14 months (F(2, 284) = 1.96, p = .14). At 24 months, however, these differences were significant; fewer parents in VIP used any physical punishment (75.0%) as compared to Control (84.7%) and BB (80.6%). This represented a significantly reduced odds of using any physical punishment in the VIP group of .59 (95% CI: .35, .99) as compared to the other randomization groups. Further, differences between groups in physical punishment scores were significant at this age (F(2, 357) = 3.86, p < .05, d = .29). Tukey post-hoc analyses indicated that parents in the Control group had significantly higher physical punishment scores (M = 4.11, SD = 1.47) than parents in VIP (M = 3.67, SD = 1.48), but were not significantly different from parents in BB (M = 4.18, SD = 1.89). The difference in physical punishment scores between parents in the BB group and parents in VIP approached significance (p = .08).
Table 2.
Mean Corporal Punishment Scores at 14 and 24 months, across Randomization Groups.
| 14 months | 24 months | |||||
|---|---|---|---|---|---|---|
| N | M (SD) | Range† | N | M (SD) | Range† | |
| VIP | 94 | 3.22 (1.30) | 2 – 8 | 152 | 3.67 (1.48) | 2 – 8 |
| BB | 91 | 3.63 (1.64) | 2 – 11 | 62 | 4.18 (1.89) | 2 – 12 |
| Control | 100 | 3.55 (1.49) | 2 – 8 | 144 | 4.11 (1.47) | 2 – 9 |
Possible range: 2–12
To examine changes in parents’ use of physical punishment, we calculated a growth curve model examining the effects of VIP and BB on physical punishment over time. This indicated that physical punishment increased with age, β = .16, SE = .03, p < .001, meaning that overall physical punishment scores increased by approximately 1/2 of a point from age 14 months to age 24 months. However, there was a linear effect of VIP, such that, across this period, VIP parents reported less frequent use of physical punishment when compared to scores of parents in the BB and Control group, β = −.12, SE = .04, p < .05. There was no significant effect of participation in BB (Figure 1), and no interaction between randomization group and age.
Figure 1.
Timing of BELLE Project interventions and assessments.
Principal components analysis yielded a single factor including both maternal depressive symptoms and parenting stress, which accounted for 62.6% of the variance in these scores. Thus, this component score was examined as a potential mediator, along with responsive parenting, between VIP participation and rates of physical punishment. Given that BB was not a significant predictor of change in physical punishment over time, and that there were no significant differences between BB and Control groups in the overall analyses, these mediation analyses examined the effect of VIP in comparison to all other groups. These models demonstrated that the lower physical punishment scores seen among VIP families were mediated through increases in responsive parenting and decreases in maternal depression. As can be seen in Table 3, and consistent with Baron & Kenny25 criteria for partial mediation, the direct effect of VIP on lower physical punishment scores at 24 months, while remaining significant, decreased when responsive parenting and maternal psychosocial risk were added to the model. Responsive parenting and maternal psychosocial risk also exhibited significant direct effects on use of physical punishment, such that increases in responsive parenting were associated with decreases in physical punishment, while the opposite was true of increases in maternal psychosocial risk. Further, there were significant indirect effects of these parent behavior and risk variables, indicating that a key pathway by which VIP influenced parents’ use of physical punishment was through its effect on these variables. Further analysis of dose effects revealed significant correlations between the number of VIP sessions completed (median = 7) and maternal psychosocial risk (r = −.26), responsive parenting (r = .24), and physical punishment at 24 months (r = −.16). Combined, these analyses indicate that VIP contributed to gains in responsive parenting and decreases in maternal psychosocial risk—especially as parents attended more sessions—and in this way led to decreased use of physical punishment.
Table 3.
The effect of VIP intervention on rates of corporal punishment at 24 months, mediated by increased responsive parenting and maternal psychosocial risk.
| Bias-Corrected 95% CI | ||||
|---|---|---|---|---|
| Point Estimate |
SE | Lower | Upper | |
| Simple Regression Model | ||||
| VIP group | −.70 | .20 | −1.08 | −.31 |
| Mediation Model | ||||
| Direct Effects | ||||
| VIP group | −.51 | .20 | −.90 | −.11 |
| Responsive parenting | −.03 | .01 | −.06 | −.01 |
| Maternal psychosocial risk | .27 | .09 | .07 | .45 |
| Indirect Effects of VIP through | ||||
| Responsive parenting | −.09 | .05 | −.22 | −.02 |
| Maternal psychosocial risk | −.10 | .06 | −.27 | −.02 |
DISCUSSION
In this study, we documented that pediatric primary care-based preventive interventions are associated with reduced physical punishment, demonstrating the potential for such programs to effect population-wide changes. More specifically, and consistent with hypothesis one, these results highlight the efficacy of the VIP parenting intervention, as opposed to BB or standard care, in reducing physical punishment among low-income families. Further, because ROR was provided to families in all groups, this difference clearly resulted from the added value of VIP. Despite this overall effect of VIP, we did not find a difference between randomization groups in the rate of growth of physical punishment from 14 to 24 months, which was inconsistent with hypothesis two. Instead, our results indicate that the effect of VIP may emerge at 24 months, when, as expected, rates of physical punishment were higher. Thus, participation in this intervention may allow parents to consider alternative discipline methods as non-compliant behavior becomes more frequent during the toddler period. Finally, we found that VIP reduced physical punishment at 24 months through improvements in responsive parenting and through decreases in maternal psychosocial risk, supporting hypothesis three—pediatric primary care interventions would lead to differences in physical punishment through direct effects on mediating parent factors.
