Abstract
OBJECTIVES:
This study examined the efficacy of emergency department (ED)-based brief interventions (BIs), delivered by a computer or therapist, with and without a post-ED session, on alcohol consumption and consequences over 12 months.
METHODS:
Patients (ages 14–20 years) screening positive for risky drinking were randomized to: BI (n = 277), therapist BI (n = 278), or control (n = 281). After the 3-month follow-up, participants were randomized to receive a post-ED BI session or control. Incorporating motivational interviewing, the BIs addressed alcohol consumption and consequences, including driving under the influence (DUI), and alcohol-related injury, as well as other concomitant drug use. The computer BI was an offline, Facebook-styled program.
RESULTS:
Among 4389 patients screened, 1054 patients reported risky drinking and 836 were enrolled in the randomized controlled trial. Regression models examined the main effects of the intervention conditions (versus control) and the interaction effects (ED condition × post-ED condition) on primary outcomes. The therapist and computer BIs significantly reduced consumption at 3 months, consequences at 3 and 12 months, and prescription drug use at 12 months; the computer BI reduced the frequency of DUI at 12 months; and the therapist BI reduced the frequency of alcohol-related injury at 12 months. The post-ED session reduced alcohol consequences at 6 months, benefiting those who had not received a BI in the ED.
CONCLUSIONS:
A single-session BI, delivered by a computer or therapist in the ED, shows promise for underage drinkers. Findings for the fully automated stand-alone computer BI are particularly appealing given the ease of future implementation.
What’s Known on This Subject:
Intervention strategies are needed to reduce underage drinking. Meta-analyses of youth alcohol brief interventions (BIs) conclude that therapist-delivered BIs are efficacious; however, to maximize public health impact, recommendations include using technology to streamline intervention delivery, for which evidence is lacking.
What This Study Adds:
A single-session BI, delivered by a computer or therapist in the emergency department, shows promise for underage drinkers. Findings for the stand-alone computer BI are particularly appealing given the ease of future implementation.
Early intervention strategies are needed to reduce underage drinking, with 16% of individuals aged 15 to 16 years1 and 19% of those aged 17 to 18 years2 reporting binge drinking. Alcohol use during adolescence increases the risk for developing an alcohol use disorder,3,4 which occurs in ∼5% of adolescents (ages 12–17 years) and ∼16% of emerging adults (ages 18–25 years).3,5,6 Additional risks of underage drinking include driving under the influence (DUI) of alcohol, with 6% of adolescents (ages 16–17 years) and 15% of emerging adults (ages 18–20 years) reporting past year DUI.7 This finding is especially alarming because youth are more likely than adult populations to have a DUI-associated motor vehicle crash,8 increasing their risk for mortality.9 Alcohol misuse during adolescence is also associated with illicit drug use10–21 and misuse of prescription medications (eg, opioids, sedatives, stimulants),19,22 thus increasing the risk for overdose, which is an escalating public health problem.15,18,23–25
Alcohol screening, brief intervention, and referral to treatment (SBIRT) approaches have largely been tested among adults in the emergency department (ED), with meta-analyses demonstrating a reduction in consequences but not consumption.26 However, a previous ED-based BI for underage drinking has also shown promise by reducing alcohol-related consequences (ie, injury, DUI) and binge drinking.27 Recent meta-analyses of youth alcohol brief interventions (BIs; up to age 25 years)28,29 across settings (eg, ED, colleges) concluded that therapist-delivered BIs are efficacious.
Although the American Academy of Pediatrics30 and the American College of Emergency Physicians,31 as well as government agencies (ie, National Institute on Alcohol Abuse and Alcoholism, Substance Abuse and Mental Health Services Administration),32 endorse alcohol SBIRT for youth in the ED, implementation of therapist-delivered BIs is limited by lack of staff time and training.33,34 To maximize the public health impact, recommendations include using technology to streamline screening and intervention delivery in the ED35,36; however, an evidenced-based, computerized alcohol BI for underage risky drinkers is currently lacking. Furthermore, a single-session BI may not be sufficient to sustain long-term changes given the cyclical nature of alcohol use among youth.35,37–39 Despite recommendations that SBIRT methods in the ED include boosters to enhance efficacy, evidence for their benefits are mixed and require further evaluation.
The present study examined: (1) the efficacy of an alcohol BI (Project U-Connect), delivered by computer or therapist, in reducing primary outcomes of alcohol consumption and consequences and secondary outcomes of DUI, alcohol-related injury, and illicit and prescription drug use, compared with control condition at 3, 6, and 12 months; (2) the efficacy of a 3-month post-ED brief session on outcomes at 6 and 12 months; and (3) the most effective combination of ED-based and post-ED intervention strategy on outcomes at 6 and 12 months.
Methods
Design
Project U-Connect was a randomized controlled trial conducted among underage drinkers presenting to an academic Level 1 ED.40 Using a 3 × 2 factorial design, eligible participants were randomized by using a computerized algorithm to 1 of 3 ED-based conditions (computer BI, therapist BI, or control) and 1 of 2 booster conditions (post-ED session or control) that were administered after the 3-month follow-up interview. We obtained Institutional Review Board Approval from the University of Michigan and a certificate of confidentiality was obtained from the National Institutes of Health.
Protocol
Recruitment occurred between ∼2 pm and 2 am 7 days a week, excluding holidays (September 2010–March 2013); initial sampling of midnight and day shifts was reduced due to low yield. ED patients (ages 14–20 years) were identified for screening by review of electronic medical records. Patients were ineligible if they could not provide informed consent (eg, medical reasons [eg, intubated, unconscious], psychiatric reasons [ie, cognitive impairment], aged <18 years without a parent/guardian present), had acute suicidal ideation or had experienced sexual assault, or could not self-administer the assessment/BI (eg, non–English-speaking [3.1%]) or participate in follow-ups (eg, homeless). Patients who were not stable to be approached in the ED were enrolled on inpatient floors within 72 hours (2.1%). Participants provided written consent (or assent and parent/guardian consent if aged <18 years) to be screened, self-administered the 15- to 20-minute survey via touchscreen tablet, and received a $1.00 gift.
