Abstract
OBJECTIVES:
To assess the adherence of premature infants with the American Academy of Pediatrics health supervision visit schedule, factors affecting adherence, and the association of adherence with preventive care.
METHODS:
Retrospective cohort of all infants ≤35 weeks’ gestation, born 2005 to 2009, receiving care at a 30-site primary care network for at least 24 months (n = 1854). Adherence was defined as having a health supervision visit within each expected time period during the first 18 months of life. Logistic regression identified sociodemographic and medical factors associated with nonadherence and risk-adjusted association between nonadherence and outcomes.
RESULTS:
Only 43% received all expected health supervision visits. Those with Medicaid insurance (adjusted odds ratio [AOR] 0.46, 95% confidence interval [CI] 0.35–0.60), a visit without insurance (AOR 0.46, 95% CI 0.32–0.67), chronic illness (AOR 0.7, 95% CI 0.51–0.97), and black race (AOR 0.7, 95% CI 0.50–0.98) were less adherent, whereas provider continuity of care (AOR 2.89, 95% CI 1.92–4.37) and lower birth weight (AOR 1.67, 95% CI 1.02–2.73) increased adherence. Infants <100% adherent were less likely to be up to date with immunizations and receive recommended preventive care. In nearly half of missed visit windows, no health supervision visit was scheduled.
CONCLUSIONS:
Fewer than half of premature infants were fully adherent with the preventive health schedule with associated gaps in health monitoring and immunization delays. These data suggest the importance of health supervision visits and the need to explore scheduling facilitators for those at risk for nonadherence.
What’s Known on This Subject:
Premature infants are at risk for medical and neurodevelopmental sequelae. Close monitoring is an important role for primary care providers. Premature infants have high use of health care services; however, little is known about the role of health supervision visits.
What This Study Adds:
This study explores the utilization and value of health supervision visits for premature infants. Fewer than half were found to be fully adherent to the health supervision visit schedule, resulting in preventive care gaps and immunization delays.
There is increased interest in providing high-quality, high-value care within the United States health care system, including the role of health supervision, or “well-child,” visits. The American Academy of Pediatrics (AAP) recommends periodic health supervision visits throughout childhood.1 These age-focused visits serve as an opportunity to assess growth, nutrition, screen for sequelae, survey development, provide guidance, and ensure immunization adequacy. These visits may have greater importance for premature infants who are at increased risk for medical and neurodevelopmental sequelae.2–15
There are few studies assessing adherence with health supervision visits in the general pediatric population and fewer in high-risk populations. According to Medical Expenditure Survey data, infants were found to be 83% adherent with the age-specific number of visits recommended by the AAP.16 Partly due to variation in the definition of adherence, reported rates range from 8.7% to 86.6%, with infants having greater adherence than older children.16–28 These studies mainly involve claims and surveys, with surveys more likely to reflect increased adherence with care.29
Children with special health care needs have been reported to have similar or higher rates of adherence compared with those without special needs.16,19 There has been only 1 study, limited to children receiving Medicaid, that compared late preterm to term children and found similar rates of adherence.18 Data about adherence rates for lower birth weight premature infants are lacking. Similarly, there is little research on the impact of health supervision visit adherence on outcomes, with most studies focusing on improved immunization rates.24,26,30–33 To our knowledge, no studies used an electronic health record to assess actual adherence to health supervision visits.
The purpose of this study was to explore the impact of preterm birth on adherence with the preventive health care visit schedule from 1 to 18 months of life, for a potential maximum of 8 recommended visits; factors affecting adherence; and the association of adherence with the receipt of preventive care.
Methods
Setting and Study Population
A retrospective cohort design evaluated care received by preterm infants (defined by a gestational age of ≥22 and ≤35 weeks) in the primary care network at The Children’s Hospital of Philadelphia born January 1, 2005, to January 1, 2009, who presented for primary care within 168 days of age (n = 2147). The network included 30 urban and suburban sites in Pennsylvania and New Jersey. The 168-day limit was selected as it corresponded to the upper age limit for the 4- to 5-month visit using the Pennsylvania Early and Periodic Screening, Diagnosis, and Treatment Program Age Requirements for Screening Visits Desk Guide.34 Infants presenting after this threshold may (1) have transferred into the practice from another practice, or (2) have significant illness severity during initial hospitalization that resulted in discharge after 168 days, and thus their use of preventive visits may not be typical of most premature infants. Infants who did not have at least 1 primary care visit between 365 days of life and before 2 years of age were excluded to eliminate those who had left the network and thus were lost to follow-up (n = 250). Infants with congenital anomalies or cancer were excluded, as their outpatient use may be atypical (n = 43). The remaining 1854 (86%) met eligibility criteria. The Children’s Hospital of Philadelphia Institutional Review Board approved this study. Patient information was documented by providers during health care encounters in the electronic health record using the EPIC Hyperspace system (EPIC manufacturing, Verona, WI).35
Definition of Adherence With Health Supervision Visits
Adherence with health supervision visits was defined as having a health supervision visit within an expected age-based time period up to 18 months of age, as defined by the Pennsylvania Early and Periodic Screening, Diagnosis, and Treatment Guide which is based on the AAP Bright Futures Guidelines.1 We examined visits during the following time periods in months (days): 1 (0–46), 2–3 (47–107), 4–5 (108–168), 6–8 (169–260), 9–11 (261–365), 12 (366–412), 15 (413–504), and 18 (505–641).
