Significance
Clarification of the presynaptic actions of general anesthetics is critical to understanding the molecular and cellular mechanisms of their prominent effects on synaptic transmission. We show that the ether anesthetic isoflurane inhibits synaptic vesicle exocytosis through inhibition of presynaptic Ca2+ influx in the absence of significant alteration of the Ca2+ sensitivity of exocytosis. The greater inhibition of glutamate release compared with GABA release is explained by the relative anesthetic resistance of Ca2+ influx in GABAergic boutons, consistent with overall reduction in excitatory synaptic tone.
Keywords: GCaMP3, pHlourin, mechanisms of anesthesia, live cell imaging, presynaptic
Abstract
Identifying presynaptic mechanisms of general anesthetics is critical to understanding their effects on synaptic transmission. We show that the volatile anesthetic isoflurane inhibits synaptic vesicle (SV) exocytosis at nerve terminals in dissociated rat hippocampal neurons through inhibition of presynaptic Ca2+ influx without significantly altering the Ca2+ sensitivity of SV exocytosis. A clinically relevant concentration of isoflurane (0.7 mM) inhibited changes in [Ca2+]i driven by single action potentials (APs) by 25 ± 3%, which in turn led to 62 ± 3% inhibition of single AP-triggered exocytosis at 4 mM extracellular Ca2+ ([Ca2+]e). Lowering external Ca2+ to match the isoflurane-induced reduction in Ca2+ entry led to an equivalent reduction in exocytosis. These data thus indicate that anesthetic inhibition of neurotransmitter release from small SVs occurs primarily through reduced axon terminal Ca2+ entry without significant direct effects on Ca2+-exocytosis coupling or on the SV fusion machinery. Isoflurane inhibition of exocytosis and Ca2+ influx was greater in glutamatergic compared with GABAergic nerve terminals, consistent with selective inhibition of excitatory synaptic transmission. Such alteration in the balance of excitatory to inhibitory transmission could mediate reduced neuronal interactions and network-selective effects observed in the anesthetized central nervous system.
The molecular and cellular mechanisms of anesthetic-induced amnesia, unconsciousness and immobilization are incompletely understood, particularly for the modern halogenated ether derivatives like isoflurane. General anesthetics, which are essential to both medical practice and experimental neuroscience, have potent and selective effects on neurotransmission (1), including both presynaptic actions (reduced neurotransmitter release) and postsynaptic actions (modulation of receptor function). These effects contribute to anesthetic-induced reductions in neuronal interactions, which are critical to information processing and consciousness (2–4). Knowledge of the fundamental synaptic effects of anesthetics is therefore essential to a molecular and physiological understanding of anesthetic mechanisms, and to development of more selective and safer anesthetics.
Although postsynaptic electrophysiological effects of anesthetics can be assessed directly using whole cell recordings and heterologous expression of putative molecular targets, their presynaptic actions have been difficult to resolve by conventional approaches that do not clearly discriminate between presynaptic and postsynaptic contributions. Direct evidence for presynaptic effects of volatile anesthetics includes selective inhibition of glutamate release from isolated nerve terminals (5, 6) and of synaptic vesicle (SV) exocytosis in intact hippocampal neurons (7). However, it remains controversial whether these effects involve direct inhibition of SV exocytosis itself or of upstream targets (8, 9). Moreover, the mechanism for the greater sensitivity of glutamate release relative to that of other transmitters is unclear.
Neurotransmitter release is supralinearly dependent on presynaptic Ca2+ influx due to the highly cooperative binding of Ca2+ to synaptotagmin 1, the principal neuronal Ca2+ sensor for triggering vesicular fusion through increases in the probability of exocytosis (Pv) (10, 11). We used sensitive quantitative fluorescence imaging approaches to characterize the effects of the widely used volatile anesthetic isoflurane on the Ca2+ sensitivity of SV exocytosis in cultured rat hippocampal neurons. Although glutamate and GABA have distinct postsynaptic actions, differences in the mechanisms and regulation of SV exocytosis from glutamatergic and GABAergic neurons are not well characterized. Because previous studies indicate that glutamate release is more sensitive to inhibition by volatile anesthetics than GABA release (12), we compared the effects of isoflurane on the coupling of Ca2+ influx to exocytosis in glutamatergic and GABAergic boutons. Our results indicate that the inhibition of SV exocytosis by isoflurane is driven by a reduction in Ca2+ influx. This reduction occurs without affecting the apparent sensitivity of exocytosis to Ca2+. Sensitivity of SV exocytosis to isoflurane is therefore determined by presynaptic targets upstream of exocytosis that determine the magnitude of action potential-evoked Ca2+ influx. Identification of neurotransmitter-selective effects of anesthetics on SV exocytosis is critical for understanding their pathway specific effects on neuronal interactions (13, 14).