These results are especially important given the immediate and long-term consequences of physical punishment. For instance, physical punishment has been associated with adverse effects on IQ and cognitive development.26 More commonly, associations have been found between physical punishment and psychosocial issues. Toddlers who have experienced physical punishment display more internalizing and externalizing problems, and such externalizing problems continue at least through early elementary school. Multiple studies have also found links between physical punishment and conduct and other mental health problems throughout childhood.4,27,28
Consequences of physical punishment often extend beyond the childhood period. In fact, adolescents and adults physically punished as children have a more negative self-concept and have higher rates of depression.8 Further, the externalizing symptoms and conduct problems seen in childhood are expressed as increased aggression and increased incidence of spousal and child abuse.4,27
Previous research has also indicated that physical punishment is more likely among parents living in poverty, and who experience violence in their neighborhoods.3 This is especially true for mothers who have low levels of education, low levels of social support, or are depressed.2,3 The reduced use of physical punishment among VIP parents, and the mediating role of maternal psychosocial risk, is, thus, important, as it indicates that VIP may help address those factors that make physical punishment more frequent in this population. In addition, although we expected an increase in physical punishment from 14 to 24 months, given its peak in the toddler period, we were encouraged to see that rates were significantly lower among families participating in VIP at 24 months. Overall, our results indicate that pediatric primary care interventions—even those that are lower-intensity and lower-cost than successful interventions like Healthy Steps—have the potential to decrease rates of physical punishment among low-income families.
The finding that, despite the recurrent discipline content included in the BB newsletters, the VIP intervention had significantly increased efficacy may be explained by three components on which VIP is built. First, the self-reflection central to the intervention empowers parents to engage in positive parenting practices. Second, the relationship built between the parent and the interventionist allows the parent to feel supported in their parenting efforts. And third, engaging in positive parenting can, in itself, reduce depressive symptoms and parents' perceptions of stress, as has been shown in previous work.14 Thus, VIP's effect on the mediating variables seen in this study—maternal psychosocial risk and responsive parenting—is a key aspect of the impact of VIP on physical punishment. In this case, the stronger relationship established between the VIP interventionist and the parent may prove more influential than the specific discipline messages delivered in BB’s “low key” mailed newsletters. This provides a starting point for future research and the development of interventions specifically targeted at reductions in physical punishment. Although the frequency of reported physical punishment was relatively low in the current study, it was similar to frequencies found in previous research. For instance, a large-scale study of parenting found that, on average, parents in the U.S. reported spanking, slapping, or hitting their child less than once a month,29 which corresponds to physical punishment scores in this study. Further, the number of parents who reported using any such discipline was similar to the national average of approximately 67%. This further highlights the need for research in developing interventions that will bring this number closer to zero.
Information and guidance that reinforces positive parenting behaviors and support that helps to reduce maternal depression and stress may be effective methods for changing parent behavior or increasing responsive behaviors already present. This may be especially effective if it starts early, as early depressive symptoms may initiate a pattern of maternal psychosocial risk. In fact, in our sample, depressive symptoms at 6 months were associated with both depressive symptoms and parenting stress at 14 months (data not shown). Reducing these risks may lead to increased positive parenting, which in turn, may affect child behavior, making physical punishment seem unnecessary. Further, it may also provide the parent with alternative strategies and increase their feelings of control when administering discipline, making their responses to misbehavior more constructive. In fact, interventions such as the Chicago Parent Program, which includes topics such as child-centered time, the importance of family routines, and stress management, in addition to specific information about discipline strategies, have demonstrated efficacy in reducing reliance on physical punishment among urban, low-income families.11 Further research specifically examining the link between parenting, maternal psychosocial risk, and physical punishment is needed to fully address these issues.