The pool of eligible visits was limited to encounters identified as office visits for health supervision with a physician or nurse practitioner in the primary care practices. Health supervision visits were identified using International Classification of Diseases, Ninth Revision (ICD-9) codes V20.0, V20.1, V20.2, or V70.0. Visits with an ICD-9 principal diagnosis indicating laboratory assessment, or administrative encounter with no other diagnosis codes, were excluded after examination of the office note verified that no health supervision occurred during the visit.
As premature infants may miss early visits due to neonatal hospitalization, we used a percentage of expected visits to determine adherence. Adherence percentage was delineated into 3 categories: 100%, 75% to 88%, and <75%. As there were a maximum of 8 possible health supervision visits in our study design, 88% was the maximum adherence if a child missed 1 health supervision visit. The maximum number of visits decreased if a child’s initial hospitalization was longer than the time period for a recommended early visit. For these infants, the denominator of expected visits was decreased by the number of visits missed due to the initial hospitalization. As a secondary analysis, adherence was assessed as missing 0, 1, 2, and 3 or more health supervision visits in the expected time periods. Finally, we reran the models by using the total number of health supervision visits, regardless of timing of visits, and assessed impact on outcomes.
Confounding Variable Definitions
Gestational age, birth weight, ethnicity, and race were classified based on information recorded in the record. As household income information was not available, zip code–level median income was used as a proxy. Insurance type was divided into 3 exclusive categories: any visit without insurance, any use of federal Medicaid insurance without ever being uninsured (including the Children's Health Insurance Program), and sole use of private insurance during the study period. Provider continuity of care was determined using the formula described by Bice and Boxerman36 (range 0–1) with 1 representing continuity with 1 provider for all health supervision visits, and 0 representing different providers for each visit.
Bright Futures recommends that additional visits should be considered if there are “variations from normal.”1 Thus, we examined whether any planned additional visits, not coded as health supervision visits, occurred over the first 18 months of age. Any encounters with a visit reason listed as “recheck,” “weight check,” or “recheck weight” were included. The remaining office visits were coded as sick or nurse immunization visits based on an examination of the office note and ICD-9 diagnosis codes. Additional planned, sick, and nurse immunization visits were expressed in terms of rate per month. The number of eligible months varied for each patient and was calculated by using the time from the first to the last visit in our database. Chronic illness was identified if any of the following complications of preterm birth associated with increased health care use37,38 or other chronic conditions were noted: bronchopulmonary dysplasia, necrotizing enterocolitis, intraventricular hemorrhage, asthma, seizures, short bowel syndrome, ventriculo-peritoneal shunt, colostomy, ileostomy, gastrostomy, tracheostomy, or supplemental oxygen.
Preventive Care Outcome Variable Definitions
Measures indicated as “to be performed” per the AAP Periodicity Schedule were identified and the following were assessed: developmental assessment; immunizations excluding influenza and Synagis; and the ordering of hematocrit, hemoglobin (Hgb), or complete blood count before completion of the 12-month visit window. Based on current guidelines,39 the ordering of lead testing before completion of the 12-month visit window was assessed only for patients receiving Medicaid. All primary care encounters during the study period, including non–health supervision visits, were included to determine if recommended care was performed.
To determine if a health supervision visit was missed because it was never scheduled, we assessed whether a health supervision visit was scheduled within the expected window and if other primary care encounters occurred during the window. The following were hand-coded at visit level for all windows with missed health supervision visits: health supervision visit was scheduled, no show or cancellation of health supervision visit; sick or nurse immunization visit, planned additional visit; left without being seen, conversion of a health supervision visit to a sick or nurse immunization visit.
Data Analysis
For univariable analysis, χ2 analysis and binary logistic regression identified factors associated with adherence with health supervision visits. A multivariable logistic regression model quantified the association of these factors on adherence. As birth weight and gestational age are collinear variables, only birth weight was included in the models. To control for the clustering of outcomes within primary care sites, these analyses and all subsequent multivariable analyses were performed by using robust SEs and fixed practice effects. To assess how adherence was associated with outcomes, multivariable logistic regression models were constructed with the 3 percentage categories of adherence or the 4 categories of missed visits as independent predictor variables and each outcome listed previously as dependent variables. Reasons for missing a health supervision visit were quantified by percentage categories of adherence. Risk-adjusted probabilities were determined from the logistic regression models by using marginal standardization.40
Results
Patient and visit characteristics are shown in Table 1. Fewer than half of the children, 43% (803), were adherent for all expected health supervision visits, with 35% (655) adherent for 75% to 88% of the visits and 21% (396) adherent for <75% of the visits. Adherence decreased after the 6- to 8-month window. Most, 77% (1432), had additional planned visits; nearly all, 96% (1777), had at least 1 sick visit; and 70% (1300) had nurse immunization visits during the study period.
TABLE 1.