Eligibility
Participants screening positive on the Alcohol Use Disorders Identification Test– Consumption41,42 (AUDIT-C; age 14–17 years, score ≥3; age 18–20 years, score ≥4)43,44 were eligible for the randomized controlled trial. After provision of written consent (age ≥18 years) or assent and parent/guardian consent (ages 14–17 years), participants self-administered a 20- to 30-minute computerized baseline survey ($20 compensation) and were randomized to a condition, stratified according to gender, age (14–17 or 18–20 years), and meeting criteria for an alcohol use disorder (see Measures).
Follow-up assessments at 3, 6, and 12 months were self-administered by participants either on a computer that was provided by staff in-person or via a Web link that was sent to participants to self-administer online. Remuneration was $35 for 3-month follow-ups, $35 for 6-month follow-ups, and $45 for 12-month follow-ups.
Measures
Demographics
Questions regarding demographic characteristics and background included age, gender, race, ethnicity, receipt of public assistance, and living situation.45–47
Risky Drinking
Participants reporting alcohol use in the past year (Add Health instrument)47 self-administered the AUDIT-C.41,42
Primary Outcomes
Alcohol Consumption Index
Responses from the past 3-month frequency variable (“How often did you have a drink containing alcohol?”: never = 0; monthly or less = 1; 2 to 4 times per month = 2; 2 to 3 times per week = 3; ≥4 times per week = 4) and the past 3-month quantity variable (How many drinks containing alcohol did you have on a typical day when you were drinking?”: 1 or 2 drinks = 1; 3 or 4 = 2; 5 or 6 = 3; 7 to 9 = 4; ≥10 = 5) of the AUDIT-C were multiplied to produce a quantity-frequency index.48 Scores ranged from 0 to 20, with higher scores indicating greater alcohol consumption.
Alcohol Consequences
The 18-item Rutgers Alcohol Problem Index assessed past 3-month alcohol-related consequences.49–51 Responses were scored dichotomously and summed (range: 0–18)51; previous research found that scores ≥8 indicate an alcohol use disorder.51
Secondary Outcomes
Driving Under the Influence
The 5-item Young Adult Driving Questions52–55 assessed past 3-month drinking and driving, with responses summed.
Alcohol-Related Injury
A question from the Adolescent Injury Checklist evaluated past 12-month alcohol-related injury.53,56,57
Drug Use
The National Institute on Drug Abuse Alcohol, Smoking, and Substance Involvement Screening Test58,59 assessed use and consequences of 6 illicit drugs (ie, marijuana, cocaine, inhalants, hallucinogens, methamphetamine, street opioids) and the nonmedical use and consequences of 3 prescription drugs (ie, opioids, sedatives, stimulants) (range per drug: 0–39).
Conditions
Computer- and Therapist-Delivered BIs
The computer BI and therapist BI incorporated principles of motivational interviewing60 to primarily address alcohol use61–63 (see Walton et al40 for additional information on intervention content). Although the modes of delivery for these 2 interventions were different (which affected some specific content included), they were designed to be parallel in structure with similar key components addressed. The tailored computer BI was an offline, Facebook-styled program (Supplemental Appendix) delivered by using touchscreen tablets with audio (via headphones). Participants chose a top “friend” to guide them and 6 virtual “friends.” Sections included: (1) reasons to avoid drinking and drugs, including prescription drugs; (2) benefits of drinking less or not drinking (ie, avoiding injury); (3) better things to do; (4) risky situations; (5) protective behavioral strategies; (6) handling negative affect (eg, chat room–style posts followed by comments expressed by virtual friends, YouTube-styled videos); and (7) avoiding DUIs (ie, zero tolerance laws, peer video sharing difficulties after a DUI). Therapist BIs were facilitated by a computerized workbook for real-time clinical decision support at each step, presenting tailored feedback and screens to prompt content. Therapists elicited change talk about alcohol and drug consequences, reasons to avoid or reduce use and combining alcohol and prescription drugs, benefits of change, building discrepancy between actions and goals, risky situations, protective behavioral strategies,64 handling negative affect, and preventing consequences (eg, injury, DUI). Therapist BI sessions were coded (97.3% [n = 249]) by using the Motivational Interviewing Treatment Integrity 3.0 system,65 with data demonstrating acceptable fidelity (mean global spirit rating: 4.6 [SD: 0.6; range: 2.7–5.0], which exceeds the competency of 4).40
Control
Considered enhanced usual care, the control condition comprised staff reviewing a brochure listing resources (eg, mental health and substance use services, leisure activities). This brochure was also given to participants in the intervention conditions.
Post-ED Session
After the 3-month follow-up data collection, the booster condition assignment was revealed on the computer, and youth received either a BI delivered by a therapist blinded to ED condition assignment or no BI (control). The post-ED session was based on motivational interviewing60 (mean: 39.7 ± 12.9 minutes). Post-ED sessions were audiotaped and coded using the Motivational Interviewing Treatment Integrity 3.0 system65; among randomly selected sessions (51% [n = 70]), the mean global spirit rating was 4.8 (SD: 0.3; range: 4.0–5.0), which exceeds the competency level of 4. Sessions addressed alcohol use, other drug use (as appropriate), and other risky behaviors (eg, injury, DUI) based on responses to the 3-month follow-up. Therapists used touchscreen tablets to guide the session and provide tailored feedback for substance use and consequences.
Data Analysis
Data were analyzed by using SAS version 9.4 (SAS Institute, Inc, Cary, NC). No statistically significant differences were found in baseline characteristics according to condition. Nonetheless, analyses controlled for randomization strata (gender; age group [14–17 years or 18–20 years]); we did not control for meeting criteria for an alcohol use disorder because it was strongly correlated with outcomes. Sample size was determined a priori based on expected effect sizes. Although 80% to 90% received the assigned conditions, an intent-to-treat approach was used (eg, includes those who did not receive assigned condition). Attrition analyses showed that baseline characteristics (ie, age group, gender) were not significantly related to follow-up completion, suggesting data were missing at random. Thus, analyses included all available cases at follow-ups, which is preferred to imputation when data are missing at random and attrition is low (ie, the follow-up rate was 86.8% at 3 months, 87.1% at 6 months, and 88.0% at 12 months). White participants were less likely than participants of other races to complete the 3-month follow-up, and male participants were less likely than female participants to complete the 12-month follow-up; however, models including race did not change the findings (data available on request). Overall, regression analyses (ie, negative binominal or Poisson based on distribution) were conducted for interventions (compared with the control) on primary outcomes (ie, alcohol consumption index, alcohol consequences) at 3, 6, and 12 months. First, to determine the most effective ED-based strategy compared with control condition, regression analyses were conducted for 3-month outcomes, controlling for baseline alcohol variables. Second, to examine the main effects of the post-ED session, regression models were conducted for 6-month outcomes, controlling for 3-month alcohol variables. Third, to examine long-term main effects of the therapist BI, computer BI, and post-ED session, regression models were conducted for 12-month outcomes, controlling for baseline alcohol variables. Fourth, to determine the most effective combination, regression models were conducted, including interaction effects for ED condition by post-ED condition on outcomes controlling for baseline alcohol variables. Finally, main effects and interaction effects on secondary outcomes were examined at 12 months (ie, illicit drug use, prescription drug use, DUI, and alcohol-related injury [not measured at 3 or 6 months]). For DUI, alcohol-related injury, and prescription drug use, zero-inflated models were used to account for the large proportion of zeros.