This study has some limitations that should be considered in the interpretation of these findings. First, these results were found in a sample of low-income, immigrant, Latino families, and therefore may not generalize to other populations with different cultural perspectives on child-rearing. Second, a loss of funding for BB follow-up prevented the planned long-term follow-up of this group. Notably, though, results comparing VIP to only the Control group (data not shown) were similar to those reported here and there were no differences in demographic characteristics between those BB participants who received no follow-up and those who continued through 14 and 24 months. The smaller sample of BB participants does, however, limit our ability to make inferences about the efficacy of BB. In addition, data on the use of physical punishment was collected during a specific period, and may not reflect current trends in parental discipline.
As with all longitudinal research, participant retention potentially limits this study. However, as noted previously, there were no demographic differences between those families lost to follow-up and those who were included in the present analyses. Further, participant retention was comparable to that of similar studies. For example, in a study examining parent interventions in a sample of low-income mothers, Katz and colleagues noted an attrition rate of 41% by 12 months.30 This indicates that, although retention is a continuing issue for long-term preventive interventions, the results of the current study are likely valid. Finally, measures of responsive parenting and physical punishment were obtained through parent-report, which may be subject to social desirability bias, given the controversial nature of parental discipline. However both instruments are valid and reliable, and rates of physical punishment—which could be especially prone to social desirability bias—align with statistics of physical punishment use in the U.S., further supporting the validity of the measure. Nevertheless, future studies incorporating direct, natural observation of parent and child interactions (i.e., in the home) are critical in providing a deeper understanding of how parent characteristics relate to the use of physical punishment.
CONCLUSIONS
The current findings provide support for the efficacy of pediatric primary care interventions aimed at improving parent-child relationships, and specifically for the VIP intervention, in reducing the use of physical punishment among low-income families. Because of the physical and emotional consequences of physical punishment, this issue is one of large clinical significance. This study provides evidence of the potential for impacts of VIP in improving child development outcomes through improvements in parent-child relationships, and indicates that such an intervention may have broad impacts on children’s health and well-being. Taken together, these results along with previous findings on maternal depression, parenting stress, and children’s cognitive development, strongly suggest the potential of VIP to reduce toxic stress in parent-child relationships in low-income families.
Figure 2.
Physical punishment used among parents in the three randomization groups.
Acknowledgments
This research was supported by NIH grants to Alan Mendelsohn (PI): 5R01 HD047740 01-04; 2R01 HD047740 05-08; 3R01 HD047740-08S1. Additional funding was provided by the Tiger Foundation, Marks Family Foundation, Rhodebeck Charitable Trust, New York Community Trust, Children of Bellevue, Inc., KiDS of NYU Foundation, Inc. and the NY City Council.
REFERENCES
- 1.Harris Interactive, The Harris Poll #67. [Polled August 14–19, 2013]; http://www.harrisinteractive.com/newsroom/harrispolls/tabid/447/ctl/readcustom%20default/mid/1508/articleid/1283/default.aspx. [Google Scholar]
- 2.Day RD, Peterson GW, McCracken C. Predicting spanking of younger and older children by mothers and fathers. Journal of Marriage and the Family. 1998;60:79–94. [Google Scholar]
- 3.Straus MA. Prevalence, societal causes, and trends in corporal punishment by parents in world perspective. Law and Contemporary Problems. 2010;73:1–30. [Google Scholar]
- 4.Gershoff ET. Corporal punishment by parents and associated child behaviors and experiences: A meta-analytic and theoretical review. Psychological Bulletin. 2002;128:539–579. doi: 10.1037/0033-2909.128.4.539. [DOI] [PubMed] [Google Scholar]
- 5.Straus MA, Mathur AK. Social change and change in approval of corporal punishment by parents from 1968 to 1994. In: Frehsee D, Horn W, Bussmann KD, editors. Family violence against children: A challenge for society. New York: Walter deGruyter; 1996. pp. 91–105. [Google Scholar]
- 6.MacKenzie M, Nicklas E, Waldfogel J, Brooks-Gunn J. Spanking and child development across the first decade of life. Pediatrics. 2013;132:e1118–e1125. doi: 10.1542/peds.2013-1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Committee on Psychosocial Aspects of Child & Family Health. Policy statement: Guidance for effective discipline. Pediatrics. 1998;101:723–728. Reaffirmed April 2014. [PubMed] [Google Scholar]