Patient and Visit Characteristics Per Adherence Category
| Adherent with all expected health supervision visits, n (%) | Total, n = 1854 | 100%, n = 803 (43) | 75%–88%, n = 655 (35) | <75%, n = 396 (21) | P |
|---|---|---|---|---|---|
| Adherent with individual health supervision visits, mo, n (%) | |||||
| 4–5, n = 1854 | 1679 (91) | 803 (100) | 608 (93) | 268 (47) | <.0001 |
| 6–8, n = 1854 | 1694 (91) | 803 (100) | 625 (95) | 266 (47) | <.0001 |
| 9–11, n = 1854 | 1577 (85) | 803 (100) | 561 (86) | 213 (50) | <.0001 |
| 12, n = 1854 | 1400 (76) | 803 (100) | 448 (68) | 149 (48) | <.0001 |
| 15, n = 1854 | 1299 (70) | 803 (100) | 371 (57) | 125 (47) | <.0001 |
| 18, n = 1854 | 1478 (80) | 803 (100) | 506 (77) | 169 (50) | <.0001 |
| Additional visits | |||||
| Patients with planned visits, n (%) | 1432 (77) | 660 (82) | 508 (78) | 264 (67) | <.0001 |
| Patients with sick visits, n (%) | 1777 (96) | 785 (98) | 631 (96) | 361 (91) | <.0001 |
| Patients with nurse immunization visits, n (%) | 1300 (70) | 639 (80) | 433 (66) | 228 (58) | <.0001 |
| Average sick visits/mo, mean ± SD | 0.36 ± 0.29 | 0.42 ± 0.32 | 0.34 ± 0.25 | 0.27 ± 0.24 | <.0001 |
| Average planned visits/mo, mean ± SD | 0.10 ± 0.10 | 0.11 ± 0.11 | 0.09 ± 0.09 | 0.08 ± 0.09 | <.0001 |
| Average nurse immunization visits/mo, mean ± SD | 0.12 ± 0.13 | 0.15 ± 0.13 | 0.11 ± 10.12 | 0.09 ± 0.13 | <.0001 |
| Provider continuity of care (health supervision visits), mean ± SD | 0.51 ± 0.32 | 0.53 ± 0.31 | 0.51 ± 0.31 | 0.46 ± 0.36 | .003 |
| Boys, n (%) | 929 (50) | 389 (48) | 347(53) | 193 (49) | .1878 |
| Birth weight, g, n (%) | <.0001 | ||||
| 2500+ | 230 (12) | 101 (13) | 92 (14) | 37 (9) | |
| 1500–<2500 | 1059 (57) | 476 (59) | 393 (60) | 190 (48) | |
| 1000–1500 | 337 (18) | 137 (17) | 99 (15) | 101 (26) | |
| <1000 | 209 (11) | 87 (11) | 61 (9) | 61 (15) | |
| Gestational age, wk, n (%) | .0012 | ||||
| 34–≤35 | 426 (23) | 169 (21) | 169 (26) | 88 (22) | |
| 32–<34 | 479 (26) | 214 (27) | 166 (25) | 99 (25) | |
| 28–<32 | 440 (24) | 187 (23) | 141 (22) | 112 (28) | |
| <28 | 191 (10) | 69 (9) | 56 (9) | 66 (17) | |
| Ethnicity/Race, n (%) | |||||
| Non-Hispanic | 1799 (97) | 778 (97) | 635 (97) | 386 (97) | .8415 |
| Black or African American | 799 (43) | 156 (19) | 343 (52) | 300 (76) | <.0001 |
| White | 767 (41) | 491 (61) | 226 (35) | 50 (13) | |
| Asian | 34 (2) | 19 (2) | 12 (2) | 3 (0.1) | |
| Other | 254 (14) | 137 (17) | 74 (11) | 43 (11) | |
| Insurance group, n (%) | <.0001 | ||||
| All private | 875 (47) | 536 (66) | 264 (40) | 75 (19) | |
| Any Medicaid | 641 (35) | 158 (20) | 263 (40) | 220 (56) | |
| Any self-pay | 338 (18) | 109 (14) | 128 (20) | 101 (26) | |
| Chronic illness | 427 (23) | 134 (17) | 150 (23) | 143 (36) | <.0001 |
Factors Affecting Adherence
Several factors were associated with adherence in multivariable analyses (Table 2). Any use of Medicaid insurance (adjusted odds ratio [AOR] 0.46, 95% confidence interval [CI] 0.35–0.60), any visit without insurance (AOR 0.46, 95% CI 0.32–0.67), chronic illness (AOR 0.7, 95% CI, 0.51–0.97), and black race (AOR 0.70, 95% CI 0.50–0.98) were associated with decreased adherence. Provider continuity of care for health supervision visits using a 10% change in Bice score (AOR 2.89, 95% CI 1.92–4.37) and birth weight <1000 g (AOR 1.67, 95% CI 1.02–2.73) were associated with increased compliance.
TABLE 2.
