Abstract
Background
In the United States (U.S.), Latinos often report fair/poor self-rated health, which is an indicator for increased morbidity and mortality. Foreign-born Latinos in new immigrant destinations, such as the South, may rate their health more poorly than their counterparts elsewhere in the U.S., due to factors associated with migration and settlement in these communities.
Methods
We assessed foreign-born Latinas’ self-rated health in Birmingham, Alabama (n=765), and compared it to that of foreign-born Latinas in the National Health Interview Survey (NHIS; n=8,746). Birmingham participants were matched to Latinas in the NHIS using propensity scores. We examined factors associated with reporting worse health using ordered logistic regression and inverse probability of treatment weights.
Results
After propensity score matching, 47.6% of foreign-born Latinas in the Birmingham study reported their health as fair/poor, compared to 17.9% of foreign-born Latinas in the NHIS (p<0.001). The association between being Mexican-born versus from other countries with poorer health was stronger in the Birmingham study (odds ratio: 4.46 [95% CI: 1.91–10.4]) than in the NHIS (odds ratio 1.09 [95%CI: 1.08–1.09]). Shorter durations of U.S. residence were associated with better health for Latinas in the NHIS but not those in Birmingham.
Conclusions
In this study of Latina immigrants in a new settlement community in the South, women reported worse health than foreign-born Latinas in other U.S. regions, suggesting they may be at increased risk for adverse health outcomes. Future studies are needed to better understand the factors associated with these differences to reduce morbidity and mortality burdens.
Keywords: Self-rated health, Hispanics, Immigrants, U.S. South
Introduction
Self-rated health is a well-established predictor of morbidity and mortality.1–3 In the United States (U.S.), Latinos often rate their health as poorer than non-Hispanic whites.4–7 Several studies have demonstrated that Latinos who rate their health as fair or poor report more days in bed, greater activity limitations, increased hospitalizations and a higher prevalence of chronic health conditions.4,5,7–9 Poorer self-rated health also is associated with increased risk of death.10
Much of what is known about self-rated health among Latinos in the U.S. has been derived from nationally representative surveys. However, these data sources may not capture changes in the distribution and composition of the foreign-born Latino population. Since the 1980’s, foreign-born Latinos have increasingly moved away from traditional receiving states like California, Texas, and New York, and settled in states in the U.S. South, which have reported the most rapid rates of increase in their Latino populations compared to other areas of the U.S.11,12 Due to the foreign-born population’s rapid growth in Southern states, as well as the large unauthorized population in this area, Latino immigrants are likely underrepresented in large U.S. surveys that rely on population estimates to form their sampling frames.13 Additionally, despite its rapid growth, the Latino population in Southern states is still relatively small compared to other racial/ethnic groups,14 and therefore data obtained through national samples may not include many Latino immigrants in these areas.
Foreign-born Latinos in Southern states represent a select sub-group of immigrants and, thus, may rate their health more poorly than those elsewhere in the U.S. For example, Latino immigrants in the South are more likely to originate from Mexico or Central America and have lower levels of education, characteristics typically associated with poorer health.7,12,15 However, Southern Latinos also tend to be younger and have shorter durations of residence, which would indicate a positive health profile.5,7,12,15 Yet, compared to Latinos elsewhere with these same characteristics, they may report poorer health because they are less likely to seek care when they need it. In communities without a long-standing history of migration, recently arrived immigrants with limited English language proficiency may face difficulties identifying health services and challenges seeking care from institutions that lack interpreters and little experience providing services to foreign-born groups.16–19 Therefore, assumptions about the health profile and potential health needs that are based on national data may be inaccurate for foreign-born Latinos in Southern destinations.
The purpose of this analysis is to examine the health status of Latina immigrants in a new Southern destination. Specifically, we assess self-rated health and factors associated with reporting worse health in a sample of foreign-born Latina women in Birmingham, Alabama. Between 2000 and 2010, Alabama recorded the second largest percent growth in its Latino population among all U.S. states, and the largest settlement of Latino immigrants is in Jefferson County – home of the city of Birmingham.14,20 We focus this analysis on Latina immigrants as previous research has found that Latina women are more likely to report poorer health and more health problems early in their adult years than Latino men, which may be due to reproductive health concerns and acculturative stressors associated with migrating into male-dominated migrant networks.21–23 Our study also examines how self-rated health and factors associated with worse health in this sample compares to that of foreign-born Latinas in the U.S. Identifying factors that are related to poorer health among Latina immigrants in the South can be used to inform the development and implementation of culturally relevant programs and policies to reduce their risk of adverse health outcomes.