Results
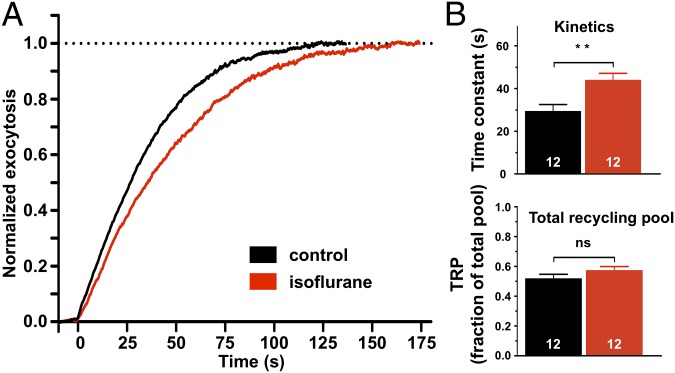
The effects of isoflurane on SV exocytosis were examined using the chimeric reporters of exocytosis vGlut-pHluorin (vG-pH) or synapto-pHlourin (syn-pH) expressed in dissociated rat hippocampal neurons in the presence of 2 or 4 mM extracellular Ca2+ ([Ca2+]e). In resting terminals the pHluorin moiety residing in the acidic SV lumen is quenched, but fluoresces upon exocytosis with luminal alkalization. The reporter is then recycled via local endocytosis and the fluorescence signal is quenched upon reacidification by the V-type H+ ATPase in the SV membrane (15). Action potential stimulation (1,500 APs at 10 Hz) in the presence of the H+ ATPase inhibitor bafilomycin A1 provides a measure of the kinetics of exocytosis of the total recycling vesicle pool (TRP; Fig. 1A) (16).
Fig. 1.
Effects of isoflurane on synaptic vesicle recycling pool size and exocytosis kinetics. (A) Synaptic vesicle exocytosis kinetics were determined by fitting vGlut-pHluorin fluorescence traces during prolonged action potential (AP) stimulation in the presence of bafilomycin A1 (10 Hz for 150 s; 1,500 APs) for control or 0.7 ± 0.06 mM isoflurane [twice the minimum alveolar concentration (MAC); equivalent to EC50 for immobilization in rat] in the presence of 2 mM extracellular Ca2+ ([Ca2+]e). (B) (Upper) Effect of isoflurane on mean exocytosis time constant. Traces were fit with a single exponential function to determine the time constant for exocytosis of the recycling pool. **P < 0.01 by two-tailed unpaired t test. (Lower) Effect of isoflurane on total recycling pool (TRP) size as a fraction of total pool size (determined using 50 mM NH4Cl), P = 0.21 by two-tailed unpaired t test. n = 12.
Isoflurane [0.7 mM; twice the minimum alveolar concentration (MAC) equivalent to the EC50 for rat; ref. 17] significantly slowed exocytosis kinetics of the total recycling pool (TRP) (mean exocytosis time constants: τcontrol = 29 ± 3 s, n = 12; τisoflurane = 44 ± 3 s, n = 12, 95% CI [4.6, 25]; Fig. 1B). Effective TRP size is a dynamic variable modulating synaptic performance (18); however the effects of isoflurane were limited to effects on exocytosis kinetics with no change in TRP size as a fraction of the total pool size (control 0.51 ± 0.03; isoflurane 0.57 ± 0.03; 95% CI [−0.14, 0.03]) determined by perfusion with 50 mM NH4Cl to alkalize all vesicles (Fig. 1B).
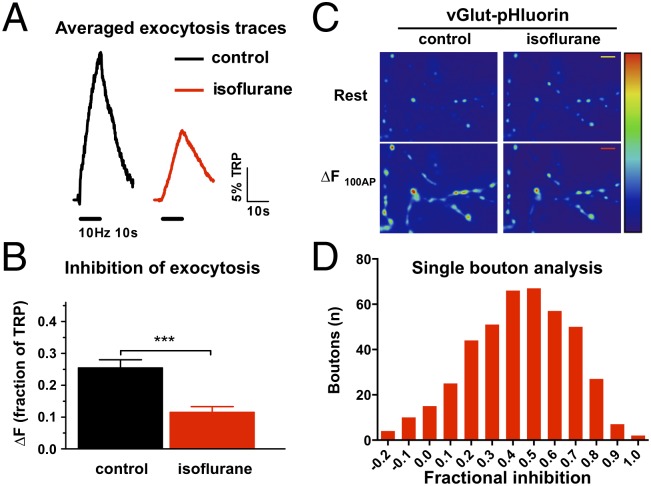
We applied stimulation with AP trains of shorter duration to more closely mimic physiological conditions. A brief burst of AP firing (100 AP at 10 Hz) led to a rapid rise in vG-pH fluorescence (Fig. 2 A and B) corresponding to exocytosis of 0.25 ± 0.026 of the TRP. The average 100-AP response (ΔF100AP) was inhibited by 55% to 0.11 ± 0.018 of TRP by 0.7 mM isoflurane (95% CI [−0.07, −0.21]; Fig. 2B). Single bouton analysis showed that essentially all boutons were inhibited, but the degree of inhibition was variable across the entire population of presynaptic boutons (Fig. 2D).
Fig. 2.
Isoflurane inhibits synaptic vesicle exocytosis evoked by a brief action potential train. (A) Ensemble average traces of a vGlut–pHluorin transfected neuron stimulated at 10 Hz for 10 s (100 APs). Fluorescence intensities were normalized to the peak of a subsequent bafilomycin A1 response (defining the total recycling pool, TRP). (B) Mean values of vGlut–pHluorin response amplitudes for control or 0.7 ± 0.06 mM isoflurane-treated neurons stimulated with 100 APs in the presence of 2 mM extracellular Ca2+ ([Ca2+]e). Average 100 AP response (ΔF100AP) was inhibited 55% by isoflurane, ***P < 0.001 by paired t-test, n = 8. (C) Representative field of vGlut–pHluorin fluorescence images at rest and difference image for 100 AP stimulation (ΔF100AP) for control or isoflurane-treated neurons. (Scale bars: 5 μm.) (D) Histogram of fractional block of vGlut–pHluorin responses in single boutons stimulated with 100 AP. Measurements from 497 boutons collected in eight experiments.