Predictors for Adherence With All Recommended Health Supervision Visits
| AOR (95% CI) | P | |
|---|---|---|
| Zip code level median income | 1.01 (1.00–1.02) | .10 |
| Chronic illness | 0.7 (0.51–0.97) | .03 |
| Race | ||
| White | Reference | Reference |
| Black/African-American | 0.70 (0.50–0.98) | .04 |
| Other | 1.31 (0.85–2.00) | .22 |
| Birth weight category, g | ||
| 2500+ | Reference | Reference |
| 1500–<2500 | 1.51 (1.04–2.20) | .04 |
| 1000–<1500 | 1.42(0.90–2.25) | .13 |
| <1000 | 1.67 (1.02–2.73) | .03 |
| Insurance group | ||
| Private | Reference | Reference |
| Any Medicaid | 0.46 (0.35–0.60) | <.0001 |
| Any self-pay | 0.46 (0.32–0.67) | <.0001 |
| Provider continuity of care (health supervision visits) | 2.89 (1.92–4.37) | <.0001 |
| Sick visits/mo | 1.54 (0.97–2.43) | .06 |
| Planned additional visits/mo | 2.99 (0.65–13.74) | .15 |
| Nurse immunization visits/mo | 1.74 (0.57–5.29) | .33 |
Impact of Adherence on Outcome
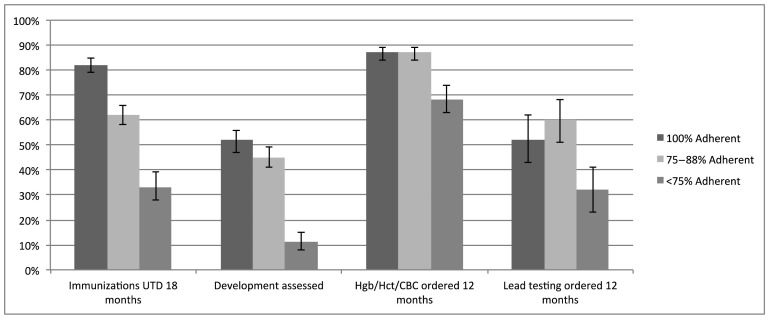
Compared with those 100% adherent, being less adherent was associated with several outcomes after controlling for patient and visit characteristics (Table 3). Predicted probabilities for the average patient are shown in Fig 1. Children who were 75% to 88% adherent were at increased risk for immunization delay at the completion of the 4- to 5-, 6- to 8-, 15-, and 18-month windows with a 62% predicted probability (AOR 0.36, 95% CI 0.25–0.52) of being up to date (UTD) at 18 months compared with 82% for fully adherent patients. Children who were <75% adherent were at increased risk for immunization delays at the completion of all visit windows, with a 33% (AOR 0.11, 95% CI 0.07–0.18) predicted probability of being UTD at 18 months. Children who were 75% to 88% adherent were at increased risk of not having development assessed (AOR 0.76, 95% CI 0.59–0.98), and those who were <75% adherent were additionally at increased risk of not having Hgb (AOR 0.33, 95% CI 0.22–0.56) or lead (AOR 0.41, 95% CI 0.22–0.79) measured by 12 months.
TABLE 3.
Impact of Adherence on Outcome by Percent Adherent Category
| 75–<88% Adherent | <75% Adherent | |||
|---|---|---|---|---|
| AOR (95% CI) | P | AOR (95% CI) | P | |
| Immunizations UTD by mo | ||||
| 2–3 | 0.95 (0.50–1.79) | .87 | 0.21 (0.12–0.37) | <.0001 |
| 4–5 | 0.51 (0.29–0.91) | .02 | 0.12 (0.07–0.21) | <.0001 |
| 6–8 | 0.74 (0.56–0.97) | .03 | 0.40 (0.24–0.67) | .0004 |
| 12 | 0.80 (0.60–1.06) | .12 | 0.59 (0.34–1.01) | .054 |
| 15 | 0.25 (0.18–0.37) | <.0001 | 0.11 (0.07–0.16) | <.0001 |
| 18 | 0.36 (0.25–0.52) | <.0001 | 0.11 (0.07–0.18) | <.0001 |
| Development assessed | 0.76 (0.59–0.98) | .04 | 0.11 (0.06–0.21) | <.0001 |
| Hgb/Hct/CBC testing ordered by 12 mo | 1.03 (0.7–1.52) | .87 | 0.33 (0.22–0.56) | <.0001 |
| Lead testing (Medicaid patients) ordered by 12 mo | 1.37 (0.80–2.33) | .25 | 0.41 (0.22–0.79) | .007 |
Adjusted for median income, sick visits per month, planned additional visits per month, nurse immunization visits per month, chronic illness, race, birth wt category, and Bice score using multivariable logistic regression models. CBC, complete blood count; Hct, hematocrit.
FIGURE 1.
Predicted probabilities of selected outcomes for the average patient, stratified by adherence category. Error bars present 95% CIs for each predicted probability.
The regression model was rerun assessing outcomes based on the number of health supervision visits missed within expected time periods (Table 4). Missing at least 1 visit increased the risk for immunization delay at the completion of the 6- to 8-, 15-, and 18-month windows. Missing ≥3 visits was associated with immunization delay at all ages and the reduced likelihood of receiving developmental assessment, Hgb, or lead testing. To control for the possibility of odds ratios being inflated due to the high rates of nonadherence, the model was rerun using categorical predicted means for both percentage adherent categories and for the number of missed health supervision visits. The findings were unchanged in both instances.
TABLE 4.