Methods
Data
For this analysis, we use data from a community-based participatory research initiative to increase breast and cervical cancer awareness and screening among Latina immigrants in the Birmingham metropolitan area. Between 2004 and 2009, lay health workers promoted the annual outreach events through their social networks in the Latino community and distributed flyers; announcements also were made on Spanish-language radio and newspapers and in area churches serving the Latino population.24 The events were open to women ages 19 and older, and hosted in two separate venues each spring. All women attending the event provided signed informed consent and completed self-administered Spanish-language questionnaires that collected information on their demographic characteristics and health care utilization. This study was approved by the Institutional Review Board at the authors’ institution.
During the 2004 and 2009 study period, 840 foreign-born Latinas completed the survey, with annual attendance ranging from 47 to 209 women per year. If a woman attended the event more than year, only data from the first event attended were included in this analysis. We also excluded women with missing information on sociodemographic characteristics or self-rated health (n=75), resulting in a sample of 765 foreign-born Latinas.
For our comparison sample of foreign-born Latina immigrants, we use data from the National Health Interview Survey (NHIS), which has been a key data source for assessments of Latino health in the U.S.5,7,10,25 The NHIS is an annual cross-sectional survey of a nationally-representative sample of U.S. households drawn from a multi-stage probability sample based on U.S. Census estimates. It consists of a face-to-face interview conducted in English or Spanish with a selected member of each household who is 18 years of age or older and collects information on sociodemographic characteristics and self-rated health. For this analysis we pooled data from 2004 to 2009 to provide an adequate sample size of foreign-born Latinas and to construct a comparable time frame to the Birmingham study. We restricted the NHIS analysis to women age 19 and older who reported Hispanic ethnicity and were born outside the U.S. (n=9,079) and excluded respondents with missing data on sociodemographic characteristics and self-rated health (n=333). The NHIS analytic sample included 8,746 foreign-born Latinas.
Measures
Our dependent variable was women’s assessment of their overall health (i.e. self-rated health). In both the Birmingham sample and NHIS, self-rated health was assessed using the question: “Would you say that your health in general is excellent, very good, good, fair or poor?” We coded self-rated health as: excellent/very good, good, and fair/poor. We used this categorization to address the small cell sizes in the “poor” and “excellent” responses in the Birmingham study while maintaining the ordinal structure of the variable to permit variation in the distribution of responses.
Our independent variables were women’s age, country of origin, duration of residence in the U.S., highest level of education, marital status, employment status, and whether she had health insurance and a regular source of health care, which we expected to differ between the two samples and which other studies have found to be associated with self-rated health among Latinos.7,15,25 To make the 2 data sets comparable, we recoded some variables. For example, the NHIS has detailed information on respondents’ type of health insurance, but the Birmingham study only asked whether or not women had health insurance. Therefore, our measure treats NHIS respondents as having any form of health insurance (e.g., public or private) or having no insurance. Additionally, the NHIS collected information on both respondent’s employment and occupational status, while only employment status was available in the Birmingham survey, providing a more limited measure of women’s economic activities. Finally, because Alabama’s Latino immigrant population is predominately from Mexico, we are unable to construct statistically meaningful categories of other Latino sub-groups (e.g. Puerto Rican) in the Birmingham study to compare with the NHIS.
Statistical Analyses
We first computed distributions for the sociodemographic characteristics and self-rated health for women in the Birmingham study and NHIS. Analyses of the NHIS were weighted to account for the complex sampling design of the survey and the pooling of data across years.26
As noted above, we expected that Latina immigrants in the Birmingham study might have a different sociodemographic profile compared to foreign-born Latinas in the NHIS, possibly due to selective migration. These differences are problematic if they are also related to women’s health status. To address this issue, we used a propensity score as a ‘balancing score,’ or summary of the covariates, to make the samples comparable. To calculate the propensity score, we pooled the 2 data sources and estimated a probit regression model where the dependent variable was being a Latina immigrant in the Birmingham study and age, country of origin, duration of U.S. residence, education, marital status, employment, health insurance and regular source of health care were independent variables. We also included age2, age3, interactions between country of origin and each of the independent variables, as well as interaction terms for age*education, age*martial status, age*insurance, duration of residence*age, duration of residence*martial status, and duration of residence*regular source of care. We selected these terms because we expected they were associated with being in the Birmingham sample, and linked to our dependent variable - self-rated health, and including them improved the comparability of the two samples27 The propensity score is the predicted probability from this model. At the upper range of the distribution of the propensity score, there was limited overlap between the 2 samples. Therefore, to increase the precision of our estimates, we excluded women with propensity scores ≥ 0.550 from subsequent analyses (NHIS: n=46 (0.5% of the sample); Birmingham: n= 94 (12.0% of the sample)).