Results
Enrollment
A total of 9228 patients (aged 14–20 years) presented to the ED during recruitment hours. Of the 5096 who were approached, 86.1% were screened (n = 4389) and 13.9% (n = 707) refused (Fig 1). At screening, male participants were more likely to refuse than female participants (15.1% and 13.0%, respectively; χ2 [1] = 4.76; P < .05) and participants of other races were more likely to refuse than white participants and African-American participants (35.0% vs 9.6% and 7.7%, respectively; χ2 [2] = 393.20; P < .001). Of those screened, 24% (n = 1054) met the criteria for risky drinking, and 79.3% (n = 836) were enrolled in the randomized controlled trial. At baseline, white participants and participants of other races were more likely to refuse than African-American participants (17.7% and 19.5% vs 3.7%, respectively; χ2 [2] = 11.02; P < .01). Compliance with assigned conditions and follow-ups exceeded 80%.
FIGURE 1.
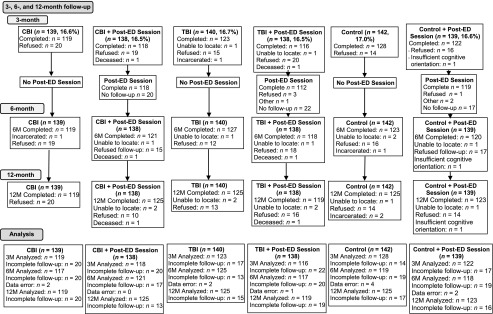
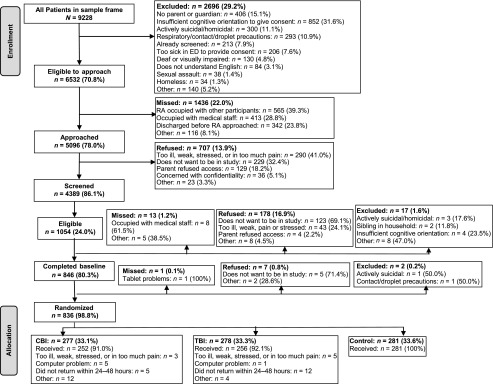
Project U-Connect flow sheet. CBI = computer BI; M = months; RA = research assistant; TBI = therapist BI.
Participant Characteristics
No significant differences were found in participant characteristics (gender, age group, race, ethnicity, receipt of public assistance, living with parents, ED visit characteristics of seeking care for injury, alcohol-related ED visit, discharge from ED, or baseline alcohol consumption, consequences, DUI, alcohol-related injury, or drug use) according to condition. Overall, 51.6% of participants were male, with a mean age of 18.6 ± 1.4 years, and 65.8% were currently in college. Most participants were white (79.4%), with 9.5% African-American and 11.1% other races; 5.5% were of Hispanic ethnicity. Only 20.1% received public assistance; 43.3% lived with their parents. About two-thirds (63.8%) presented with a medical complaint, and most youth were discharged from the ED (86.8%).
Three-Month Primary Outcomes
Regression analyses showed that the computer BI and therapist BI significantly decreased the alcohol consumption index score and alcohol consequences compared with control (Table 1). Cohen’s d effect sizes were as follows: alcohol consumption index, 0.10 (computer BI) and 0.13 (therapist BI); alcohol consequences, 0.11 (computer BI) and 0.14 (therapist BI).
TABLE 1.
Main Effects of Computer and Therapist BIs (Versus Control) on the Alcohol Consumption Index and Alcohol Consequences at 3-Month Follow-up
| Variable | 3-Month (N = 726) IRR (95% CI) | P |
|---|---|---|
| Alcohol consumption indexa | ||
| Computer BI | 0.88 (0.78–0.99) | .041 |
| Therapist BI | 0.86 (0.77– 0.98) | .018 |
| Alcohol consequencesb | ||
| Computer BI | 0.85 (0.76–0.95) | .004 |
| Therapist BI | 0.87 (0.79–0.97) | .014 |
The reference group is the control group. These models controlled for baseline values of the domain (ie, alcohol consumption index or alcohol consequences) and age group and gender.
Responses from the past 3-month frequency variable (“How often did you have a drink containing alcohol?”: never = 0; monthly or less = 1; 2–4 times per month = 2; 2–3 times per week = 3; ≥4 times per week = 4) and the past 3-month quantity variable (“How many drinks containing alcohol did you have on a typical day when you were drinking?”: 1 or 2 drinks = 1; 3 or 4 = 2; 5 or 6 = 3; 7 to 9 = 4; ≥10 = 5) of the AUDIT-C were multiplied to produce a quantity-frequency index. Scores ranged from 0 to 20, with higher scores indicating greater alcohol consumption.
The 18-item Rutgers Alcohol Problem Index assessed past 3-month alcohol-related consequences. Responses were scored dichotomously and summed (range: 0–18).
Six-Month Primary Outcomes: Main Effects
Regression models examining the main effects of the computer BI, therapist BI, and post-ED session on alcohol consumption index scores and consequences at 6 months (controlling for 3-month levels of alcohol domain) showed no significant effects for either of the BIs. The main effect of the post-ED session was significant for alcohol consequences but not for consumption (data not shown, Cohen’s d = 0.12).
