Abstract
OBJECTIVE:
To determine whether subsequent births after short and long interpregnancy intervals (IPIs) are associated with risk of autism spectrum disorder (ASD).
METHOD:
We assessed the association between IPI and ASD risk in a cohort of 45 261 children born at Kaiser Permanente Northern California (KPNC) between 2000 and 2009. Children with ASD were identified from International Classification of Diseases, Revision 9 diagnostic codes 299.0, 299.8, and 299.9 recorded in KPNC electronic medical records. IPI was defined as the time from the birth of the first child to the conception of the second child. Survival analysis and logistic regression models were used to evaluate the association between IPI and risk of ASD in second-born children.
RESULTS:
Children born after an IPI of <12 months or ≥72 months had a 2- to 3-fold increased ASD risk compared with children born after an interval of 36 to 47 months. Respective adjusted hazard ratios (95% confidence intervals) were as follows: <6 months, 3.0 (1.9–4.7); 6 to 8 months, 2.1 (1.4–3.3); 9 to 11 months, 1.9 (1.3–2.1); 12 to 23 months, 1.5 (1.1–2.1); and ≥72 months, 2.4 (1.5–3.7). The results are not explained by maternal BMI or change in BMI between pregnancies or by parental age, maternal antidepressant medication use, or unfavorable events occurring during the first or second pregnancy.
CONCLUSIONS:
Children born after interpregnancy intervals <2 years or >6 years may be at increased risk of ASD. The mechanism explaining this association is unknown, and more research is needed.
What’s Known on This Subject:
Both short and long interpregnancy intervals are associated with increased risk of autism in second-born children. However, it is not known if the association is explained by unfavorable birth outcomes of the previous siblings.
What This Study Adds:
Both short and long interpregnancy intervals increase risk of autism in second-born children independently of previous siblings being born premature, having low birth weight, or being born by cesarean delivery and independently of maternal antidepressant use 3 months before pregnancy.
Interpregnancy interval (IPI), defined as the time between the birth date of one child and conception of the subsequent child, has been reported to influence both pregnancy and child outcomes. Several studies have associated both short and long IPIs with increased risk of adverse perinatal outcomes, including low birth weight, small for gestational age, preterm birth, neonatal death, and stillbirth.1–7 A few studies have reported increased risk with only short5 or long8 IPIs.
Short IPIs have also been reported to increase the risk of psychiatric and neurodevelopmental disorders. A registry-based study from Sweden reported a 3-fold increased risk of schizophrenia in individuals who were conceived 6 months after the birth of a sibling compared with 12 to 24 months.9 An analysis of the Danish psychiatric registry data also found an increased risk of schizophrenia associated with an interbirth interval of <26 months (corresponding to an IPI of ∼18 months) compared with an interbirth interval of ≥45 months (or an IPI ≥31 months).10
Autism spectrum disorder (ASD) is a neurodevelopmental condition with unknown cause for the vast majority of cases. Both genetic and environmental factors are recognized to play a role in its etiology.11,12 A number of previous studies reported associations between pre-, peri-, and neonatal factors and risk of ASD.13–15 However, very few studies have investigated the relationship between IPI and ASD. Two studies reported an association between short IPI and increased risk of ASD,16,17 whereas 2 others found an increased risk of ASD associated with both short and long IPIs.18,19
The objective of the current study is to further investigate the association between IPI and ASD and expand on previous studies by controlling for additional potential confounding factors, including maternal use of antidepressant medication before pregnancy, prepregnancy BMI, and change in BMI between the first and second pregnancies, as well as unfavorable outcomes of the first pregnancy. Furthermore, we explored whether the association was affected by intermediate factors, including low birth weight and preterm birth status of the second-born child.
Methods
Study Population
The study population was drawn from the cohort of children born between January 1, 2000, and December 31, 2009 (n = 350 956) at Kaiser Permanente Northern California (KPNC), an integrated health-care delivery organization that provides health care to >3 million residents (∼25% to 30%) of the San Francisco and Sacramento metropolitan areas and surrounding counties. KPNC members are broadly representative of the local and statewide population in terms of sociodemographic characteristics, except for the extremes of income distribution.20 Eligibility was restricted to singleton children of known parity who were born at a gestational age of ≥24 weeks, who remained health plan members until at least 2 years of age, and who had a sibling born between 1990 and 2009 (n = 150 649). From this cohort, we excluded 50 036 children whose siblings were not born at KPNC, 16 659 whose siblings were not full siblings, and 32 640 whose birth order was >2. We additionally excluded 6053 children whose mother had an indication of pregnancy loss between the births of her first and second children (using information on the birth certificates of the first and second child) and children for whom data on gender, parental age, or race/ethnicity were missing. Our main analysis focused on second-born children whose older (firstborn) siblings did not have ASD (n = 44 383). A secondary analysis was conducted among second-born children whose firstborn full sibling had an ASD diagnosis (n = 878).