- 8.Olds DL. Preventing child maltreatment and crime with prenatal and infancy support of parents: The Nurse-Family Partnership. Journal of Scandinavian Studies in Criminology and Crime Prevention. 2008;9:2–24. doi: 10.1080/14043850802450096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gardner F, Shaw DS, Dishion TJ, Burton J, Supplee L. Randomized prevention trial for early conduct problems: Effects on proactive parenting and links to toddler disruptive behavior. Journal of Family Psychology. 2007;21:398–406. doi: 10.1037/0893-3200.21.3.398. [DOI] [PubMed] [Google Scholar]
- 10.De Graaf I, Speetjens P, Smit F, deWolff M, Tavecchio L. Effectiveness of the Triple P Positive Parenting Program on parenting: A meta-analysis. Family Relations. 2008;57:553–566. doi: 10.1177/0145445508317134. [DOI] [PubMed] [Google Scholar]
- 11.Gross D, Garvey C, Julion W, Fogg L, Tucker S, Mokros H. Efficacy of the Chicago Parent Program with low-income african american and latino parents of young children. Prevention Science. 2009;10:54–65. doi: 10.1007/s11121-008-0116-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Orrell-Valente JK, Pinderhughes EE, Valente E, Laird RD Conduct Problems Prevention Research Group. If it’s offered, will they come? Influences on parents’ participation in a community-based conduct problems prevention program. Am J Community Psychol. 1999;27:753–783. doi: 10.1023/a:1022258525075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caughy MO, Miller TL, Genevo JL, Huang KY, Nautiyal C. The effects of Healthy Steps on discipline strategies of parents of young children. Applied Developmental Psychology. 2003;24:517–534. [Google Scholar]
- 14.Berkule SB, Cates CB, Dreyer BP, et al. Reducing maternal depressive symptoms through promotion of parenting in pediatric primary care. Clinical Pediatrics. 2014;53:460–469. doi: 10.1177/0009922814528033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cates CB, Weisleder A, Dreyer BP, et al. Leveraging health care to promote responsive parenting and school readiness in low-income families: Impact of the Video Interaction Project on parenting stress. 2015 doi: 10.1007/s10826-015-0267-7. Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dietz TL. Disciplining children: Characteristics associated with the use of corporal punishment. Child Abuse & Neglect. 2000;24:1529–1542. doi: 10.1016/s0145-2134(00)00213-1. [DOI] [PubMed] [Google Scholar]
- 17.Mendelsohn AL, Huberman HS, Berkule SB, Brockmeyer CA, Morrow LM, Dreyer BP. Primary care strategies for promoting parent-child interaction and school readiness in at-risk families: The Bellevue Project for Early Language, Literacy, and Education Success. Archives of Pediatric & Adolescent Medicine. 2011;165:33–41. doi: 10.1001/archpediatrics.2010.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zuckerman B. Promoting early literacy in pediatric practice: Twenty years of Reach Out and Read. Pediatrics. 2009;124:1660–1665. doi: 10.1542/peds.2009-1207. [DOI] [PubMed] [Google Scholar]
- 19.Bricker DD, Squires J, Mounts L. Ages & Stages Questionnaires: A parent-completed, child-monitoring system. Baltimore, MD: Paul H. Brookes; 1999. [Google Scholar]
- 20.Hollingshead AB. Four factor index of social status. New Haven, CT: Yale University; 1975. [Google Scholar]
- 21.Socolar R, Savage E, Devellis RF, Evans H. The discipline survey: A new measure of parental discipline. Amb Peds. 2004;4:166–173. doi: 10.1367/A03-071R1.1. [DOI] [PubMed] [Google Scholar]
- 22.Kroenke K, Spitzer RL, Williams JB. The PHQ-9. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reitman D, Currier RO, Stickle TR. A critical evaluation of the Parenting Stress Index-Short Form (PSI-SF) in a head start population. Journal of Clinical Child and Adolescent Psychology. 2002;31:384–392. doi: 10.1207/S15374424JCCP3103_10. [DOI] [PubMed] [Google Scholar]
- 24.Dreyer BP, Mendelsohn AL, Tamis-LeMonda CS. Assessing the child’s cognitive home environment through parental report: Reliability and validity. Early Development and Parenting. 1996;5:271–287. [Google Scholar]
- 25.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 26.Smith JR, Brooks-Gunn J. Correlates and consequences of harsh discipline for young children. Arch Pediatr Adolesc Med. 1997;151:777–786. doi: 10.1001/archpedi.1997.02170450027004. [DOI] [PubMed] [Google Scholar]
- 27.McCord J. Unintended consequences of punishment. Pediatrics. 1996;98:832–834. [PubMed] [Google Scholar]
- 28.Straus MA, Sugarman DB, Giles-Sims J. Spanking by parents and subsequent antisocial behavior of children. Archives of Pediatrics and Adolescent Medicine. 1997;151:761–767. doi: 10.1001/archpedi.1997.02170450011002. [DOI] [PubMed] [Google Scholar]
- 29.Lansford J, Alampay L, Al-Hassan S, et al. Corporal punishment of children in nine countries as a function of child gender and parent gender. International Journal of Pediatrics. 2010;2010:1–12. doi: 10.1155/2010/672780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Katz K, El-Mohandes A, McNeely Johnson D, et al. Retention of low income mothers in a parenting intervention study. Journal of Community Health. 2001;26:203–218. doi: 10.1023/a:1010373113060. [DOI] [PubMed] [Google Scholar]