Twelve-Month Primary Outcomes: Main Effects
At 12 months, the therapist BI and computer BI did not significantly affect alcohol consumption index scores but did reduce alcohol consequences (Cohen’s d effect sizes = 0.12 [therapist BI versus enhanced usual care] and 0.17 [computer BI versus enhanced usual care]) (Table 2). There were no main effects of the post-ED session on alcohol-related outcomes at 12 months.
TABLE 2.
Main Effects for the ED BIs and Post-ED Session on the Alcohol Consumption Index and Alcohol Consequences at 12 Months
| Variable | 12-Month (N = 735) IRR (95% CI) | P |
|---|---|---|
| Alcohol consumption index | ||
| Computer BI | 1.05 (0.92–1.20) | .478 |
| Therapist BI | 1.00 (0.88–1.15) | .956 |
| Post-ED session | 0.95 (0.86–1.06) | .393 |
| Alcohol consequences | ||
| Computer BI | 0.86 (0.75–0.98) | .024 |
| Therapist BI | 0.87 (0.76–0.98) | .029 |
| Post-ED session | 0.98 (0.88–1.09) | .726 |
The reference group is the control group. These models controlled for baseline values of the domain (ie, alcohol consumption index or alcohol consequences) and age group and gender.
Six- and 12-Month Primary Outcomes: Interaction Effects
At 6 months, among those receiving the control condition in the ED, those who received the post-ED session had fewer alcohol consequences (incidence rate ratio [IRR]: 0.84 [confidence interval (CI): 0.71–0.99]) than those who did not receive the post-ED session (Table 3). Among those receiving the therapist BI in the ED, those who received the post-ED session had more alcohol consequences (IRR: 1.33 [CI: 1.05–1.68]) than those who did not receive the post-ED session. At 12 months, among those receiving the control condition in the ED, those who received the post-ED session had fewer alcohol consequences (IRR: 0.73 [CI: 0.61–0.88]) than those who did not receive the post-ED session, and among those receiving the computer BI in the ED, those who received the post-ED session noted more alcohol consequences (IRR: 1.38 [CI: 1.06–1.79]) than those who did not receive the post-ED session.
TABLE 3.
Six- and 12-Month Interaction Effects to Examine the Most Effective Combination of ED and Post-ED Session
| Variable | 6-Month (N = 717) IRR (95% CI) | P | 12-Month (N = 735) IRR (95% CI) | P |
|---|---|---|---|---|
| Alcohol consumption indexa | ||||
| Computer BI | 0.93 (0.74–1.17) | .5422 | 0.97 (0.81–1.17) | .7431 |
| Therapist BI | 0.80 (0.64–1.01) | .0615 | 0.99 (0.82–1.18) | .8713 |
| Post-ED session | 0.86 (0.68–1.09) | .2041 | 0.89 (0.74–1.08) | .2367 |
| Computer BI * post-ED session | 1.16 (0.84–1.62) | .3670 | 1.17 (0.90–1.52) | .2441 |
| Therapist BI * post-ED session | 1.29 (0.93–1.80) | .1327 | 1.04 (0.80–1.35) | .7733 |
| Alcohol consequencesb | ||||
| Computer BI | 0.99 (0.85–1.17) | .9410 | 0.73 (0.61–0.88) | .0011 |
| Therapist BI | 0.90 (0.76–1.06) | .2044 | 0.86 (0.72–1.02) | .0792 |
| Post-ED session | 0.84 (0.71–0.99) | .0409 | 0.88 (0.74–1.05) | .1665 |
| Computer BI × post-ED session | 1.09 (0.86–1.39) | .4871 | 1.38 (1.06–1.79) | .0167 |
| Therapist BI × post-ED session | 1.33 (1.05–1.68) | .0199 | 1.02 (0.79–1.33) | .8594 |
The reference group is the control group. These models controlled for baseline values of the domain (ie, alcohol consumption index or alcohol consequences) and age group and gender.
Quantity-frequency index; higher scores indicate greater alcohol consumption.
The 18-item Rutgers Alcohol Problem Index assessed alcohol-related consequences.
Secondary Outcomes
The computer BI reduced the frequency of DUI (Cohen’s d = 0.13) and prescription drug use (Cohen d = 0.20) at 12 months. The therapist BI reduced alcohol-related injury (Cohen’s d = 0.22) and prescription drug use (Cohen’s d = 0.25) at 12 months (Table 4) compared with the control. No significant main effects were found for illicit drug use, and interaction effects (data not shown) were not significant for these secondary outcomes.
TABLE 4.
Main Effects for the ED-Based BIs and Post-ED Session on Secondary Outcomes at 12 Months
| Variable | IRR (95% CI) Prevalence | IRR (95% CI) Frequency | P Value Prevalence | P Value Frequency |
|---|---|---|---|---|
| Drinking and driving | ||||
| Computer BI | 0.53 (0.23–1.25) | 0.48 (0.29–0.80) | .147 | .005 |
| Therapist BI | 0.63 (0.28–1.41) | 0.69 (0.41–1.17) | .256 | .166 |
| Post-ED session | 0.80 (0.41–1.58) | 0.80 (0.52–1.21) | .527 | .286 |
| Alcohol-related injury | ||||
| Computer BI | 0.92 (0.26–3.24) | 0.63 (0.30–1.32) | .900 | .216 |
| Therapist BI | 0.87 (0.26–2.96) | 0.44 (0.22–0.92) | .828 | .028 |
| Post-ED session | 0.56 (0.16–1.95) | 0.71 (0.37–1.37) | .362 | .312 |
| Prescription drug use | ||||
| Computer BI | 0.83 (0.56–1.25) | 0.59 (0.52–0.66) | .376 | <.001 |
| Therapist BI | 1.16 (0.77–1.76) | 0.63 (0.56–0.70) | .474 | <.001 |
| Post-ED session | 1.14 (0.81–1.59) | 1.08 (0.98–1.19) | .453 | .103 |
| Estimate (SE) | P | |||
| Illicit drug use | ||||
| Computer BI | — | 0.96 (0.72–1.27) | — | .772 |
| Therapist BI | — | 0.96 (0.72–1.28) | — | .790 |
| Post ED session | — | 0.89 (0.71–1.12) | — | .330 |
The reference group is the control group. Zero-inflated negative binomial for DUI, zero-inflated Poisson for alcohol-related injury, zero-inflated Poisson for prescription drug use (and thus have both prevalence and frequency). A negative binomial was conducted for illicit drug use (thus only data in frequency columns is available). These models controlled for baseline values of the domain and the strata on which the participants were randomized (age group and gender). Illicit drug use includes marijuana, cocaine, inhalants, hallucinogens, methamphetamine, and street opioids.