Identification of Siblings
All singleton siblings were identified by linking the cohort to the State of California vital statistics birth files by child’s first and last name, child’s date and place of birth, mother’s first and maiden name and date of birth, and father’s last name and date of birth. Children with matching information on both parents were considered full siblings.
Ascertainment of ASD
Children with ≥1 ASD diagnosis, defined according to International Classification of Diseases, Ninth Revision codes 299.0, 299.8, and 299.9 and recorded in the KPNC outpatient database as of December 31, 2013, were considered cases. To identify additional children with ASD who were born at KPNC but left the health plan before being diagnosed with ASD, we linked the study cohort to the California Department of Developmental Services (DDS) client databases. DDS operates a system of 21 regional centers that coordinate services for individuals with ASD, intellectual disability, and other developmental disabilities. DDS/regional center eligibility is determined and services are provided without regard to citizenship or financial status, thus capturing a wide range of socioeconomic levels and racial/ethnic groups. Children who appeared in the DDS Client Development Evaluation Form file as of December 31, 2012, and who were receiving services for ASD were also considered cases in secondary/sensitivity analyses.
Definition of IPI
Interpregnancy interval was defined as the time between the birth of the firstborn child and the conception of the second-born child. For each pair of consecutive siblings, the IPI was calculated as the number of elapsed days between the dates of birth of each child minus the gestational age (in days) of the second-born. Assuming 30 days in a month, IPI was categorized as follows: <6 months, 6 to 8 months, 9 to 11 months, 12 to 23 months, 24 to 35 months, 36 to 47 months, 48 to 59 months, 60 to 71 months, and ≥72 months. For the main analyses, the reference category was 36 to 47 months. To compare our findings with previous studies, we also ran an analysis redefining our reference category to be IPI ≥36 months.
Covariates
Information on several parental and infant characteristics was obtained from KPNC maternal prenatal and pediatric electronic medical records and state vital statistics databases and was used to adjust the measure of association between IPI and risk of ASD in multivariate analyses. The covariates included child gender, year of birth, maternal and paternal age at birth of the study child (<20, 20 to 24, 25 to 29, 30 to 34, and ≥35 years; continuous), maternal education (less than high school, high school, college, postgraduate, or unknown), maternal race/ethnicity (white, non-Hispanic; white, Hispanic; Black; Asian; or other), maternal place of birth (United States, Mexico, or other), maternal BMI (used as a continuous variable) based on second-trimester pregnancy weight and height measured during the α-fetoprotein screening, and maternal antidepressant use (serotonin-specific reuptake inhibitors and heterocyclic antidepressants dispensed at a KPNC pharmacy in the 3 months before the date of conception of the second child). These covariates have been previously reported to increase risk of ASD.21–29 Change in maternal BMI between the 2 consecutive pregnancies (a proxy for maternal weight retention), birth weight, type of delivery, gestational age, and ASD status of the first child were also included in our analysis because they could possibly influence the length of IPI. We also explored the effect of intermediate variables preterm birth, low birth weight, and mode of delivery of second-born child on the measure of association between IPI and ASD.
Data Analysis
To account for differential time of follow-up until an ASD diagnosis could be made, we used a Cox proportional hazards regression model to estimate the association between IPI and risk of ASD. The censoring date was the date of the first ASD diagnosis, or if no diagnosis, the date of last membership in the health plan or the end of the study period of December 31, 2013, whichever came first. In the multivariate analyses, we included parental age and child gender because parental age was associated with both IPI and risk of ASD. Although child gender was not associated with IPI, we included it in all analyses because of its strong association with ASD. We further adjusted the main results for maternal antidepressant use 3 months before the conception of the second-born child because of its possible association with IPI and ASD. Additionally, we conducted analyses restricting our sample to second-born children whose firstborn siblings were not low birth weight, not preterm birth, or not born by cesarean delivery because these factors can possibly increase the length of IPI between the birth of the first child and the conception of the second child.