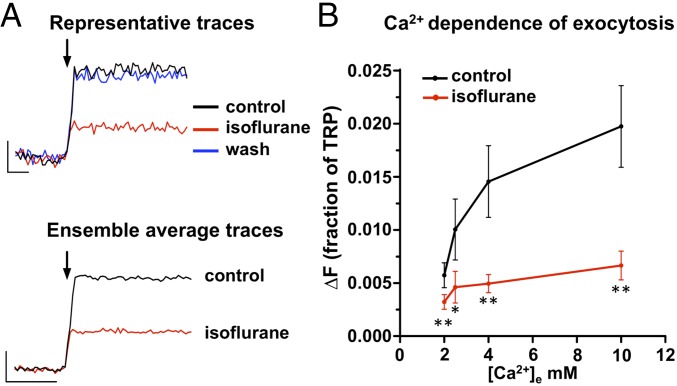
To narrow the possible mechanisms involved in inhibition of SV exocytosis, we examined the effect of isoflurane on exocytosis driven by single AP stimuli. Isoflurane markedly inhibited SV exocytosis in response to 1 AP from 0.015 ± 0.003 of TRP to 0.0049 ± 0.0009 of TRP (mean inhibition 62 ± 3%; 95% CI [−0.003, −0.016]) at 4 mM [Ca2+]e (Fig. 3 A and B). Inhibition was completely reversible: Removal of isoflurane restored exocytosis to control levels (Fig. 3A). Given the cooperative nature of Ca2+ activation of neurotransmitter release, we investigated the effect of isoflurane on the Ca2+ dependence of SV exocytosis in response to a single AP stimulus at varied external Ca2+ concentrations. Single AP-evoked exocytosis was strongly enhanced by elevating [Ca2+]e, saturating at high [Ca2+]e (Fig. 3B). Isoflurane significantly inhibited exocytosis at all Ca2+ concentrations. The effect of isoflurane on SV exocytosis elicited by a single AP stimulus (Fig. 3) was comparable to that elicited by multiple-AP trains (Fig. 2).
Fig. 3.
Reversibility of isoflurane inhibition and Ca2+ dependence of synaptic vesicle exocytosis. (A) (Upper) Representative vGlut–pHlourin fluorescence responses elicited by a single AP at 4 mM extracellular Ca2+ ([Ca2+]e) for control (black), 0.7 mM isoflurane (red), and wash (blue) conditions. Arrow indicates single AP stimulus (n = 8 trials each, ∼25 boutons analyzed per neuron). (Lower) Ensemble average traces of vGlut-pHlourin responses relative to total releasable pool (TRP) size to single AP stimulation at 4 mM extracellular Ca2+ ([Ca2+]e) (10 trial average, ∼25 boutons per neuron). (Scale bar: 0.5% TRP, 100 ms.) (B) Isoflurane inhibition of single AP-stimulated release is not overcome by elevated extracellular Ca2+ ([Ca2+]e). Average relative peak (∆F) evoked by a single AP stimulus expressed as a fraction of the TRP (n = 7–11). *P < 0.05, **P < 0.01 compared with respective control by paired t test. Mean isoflurane concentration 0.70 ± 0.06 mM.
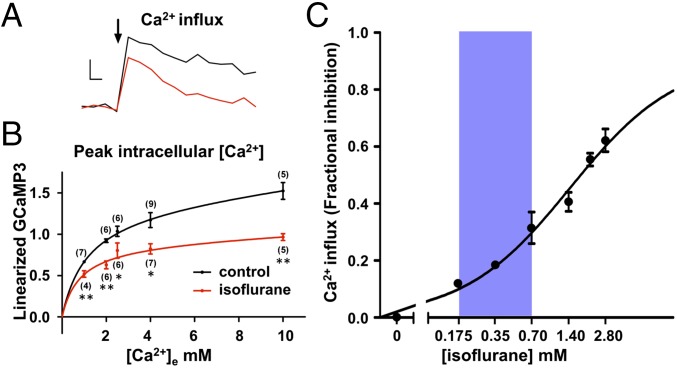
Strong inhibition of single AP-triggered exocytosis implies that isoflurane acts either on Ca2+ entry through voltage-gated Ca2+ channels or on SV fusion in response to increased presynaptic [Ca2+]i. We examined the impact of isoflurane on single-AP driven Ca2+ influx (18, 19) using the genetically-encoded Ca2+ indicator syn-GCaMP3 (20). Isoflurane reduced the linearized syn-GCaMP3 response by 30% from 1.2 ± 0.09 to 0.82 ± 0.06 at 4 mM [Ca2+]e (95% CI [−0.13, −0.66]; Fig. 4 A and B), which indicates that isoflurane inhibits AP-triggered Ca2+ influx (18, 21). Using single AP-triggered activation with [Ca2+]e from 1.5 to 10 mM, Ca2+ influx saturated at high [Ca2+]e, similar to previous findings in the hippocampus (21) and calyx of Held (22) (Fig. 4B). Isoflurane significantly inhibited Ca2+ influx over this entire range of [Ca2+]e, which is consistent with a noncompetitive mechanism of action with respect to [Ca2+]e. We next examined inhibition Ca2+ influx over a range of isoflurane concentrations (with [Ca2+]e = 4 mM). Isoflurane inhibited single AP-evoked Ca2+ influx in a concentration-dependent manner with IC50 = 1.4 ± 1.0 mM (Fig. 4C). Significant inhibition occurred within the clinically relevant concentration range of 0.175 mM to 0.70 mM (defined as 0.5–2 × MAC).
Fig. 4.