Next, we used the propensity scores to create inverse probability of treatment weights (IPTW), where the weight for each observation is the inverse probability of being in the Birmingham sample. Women with low probabilities are given larger weights, thereby increasing their relative contribution to calculations. This creates a pseudo-population in which the distribution of characteristics is similar for the 2 samples. To further improve the precision of our estimates, we also trimmed the IPTWs at 1st and 99th percentiles, but this did not affect the overall balance of characteristics.
Then, using the IPTWs as analytic weights and the restricted sample (9,371 women with propensity scores < 0.550), we computed the distribution of self-rated health to assess whether differences remained after accounting for compositional differences between groups. Finally, we examined factors associated with reporting worse health, by calculating multivariable-adjusted odds ratios, derived from survey-weighted ordered logistic regression models that were stratified by data source and used the IPTWs as sampling weights. In demographically similar samples, factors which are uniquely associated with worse health in one group would suggest that contextual influences, or the way in which they interact with immigrants’ characteristics, play an important role in shaping women’s health. We determined the statistical significance of differences in the distribution of sociodemographic characteristics in the restricted, weighted sample and in the odds ratios between the Birmingham and NHIS respondents using the estimated proportions (beta coefficients) and standard errors and a bootstrap procedure with 1,000 iterations.28
Because interview language was only available for the NHIS family respondent and not the sampled adult reporting self-rated health, we did not limit the NHIS sample to foreign-born Latinas who completed the interview in Spanish. However, since language may influence one’s understanding of the response options,21 we used the family interview language as a proxy to conduct a sensitivity analysis that restricted the NHIS foreign-born Latina sample to those living in households where the family respondent was interviewed in Spanish. All analyses were conducted using Stata 11.0 (StataCorp LP, College Station, TX).
Results
Women the Birmingham study were younger, more likely to be from Mexico, have shorter durations of U.S. residence and lower levels of education than foreign-born Latinas in the NHIS (Table 1, left column). Only 6.8% of women in the Birmingham study reported having health insurance compared with 56.2% of foreign-born Latinas in the NHIS. However, the percentage of women reporting a regular source of health care was similar for the 2 groups.
Table 1.
Characteristics of foreign-born Latina women in Birmingham, Alabama and the National Health Interview Survey (NHIS) before and after propensity score estimation
| Original samplea |
Restricted, weighted sampleb,c |
|||
|---|---|---|---|---|
| Birmingham (n=765) |
NHIS (n=8,746) |
Birmingham (n=671) |
NHIS (n=8,700) |
|
| (%) | (%) | (%) | (%) | |
| Age group, years | ||||
| 19 – 24 | 12.4 | 11.0 | 9.5 | 9.4 |
| 25 – 34 | 39.4 | 25.7 | 33.4 | 27.5 |
| 35 – 44 | 28.1 | 25.0 | 25.3 | 25.7 |
| ≥ 45 | 20.1 | 38.3 | 31.8 | 37.4 |
| Latino subgroup | ||||
| Mexican | 80.4 | 55.6 | 57.3 | 55.8 |
| Other Latino | 19.6 | 44.4 | 42.7 | 44.2 |
| Duration of residence in US, years | ||||
| < 5 | 47.7 | 11.2 | 12.6 | 12.3 |
| 5 – 9 | 32.8 | 19.3 | 19.1 | 19.2 |
| ≥ 10 | 19.5 | 69.4 | 68.3 | 68.4 |
| Marital status | ||||
| Single, never married | 11.1 | 12.8 | 13.8 | 15.0 |
| Married/ in union | 76.1 | 66.2 | 62.4 | 57.4 |
| Previously married | 12.8 | 21.0 | 23.8 | 27.6 |
| Educational attainment | ||||
| Less than high school | 65.2 | 51.6 | 56.4 | 54.3 |
| High school (or equivalent) | 17.0 | 22.5 | 21.5 | 21.5 |
| Some college/ college degree | 17.8 | 25.8 | 22.1 | 24.2 |
| Employed | 45.2 | 49.3 | 52.6 | 49.0 |
| Has health insurance | 6.8 | 56.2 | 51.0 | 55.0 |
| Has a regular source of health care | 76.6 | 79.8 | 79.1 | 79.5 |
Reported percentages for the National Health Interview Survey are weighted, reflecting the sampling design for the survey.
Samples restricted to women with propensity scores < 0.550
Reported percentages are weighted using the inverse probability of being in the Birmingham sample.