As a sensitivity analysis, we conducted a multivariate logistic regression analysis excluding cases with only 1 ASD diagnosis. In a second sensitivity analysis, we included additional cases of ASD (n = 18) who were identified in the DDS client database as of December 31, 2012, but were not identified in KPNC databases because they left the health plan before being diagnosed. In a third sensitivity analysis that included 18 140 (40.9%) of the sibling pairs for whom information on maternal BMI was available for both pregnancies, we additionally adjusted the results for maternal BMI during the pregnancy of the second-born and change in maternal BMI between the first and second pregnancies. Finally, a secondary analysis was conducted among second-born children whose firstborn full siblings had an ASD diagnosis (n = 878). The study protocol was approved by the KPNC Institutional Review Board and the California State Committee for the Protection of Human Subjects.
Results
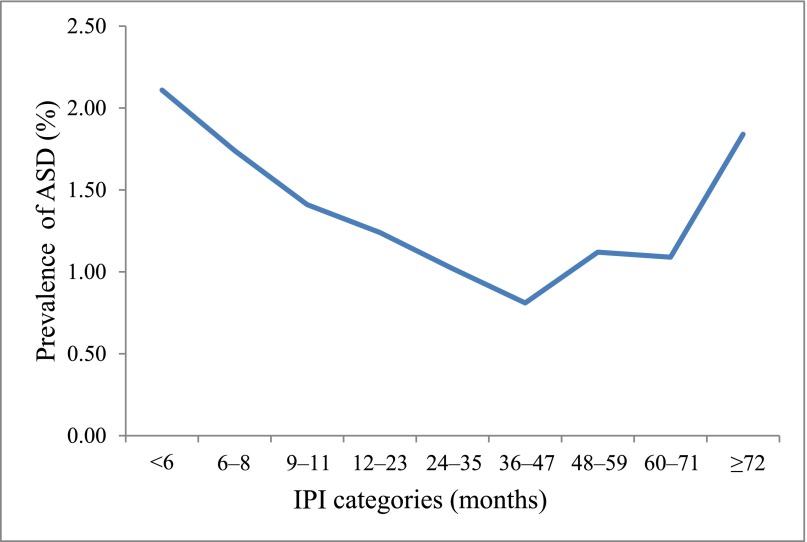
Of the 44 383 second-born children who had a firstborn full sibling without an ASD, 547 (1.2%) were diagnosed with an ASD by the end of the study period (377 autistic disorder, 117 Asperger’s disorder, and 53 pervasive developmental disorder not otherwise specified). There were no differences between second-born children with ASD and those without ASD with respect to maternal education, place of birth, or race/ethnicity. However, a higher proportion of children with ASD had mothers age ≥35 years and were born between 2000 and 2003 compared with children without ASD. The male-to-female ratio was much higher for those with ASD (4.6:1) than those without ASD (1:1). Children with ASD were more likely than children without ASD to be low birth weight and preterm (Table 1). The relationship between IPI and the prevalence of ASD in the second-born children approximated a U-shaped distribution, with the highest prevalence of ASD at both short (<6 months: 2.1%) and long (≥72 months: 1.8%) intervals (Fig 1).
TABLE 1.