Discussion
Our results provide novel data supporting the efficacy of brief, single-session alcohol interventions among youth in the ED, delivered by a therapist or a computer, in decreasing alcohol consumption index scores and alcohol-related consequences. Furthermore, the Project U-Connect BIs reduced DUI and/or alcohol-related injury. For example, youth receiving a BI experienced a ∼10% reduction in consequences (eg, arguments, physical or mental health problems due to drinking) at the 1-year follow-up. These findings, albeit modest, are clinically significant given that alcohol-related injury and DUI are leading causes of mortality and morbidity among youth9 and that drinking during adolescence is related to the development of alcohol use disorders as well as other psychosocial problems as adults.66–69 Importantly, reduction in prescription drug use (computer BI: ∼30%; therapist BI: ∼50%) among risky drinkers is clinically significant because the combination of alcohol and prescription drugs increases the risk for overdose and other negative health consequences.23
Findings supporting the efficacy of the stand-alone computer BI are particularly innovative and important. Although evidence-based, computerized, brief alcohol interventions are available for college students,70–74 no evidence-based interventions exist to date for underage youth in the ED who are risky drinkers. One prior ED study that was focused on youth with any alcohol use (instead of risky drinkers) tested a computerized alcohol BI and found efficacy among a subsample of youth reporting drinking and driving at baseline.75 Another study of a computerized BI also focused on the combination of youth violence and any alcohol found a reduction in alcohol consequences.76,77 Our therapist BI was guided by a computerized workbook guide for real-time clinical decision support that the therapist used to structure the session, which may increase fidelity in the busy ED setting.
Findings regarding the efficacy of BIs on reducing DUI and alcohol-related injury were mixed, with the computer BI reducing DUI and the therapist BI reducing alcohol-related injuries. These findings may reflect differences in the content based on delivery mechanism. For example, the computer BI contained a video clip in which a teen described financial and legal stresses after a DUI charge. In contrast, therapists had discretion to elicit alcohol-related consequences, such as injury.
The present study contributes to the literature by examining the efficacy of a post-ED session, with and without an initial ED-based BI. The post-ED session had minimal short-term benefits (at 6 months) for those who did not receive a BI in the ED; however, as indicated by the analysis of the interaction effects, this post-ED session did not enhance the efficacy of the Project U-Connect BI delivered by either the computer or the therapist in the ED. This finding is notable because >80% who were assigned actually received the post-ED session, addressing dose and retention issues that can occur with post-ED therapy delivery. Previous data on the efficacy of a follow-up booster are inconsistent, perhaps reflecting variation in participation and content.78–80
In terms of future translation and implementation, the Project U-Connect BI seems to be efficacious delivered by either a computer or a therapist, and a post-ED session at 3 months after the ED visit is of possible benefit for settings in which there is no staff mechanism to deliver the BI during the ED visit. Given resources required to re-contact youth and deliver a session postdischarge, administration of the BI in the ED seems preferable, although future studies could consider technology-based staff-free boosters. In particular, findings for the computer BI are promising because this delivery mode addresses barriers regarding staff time and training, with youth completing the intervention independently. Future examination of the costs for this intervention is needed to aid implementation decisions.
A limitation of the present study is that the findings may not be generalized to patient groups who were not included in this single-site study or to those excluded (eg, those with acute suicidal ideation); replication among larger, more diverse samples is necessary to examine all outcomes as well as the characteristics of responders/nonresponders. The use of self-report data is a potential limitation; however, recent reviews support their reliability and validity when privacy/confidentiality is assured and when self-administered, computerized assessments are used.81 In addition, despite follow-up rates exceeding 85% at 12 months, concerns regarding attrition cannot be completely eliminated.
Conclusions
A single-session BI delivered by a computer or therapist reduced risky drinking and alcohol consequences among these underage drinkers in the ED. A post-ED session added benefit for youth who did not receive a BI during the ED visit; however, no additional benefit of the booster was found after an ED-based BI. Although effect sizes were modest, findings for the stand-alone single-session, fully automated computer BI are particularly appealing given the ease of future implementation.
Acknowledgments
We acknowledge Wendi Mohl, BS, and Jessica Roche, MPH, for their assistance in manuscript preparation and Linping Duan, MS, for her assistance with statistical analysis. We also thank the patients and medical staff of the University of Michigan Emergency Department for their support of this project.
Glossary
- AUDIT-C
Alcohol Use Disorders Identification Test–Consumption
- BI
brief intervention
- CI
confidence interval
- DUI
driving under the influence
- ED
emergency department
- IRR
incidence rate ratio
- SBIRT
screening, brief intervention, and referral to treatment
Footnotes
Dr Cunningham was responsible for the study concept, design, acquisition, analysis, and interpretation of data; administrative, technical, or material support of the study; study supervision; and drafting of the manuscript, including both the initial draft and subsequent revisions. Dr Chermack was responsible for the study concept and design, study supervision, and critical revisions to the manuscript; Drs Ehrlich, Blow, and Barry were responsible for the study concept and design and critical revisions to the manuscript; Dr Carter was responsible for analysis and interpretation of data and critical revisions to the manuscript; and Dr Booth was responsible for the study concept, design, acquisition, analysis, and interpretation of data, as well as critical revisions to the manuscript. Dr Walton was responsible for the study concept, design, acquisition, analysis, and interpretation of data; administrative, technical, or material support of the study; study supervision; and critical revisions to the manuscript. All authors take responsibility for the integrity and accuracy for their contributions. Dr. Cunningham had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
This trial has been registered at www.clinicaltrials.gov (NCT01051141).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the National Institute on Alcohol Abuse and Alcoholism (grant 018122). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found on page e1002, online at www.pediatrics.org/cgi/doi/10.1542/peds.2015-2713.