Impact of Adherence on Outcome by Number of Health Supervision Visits Missed Within Expected Time Periods
| 1 Missed Visit, n = 478 (26%) | 2 Missed Visits, n = 286 (15%) | 3+ Missed Visits, n = 287 (15%) | ||||
|---|---|---|---|---|---|---|
| AOR (95% CI) | P | AOR (95% CI) | P | AOR (95% CI) | P | |
| Immunizations UTD by mo | ||||||
| 2–3 | 1.01 (0.49–2.09) | .98 | 0.44 (0.23- 0.85) | .01 | 0.19 (0.1–0.36) | <.0001 |
| 4–5 | 0.63 (0.33–1.21) | .16 | 0.27 (0.15–0.46) | <.0001 | 0.09 (0.06–0.16) | <.0001 |
| 6–8 | 0.71 (0.53–0.95) | .02 | 0.75 (0.53–1.05) | .09 | 0.32 (0.19–0.55) | <.0001 |
| 12 | 0.77 (0.57–1.03) | .08 | 0.84 (0.59–1.21) | .36 | 0.51 (0.29–0.92) | .03 |
| 15 | 0.25 (0.18–0.36) | <.0001 | 0.21 (0.13–0.35) | <.0001 | 0.09 (0.06–0.14) | <.0001 |
| 18 | 0.37 (0.26–0.54) | <.0001 | 0.26 (0.17–0.39) | <.0001 | 0.09 (0.05–0.14) | <.0001 |
| Development assessed | 0.83 (0.64–1.08) | .16 | 0.42 (0.3–0.59) | <.0001 | 0.07 (0.03–0.16) | <.0001 |
| Hgb/Hct/CBC testing ordered by 12 mo | 1.20 (0.80–1.79) | .38 | 0.63 (0.38–1.07) | .09 | 0.27 (0.16–0.45) | <.0001 |
| Lead testing (Medicaid patients) ordered by 12 mo | 1.47 (0.87–2.49) | .15 | 1.13 (0.5- 2.56) | .77 | 0.28 (0.13–0.64) | .002 |
Adjusted for median income, sick visits per month, planned additional visits per month, nurse immunization visits per month, chronic illness, race, birth weight category, and Bice score for continuity of care. All AORs are compared with the reference group of 0 missed health supervision visits. CBC, complete blood count; Hct, hematocrit.
Fourteen percent (260) of the children had health supervision visits outside the expected time periods. Using the total number of health supervision visits regardless of timing, outcomes were unchanged.
Missing Health Supervision Visits
There were 2071 windows with missed health supervision visits (Table 5). We found that in 49% (1012) of those windows, a health supervision visit had never been scheduled. A non–health supervision visit within the primary care office occurred in 42% (425) of those windows. In windows with a scheduled health supervision visit, the most common reason for a missed visit was a no show (n = 718, 68%).
TABLE 5.
Windows Missing Health Supervision Visits
| Overall, 2071, n (%) | 75%–88% Adherent, 832 (40%), n (%) | <75% Adherent, 1239 (60%), n (%) | |
|---|---|---|---|
| No health supervision visit scheduled | 1012 (49) | 430 (52) | 582 (47) |
| Sick visit | 342 (34) | 177 (41) | 165 (28) |
| Additional health supervision visit before/after | 216 (21) | 99 (23) | 117 (20) |
| missed visit window | |||
| Planned additional visit | 46 (5) | 27 (6) | 19 (3) |
| Nurse immunization visit | 114 (11) | 63 (15) | 51 (9) |
| Sick/planned/nurse immunization visits combined | 425 (42) | 227 (53) | 198 (34) |
| Health supervision visit scheduled | 1059 (51) | 402 (48) | 657 (53) |
| No show | 718 (68) | 227 (57) | 491 (75) |
| Cancel | 498 (47) | 226 (56) | 272 (41) |
| Sick visit with missed health supervision visit | 506 (48) | 207 (52) | 299 (46) |
| Additional health supervision visit before/after missed visit window | 245 (23) | 97 (24) | 148 (23) |
| Planned additional visit with missed health supervision visit | 136 (13) | 55 (14) | 81 (12) |
| Nurse immunization visit with missed health supervision visit | 196 (19) | 74 (18) | 122 (19) |
| Sick/planned/nurse immunization visits combined | 631 (60) | 246 (41) | 385 (45) |
| Converted health supervision visit to sick visita | 81 (8) | 37 (9) | 44 (7) |
| Converted health supervision visit to nurse immunization visita | 23 (2) | 9 (2) | 14 (2) |
| Converted health supervision visit to sick/nurse immunization visits combineda | 102 (10) | 46 (11) | 56 (9) |
| Left without being seen | 1 (<1) | 0 | 1 (<1) |
Occurred same day.
Approximately one-fifth of health supervision visits were scheduled outside of the expected window, resulting in 2 visits in 1 window and a missed visit in an adjoining window. The median interval between same-window visits in the first year of life was 52 days (interquartile range 35–70). We also found instances in which health supervision visits were converted to sick or nurse immunization encounters resulting in missed health supervision visits.
Discussion
Although considered a high-risk group, only 43% of the premature infants in this study were fully adherent with the AAP health supervision visit schedule. This is lower than the Medical Expenditure Study and the National Committee for Quality Assurance’s Health Plan Employer Data and Information Set.41 According to recent Health Plan Employer Data and Information Set data, 76.9% to 79.0% of commercially insured infants and 61.6% of those on Medicaid had 6 or more well-child visits in the first 15 months of life. We found gaps in health monitoring of this high-risk group and delays in immunizations that persisted throughout most of the first 18 months of life. The most common reason a health supervision visit was missing from a window was that it had never been scheduled in that window.
There has been limited research exploring the effectiveness of preventive care visit adherence in the pediatric population. Similar to our findings, several studies have shown an UTD immunization status to be associated with greater adherence to health supervision visits.24,26,30–33 Being adherent with preventive care visits has been shown to decrease the likelihood of avoidable hospitalizations,19,24,42,43 and missing visits was associated with increased risk of emergency department visits.22 Besides immunization delays, we found that developmental assessment, and anemia and lead screening, were less likely to occur if a child was not fully adherent to the health supervision visit schedule.