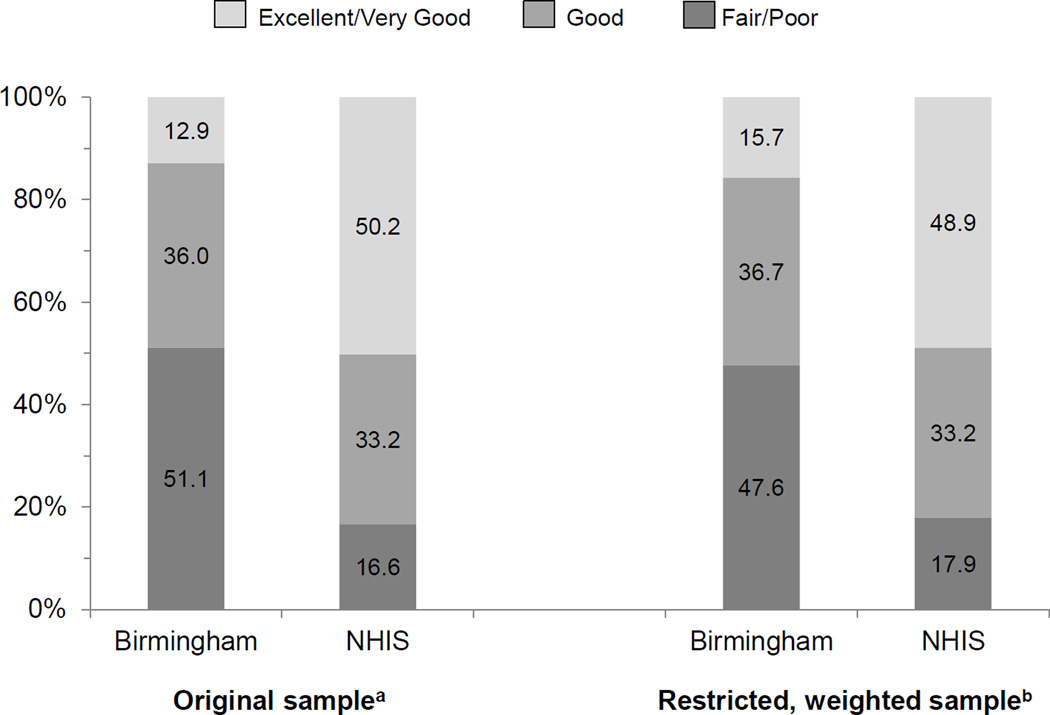
Overall, 51.1% of Latinas in the Birmingham study reported their health as fair or poor, compared to 16.6% of Latinas in the NHIS (Figure 1, left panel). Relatedly, Latinas in the NHIS were more likely to report very good/excellent health (50.2% compared to 12.9% of women in the Birmingham study).
Figure 1.
Distribution of self-rated health among foreign-born Latina women in Birmingham, Alabama and the National Health Interview Survey (NHIS) before and after propensity score estimation
a. Reported percentages for the NHIS are weighted, reflecting the sampling design for the survey.
b. Reported percentages are weighted using the inverse probability of being in the Birmingham sample. Samples restricted to women with propensity scores < 0.550.
In our propensity score-matched sample, no significant differences in sociodemographic characteristics were present between Latinas in the Birmingham study and Latinas NHIS (Table 1, right column). However, large differences were still present in the distribution of self-rated health (Figure 1, right panel). Also, women in Birmingham were more likely to report fair/poor health and less likely to report very good/excellent health compared to Latinas in NHIS.
Following multivariable adjustment, foreign-born Latinas in the NHIS who were age 35 to 44 and ≥ 45 years reported worse health compared to women who were 25 to 34 years old (Table 2). In contrast, older age was not associated with worse health for foreign-born Latinas in the Birmingham study. Odds ratios for worse self-rated health were higher for Mexican-origin women compared to other Latinas, and the effect was larger among women in Birmingham. Shorter durations of residence in the U.S. were associated with better health for women in the NHIS, but this relationship was not present among Latinas in the Birmingham study.
Table 2.