Isoflurane reduces action potential-stimulated increases in presynaptic Ca2+ influx. (A) Control (black) and 0.70 ± 0.06 mM isoflurane (red) ensemble average traces of single AP-evoked [Ca2+] influx determined by linearized responses synaptophysin–GCaMP3 at 4 mM extracellular Ca2+ ([Ca2+]e). Arrow indicates single AP stimulus. (Scale bar: 30% ∆F/F0, 100 ms.) (B) Inhibition by 0.70 ± 0.06 mM isoflurane of average peak ∆F/F0 evoked by single AP stimulus as a function of [Ca2+]e. Data are fitted to a single site binding model using a Levenberg–Marquardt algorithm optimization method (control: EC50 = 1.3 ± 0.1 mM, Emax = 1.6 ± 0.5, R2 = 99.8; isoflurane: EC50= 0.8 ± 0.4 mM, Emax = 0.9 ± 0.2, R2 = 92.3); both P < 0.05 by two-sample sum-of-squares F test comparison against the null hypothesis that Emax and EC50 values are identical. (C) Inhibition of Ca2+ influx as a function of log [isoflurane] using synaptopysin-GCaMP3 at 4 mM [Ca2+]e (n = 27). Shaded area indicates the clinical concentration range of isoflurane for general anesthesia in rat (0.18–0.7 mM; 0.5–2 × MAC). Data are fitted to a generalized Hill model by least-squares analysis (Imax = 0.92 ± 0.17; IC50 = 1.4 ± 1.0 mM). Inhibition data were all significantly different from paired control values (*P < 0.05 in two-tailed paired t test).
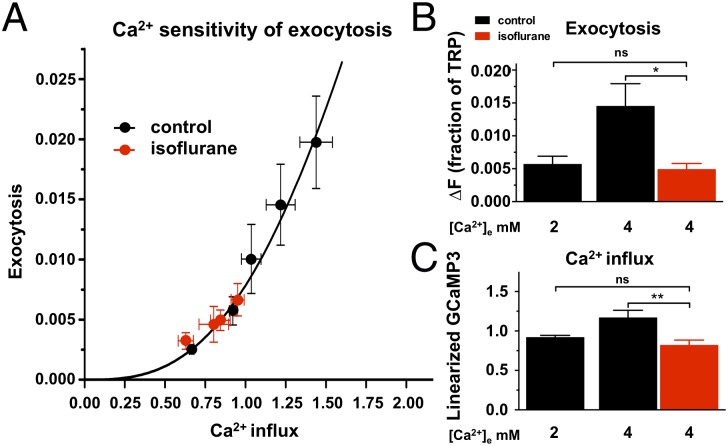
These experiments strongly suggest that isoflurane inhibits SV exocytosis by reducing Ca2+ influx as reported by changes in single AP-triggered syn-GCaMP3 signals. We tested this hypothesis in two ways. First, we examined the cooperative relationship of single AP-triggered Ca2+ influx to SV exocytosis, which is well described by a generalized Hill equation: exocytosis = [Ca2+]in/(Kn + [Ca2+]in) (18, 21) that effectively quantifies the efficiency of exocytosis at different degrees of Ca2+ influx (Fig. 5A). If isoflurane inhibits exocytosis purely by inhibiting AP-driven Ca2+ entry, then the same quantitative relationship should hold. The paired isoflurane data fell on the control curve, which indicates that the effect of isoflurane on SV exocytosis can be attributed to reductions in [Ca2+]i without significant contributing effects on the Ca2+-sensitivity of exocytosis. Second, if inhibition of Ca2+ influx is sufficient to explain reduced exocytosis, then simply lowering [Ca2+]e should mimic the effect of isoflurane on the syn-GCaMP3 signal and replicate isoflurane inhibition of exocytosis. Reducing [Ca2+]e from 4 mM to 2 mM reduced exocytosis from 0.0146 ± 0.0033 of TRP to 0.0057 ± 0.0012 of TRP (61 ± 8% inhibition; 95% CI [−0.0010, −0.0166]), which was comparable to inhibition by 0.7 mM isoflurane to 0.0049 ± 0.0009 of TRP at 4 mM [Ca2+]e (62 ± 3% inhibition; 95% CI [−0.0034, −0.0158]; 95% CI for difference between 2 mM [Ca2+]e and 4 mM [Ca2+]e + isoflurane [−0.0023, 0.0039]; Fig. 5B, and see above Fig. 3). Similarly, lowering [Ca2+]e from 4 mM to 2 mM reduced the syn-GCaMP3 signal from 1.1 ± 0.06 to 0.92 ± 0.02 linearized GCaMP3 units (by 16 ± 2%; 95% CI [−0.030, −0.314]), comparable to the reduction produced by 0.7 mM isoflurane to 0.82 ± 0.06 at [Ca2+]e = 4 mM (by 25 ± 3%; 95% CI [−0.181, −0.363]; 95% CI for difference between 2 mM [Ca2+]e and 4 mM [Ca2+]e + isoflurane [−0.054, 0.254]; Fig. 5C).
Fig. 5.