Risk factors associated with nonadherence in our study included lack of private insurance, black race, and chronic illness. Several of these factors have been shown to affect adherence for the general pediatric population. Children with Medicaid have been found to have low adherence with health supervision visits,17,18,24,44 and black race was the strongest predictor for inadequate health supervision care when using national survey data.25 Similar to our findings, other general pediatric studies have found provider continuity of care to be a strong predictor for receipt of preventive care services.45–51
In contrast to other studies in which special health care needs have been associated with increased adherence,16,19,20,52 chronically ill premature infants were less likely to be adherent with the preventive health schedule. However, we found an opposite relationship between extreme prematurity and chronic illness with regard to adherence (Table 2). This may reflect our definition of chronic illness that included illnesses not only seen in extremely premature infants.
Despite most children in our study having additional visits, immunization delays and gaps in care due to missed preventive visits were found. Similar to our findings, frequent non–health supervision pediatric visits by premature infants have been documented by others.18,37,38 The AAP has a policy statement addressing community readiness when discharging high-risk infants.53 Educating families about the role of health supervision visits and how these differ from other visits their child will be having is an important consideration in discharge preparation.
We found that nearly half of missed health supervision visits were never scheduled in the windows when due, and in some cases children were in the practice for other reasons during those missed visit windows. The benefit of scheduling health supervision visits was demonstrated in a recent study exploring delivery of well-child care at acute visits. For those who were not UTD, 28% to 45% did not schedule a well-child visit. However, if a well-child appointment was scheduled for those not UTD, appointments occurred 65% to 77% of the time.54 Our findings regarding scheduling issues bear scrutiny by practices of barriers to scheduling, mechanisms by which to recognize the need to schedule patients when they appear in the practice for other reasons, and the use of non–health supervision encounters as a way to provide preventive care for high-risk infants.
Limitations for our study included not being able to assess the impact of hospitalizations and emergency department visits on adherence, as this information was not available for the entire cohort. In addition, we could not assess how specialty visits affected adherence, as only a few specialty practices were on the electronic health record during the study period. Children without 2 or more consecutive health supervision visits and who never returned for any visit were assumed to have left the practice. This could have overestimated adherence, as we potentially eliminated children whose missed visits were the result of not seeking any health care. In this case, our results underestimate the effect of nonadherence and outcomes. Household income, census tract, or block group area information was not available, necessitating the use of the zip code as a socioeconomic proxy, which could have resulted in detecting a smaller effect. As this study reflects 1 pediatric hospital network in which most providers are physicians, this may limit generalizability to nonphysician models of health supervision.
Conclusions
In summary, only 43% of premature infants were fully adherent with the AAP health supervision schedule during the first 18 months of life. In nearly half of the windows with missing health supervision visits, a visit had not been scheduled. A primary care encounter occurred in 42% of those windows. Adherence with health supervision visits appeared to play an important role in meeting the preventive health needs of premature infants. Although nearly all children had additional primary care non–health supervision visits, being less adherent for health supervision visits resulted in delays in immunizations and gaps in health monitoring. These data suggest adherence to the health supervision visit schedule plays a role in maximizing preventive care for this high-risk population and the importance of exploring scheduling practices to facilitate visit adherence.
Glossary
- AAP
American Academy of Pediatrics
- AOR
adjusted odds ratio
- CI
confidence interval
- Hgb
hemoglobin
- ICD-9
International Classification of Diseases, Ninth Revision
- UTD
up to date
Footnotes
Dr D’Agostino conceptualized and designed the study, and drafted the initial manuscript; Ms Passarella, Mr Saynisch, and Ms Macheras carried out the initial analyses, and critically reviewed the manuscript; Ms Martin critically reviewed the final manuscript as submitted; Dr Lorch conceptualized and designed the study, and revised the initial manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: All phases of this study were supported by National Institutes of Health grant R01 HD057168. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Hagan JF, Shaw JS, Duncan PM. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 3rd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2008 [Google Scholar]
- 2.March of Dimes PMNCH, Save the Children, WHO. Born Too Soon: The Global Action Report on Preterm Birth. Geneva, Switzerland: World Health Organization; 2012 [Google Scholar]