Characteristics of Second-Born Children Whose Previous Full Sibling Did Not Have a Diagnosis of ASD: Kaiser Permanente Northern California Birth Cohort 2000 to 2009
| Characteristic | ASD (N = 547) n (%) | No ASD (N = 43 836) n (%) | Pa |
|---|---|---|---|
| Gender | <.0001 | ||
| Male | 450 (82.3) | 22 452 (51.2) | |
| Female | 97 (17.7) | 21 384 (48.8) | |
| Maternal age, years | .031 | ||
| <20 | 2 (0.4) | 262 (0.6) | |
| 20 to 24 | 67 (12.3) | 4670 (10.7) | |
| 25 to 29 | 141 (25.8) | 12 330 (28.1) | |
| 30 to 34 | 185 (33.8) | 16 533 (37.7) | |
| ≥35 | 152 (27.8) | 10 041 (22.9) | |
| Mean (SD) | 31.6 (5.2) | 31.3 (4.9) | .128 |
| Paternal age (years) | .095 | ||
| <20 | 0 | 64 (0.2) | |
| 20–24 | 30 (5.5) | 2176 (5.0) | |
| 25–29 | 83 (15.2) | 8607 (19.6) | |
| 30–34 | 195 (35.7) | 15 111 (34.5) | |
| ≥35 | 239 (43.7) | 17 878 (40.8) | |
| Mean (SD) | 34.6 (6.2) | 34.0 (5.9) | .020 |
| Maternal education | .920 | ||
| Less than high school | 21 (3.8) | 1844 (4.2) | |
| High school | 103 (18.8) | 8353 (19.1) | |
| College | 312 (57.0) | 24 208 (55.2) | |
| Postgraduate | 101 (18.5) | 8636 (19.7) | |
| Unknown | 10 (1.8) | 795 (1.8) | |
| Maternal race/ethnicity | .156 | ||
| White, non-Hispanic | 231 (42.2) | 19 993 (45.6) | |
| White, Hispanic | 118 (21.6) | 8733 (19.9) | |
| Black | 21 (3.8) | 1729 (3.9) | |
| Asian | 145 (26.5) | 10 125 (23.1) | |
| Other | 32 (5.9) | 3256 (7.4) | |
| Maternal place of birth | .484 | ||
| United States | 326 (59.6) | 27 153 (61.9) | |
| Mexico | 44 (8.0) | 3133 (7.2) | |
| Other | 177 (32.4) | 13 550 (30.9) | |
| Antidepressant use 3 mo before conception | 18 (3.3) | 920 (2.1) | .05 |
| Child birth year | .002 | ||
| 2000 to 2001 | 107 (19.6) | 7578 (17.3) | |
| 2002 to 2003 | 132 (24.1) | 8133 (18.6) | |
| 2004 to 2005 | 108 (19.7) | 8946 (20.4) | |
| 2006 to 2007 | 96 (17.6) | 9441 (21.5) | |
| 2008 to 2009 | 104 (19.0) | 9738 (22.2) | |
| Birth weight <2500 g | 26 (4.8) | 1210 (2.8) | .005 |
| Gestational age <37 wk | 42 (7.7) | 2167 (4.9) | .004 |
| Born by cesarian delivery | 129 (23.6) | 10 035 (22.9) | .700 |
Values are expressed as n (%) unless noted otherwise.
χ2 or t test.
FIGURE 1.
Prevalence of ASD in second-born children by IPI category: Kaiser Permanente Birth Cohort 2000 to 2009.
After adjustment for child gender and parental age, the risk of ASD was 1.5 to 3.0 times higher for IPIs <24 months and ≥72 months compared with an IPI of 36 to 47 months (Table 2). Of the 547 ASD cases, 36 had an ASD diagnosis recorded only once in their medical record. Excluding these 36 cases had no effect on the results (data not shown). To compare our findings with previous studies,16,17 we redefined the reference category as IPI ≥36 months. Results remained unchanged for IPIs <12 months (IPI <6 months, hazard ratio [HR] 2.3, 95% confidence interval [CI] 1.6–3.3; IPI 6 to 8 months, HR 1.6, 95% CI 1.1–2.3; IPI 9 to 11 months, HR 1.4, 95% CI 1.0–2.0; IPI 12 to 23 months, HR 1.1, 95% CI 0.9–1.4; and IPI 24 to 35 months, HR 0.9, 95% CI 0.7–1.2). Adjustment for maternal antidepressant use 3 months before the pregnancy of the second-born child did not affect the results (Table 2).
TABLE 2.
ASD in Second-Born Children Associated With IPI (months) After Firstborn Full Siblings Who Did Not Have ASD: Kaiser Permanente Northern California Births 2000 to 2009
| IPI, months | ASD (n = 547) n (%) | No ASD (n = 43 836) n (%) | HR (95% CI) | ||
|---|---|---|---|---|---|
| Crude | Adjusted, Model 1 | Adjusted, Model 2 | |||
| <6 | 37 (6.8) | 1546 (3.5) | 2.9 (1.8–4.4) | 3.0 (1.9–4.7) | 3.0 (2.0–4.7) |
| 6 to 8 | 37 (6.8) | 2297 (5.2) | 2.0 (1.3–3.0) | 2.1 (1.4–3.3) | 2.1 (1.4–3.3) |
| 9 to 11 | 51 (9.3) | 3419 (7.8) | 1.8 (1.2–2.8) | 1.9 (1.3–2.8) | 1.9 (1.3–2.9) |
| 12 to 23 | 192 (35.1) | 15 377 (35.1) | 1.5 (1.1–2.1) | 1.5 (1.1–2.1) | 1.5 (1.1–2.1) |
| 24 to 35 | 100 (18.3) | 9666 (22.1) | 1.2 (0.9–1.8) | 1.2 (0.9–1.7) | 1.2 (0.9–1.8) |
| 36 to 47 | 43 (7.9) | 5027 (11.5) | Reference | Reference | Reference |
| 48 to 59 | 32 (5.9) | 2899 (6.6) | 1.3 (0.8–2.0) | 1.3 (0.8–2.0) | 1.3 (0.8–2.0) |
| 60 to 71 | 17 (3.1) | 1566 (3.6) | 1.3 (0.7–2.3) | 1.3 (0.7–2.3) | 1.3 (0.7–2.3) |
| ≥72 | 38 (7.0) | 2039 (4.7) | 2.4 (1.6–3.7) | 2.4 (1.5–3.7) | 2.4 (1.5–3.7) |
Values are expressed as n (%). Model 1 adjusted for maternal age, paternal age, and child gender; model 2 adjusted for maternal age, paternal age, child gender and maternal use of antidepressants 3 months before the pregnancy of the second child.