Effect of isoflurane on synaptic vesicle exocytosis as a function of Ca2+ influx. (A) Exocytosis determined using synaptophysin-pHlourin (ΔF/F) in response to a single AP stimulus relative to total releasable pool (TRP) at 1.5, 2, 2.5, 4, 10 mM [Ca2+]e is plotted against Ca2+ influx determined using synaptophysin-GCaMP3 (ΔF) under similar conditions in the absence or presence of 0.70 ± 0.06 mM isoflurane to reveal the Ca2+ sensitivity of exocytosis (n = 34 for syn-pH experiments, n = 28–33 for syn-GCaMP3 experiments). Data are fitted to a generalized Hill model [exocytosis = [Ca2+]in/(Kn+[Ca2+]in), n = 2.9 ± 0.5, K = 2.8 ± 0.2]. (B) Reduction of [Ca2+]e from 4 mM to 2 mM mimicked the reduction in exocytosis produced by 0.70 ± 0.06 mM isoflurane at 4 mM [Ca2+]e. *P < 0.05 by one-way ANOVA with Tukey’s post hoc test. (C) Reduction of [Ca2+]e from 4 mM to 2 mM mimicked the reduction in syn-GCaMP3 signal produced by 0.70 ± 0.06 mM isoflurane at 4 mM [Ca2+]e. **P < 0.01 by one-way ANOVA with Tukey’s post hoc test.
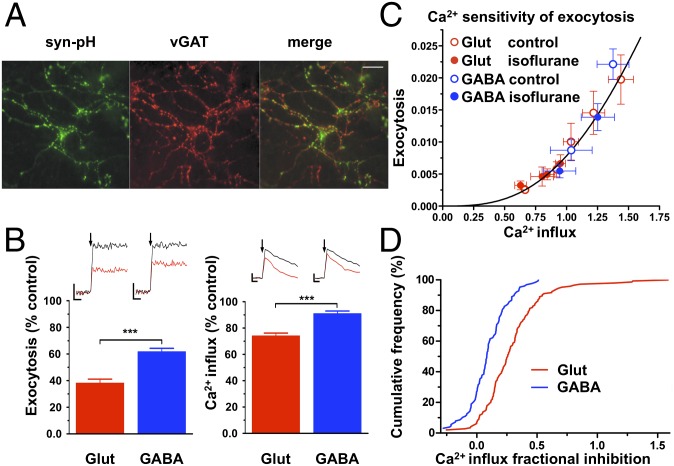
To compare the effects of isoflurane on SV exocytosis from glutamatergic or GABAergic neurons separately, we used live-cell imaging of GABAergic boutons identified by vGAT–Oyster 550 immunolabeling (23) (Fig. 6A). Single AP-evoked SV exocytosis was measured by syn-pH and Ca2+ influx by syn-GCaMP3 (Fig. 6B) averaged over multiple trials (10–15) across populations of glutamatergic or GABAergic synapses. Individual glutamatergic boutons (vGAT-negative) exhibited greater inhibition by isoflurane than did GABAergic boutons (vGAT-positive) of peak syn-pH (62% compared with 38% inhibition; 95% CI [−13, −34]) and syn-GCaMP3 fluorescence (26% compared with 9% inhibition; 95% CI [−10, −24]) (Fig. 6B). For both neurotransmitter phenotypes, the effect of isoflurane on Ca2+ influx correlated with its effect on exocytosis over a range of [Ca2+]e, indicative of a minimal direct effect on the Ca2+ sensitivity of exocytosis (Fig. 6C). The Ca2+ sensitivity of SV exocytosis for glutamatergic or GABAergic boutons was not significantly different. Isoflurane shifted the frequency-response histogram for fractional inhibition of Ca2+ influx further to the right in glutamatergic boutons compared with GABAergic boutons (Fig. 6D).
Fig. 6.
Differential effects of isoflurane on synaptic vesicle exocytosis in glutamatergic and GABAergic neurons is proportional to reduction Ca2+ influx. (A) Representative live-cell image of syn-pH-positive boutons (green, Left), GABAergic boutons immunolabeled using vGAT–Oyster 550 (red, Center), and merge shown as yellow (Right), with surrounding vGAT-positive boutons (red, Right) from untransfected neurons. (Scale bar: 20 μm.) (B Left) The effect of 0.70 ± 0.06 mM isoflurane on single AP exocytosis is greater in glutamatergic (vGAT-negative; 62 ± 3% block, n = 11) than in GABAergic (vGAT-positive; 38 ± 3% block, n = 5) boutons at 4 mM extracellular [Ca2+]e, ***P < 0.001 by unpaired t test. (Insets) Exemplar single AP stimulus (arrow) syn-pH fluorescence traces before (black) and after (red) isoflurane in glutamatergic (Left) and GABAergic (Right) boutons. (Scale bars: 0.5% TRP, 100 ms.) (B, Right) Effect of isoflurane on presynaptic Ca2+ influx is greater in glutamatergic (26 ± 2% block, n = 7) than in GABAergic (9.2 ± 2% block, n = 7) boutons at 4 mM extracellular [Ca2+]e, ***P < 0.001 by unpaired t test. (Insets) Exemplar single AP stimulus (arrow) syn-GCaMP3 fluorescence traces before (black) and after (red) isoflurane in glutamatergic and GABAergic boutons. (Scale bars: 30% ∆F/F0, 200 ms.) (C) Effect of 0.70 ± 0.06 mM isoflurane on exocytosis as a function of Ca2+ influx in glutamatergic and GABAergic boutons. Exocytosis determined using syn-pH in response to single AP relative to TRP is plotted against relative increases in Ca2+ influx determined using syn-GCaMP3 over a range of [Ca2+]e from 1.5 to 10 mM under similar conditions to yield the Ca2+ sensitivity of exocytosis (n = 26 for exocytosis, n = 24 for Ca2+ influx). The curve indicates the data from Fig. 5A. (D) Cumulative frequency distribution of 0.70 ± 0.06 mM isoflurane inhibition of peak [Ca2+]i for GABAergic and glutamatergic boutons. Data from 272 boutons collected in 12 experiments.