Multivariable adjusted odds ratios for worse self-rated health among foreign-born Latina women in Birmingham, Alabama and the National Health Interview Survey (NHIS)a
| Birmingham | NHIS | ||
|---|---|---|---|
| Odds Ratio (95% CI) |
Odds Ratio (95% CI) |
p-valueb | |
| Age group, years | |||
| 19 – 24 | 0.99 (0.37 – 2.63) | 0.98 (0.90 – 1.07) | 0.999 |
| 25 – 34 | 1.00 (ref) | 1.00 (ref) | |
| 35 – 44 | 1.11 (0.46 – 2.69) | 1.46 (1.27 – 1.67)* | 0.540 |
| ≥ 45 | 0.62 (0.24 – 1.61) | 2.98 (2.93 – 3.03)* | 0.001 |
| Latino subgroup | |||
| Mexican | 4.46 (1.91 –10.4)* | 1.09 (1.08 – 1.09) | 0.001 |
| Other Latino | 1.00 (ref) | 1.00 (ref) | |
| Duration of residence in US, years | |||
| < 5 | 1.05 (0.49 – 2.25) | 0.78 (0.73 – 0.83)* | 0.465 |
| 5 – 9 | 1.66 (0.76 – 3.65) | 0.85 (0.81 – 0.89)* | 0.094 |
| ≥ 10 | 1.00 (ref) | 1.00 (ref) | |
| Marital status | |||
| Single, never married | 0.38 (0.13 – 1.10) | 1.36 (1.28 – 1.43)* | 0.019 |
| Married/ in union | 1.00 (ref) | 1.00 (ref) | |
| Previously married | 6.32 (2.39 – 16.7)* | 1.37 (1.33 – 1.42)* | 0.002 |
| Educational attainment | |||
| Less than high school | 1.08 (0.49 – 2.37) | 1.53 (1.44 – 1.63)* | 0.394 |
| High school (or equivalent) | 1.00 (ref) | 1.00 (ref) | |
| Some college/ college degree | 0.10 (0.03 – 0.33)* | 0.76 (0.70 – 0.83)* | <0.001 |
| Employed (vs not employed) | 0.97 (0.46 – 2.06) | 0.54 (0.53 – 0.54)* | 0.129 |
| Has health insurance (vs no insurance) | 1.93 (0.88 – 4.24) | 1.07 (1.03 – 1.10)* | 0.130 |
| Has a regular source of health care (vs no regular source) | 0.53 (0.22 – 1.25) | 1.00 (0.93 – 1.08) | 0.147 |
Odds ratios from ordered logistic models with values above one representing worse self-rated health and values below one representing better self-rated health, relative to the reference category. All variables included in a single regression model.
Reported odds ratios and confidence intervals are weighted using the inverse probability of being in the Birmingham sample. Samples restricted to women with propensity scores < 0.550.
p-value comparing difference between the Birmingham sample and NHIS for each covariate category.
CI = Confidence interval
p<0.001 for within dataset differences in self-rated health
Although education beyond high school was associated with better health for both groups, the effect was larger for women in the Birmingham study. In addition, having less than a high school education was associated with worse health for women in the NHIS, but there was no association in the Birmingham study. The odds ratios of worse health were significantly lower for employed women compared to those who were unemployed in the NHIS, but no association between employment and self-rated health was evident in the Birmingham study. Finally, having health insurance was associated with worse self-rated health for Latinas in the NHIS and approached significance for women in the Birmingham study, but having a regular source of health care was not associated with self-rated health in the Birmingham study or NHIS.
Results from our sensitivity analysis limiting the NHIS sample to respondents in Spanish-speaking households were similar.
Discussion
Similar to other studies of Latino immigrants in new destination areas,17,29 we found a large percentage of foreign-born Latinas in Birmingham reported their health as fair or poor. This percentage was larger relative to foreign-born Latinas in the NHIS in our initial comparison, and, these differences in self-rated health remained even after employing propensity score methods to make the 2 samples of women more comparable. Additionally, characteristics, such as shorter duration of U.S. residence, were not associated with reporting better health among Latinas in the Birmingham study. Together these findings suggest that Latina immigrants in new Southern destinations may be at increased risk for adverse health outcomes compared to foreign-born Latinas elsewhere in the U.S.
The unadjusted differences we observed in self-rated health between foreign-born Latinas in the Birmingham study and NHIS could be due to the fact that the predominantly Mexican-origin migrants settling in metropolitan areas of Alabama are less healthy than Latino immigrants residing elsewhere in the U.S. Recent Mexican migrants’ reports of poorer health compared to other immigrant groups has been attributed to both the nature of Mexican migration, such as the predominance of Mexicans granted residency through family preference, as well as their socioeconomic profile.30 Indeed, the sociodemographic characteristics of women in the Birmingham study correspond to a profile of immigrants that are not selected on better health status. Additionally, the Latino population in the South includes many unauthorized immigrants,31 who may report poorer health because they are channeled into informal sectors of the economy where there are few - if any - health benefits, or because of increased fears of deportation, which may lead to chronic stress and exacerbate any current health problems.32 Yet, after we addressed the potential effect of selectively by using propensity scores, Latinas in the Birmingham study still had worse self-rated health. This may be due to the interrelationship between immigrants’ characteristics and the social context.