References
- 1.Patrick ME, Schulenberg JE. Prevalence and predictors of adolescent alcohol use and binge drinking in the United States. Alcohol Res. 2013;35(2):193–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg J. Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings, 2014. Ann Arbor, MI: Institute for Social Research, the University of Michigan; 2015 [Google Scholar]
- 3.Grant BF. Prevalence and correlates of alcohol use and DSM-IV alcohol dependence in the United States: results of the National Longitudinal Alcohol Epidemiologic Survey. J Stud Alcohol. 1997;58(5):464–473 [DOI] [PubMed] [Google Scholar]
- 4.Wells JE, Horwood LJ, Fergusson DM. Drinking patterns in mid-adolescence and psychosocial outcomes in late adolescence and early adulthood. Addiction. 2004;99(12):1529–1541 [DOI] [PubMed] [Google Scholar]
- 5.Lewinsohn PM, Rohde P, Seeley JR. Alcohol consumption in high school adolescents: frequency of use and dimensional structure of associated problems. Addiction. 1996;91(3):375–390 [DOI] [PubMed] [Google Scholar]
- 6.Harford TC, Grant BF, Yi HY, Chen CM. Patterns of DSM-IV alcohol abuse and dependence criteria among adolescents and adults: results from the 2001 National Household Survey on Drug Abuse. Alcohol Clin Exp Res. 2005;29(5):810–828 [DOI] [PubMed] [Google Scholar]
- 7.US Department of Health Human Services. Results from the 2010 National Survey on Drug Use and Health: summary of national findings. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Series H-41, HHS Publication No. (SMA) 11-4658; 2011
- 8.Bingham CR, Shope JT, Parow JE, Raghunathan TE. Crash types: markers of increased risk of alcohol-involved crashes among teen drivers. J Stud Alcohol Drugs. 2009;70(4):528–535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zador PL, Krawchuk SA, Voas RB. Alcohol-related relative risk of driver fatalities and driver involvement in fatal crashes in relation to driver age and gender: an update using 1996 data. J Stud Alcohol. 2000;61(3):387–395 [DOI] [PubMed] [Google Scholar]
- 10.Office of Applied Studies Results from the 2009 National Survey on Drug Use and Health, Vol. 1: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2010 [Google Scholar]
- 11.Collins D, Abadi MH, Johnson K, Shamblen S, Thompson K. Non-medical use of prescription drugs among youth in an Appalachian population: prevalence, predictors, and implications for prevention. J Drug Educ. 2011;41(3):309–326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Committee on Health Care for Underserved Women, The American College of Obstetricians and Gynecologists. Committee Opinion No. 538: Nonmedical Use of Prescription Drugs. Obstet Gynec. 2012;120(4): 977–982 [DOI] [PubMed]
- 13.Benotsch EG, Koester S, Luckman D, Martin AM, Cejka A. Non-medical use of prescription drugs and sexual risk behavior in young adults. Addict Behav. 2011;36(1–2):152–155 [DOI] [PubMed] [Google Scholar]
- 14.Back SE, Payne RL, Simpson AN, Brady KT. Gender and prescription opioids: findings from the National Survey on Drug Use and Health. Addict Behav. 2010;35(11):1001–1007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Center for Lawful Access and Abuse Deterrence (CLAAD). The National Prescription Drug Abuse Prevention Strategy: 2011-2012 Update. Arlington, 2011. Available at: http://claad.org/wp-content/uploads/2013/10/CLAAD_Strategy2011_v3.pdf. Accessed June 5, 2015 [Google Scholar]
- 16.McCauley JL, Amstadter AB, Macdonald A, et al. Non-medical use of prescription drugs in a national sample of college women. Addict Behav. 2011;36(7):690–695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Young A, Grey M, Boyd CJ, McCabe SE. Adolescent sexual assault and the medical and nonmedical use of prescription medication. J Addict Nurs. 2011;11(1–2):25–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Viana AG, Trent L, Tull MT, et al. Non-medical use of prescription drugs among Mississippi youth: constitutional, psychological, and family factors. Addict Behav. 2012;37(12):1382–1388 [DOI] [PubMed] [Google Scholar]
- 19.Fiellin LE, Tetrault JM, Becker WC, Fiellin DA, Hoff RA. Previous use of alcohol, cigarettes, and marijuana and subsequent abuse of prescription opioids in young adults. J Adolesc Health. 2013;52(2):158–163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ford JA, Arrastia MC. Pill-poppers and dopers: a comparison of non-medical prescription drug use and illicit/street drug use among college students. Addict Behav. 2008;33(7):934–941 [DOI] [PubMed] [Google Scholar]
- 21.McCabe SE, West BT, Teter CJ, Cranford JA, Ross-Durow PL, Boyd CJ. Adolescent nonmedical users of prescription opioids: brief screening and substance use disorders. Addict Behav. 2012;37(5):651–656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu LT, Ringwalt CL, Mannelli P, Patkar AA. Prescription pain reliever abuse and dependence among adolescents: a nationally representative study. J Am Acad Child Adolesc Psychiatry. 2008;47(9):1020–1029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schillie SF, Shehab N, Thomas KE, Budnitz DS. Medication overdoses leading to emergency department visits among children. Am J Prev Med. 2009;37(3):181–187 [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. CDC Grand Rounds: Prescription Drug Overdoses—A US Epidemic. Atlanta, GA: Centers for Disease Control and Prevention; 2012 [PubMed] [Google Scholar]
- 25.White AM, MacInnes E, Hingson RW, Pan IJ. Hospitalizations for suicide-related drug poisonings and co-occurring alcohol overdoses in adolescents (ages 12-17) and young adults (ages 18-24) in the United States, 1999-2008: results from the Nationwide Inpatient Sample. Suicide Life Threat Behav. 2013;43(2):198–212 [DOI] [PubMed] [Google Scholar]
- 26.Havard A, Shakeshaft A, Sanson-Fisher R. Systematic review and meta-analyses of strategies targeting alcohol problems in emergency departments: interventions reduce alcohol-related injuries. Addiction. 2008;103(3):368–376; discussion 377–378 [DOI] [PubMed]