When we restricted the analysis to second-born children whose firstborn full siblings had a birth weight ≥2500 g, were born at term (gestational age ≥37 weeks), or were born vaginally, short and long IPI remained associated with increased risk of ASD (Supplemental Table 4). Short and long IPI were associated with increased risk regardless of ASD subtype (data not shown). Controlling for the gestational age or birth weight of the second-born, which can be intermediate variables between IPI and ASD, did not affect the measure of association between IPI and ASD (Supplemental Table 5). In sensitivity analyses that included 18 additional ASD cases ascertained from the DDS client databases, findings were similar (Supplemental Table 6).
The pattern of association between ASD and IPI was unchanged after additional adjustment for maternal second-trimester BMI or change in maternal BMI between the first and second pregnancies among the subgroup for whom information on maternal BMI was available. Risk estimates ranged from 2.0 to 3.4 for IPI intervals <24 months and 2.6 to 4.4 for intervals >60 months (Supplemental Table 7). Finally, in a secondary analysis, we found a similar association trend between short and long IPI and ASD in second-born children whose firstborn full siblings were diagnosed with ASD (Table 3).
TABLE 3.
Association Between IPI and ASD in Second-Born Children After Firstborn Full Siblings Who Had a Diagnosis of ASD: Kaiser Permanente Northern California births 2000 to 2009.
| IPI, months | ASD (n = 111) n (%) | No ASD (n = 767) n (%) | HR (95% CI) | |
|---|---|---|---|---|
| Crude | Adjusted | |||
| <24 | 65 (58.6) | 392 (51.1) | 1.4 (1.0–2.1) | 1.5 (1.0–2.2) |
| 24 to 71 | 40 (36.0) | 353 (46.0) | Reference | Reference |
| ≥72 | 6 (5.4) | 22 (2.9) | 2.2 (1.0–5.2) | 1.7 (0.7–3.9) |
Values are expressed as n (%). HR adjusted for maternal age, paternal age, and child gender.
Discussion
Our results of a U-shaped association between IPI and risk of ASD are similar to 2 recent studies that reported increased risk of ASD associated with both short and long IPI.18,19 In a case control study including 2208 second-born children with ASD and 5163 matched controls identified from the Finnish Medical Birth Register, Cheslack-Postava et al reported that children born after IPIs of <12 or >60 months had a 28% to 50% increased risk of ASD.18 In a population-based case-cohort study that included 160 second-born children with ASD and 31 467 controls, Durkin et al found that children conceived after IPIs of <12 or >84 months were at ∼2-fold increased risk of ASD compared with those conceived between 24 and 47 months.19
Our finding of a >2-fold increased risk of ASD in second-born children associated with IPI <12 months is consistent with findings from 2 other previous studies.16,17 Our results are also consistent with those of another previous study showing a higher recurrence rate of ASD associated with short IPI.30 Our results show that the association between short or long IPI and ASD was not explained by unfavorable outcomes of the first pregnancy, including low birth weight, prematurity, or cesarean delivery. These factors could increase the length of time between the birth of the first child and the conception of the second child, and previous studies did not take them into account in their analyses, which could have affected their effect measures. In the current study, we also report that the association between IPI and risk of ASD in the second-born child is not explained by the ASD status of the firstborn child, which, to our knowledge, has not been previously reported.