Discussion
Using sensitive and specific assays of presynaptic anesthetic effects, we find that the widely used ether anesthetic isoflurane inhibits AP-evoked SV exocytosis without affecting the coupling between Ca2+ influx and exocytosis in mature cultured rat hippocampal neurons. Analysis of individual nerve terminals and neurons allowed us to isolate presynaptic mechanisms of isoflurane on exocytosis without interference from intrinsic neuronal networks or postsynaptic effects. A single AP stimulus provides a very brief local increase in intracellular free Ca2+, allowing for high time resolution observations of presynaptic responses. Isoflurane inhibition of SV exocytosis measured using pHluorin indicators correlated with reduced Ca2+ influx measured using syn-GCaMP3; there were no direct effects on the Ca2+ sensitivity of SV exocytosis. By varying [Ca2+]e, we observed that the Ca2+ dependence of SV exocytosis follows the same supralinear relationship in the presence or absence of isoflurane. Moreover, isoflurane inhibited SV exocytosis from glutamatergic boutons more potently than from GABAergic boutons in proportion to the reduction in presynaptic Ca2+ influx. This presynaptic selectivity was not due to an intrinsic difference in the Ca2+ sensitivity of exocytosis between glutamatergic and GABAergic terminals, which were in fact similar in control conditions. These findings elucidate fundamental synaptic mechanisms that lead to neurotransmitter-selective effects that are critical to understanding the actions of anesthetics on sensitive neuronal networks (13, 14).
Neurotransmitter release is determined by the highly cooperative relationship between Ca2+ entry and SV exocytosis, and by the number of docked and primed vesicles (readily releasable pool) (24). Ca2+ entry is regulated mainly by presynaptic ion channels (e.g., Na+, Ca2+, and K+ channels), presynaptic receptors, and modulatory cell signaling mechanisms (25). We have shown previously that isoflurane has transmitter-specific effects on neurotransmitter release from a heterogeneous population of isolated axon terminals (26), and inhibits chemically evoked glutamate release more potently than release of other neurotransmitters (12, 26). Pharmacological differences between glutamate and GABA release could result from synapse-specific differences in expression and/or coupling of specific isoforms of ion channels or other proteins regulating SV exocytosis (27, 28). Hippocampal glutamate and GABA containing SVs differ in their release properties during AP trains as well as in their adaptive response to strong depolarization (29–31). Different profiles of presynaptic ion channel expression underlie exocytosis in glutamatergic and GABAergic synapses (32–34). Our findings that greater isoflurane sensitivity of glutamatergic compared with GABAergic SV exocytosis is determined by larger effects on Ca2+ influx are consistent with transmitter phenotype-specific differences in expression of the presynaptic ion channels that determine [Ca2+]i, including distinct subtypes of Nav, Cav, and Kv channels (35).
Greater sensitivity of glutamate release to anesthetic inhibition is consistent with a net reduction in network excitability involving both presynaptic and postsynaptic inhibition of glutamatergic transmission. The relative anesthetic insensitivity of GABA release coupled with the potent anesthetic potentiation of postsynaptic GABAA receptors (1) and increased asynchronous GABA release (36) together enhance net hippocampal network inhibition (37). The balance of anesthetic actions on overall network excitability can vary between brain regions, consistent with synaptic and regional differences in anesthetic target expression and/or functional roles (38). The presynaptic selectivity of volatile anesthetics like isoflurane in suppressing excitatory neurotransmission is expected to scale up to reduced neuronal interactions and information transfer at the network level, which is considered a leading mechanism for anesthetic-induced unconsciousness (2, 39).
The molecular mechanisms of general anesthetics involve effects on both excitatory and inhibitory synaptic transmission (1). Potentiation of GABAA receptors represents the major action of most i.v. anesthetics (40, 41), but this mechanism alone does not account for the lesser target selectivity of volatile anesthetics compared with i.v. anesthetics (42, 43). Potential synaptic volatile anesthetic targets involved in regulating transmitter release include glutamate receptors, Nav channels (44), K2P channels (45), nicotinic acetylcholine receptors (34), Cav channels (46), neurotransmitter transporters (47, 48), and SNARE proteins (8, 49). Evidence suggests that the presynaptic effects of volatile anesthetics on neurotransmitter release are mediated by reduced nerve terminal excitability from inhibition of Nav channels rather than direct inhibition of Ca2+ influx by inhibition of Cav channels (7, 44, 50, 51). A critical distinction is between presynaptic reductions in Ca2+ influx involving direct inhibition of Cav (e.g., 52) or indirect effects involving alterations in the presynaptic AP waveform as a result of effects on other ion channels including Kv and Nav (35, 50, 51, 53). We have previously shown that hippocampal neuron SV exocytosis is much less sensitive to isoflurane when evoked by elevated extracellular KCl to open Cav rather than by electrical simulation of action potentials (7), which provides further support for a major target upstream of Ca2+ entry. Recent enhancements in the use of microbial rhodopsin-based indicators of membrane voltage that are sensitive and fast enough to detect presynaptic APs (54, 55) will facilitate tests of this hypothesis by allowing quantification of anesthetic effects on AP properties in individual hippocampal boutons.