- 27.Spirito A, Monti PM, Barnett NP, et al. A randomized clinical trial of a brief motivational intervention for alcohol-positive adolescents treated in an emergency department. J Pediatr. 2004;145(3):396–402 [DOI] [PubMed] [Google Scholar]
- 28.Foxcroft DR, Coombes L, Wood S, Allen D, Almeida Santimano NM. Motivational interviewing for alcohol misuse in young adults. Cochrane Database Syst Rev. 2014;8:CD007025. [DOI] [PubMed] [Google Scholar]
- 29.Carey KB, Scott-Sheldon LA, Elliott JC, Garey L, Carey MP. Face-to-face versus computer-delivered alcohol interventions for college drinkers: a meta-analytic review, 1998 to 2010. Clin Psychol Rev. 2012;32(8):690–703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Levy SJ, Kokotailo PK, Committee on Substance Abuse . Substance use screening, brief intervention, and referral to treatment for pediatricians. Pediatrics. 2011;128(5). Available at: www.pediatrics.org/cgi/content/full/128/5/e1330 [DOI] [PubMed] [Google Scholar]
- 31.American College of Emergency Physicians. Alcohol screening in the emergency department. Available at: www.acep.org/practres.aspx?id=29074. Accessed June 30, 2009
- 32.Substance Abuse and Mental Health Service Administration (SAMHSA), Committee on Trauma Quick Guide. Alcohol screening and brief interventions (SBI) for trauma patients. Available at: www.facs.org/∼/media/files/quality%20programs/trauma/publications/sbirtguide.ashx. Accessed March 17, 2015
- 33.Van Hook S, Harris SK, Brooks T, et al. New England Partnership for Substance Abuse Research . The “six T’s”: barriers to screening teens for substance abuse in primary care. J Adolesc Health. 2007;40(5):456–461 [DOI] [PubMed] [Google Scholar]
- 34.Bernstein SL, Bernstein E, Boudreaux ED, et al. Public health considerations in knowledge translation in the emergency department. Acad Emerg Med. 2007;14(11):1036–1041 [DOI] [PubMed] [Google Scholar]
- 35.Academic ED, Academic ED SBIRT Research Collaborative . The impact of screening, brief intervention, and referral for treatment on emergency department patients’ alcohol use. Ann Emerg Med. 2007;50(6):699–710, 710.e1–710.e6 [DOI] [PubMed] [Google Scholar]
- 36.Ondersma SJ, Grekin ER, Svikis D. The potential for technology in brief interventions for substance use, and during-session prediction of computer-delivered brief intervention response. Subst Use Misuse. 2011;46(1):77–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Latimer WW, Winters KC, Stinchfield R, Traver RE. Demographic, individual, and interpersonal predictors of adolescent alcohol and marijuana use following treatment. Psychol Addict Behav. 2000;14(2):162–173 [DOI] [PubMed] [Google Scholar]
- 38.Maggs JL, Schulenberg JE. Initiation and course of alcohol consumption among adolescents and young adults. Recent Dev Alcohol. 2005;17:29–47 [DOI] [PubMed] [Google Scholar]
- 39.Mello MJ, Longabaugh R, Baird J, Nirenberg T, Woolard R. DIAL: a telephone brief intervention for high-risk alcohol use with injured emergency department patients. Ann Emerg Med. 2008;51(6):755–764 [DOI] [PubMed] [Google Scholar]
- 40.Walton MA, Chermack ST, Blow FC, et al. Components of brief alcohol interventions for youth in the emergency department [published online ahead of print September 15, 2014]. Subst Abus. doi:10.1080/08897077.2014.958607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction. 1993;88(6):791–804 [DOI] [PubMed] [Google Scholar]
- 42.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–1795 [DOI] [PubMed] [Google Scholar]
- 43.Chung T, Colby SM, Barnett NP, Rohsenow DJ, Spirito A, Monti PM. Screening adolescents for problem drinking: performance of brief screens against DSM-IV alcohol diagnoses. J Stud Alcohol. 2000;61(4):579–587 [DOI] [PubMed] [Google Scholar]
- 44.Knight JR, Sherritt L, Harris SK, Gates EC, Chang G. Validity of brief alcohol screening tests among adolescents: a comparison of the AUDIT, POSIT, CAGE, and CRAFFT. Alcohol Clin Exp Res. 2003;27(1):67–73 [DOI] [PubMed] [Google Scholar]
- 45.Smith GR, Ross RL, Rost KM. Psychiatric outcomes module: substance Abuse Outcomes Module (SOAM). In: Sederer LI, Dickey B, eds. Outcomes Assessment in Clinical Practice. Baltimore, MD: Williams & Wilkins; 1996:85–88 [Google Scholar]
- 46.Handelsman L, Stein JA, Grella CE. Contrasting predictors of readiness for substance abuse treatment in adults and adolescents: a latent variable analysis of DATOS and DATOS-A participants. Drug Alcohol Depend. 2005;80(1):63–81 [DOI] [PubMed] [Google Scholar]
- 47.Bearman PS, Jones J, Udry JR. The National Longitudinal Study of Adolescent Health: research design. Available at: www.cpc.unc.edu/projects/addhealth. Accessed May 15, 2015
- 48.Shakeshaft AP, Bowman JA, Sanson-Fisher RW. A comparison of two retrospective measures of weekly alcohol consumption: diary and quantity/frequency index. Alcohol Alcohol. 1999;34(4):636–645 [DOI] [PubMed] [Google Scholar]
- 49.White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. J Stud Alcohol. 1989;50(1):30–37 [DOI] [PubMed] [Google Scholar]
- 50.Martens MP, Neighbors C, Dams-O’Connor K, Lee CM, Larimer ME. The factor structure of a dichotomously scored Rutgers Alcohol Problem Index. J Stud Alcohol Drugs. 2007;68(4):597–606 [DOI] [PubMed] [Google Scholar]
- 51.Neal DJ, Corbin WR, Fromme K. Measurement of alcohol-related consequences among high school and college students: application of item response models to the Rutgers Alcohol Problem Index. Psychol Assess. 2006;18(4):402–414 [DOI] [PubMed] [Google Scholar]
- 52.Donovan JE. Young adult drinking-driving: behavioral and psychosocial correlates. J Stud Alcohol. 1993;54(5):600–613 [DOI] [PubMed] [Google Scholar]
- 53.Monti PM, Colby SM, Barnett NP, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psychol. 1999;67(6):989–994 [DOI] [PubMed] [Google Scholar]