Several biological mechanisms have been hypothesized to explain the link between short IPI and risk of ASD. A short interval between two pregnancies can cause maternal nutritional depletion when the mother’s body does not have enough time to recover from the physiologic stresses of the preceding pregnancy.16,31,32 One of the most important nutrients for healthy fetal development is folic acid, which plays an important role in neuronal development.33 During pregnancy, the demand for folic acid is increased because it is required for rapid cell proliferation of the uterus and the fetus. Thus, by the end of pregnancy, a woman may be at risk for folate deficiency.34 Low maternal folic acid intake in pregnancy has been associated with increased risk of ASD.35,36
High maternal BMI related to conception shortly after a previous birth has also been hypothesized to explain the link between short IPI and ASD risk. Both maternal obesity25 and gestational weight gain22 have been reported to moderately increase risk of ASD. If a woman has gained substantial weight during her first pregnancy, the probability of high BMI at the start of the second pregnancy after a short IPI will be high. However, in our study, the association between short IPI and risk of ASD was strengthened after controlling for maternal prepregnancy BMI and change in BMI between the first and second pregnancy. Ours results also show that the association between short and long IPI and ASD are not explained by maternal antidepressant use 3 months before the date of conception of the index child.
The interpretation of the association between long IPI and ASD is not straightforward. Infertility37 and advanced parental age24,28 can be associated with long IPI and are associated with increased risk of ASD. However, controlling for parental age had no effect on the relationship between IPI and ASD in the current study. Unfavorable events including cesarean delivery, low birth weight, or prematurity in the first pregnancy may lead some women to wait longer before getting pregnant with their second child. To account for these factors, we conducted analyses restricting the sample to second-born children whose firstborn siblings had none of these factors and found an increased risk of ASD associated with both long and short IPI. Thus, unfavorable events in the first pregnancy do not explain our current findings. Our results were also not explained by intermediate variables such as birth weight, gestational age, and cesarean delivery in the second-born child.
Our findings should be interpreted in light of several study limitations. ASD status was determined by diagnoses recorded in medical records and not validated by a standardized clinical assessment for all cases. However, record review and clinical validation studies have demonstrated that ≥90% of children with an ASD diagnosis recorded in the KPNC electronic databases have documentation consistent with a diagnosis of autism based on criteria from the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition.38 We were unable to control for several possible confounders, including infertility, maternal nutritional status (including folate and iron), breastfeeding, and maternal stress, which are factors that can either affect the IPI or be associated with risk of ASD. Inaccuracy related to the estimation of gestational age may have affected the calculation of IPI. Although we limited our analysis to sibling pairs with no indication of pregnancy loss between them, we were unable to account for early, unrecorded pregnancy losses that may have affected the estimated IPI. However, we do not expect any such inaccuracies to be related to a diagnosis of ASD. The present findings are strengthened by accurate linkage of child and mother by requiring that both firstborn and second-born children be health plan members. By using the Cox regression model, we were able to account for differential follow-up time. In addition, the large sample size allowed us to examine a greater number of shorter IPIs. Our study went beyond previous studies to control for maternal BMI and change in maternal BMI between the 2 index pregnancies, maternal medication use before the conception of the second-born, gestational age, birth weight, and type of delivery of the second-born child and found that these factors and the ASD status of the firstborn child did not explain the association between IPI and risk of ASD.
Conclusions
Our study confirms results from previous studies of an association between short and long IPI and risk of ASD. This association was not explained by maternal BMI, antidepressant medication use before pregnancy, or unfavorable events during the first or second pregnancy. Future studies incorporating data on maternal nutritional status, including folate and iron, and other potential explanatory factors such as infertility are needed to elucidate the mechanisms explaining this association.