For example, in the Birmingham sample, younger women and those who had a regular source of health care did not report better health. This could be related to a high prevalence of unrecognized or untreated chronic health conditions, such as hypertension and diabetes.33,34 Additionally, young immigrants’ settlement in the often isolated apartment complexes and mobile home parks in the area may lead to increased obesity, which is associated with reporting poorer health even in the absence of chronic health conditions.35 A study of obese Latinas in this community reported that women were not as physically active after moving to the U.S, and attributed their weight gain following migration to a lack of physical activity.36 Even when Latina immigrants in this setting seek services, their health care needs may not be adequately addressed in the clinical encounter, possibly due to the limited availability of bilingual staff and interpretation services.18 A recent study of Spanish-speaking Latinos seeking care from public clinics in Alabama found that they were less likely to report their medical problems were resolved following an appointment than English-speaking patients.37
We also found that Mexican-origin women in Birmingham had poorer health than Mexican-born women in the NHIS and that those with shorter durations of residence did not report better health. Without the connections of long-standing migrant networks found in traditional receiving areas and limited social support outside their partner’s extended kin, Mexican immigrants to the South may lack the social capital that would facilitate settlement and adaptation to a new environment.38,39 Furthermore, in communities that do not have long histories of foreign-born settlement, immigrants may have a greater sense of social isolation stemming from experiences of discrimination based on their limited English language ability, social class and perceived unauthorized status.11,40,41 This could contribute to high levels of distress and depression among women in the Birmingham study, which previous studies demonstrate is a strong predictor of poor self-rated health in Latinas.4,8
It is concerning that half of the women in this sample reported their health as fair or poor. Worse self-rated health has been associated with many comorbid conditions and an increased risk for adverse outcomes including mortality. Future research is needed to explore potential explanations for this finding in order to develop appropriate strategies to improve health. Possible approaches could include using community health workers to deliver culturally relevant health programs that would address modifiable risk factors for chronic diseases, and which also may alleviate immigrants’ sense of social isolation and lack of social cohesion in these communities. Additionally, efforts to strengthen the linguistic and cultural competency at locations where Latina immigrants seek health care would likely improve the diagnosis and treatment of health conditions among Latinos in these communities.
This study has several limitations. Our data for foreign-born Latinas in a new Southern destination derive from a convenience sample of women living in a metropolitan area in one state and may not be representative of foreign-born immigrants elsewhere in the region or reflect the perceived health status of Latino immigrant men. However, the community-based participatory research approach used to conduct this study, and specifically the use of lay health workers who were trusted in the community, likely increased participation by a broader segment of the Latina immigrant community (e.g., recent and undocumented Latina immigrants) than would otherwise be expected, and the sample characteristics were largely similar to those of Latina immigrants recruited through door-to-door sampling in other studies in Birmingham, as well as estimates of the foreign-born Latino population in the state.19,42 Additionally, women attending the outreach event from which the Birmingham data were collected may be more concerned about their health than women who did not attend. This selectivity is possible, and we caution readers to consider our results in this context. While we were able to create comparable measures of key factors associated with health status reported in other studies, we were unable to include others like language proficiency, other socioeconomic status indicators, and contextual variables. Such indicators would shed light on the large discrepancies in health observed here and should be included in future research examining the health of Latino immigrants in new destination areas. Finally, the mode of assessment differed for the two surveys, although we do not anticipate that this would affect respondents’ ratings of their health since the question does not ask about a highly sensitive or taboo topic.
Conclusion
The poorer assessments of health among foreign-born Latinas in this Southern metropolitan area, as well as other new destination settings,17,29 indicate that relying on nationally representative data may obscure important heterogeneity in the Latino immigrant population. Recognizing such variation is critical so that public health systems can respond to local needs and reduce potential risks for chronic disease and adverse health outcomes in the community.
Acknowledgments
Sources of Funding
The data collection for the Birmingham study was supported by Susan G. Komen for Cure North-Central Alabama Affiliate and the National Cancer Institute at the National Institutes of Health (R25CA106870).
Footnotes
Conflicts of Interest: The authors have no conflicts of interest.
Contributor Information
Kari White, University of Alabama at Birmingham, Health Care Organization & Policy.
Isabel C. Scarinci, University of Alabama at Birmingham, Division of Preventive Medicine.