- 54.Bingham CR, Shope JT, Tang X. Drinking behavior from high school to young adulthood: differences by college education. Alcohol Clin Exp Res. 2005;29(12):2170–2180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thompson AL, Molina BS, Pelham W, Jr, Gnagy EM. Risky driving in adolescents and young adults with childhood ADHD. J Pediatr Psychol. 2007;32(7):745–759 [DOI] [PubMed] [Google Scholar]
- 56.Jelalian E, Alday S, Spirito A, Rasile D, Nobile C. Adolescent motor vehicle crashes: the relationship between behavioral factors and self-reported injury. J Adolesc Health. 2000;27(2):84–93 [DOI] [PubMed] [Google Scholar]
- 57.Jelalian E, Spirito A, Rasile D, Vinnick L, Rohrbeck C, Arrigan M. Risk taking, reported injury, and perception of future injury among adolescents. J Pediatr Psychol. 1997;22(4):513–531 [DOI] [PubMed] [Google Scholar]
- 58.WHO ASSIST Working Group . The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183–1194 [DOI] [PubMed] [Google Scholar]
- 59.National Institute on Drug Abuse. NIDA quick screen. Available at: www.drugabuse.gov/sites/default/files/pdf/nmassist.pdf. Accessed March 17, 2015
- 60.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: The Guilford Press; 2002 [Google Scholar]
- 61.Rollnick S, Miller W, Butler C. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York, NY: Guilford; 2007 [Google Scholar]
- 62.Rollnick S, Butler CC, McCambridge J, Kinnersley P, Elwyn G, Resnicow K. Consultations about changing behaviour. BMJ. 2005;331(7522):961–963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Resnicow K, Rollnick S. Motivational Interviewing in Health Promotion and Behavioral Medicine. Handbook of Motivational Counseling: Goal-Based Approaches to Assessment and Intervention with Addiction and Other Problems. Hoboken, NJ: John Wiley & Sons, Ltd; 2011 [Google Scholar]
- 64.Borden LA, Martens MP, McBride MA, Sheline KT, Bloch KK, Dude K. The role of college students’ use of protective behavioral strategies in the relation between binge drinking and alcohol-related problems. Psychol Addict Behav. 2011;25(2):346–351 [DOI] [PubMed] [Google Scholar]
- 65.Moyers T, Martin T, Manuel J, Miller W, Ernst D. Revised Global Scales: Motivational Interviewing Treatment Integrity 3.0 (MITI 3.0). Albuquerque, NM: University of New Mexico, Center on Alcoholism, Substance Abuse and Addictions; 2007:28 [Google Scholar]
- 66.White HR, Xie M, Thompson W, Loeber R, Stouthamer-Loeber M. Psychopathology as a predictor of adolescent drug use trajectories. Psychol Addict Behav. 2001;15(3):210–218 [PubMed] [Google Scholar]
- 67.Blackson TC, Butler T, Belsky J, Ammerman RT, Shaw DS, Tarter RE. Individual traits and family contexts predict sons’ externalizing behavior and preliminary relative risk ratios for conduct disorder and substance use disorder outcomes. Drug Alcohol Depend. 1999;56(2):115–131 [DOI] [PubMed] [Google Scholar]
- 68.Zucker RA, Chermack ST, Curran GM. Alcoholism: a lifespan perspective on etiology and course. In: Sameroff AJ, Lewis M, Miller R, eds. Handbook of Developmental Psychopathology. 2nd ed. New York, NY: Plenum; 2000:569–587 [Google Scholar]
- 69.Ellickson PL, Tucker JS, Klein DJ. Ten-year prospective study of public health problems associated with early drinking. Pediatrics. 2003;111(5 pt 1):949–955 [DOI] [PubMed] [Google Scholar]
- 70.Doumas DM, Nelson K, DeYoung A, Renteria CC. Alcohol‐related consequences among first‐year university students: effectiveness of a web‐based personalized feedback program. J Coll Couns. 2014;17(2):150–162 [Google Scholar]
- 71.Doumas DM, Kane CM, Navarro TB, Roman J. Decreasing heavy drinking in first‐year students: evaluation of a web‐based personalized feedback program administered during orientation. J Coll Couns. 2011;14(1):5–20 [Google Scholar]
- 72.Fachini A, Aliane PP, Martinez EZ, Furtado EF. Efficacy of brief alcohol screening intervention for college students (BASICS): a meta-analysis of randomized controlled trials. Subst Abuse Treat Prev Policy. 2012;7:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bingham CR, Barretto AI, Walton MA, Bryant CM, Shope JT, Raghunathan TE. Efficacy of a web-based, tailored, alcohol prevention/intervention program for college students: 3-month follow-up. J Drug Educ. 2011;41(4):405–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bingham CR, Barretto AI, Walton MA, Bryant CM, Shope JT, Raghunathan TE. Efficacy of a web-based, tailored, alcohol prevention/intervention program for college students: initial findings. J Am Coll Health. 2010;58(4):349–356 [DOI] [PubMed] [Google Scholar]
- 75.Maio RF, Shope JT, Blow FC, et al. A randomized controlled trial of an emergency department-based interactive computer program to prevent alcohol misuse among injured adolescents. Ann Emerg Med. 2005;45(4):420–429 [DOI] [PubMed] [Google Scholar]
- 76.Walton MA, Chermack ST, Shope JT, et al. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA. 2010;304(5):527–535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cunningham RM, Chermack ST, Zimmerman MA, et al. Brief motivational interviewing intervention for peer violence and alcohol use in teens: one-year follow-up. Pediatrics. 2012;129(6):1083–1090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kypri K, Langley JD, Saunders JB, Cashell-Smith ML, Herbison P. Randomized controlled trial of web-based alcohol screening and brief intervention in primary care. Arch Intern Med. 2008;168(5):530–536 [DOI] [PubMed] [Google Scholar]
- 79.Bogenschutz MP, Donovan DM, Mandler RN, et al. Brief intervention for patients with problematic drug use presenting in emergency departments: a randomized clinical trial [published correction appears in JAMA Intern Med. 2015;175(3):470]. JAMA Intern Med. 2014;174(11):1736–1745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Saitz R, Palfai TP, Cheng DM, et al. Screening and brief intervention for drug use in primary care: the ASPIRE randomized clinical trial. JAMA. 2014;312(5):502–513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Brener ND, Billy JO, Grady WR. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literature. J Adolesc Health. 2003;33(6):436–457 [DOI] [PubMed] [Google Scholar]