The observation that isoflurane inhibits SV exocytosis in a way that is quantitatively consistent with reductions in Ca2+ influx indicates anesthetic target(s) upstream of Ca2+-exocytosis coupling. Our findings in intact hippocampal neurons using sensitive and direct assays of SV fusion and Ca2+ influx support isoflurane effects on AP-evoked increases in [Ca2+]i as the principal presynaptic mechanism of action. In contrast, studies using reduced cell preparations (permeabilized pheochromocytoma cells) have suggested direct effects of isoflurane on SNARE-mediated SV fusion (8, 9). This discrepancy might be in part due to the use of permeabilized tumor cells to measure release of catecholamines, which is known to involve different mechanisms compared with typical small SVs, including distinct Ca2+ sensitivity of SV vesicle exocytosis (56). Whether these differences represent transmitter-specific differences in release from large dense core vesicles in pheochromocytoma cells compared with release from small SVs in hippocampal neurons (26, 55) or artifacts due to use of detergents and ionophores for membrane permeabilization (8, 9) will require confirmation in intact catecholamine-releasing neurons using live cell imaging approaches. Our findings appear to contradict a report that isoflurane inhibits ionomycin-evoked RH414 destaining of rat hippocampal neuron boutons with no change in neuronal [Ca2+] (9). However, the measurements of whole cell peak [Ca2+] reported using fura 2 reflect primarily changes in somatic rather than nerve terminal [Ca2+], and involve contributions from distinct Ca2+ sources and combinations of Ca2+ channel subtypes due to differences in subcellular expression (57).
Several factors must be considered in interpreting these results. Experiments were performed at 30 °C to facilitate recording stability and pharmacological analysis. The kinetics of SV exocytosis and endocytosis are faster at higher physiological temperatures, but exhibit similar fundamental properties (58). Cultured hippocampal neurons provide an accessible model for analyzing nerve terminal physiology, but they lack the tissue structure of slice preparations and therefore might not fully reflect properties of typical hippocampal neuron terminals in situ. Differences in isoflurane effects on SV exocytosis from other neuronal types and in other brain regions must also be considered (26).
Our findings indicate that isoflurane reduces presynaptic Ca2+ influx preferentially in glutamatergic compared with GABAergic boutons imply that at least one of the key molecular players controlling AP-driven Ca2+ influx is different in these two neuronal subtypes. Further studies are required to identify these molecular target(s) for isoflurane inhibition (26), but the studies presented here significantly narrow the list of possibilities. Volatile anesthetics have multiple cellular actions including depression of glutamate-mediated excitatory transmission and facilitation of inhibitory GABAergic transmission, in contrast to the principally GABAergic i.v. anesthetics propofol and etomidate that selectively potentiate GABAA receptors (1, 13, 59). Although both propofol and the volatile anesthetic sevoflurane produce similar frontal coherent alpha and slow electroencephalographic oscillations in vivo, probably due to shared GABAergic mechanisms mediating amnesia and unconsciousness, sevoflurane has additional distinct encephalographic effects consistent with nonGABAergic actions (60). The depressive effects of isoflurane on hippocampal CA1 neuron excitability in rat brain slices involve primarily nonGABAergic mechanisms including direct depression of glutamate-mediated excitation (61), which supports an important role for effects on glutamatergic transmission. A nonGABAergic mechanism such as suppression of excitatory transmission through Nav channel blockade (42, 43, 62) is likely to mediate isoflurane-induced immobility, a ventral spinal anesthetic endpoint (63). At higher doses, inhibition of glutamatergic transmission likely contributes to electroencephalographic silence in vivo (64, 65). Clarification of such fundamental molecular and cellular mechanisms for the synaptic selectivity of volatile anesthetics such as isoflurane in depressing excitatory neurotransmission presynaptically while enhancing inhibitory neurotransmission postsynaptically provides a framework for explaining the higher order neuronal network processes relevant to specific anesthetic endpoints including amnesia, unconsciousness and immobility (13, 14).
Materials and Methods
Materials and Solutions.
Cells were perfused at 0.27 mL min−1 with Tyrode’s solution (119 mM NaCl, 2.5 mM KCl, 1.5–10 mM CaCl2, 25 mM Hepes buffered to pH 7.4, 30 mM glucose) containing 10 μM 6-cyano-7-nitroquinoxaline-2,3-dione (CNQX) and 50 μM D,L-2-amino-5-phosphonovaleric acid (AP5). Isoflurane dissolved in Tyrode’s solution was perfused focally onto imaged cells via a 150-μm-diameter pipette; delivered isoflurane concentrations were determined by gas chromatography (66).
Neuron Imaging.
Experiments were approved by the Weill Cornell Medical College Institutional Animal Care and Use Committee and conformed to NIH Guidelines for the Care and Use of Animals. Hippocampal CA3–CA1 regions were dissected from neonatal Sprague–Dawley rats, and cells were dissociated, plated, and transfected as described (67). Live-cell imaging was performed at 30.0 ± 0.2 °C using an epifluorescence microscope (ZEISS Axio Observer Z1). Synaptophysin-pHluorin (syn-pH), was used as an optical sensor of SV exocytosis (68, 69); for experiments requiring higher signal-to-noise ratio, vGlut-pHluorin (vG-pH) was used (58). Synaptophysin-GCaMP3 (syn-GCaMP3) was used to measure intracellular Ca2+ ([Ca2+]i) in hippocampal neuron boutons stimulated by field-potential-generated APs. Fluorescence images were acquired with an Andor iXon1 camera (model DU-897E-BV) with a solid-state diode pumped 488-nm laser.
Exocytosis and Calcium Measurements.