- 3.Saigal S, Stoskopf B, Streiner D, Paneth N, Pinelli J, Boyle M. Growth trajectories of extremely low birth weight infants from birth to young adulthood: a longitudinal, population-based study. Pediatr Res. 2006;60(6):751–758 [DOI] [PubMed] [Google Scholar]
- 4.Hack M, Schluchter M, Cartar L, Rahman M, Cuttler L, Borawski E. Growth of very low birth weight infants to age 20 years. Pediatrics. 2003;112(1 pt 1). Available at: www.pediatrics.org/cgi/content/full/112/1/e30 [DOI] [PubMed] [Google Scholar]
- 5.Euser AM, de Wit CC, Finken MJ, Rijken M, Wit JM. Growth of preterm born children. Horm Res. 2008;70(6):319–328 [DOI] [PubMed] [Google Scholar]
- 6.DeMauro SB, Patel PR, Medoff-Cooper B, Posencheg M, Abbasi S. Postdischarge feeding patterns in early- and late-preterm infants. Clin Pediatr (Phila). 2011;50(10):957–962 [DOI] [PubMed] [Google Scholar]
- 7.Buswell CA, Leslie P, Embleton ND, Drinnan MJ. Oral-motor dysfunction at 10 months corrected gestational age in infants born less than 37 weeks preterm. Dysphagia. 2009;24(1):20–25 [DOI] [PubMed] [Google Scholar]
- 8.Berglund S, Westrup B, Domellöf M. Iron supplements reduce the risk of iron deficiency anemia in marginally low birth weight infants. Pediatrics. 2010;126(4). Available at: www.pediatrics.org/cgi/content/full/126/4/e874 [DOI] [PubMed] [Google Scholar]
- 9.Baker RD, Greer FR, Committee on Nutrition American Academy of Pediatrics . Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics. 2010;126(5):1040–1050 [DOI] [PubMed] [Google Scholar]
- 10.Rao R, Georgieff MK. Iron therapy for preterm infants. Clin Perinatol. 2009;36(1):27–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stephens BE, Vohr BR. Neurodevelopmental outcome of the premature infant. Pediatr Clin North Am. 2009;56(3):631–646 [DOI] [PubMed] [Google Scholar]
- 12.Jessop LJ, Kelleher CC, Murrin C, et al. Lifeways Cohort Study Steering Group . Determinants of partial or no primary immunisations. Arch Dis Child. 2010;95(8):603–605 [DOI] [PubMed] [Google Scholar]
- 13.Crawford NW, Yeo V, Hunt RW, Barfield C, Gelbart B, Buttery JP. Immunisation practices in infants born prematurely: neonatologists’ survey and clinical audit. J Paediatr Child Health. 2009;45(10):602–609 [DOI] [PubMed] [Google Scholar]
- 14.Langkamp DL, Hoshaw-Woodard S, Boye ME, Lemeshow S. Delays in receipt of immunizations in low-birth-weight children: a nationally representative sample. Arch Pediatr Adolesc Med. 2001;155(2):167–172 [DOI] [PubMed] [Google Scholar]
- 15.Davis RL, Rubanowice D, Shinefield HR, et al. Centers for Disease Control and Prevention Vaccine Safety Datalink Group . Immunization levels among premature and low-birth-weight infants and risk factors for delayed up-to-date immunization status. JAMA. 1999;282(6):547–553 [DOI] [PubMed] [Google Scholar]
- 16.Selden TM. Compliance with well-child visit recommendations: Evidence from the medical expenditure panel survey, 2000–2002. Pediatrics 2006;118(6). Available at: www.pediatrics.org/cgi/content/full/118/6/e1766 [DOI] [PubMed]
- 17.Pittard WB, III. Well-child care in infancy and emergency department use by South Carolina Medicaid children birth to 6 years old. South Med J. 2011;104(8):604–608 [DOI] [PubMed] [Google Scholar]
- 18.Pittard WB, III. Well-child care in infancy and healthcare services utilization from birth to 6 years by late preterm children receiving Medicaid benefits. South Med J. 2013;106(2):173–179 [DOI] [PubMed] [Google Scholar]
- 19.Tom JO, Tseng CW, Davis J, Solomon C, Zhou C, Mangione-Smith R. Missed well-child care visits, low continuity of care, and risk of ambulatory care-sensitive hospitalizations in young children. Arch Pediatr Adolesc Med. 2010;164(11):1052–1058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mitchell JM, Gaskin DJ, Kozma C. Health supervision visits among SSI-eligible children in the D.C. Medicaid program: a comparison of enrollees in fee-for-service and partially capitated managed care. Inquiry. 2008;45(2):198–214 [DOI] [PubMed] [Google Scholar]
- 21.Olson LM, Tang SF, Newacheck PW. Children in the United States with discontinuous health insurance coverage. N Engl J Med. 2005;353(4):382–391 [DOI] [PubMed] [Google Scholar]
- 22.Hakim RB, Ronsaville DS. Effect of compliance with health supervision guidelines among US infants on emergency department visits. Arch Pediatr Adolesc Med. 2002;156(10):1015–1020 [DOI] [PubMed] [Google Scholar]
- 23.Yu SM, Bellamy HA, Kogan MD, Dunbar JL, Schwalberg RH, Schuster MA. Factors that influence receipt of recommended preventive pediatric health and dental care. Pediatrics. 2002;110(6). Available at: www.pediatrics.org/cgi/content/full/110/6/e73 [DOI] [PubMed] [Google Scholar]
- 24.Hakim RB, Bye BV. Effectiveness of compliance with pediatric preventive care guidelines among Medicaid beneficiaries. Pediatrics. 2001;108(1):90–97 [DOI] [PubMed] [Google Scholar]
- 25.Ronsaville DS, Hakim RB. Well child care in the United States: racial differences in compliance with guidelines. Am J Public Health. 2000;90(9):1436–1443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Freed GL, Clark SJ, Pathman DE, Schectman R. Influences on the receipt of well-child visits in the first two years of life. Pediatrics. 1999;103(4 pt 2):864–869 [PubMed] [Google Scholar]
- 27.Byrd RS, Hoekelman RA, Auinger P, American Academy of Pediatrics . Adherence to AAP guidelines for well-child care under managed care. Pediatrics. 1999;104(3 pt 1):536–540 [DOI] [PubMed] [Google Scholar]