References
- 1.DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question: A meta-analysis. J Gen Int Med. 2005;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. [PubMed] [Google Scholar]
- 3.Idler EL, Kasl SV. Self-ratings of health: do they also predict change in functional ability? J Gerontol. Series B: Psychol Soc Sci. 1995;50(6):S344–S353. doi: 10.1093/geronb/50b.6.s344. [DOI] [PubMed] [Google Scholar]
- 4.Benjamins MR, Hirschman J, Hirschtick J, Whitman S. Exploring differences in self-rated health among Blacks, Whites, Mexicans and Puerto Ricans. Ethn Health. 2012;17(5):463–476. doi: 10.1080/13557858.2012.654769. [DOI] [PubMed] [Google Scholar]
- 5.Borrell LN, Dallo FJ. Self-rated health and race among Hispanic and non-Hispanic adults. J Immigr Minor Health. 2008;10:229–238. doi: 10.1007/s10903-007-9074-6. [DOI] [PubMed] [Google Scholar]
- 6.Zack MM. Health-related quality of life - United States, 2006 and 2010. Morbid Mortal Wkly Rep. 2013;62(Supp 3):105–111. [PubMed] [Google Scholar]
- 7.Cho Y, Frisbie WP, Hummer RA, Rogers RG. Nativity, duration of residence and the health of Hispanic adults in the United States. Int Migr Rev. 2004;38(1):184–211. [Google Scholar]
- 8.Wilkinson AV, Hernandez-Valero MA, Etzel CJ, et al. Self-rated health among adult women of Mexican-origin. Hisp J Behavi Sci. 2006;28(1):127–142. doi: 10.1177/0739986305283221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Racial/ethnic disparities in self-rated health status among adults with and without disabilities - United States, 2004–2006. Morbid Mortal Wkly Rep. 2008;57(39):1069–1073. [PubMed] [Google Scholar]
- 10.Finch BK, Hummer RA, Reindl M, Vega WA. Validity of self-rated health among Latino(a)s. Am J Epidemiol. 2002;155(8):755–759. doi: 10.1093/aje/155.8.755. [DOI] [PubMed] [Google Scholar]
- 11.Massey DS. New faces in new places: The changing geography of American immigration. New York: Russell Sage Foundation; 2008. [Google Scholar]
- 12.Kochhar R, Suro R, Tafoya S. The new Latino South: The context and consequences of rapid population growth. Washington, D.C.: Pew Hispanic Center; 2005. [Google Scholar]
- 13.Passell JS, Cohn D. How many Hispanics? Comparing new census counts with the latest census estimates. Washington, D.C.: Pew Hispanic Center; 2011. [Google Scholar]
- 14.Passell JS, Cohn D, Lopez MH. Census 2010: 50 Million Latinos. Hispanics account for more than half of the nation’s growth in the past decade. Washington, D.C.: Pew Hispanic Center; 2011. [Google Scholar]
- 15.Mulvaney-Day NE, Alegria M, Sribney W. Social cohesion, social support and health among Latinos in the United States. Soc Sci Med. 2007;64:477–495. doi: 10.1016/j.socscimed.2006.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Erwin DO. An ethnographic description of Latino immigration in rural Arkansas: Intergroup relations and utilization of health care services. Southern Rural Sociol. 2003;19(1):46–72. [Google Scholar]
- 17.Harari N, Davis M, Heisler M. Strangers in a strange land: Health care experiences for recent Latino immigrants in Midwest communities. J Health Care Poor Underserved. 2008;9:1350–1367. doi: 10.1353/hpu.0.0086. [DOI] [PubMed] [Google Scholar]
- 18.Garces-Palacio IC, Scarinci IC, Harrison L. An examination of sociocultural factors associated with health and health-seeking among Latina immigrants. J Immigr Minor Health. 2006;8(4):377–385. doi: 10.1007/s10903-006-9008-8. [DOI] [PubMed] [Google Scholar]
- 19.Hidalgo B, Garces-Palacio IC, Scarinci IC. Preventive and curative care utilization among Mexican immigrant women in Birmingham, AL. J Immigr Minor Health. 2012;14(6):983–989. doi: 10.1007/s10903-012-9594-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.U.S. Census Bureau. 2010 Census redistricting data (Public Law 94–171) Summary File Table 1 P1. [Accessed January 2012];2010 http://2010.census.gov/news/releases/operations/cb11-cn47.html.