Glossary
- ASD
autism spectrum disorders
- CI
confidence interval
- DDS
Department of Developmental Services
- HR
hazard ratio
- IPI
interpregnancy interval
- KPNC
Kaiser Permanente Northern California
Footnotes
Dr Zerbo conceptualized and designed the study and drafted the initial and final manuscript with substantial contribution from Dr Croen; Ms Yoshida conducted all the statistical analyses with input from Drs Croen and Zerbo; Drs Croen, Gunderson, and Dorward critically reviewed the manuscript and participated in the interpretation of findings; and all authors critically reviewed the manuscript and approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported in part by the Kaiser Foundation Research Institute and grant 3R01ES016669 from the National Institute of Environmental Health Sciences. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Conde-Agudelo A, Belizán JM, Norton MH, Rosas-Bermúdez A. Effect of the interpregnancy interval on perinatal outcomes in Latin America. Obstet Gynecol. 2005;106(2):359–366 [DOI] [PubMed] [Google Scholar]
- 2.Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta AC. Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. JAMA. 2006;295(15):1809–1823 [DOI] [PubMed] [Google Scholar]
- 3.DaVanzo J, Hale L, Razzaque A, Rahman M. Effects of interpregnancy interval and outcome of the preceding pregnancy on pregnancy outcomes in Matlab, Bangladesh. BJOG. 2007;114(9):1079–1087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grisaru-Granovsky S, Gordon ES, Haklai Z, Samueloff A, Schimmel MM. Effect of interpregnancy interval on adverse perinatal outcomes: a national study. Contraception. 2009;80(6):512–518 [DOI] [PubMed] [Google Scholar]
- 5.Shachar BZ, Lyell DJ. Interpregnancy interval and obstetrical complications. Obstet Gynecol Surv. 2012;67(9):584–596 [DOI] [PubMed] [Google Scholar]
- 6.Zhu BP. Effect of interpregnancy interval on birth outcomes: findings from three recent US studies. Int J Gynaecol Obstet. 2005;89(Suppl 1):S25–S33 [DOI] [PubMed] [Google Scholar]
- 7.Zhu BP, Rolfs RT, Nangle BE, Horan JM. Effect of the interval between pregnancies on perinatal outcomes. N Engl J Med. 1999;340(8):589–594 [DOI] [PubMed] [Google Scholar]
- 8.Stephansson O, Dickman PW, Cnattingius S. The influence of interpregnancy interval on the subsequent risk of stillbirth and early neonatal death. Obstet Gynecol. 2003;102(1):101–108 [DOI] [PubMed] [Google Scholar]
- 9.Gunawardana L, Smith GD, Zammit S, et al. Pre-conception inter-pregnancy interval and risk of schizophrenia. Br J Psychiatry. 2011;199(4):338–339 [DOI] [PubMed] [Google Scholar]
- 10.Smits L, Pedersen C, Mortensen P, van Os J. Association between short birth intervals and schizophrenia in the offspring. Schizophr Res. 2004;70(1):49–56 [DOI] [PubMed] [Google Scholar]
- 11.Colvert E, Tick B, McEwen F, et al. Heritability of autism spectrum disorder in a UK population-based twin sample. JAMA Psychiatry. 2015;72(5):415–423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hallmayer J, Glasson EJ, Bower C, et al. On the twin risk in autism. Am J Hum Genet. 2002;71(4):941–946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gardener H, Spiegelman D, Buka SL. Prenatal risk factors for autism: comprehensive meta-analysis. Br J Psychiatry. 2009;195(1):7–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guinchat V, Thorsen P, Laurent C, Cans C, Bodeau N, Cohen D. Pre-, peri- and neonatal risk factors for autism. Acta Obstet Gynecol Scand. 2012;91(3):287–300 [DOI] [PubMed] [Google Scholar]
- 15.Kuzniewicz MW, Wi S, Qian Y, Walsh EM, Armstrong MA, Croen LA. Prevalence and neonatal factors associated with autism spectrum disorders in preterm infants. J Pediatr. 2014;164(1):20–25 [DOI] [PubMed] [Google Scholar]
- 16.Cheslack-Postava K, Liu K, Bearman PS. Closely spaced pregnancies are associated with increased odds of autism in California sibling births. Pediatrics. 2011;127(2). Available at: www.pediatrics.org/cgi/content/full/127/2/e246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gunnes N, Surén P, Bresnahan M, et al. Interpregnancy interval and risk of autistic disorder. Epidemiology. 2013;24(6):906–912 [DOI] [PubMed] [Google Scholar]
- 18.Cheslack-Postava K, Suominen A, Jokiranta E, Lehti V, McKeague IW, Sourander A, Brown AS. Increased risk of autism spectrum disorders at short and long interpregnancy intervals in Finland. J Am Acad Child Adolesc Psychiatry. 2014;53(10):1074–1081 [DOI] [PMC free article] [PubMed]