- 28.Mangione-Smith R, DeCristofaro AH, Setodji CM, et al. The quality of ambulatory care delivered to children in the United States. N Engl J Med. 2007;357(15):1515–1523 [DOI] [PubMed] [Google Scholar]
- 29.Chung PJ, Lee TC, Morrison JL, Schuster MA. Preventive care for children in the United States: quality and barriers. Annu Rev Public Health. 2006;27:491–515 [DOI] [PubMed] [Google Scholar]
- 30.Hambidge SJ, Phibbs SL, Chandramouli V, Fairclough D, Steiner JF. A stepped intervention increases well-child care and immunization rates in a disadvantaged population. Pediatrics. 2009;124(2):455–464 [DOI] [PubMed] [Google Scholar]
- 31.Schempf AH, Minkovitz CS, Strobino DM, Guyer B. Parental satisfaction with early pediatric care and immunization of young children: the mediating role of age-appropriate well-child care utilization. Arch Pediatr Adolesc Med. 2007;161(1):50–56 [DOI] [PubMed] [Google Scholar]
- 32.Bordley WC, Margolis PA, Lannon CM. The delivery of immunizations and other preventive services in private practices. Pediatrics. 1996;97(4):467–473 [PubMed] [Google Scholar]
- 33.Rodewald LE, Szilagyi PG, Shiuh T, Humiston SG, LeBaron C, Hall CB. Is underimmunization a marker for insufficient utilization of preventive and primary care? Arch Pediatr Adolesc Med. 1995;149(4):393–397 [DOI] [PubMed] [Google Scholar]
- 34.Pennsylvania's Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) Program Age Range Requirements for Screening Visits Desk Guide. Available at: www.keystonefirstpa.com/pdf/provider/resources/epsdt/desk-guide.pdf. Accessed April 4, 2014
- 35.EPIC. Choosing what fits or have it all. 2012. Available at: www.epic.com/software-ambulatory.php. Accessed April 4, 2014
- 36.Bice TW, Boxerman SB. A quantitative measure of continuity of care. Med Care. 1977;15(4):347–349 [DOI] [PubMed] [Google Scholar]
- 37.Wade KC, Lorch SA, Bakewell-Sachs S, Medoff-Cooper B, Silber JH, Escobar GJ. Pediatric care for preterm infants after NICU discharge: high number of office visits and prescription medications. J Perinatol. 2008;28(10):696–701 [DOI] [PubMed] [Google Scholar]
- 38.Ray KN, Escobar GJ, Lorch SA. Premature infants born to adolescent mothers: health care utilization after initial discharge. Acad Pediatr. 2010;10(5):302–308 [DOI] [PubMed] [Google Scholar]
- 39.American Academy of Pediatrics Committee on Environmental Health . Lead exposure in children: prevention, detection, and management. Pediatrics. 2005;116(4):1036–1046 [DOI] [PubMed] [Google Scholar]
- 40.Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. 2014;43(3):962–970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.National Committee for Quality Assurance. The state of health care quality 2014. October 2014. Available at: www.ncqa.org/Portals/0/Newsroom/2014/SOHC-web.pdf. Accessed April 17, 2015
- 42.Steiner JF, Braun PA, Melinkovich P, et al. Primary-care visits and hospitalizations for ambulatory-care-sensitive conditions in an inner-city health care system. Ambul Pediatr. 2003;3(6):324–328 [DOI] [PubMed] [Google Scholar]
- 43.Gadomski A, Jenkins P, Nichols M. Impact of a Medicaid primary care provider and preventive care on pediatric hospitalization. Pediatrics. 1998;101(3). Available at: www.pediatrics.org/cgi/content/full/101/3/E1 [DOI] [PubMed] [Google Scholar]
- 44.Department of Health and Human Services. Office of Inspector General. Most Medicaid children in nine states are not receiving all required preventive screening services. OEI-05–08–00520, May 2010. Available at: http://oig.hhs.gov/oei/reports/oei-05-08-00520.pdf. Accessed December 19, 2014
- 45.O’Malley AS. Current evidence on the impact of continuity of care. Curr Opin Pediatr. 2004;16(6):693–699 [DOI] [PubMed] [Google Scholar]
- 46.Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics. 2001;107(3):524–529 [DOI] [PubMed] [Google Scholar]
- 47.Cabana MD, Jee SH. Does continuity of care improve patient outcomes? J Fam Pract. 2004;53(12):974–980 [PubMed] [Google Scholar]
- 48.Brousseau DC, Meurer JR, Isenberg ML, Kuhn EM, Gorelick MH. Association between infant continuity of care and pediatric emergency department utilization. Pediatrics. 2004;113(4):738–741 [DOI] [PubMed] [Google Scholar]
- 49.Mainous AG, III, Gill JM. The importance of continuity of care in the likelihood of future hospitalization: is site of care equivalent to a primary clinician? Am J Public Health. 1998;88(10):1539–1541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Inkelas M, Newacheck PW, Olson LM, Zuckerman B, Schuster MA. Does having a regular primary care clinician improve quality of preventive care for young children? Med Care. 2008;46(3):323–330 [DOI] [PubMed] [Google Scholar]
- 51.Flores AI, Bilker WB, Alessandrini EA. Effects of continuity of care in infancy on receipt of lead, anemia, and tuberculosis screening. Pediatrics. 2008;121(3). Available at: www.pediatrics.org/cgi/content/full/121/3/e399 [DOI] [PubMed] [Google Scholar]
- 52.Van Cleave J, Davis MM. Preventive care utilization among children with and without special health care needs: associations with unmet need. Ambul Pediatr. 2008;8(5):305–311 [DOI] [PubMed] [Google Scholar]
- 53.American Academy of Pediatrics Committee on Fetus and Newborn . Hospital discharge of the high-risk neonate. Pediatrics. 2008;122(5):1119–1126 [DOI] [PubMed] [Google Scholar]
- 54.Patterson BL, Gregg WM, Biggers C, Barkin S. Improving delivery of EPSDT well-child care at acute visits in an academic pediatric practice. Pediatrics. 2012;130(4). Available at: www.pediatrics.org/cgi/content/full/130/4/e988 [DOI] [PMC free article] [PubMed] [Google Scholar]