- 21.Franzini L, Fernandez-Esquer ME. Socioeconomic, cultural and personal influences on health outcomes among low-income Mexican-origin individuals in Texas. Soc Sci Mede. 2004;59:1629–1646. doi: 10.1016/j.socscimed.2004.02.014. [DOI] [PubMed] [Google Scholar]
- 22.Read JG, Gorman BK. Gender inequalities in US adult health: The interplay of race and ethnicity. Soc Sci Med. 2006 Mar;62(5):1045–1065. doi: 10.1016/j.socscimed.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 23.Gorman BK, Read JG, Krueger PM. Gender, acculturation, and health among Mexican Americans. J Health Soc Behav. 2010 Dec;51(4):440–457. doi: 10.1177/0022146510386792. [DOI] [PubMed] [Google Scholar]
- 24.White K, Garces I, Bandura L, McGuire AA, Scarinci IC. Design and evaluation of a theory-based, culturally relevant outreach model for breast and cervical cancer screening for Latina immigrants. Ethn Dis. 2012;22:274–280. [PMC free article] [PubMed] [Google Scholar]
- 25.Zsembik BA, Fennell D. Ethnic variation in health and the determinants of health among Latinos. Soc Sci Med. 2005;61:53–63. doi: 10.1016/j.socscimed.2004.11.040. [DOI] [PubMed] [Google Scholar]
- 26.National Center for Health Statistics. NHIS Survey Description. Hyattsville, MD: Division of Health Interview Statistics, National Center for Health Statistics; 2009. [Google Scholar]
- 27.Brookhart MA, Schneeweiss S, Rothman KJ, Glynn RJ, Avorn J, Sturmer T. Variable selection for propensity score models. Am J Epidemiol. 2006 Jun 15;163(12):1149–1156. doi: 10.1093/aje/kwj149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Efron B. Bootstrap methods: Another look at the jackknife. Ann Statist. 1979;7(1):1–26. [Google Scholar]
- 29.Denham AC, Frasier PY, Hooten EG, et al. Intimate partner violence among Latinas in eastern North Carolina. Violence Against Women. 2007 Feb;13(2):123–140. doi: 10.1177/1077801206296983. [DOI] [PubMed] [Google Scholar]
- 30.Redstone Akresh I, Frank R. Health selection among new immigrants. Am J Pub Health. 2008;98(11):2058–2064. doi: 10.2105/AJPH.2006.100974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Passell JS, Cohn D. A portrait of unauthorized immigrants in the United States. Washington, D.C.: Pew Hispanic Center; 2009. [Google Scholar]
- 32.Hacker K, Chu J, Leung C, et al. The impact of Immigration and Customs Enforcement on immigrant health: Perceptions of immigrants in Everett, Massachusetts, USA. Soc Sci Med. 2011 Aug;73(4):586–594. doi: 10.1016/j.socscimed.2011.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.White K, Potter JE, Hopkins K, Amastae J, Grossman D. Hypertension among oral contraceptive users in El Paso, Texas. J Health Care Poor Underserved. 2013;24(4):1511–1521. doi: 10.1353/hpu.2013.0172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barcellos SH, Goldman DP, Smith JP. Undiagnosed disease, especially diabetes, casts doubt on some of reported health 'advantage' of recent Mexican immigrants. Health Aff (Millwood) 2012;31(12):2727–2737. doi: 10.1377/hlthaff.2011.0973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Okosun IS, Choi S, Matamoros T, Dever GE. Obesity is associated with reduced self-rated general health status: Evidence from a representative sample of white, black and Hispanic Americans. Prev Med. 2001;32(5):429–436. doi: 10.1006/pmed.2001.0840. [DOI] [PubMed] [Google Scholar]
- 36.Agne A, Daubert R, Munoz ML, Scarinci IC, Cherrington A. The cultural context of obesity: Exploring perceptions of obesity and weight loss among Latina immigrants. J Immigr Minor Health. 2012;14:1063–1070. doi: 10.1007/s10903-011-9557-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Welty E, Yeager VA, Ouimet C, Menachemi N. Patient Satisfaction Among Spanish-Speaking Patients in a Public Health Setting. J Healthcare Qual. 2012;34(5):31–38. doi: 10.1111/j.1945-1474.2011.00158.x. [DOI] [PubMed] [Google Scholar]
- 38.Palloni A, Massey DS, Ceballos M, Espinosa KE, Spittel M. Social capital and international migration: A test using information on family networks. Am J Sociol. 2001;106(5):1262–1298. [Google Scholar]
- 39.Lacy EC. Integrating into new communities: The Latino perspective. In: Lippard CD, Gallagher CA, editors. Being brown in Dixie: Race, ethnicity and Latino immigration in the New South. Boulder: First Forum Press; 2011. pp. 115–132. [Google Scholar]
- 40.Marrow HB. Intergroup relations: Reconceptualizing discrimination and hierarchy. In: Lippard CD, Gallagher CA, editors. Being brown in Dixie: Race, ethnicity and Latino immigration in the New South. Boulder: First Forum Press; 2011. pp. 53–76. [Google Scholar]
- 41.Ornelas I, Perreira K, Beeber L, Maxwell L. Challenges and strategies to maintaining emotional health: Qualitative perspectives of Mexican immigrant mothers. J Fam Issues. 2009;30(11):1556–1575. [Google Scholar]
- 42.Pew Hispanic Center. Demographic profile of Hispanics in Alabama. Washington, D.C.: Pew Hispanic Center; 2010. [Google Scholar]