- 19.Durkin MS, DuBois LA, Maenner MJ. Inter-pregnancy intervals and the risk of autism spectrum disorder: results of a population-based study. J Autism Dev Disord. 2015;45(7):2056–2066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82(5):703–710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bilder D, Pinborough-Zimmerman J, Miller J, McMahon W. Prenatal, perinatal, and neonatal factors associated with autism spectrum disorders. Pediatrics. 2009;123(5). Available at: www.pediatrics.org/cgi/content/full/123/5/e1293 [DOI] [PubMed] [Google Scholar]
- 22.Bilder DA, Bakian AV, Viskochil J, et al. Maternal prenatal weight gain and autism spectrum disorders. Pediatrics. 2013;132(5). Available at: www.pediatrics.org/cgi/content/full/132/5/e1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Croen LA, Grether JK, Yoshida CK, Odouli R, Hendrick V. Antidepressant use during pregnancy and childhood autism spectrum disorders. Arch Gen Psychiatry. 2011;68(11):1104–1112 [DOI] [PubMed] [Google Scholar]
- 24.Croen LA, Najjar DV, Fireman B, Grether JK. Maternal and paternal age and risk of autism spectrum disorders. Arch Pediatr Adolesc Med. 2007;161(4):334–340 [DOI] [PubMed] [Google Scholar]
- 25.Krakowiak P, Walker CK, Bremer AA, et al. Maternal metabolic conditions and risk for autism and other neurodevelopmental disorders. Pediatrics. 2012;129(5). Available at: www.pediatrics.org/cgi/content/full/129/5/e1121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lehti V, Hinkka-Yli-Salomäki S, Cheslack-Postava K, Gissler M, Brown AS, Sourander A. Maternal socio-economic status based on occupation and autism spectrum disorders: A national case-control study [published online ahead of print March 3, 2015]. Nord J Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rai D, Lee BK, Dalman C, Golding J, Lewis G, Magnusson C. Parental depression, maternal antidepressant use during pregnancy, and risk of autism spectrum disorders: population based case-control study. BMJ. 2013;346:f2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shelton JF, Tancredi DJ, Hertz-Picciotto I. Independent and dependent contributions of advanced maternal and paternal ages to autism risk. Autism Res. 2010;3(1):30–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sun X, Allison C, Auyeung B, Baron-Cohen S, Brayne C. Parental concerns, socioeconomic status, and the risk of autism spectrum conditions in a population-based study. Res Dev Disabil. 2014;35(12):3678–3688 [DOI] [PubMed] [Google Scholar]
- 30.Risch N, Hoffmann TJ, Anderson M, Croen LA, Grether JK, Windham GC. Familial recurrence of autism spectrum disorder: evaluating genetic and environmental contributions. Am J Psychiatry. 2014;171(11):1206–1213 [DOI] [PubMed] [Google Scholar]
- 31.Conde-Agudelo A, Rosas-Bermudez A, Castaño F, Norton MH. Effects of birth spacing on maternal, perinatal, infant, and child health: a systematic review of causal mechanisms. Stud Fam Plann. 2012;43(2):93–114 [DOI] [PubMed] [Google Scholar]
- 32.van Eijsden M, Smits LJ, van der Wal MF, Bonsel GJ. Association between short interpregnancy intervals and term birth weight: the role of folate depletion. Am J Clin Nutr. 2008;88(1):147–153 [DOI] [PubMed] [Google Scholar]
- 33.Czeizel AE, Dudás I. Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med. 1992;327(26):1832–1835 [DOI] [PubMed] [Google Scholar]
- 34.Fekete K, Berti C, Trovato M, et al. Effect of folate intake on health outcomes in pregnancy: a systematic review and meta-analysis on birth weight, placental weight and length of gestation. Nutr J. 2012;11:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schmidt RJ, Hansen RL, Hartiala J, et al. Prenatal vitamins, one-carbon metabolism gene variants, and risk for autism. Epidemiology. 2011;22(4):476–485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schmidt RJ, Tancredi DJ, Krakowiak P, Hansen RL, Ozonoff S. Maternal intake of supplemental iron and risk of autism spectrum disorder. Am J Epidemiol. 2014;180(9):890–900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grether JK, Qian Y, Croughan MS, et al. Is infertility associated with childhood autism? J Autism Dev Disord. 2013;43(3):663–672 [DOI] [PubMed] [Google Scholar]
- 38.Croen LA, Matevia M, Yoshida CK, Grether JK. Maternal Rh D status, anti-D immune globulin exposure during pregnancy, and risk of autism spectrum disorders. Am J Obstet Gynecol. 2008;199(3):234.e1–e6 [DOI] [PubMed]