For exocytosis, ΔF of syn-pH and vG-pH was determined as the difference between the average of 10 frames before and after a single AP stimulus. Signals were expressed as a fraction or percentage of TRP, determined by applying a maximally depleting stimulus (1,500 APs at 10 Hz) in the presence of bafilomycin A1 (Fig. 1). Superfusion of 0.7 mM isoflurane for 5 min did not affect baseline fluorescence or maximal fluorescence elicited by 1,500 APs in the presence of bafilomycin A (TRP; ΔF < 4%) of either syn-pH or vG-pH transfected boutons. For Ca2+ influx, ΔF of syn-GCaMP3 was determined as the difference between the average of 10 frames before and the 5 highest points after a single AP stimulus. Changes in fluorescence were normalized to syn-GCaMP intensity at Ca2+ saturation (FMAX) determined by applying 200 μM ionomycin, which caused a 6.1- to 6.6-fold increase in syn-GCaMP3 fluorescence in agreement with previous results (19). Changes in GCaMP3 fluorescence (ΔF/F) are related to changes in intracellular Ca2+ according to a generalized Hill equation (Vmax = 1, k = 9.077, n = 2.5; adjusted R2 = 0.997; ref. 19), and can be linearized to the single AP signal obtained using the linear indicator Magnesium Green (Life Technologies) as (ΔF/F)linear = (((ΔF/F)/FMAX) × kn)/(1 − ((ΔF/F)/FMAX))(1/n). Superfusion of 0.7 mM isoflurane for 5 min did not affect baseline fluorescence (ΔF < 4%) of syn-GCaMP3 transfected boutons.
Image and Data Analysis.
Images were analyzed in ImageJ (rsb.info.nih.gov/ij) using a custom plugin (rsb.info.nih.gov/ij/plugins/time-series.html). Rabbit vGAT-Oyster 550 luminal domain antibody was used to identify GABAergic neurons (23). Values are shown as mean ± SEM. ANOVA with Tukey’s post hoc test, Student’s or Welch’s unpaired t test (P < 0.05), and 95% confidence intervals on the difference of the means were used to determine statistical significance.
Acknowledgments
We thank L. Looger, Y. Zhu, S. Voglmaier, and R. Edwards for generously providing plasmids, and members of the H.C.H. and T.A.R. laboratories for constructive comments. This work was supported by National Institutes of Health Grants T32DA07274 (to J.P.B.), R01MH085783 (to T.A.R.), and R01GM58055 (to H.C.H.).
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
References
- 1.Hemmings HC, Jr, et al. Emerging molecular mechanisms of general anesthetic action. Trends Pharmacol Sci. 2005;26(10):503–510. doi: 10.1016/j.tips.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Alkire MT, Hudetz AG, Tononi G. Consciousness and anesthesia. Science. 2008;322(5903):876–880. doi: 10.1126/science.1149213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewis LD, et al. Rapid fragmentation of neuronal networks at the onset of propofol-induced unconsciousness. Proc Natl Acad Sci USA. 2012;109(49):E3377–E3386. doi: 10.1073/pnas.1210907109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blain-Moraes S, et al. Neurophysiological correlates of sevoflurane-induced unconsciousness. Anesthesiology. 2015;122(2):307–316. doi: 10.1097/ALN.0000000000000482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schlame M, Hemmings HC., Jr Inhibition by volatile anesthetics of endogenous glutamate release from synaptosomes by a presynaptic mechanism. Anesthesiology. 1995;82(6):1406–1416. doi: 10.1097/00000542-199506000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Miao N, Frazer MJ, Lynch C., 3rd Volatile anesthetics depress Ca2+ transients and glutamate release in isolated cerebral synaptosomes. Anesthesiology. 1995;83(3):593–603. doi: 10.1097/00000542-199509000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Hemmings HC, Jr, Yan W, Westphalen RI, Ryan TA. The general anesthetic isoflurane depresses synaptic vesicle exocytosis. Mol Pharmacol. 2005;67(5):1591–1599. doi: 10.1124/mol.104.003210. [DOI] [PubMed] [Google Scholar]
- 8.Herring BE, Xie Z, Marks J, Fox AP. Isoflurane inhibits the neurotransmitter release machinery. J Neurophysiol. 2009;102(2):1265–1273. doi: 10.1152/jn.00252.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xie Z, et al. Interaction of anesthetics with neurotransmitter release machinery proteins. J Neurophysiol. 2013;109(3):758–767. doi: 10.1152/jn.00666.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Augustine GJ. How does calcium trigger neurotransmitter release? Curr Opin Neurobiol. 2001;11(3):320–326. doi: 10.1016/s0959-4388(00)00214-2. [DOI] [PubMed] [Google Scholar]
- 11.Chapman ER. How does synaptotagmin trigger neurotransmitter release? Annu Rev Biochem. 2008;77:615–641. doi: 10.1146/annurev.biochem.77.062005.101135. [DOI] [PubMed] [Google Scholar]
- 12.Westphalen RI, Hemmings HC., Jr Volatile anesthetic effects on glutamate versus GABA release from isolated rat cortical nerve terminals: 4-aminopyridine-evoked release. J Pharmacol Exp Ther. 2006;316(1):216–223. doi: 10.1124/jpet.105.090662. [DOI] [PubMed] [Google Scholar]
- 13.Franks NP. General anaesthesia: From molecular targets to neuronal pathways of sleep and arousal. Nat Rev Neurosci. 2008;9(5):370–386. doi: 10.1038/nrn2372. [DOI] [PubMed] [Google Scholar]
- 14.Brown EN, Purdon PL, Van Dort CJ. General anesthesia and altered states of arousal: A systems neuroscience analysis. Annu Rev Neurosci. 2011;34:601–628. doi: 10.1146/annurev-neuro-060909-153200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sankaranarayanan S, De Angelis D, Rothman JE, Ryan TA. The use of pHluorins for optical measurements of presynaptic activity. Biophys J. 2000;79(4):2199–2208. doi: 10.1016/S0006-3495(00)76468-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sankaranarayanan S, Ryan TA. Calcium accelerates endocytosis of vSNAREs at hippocampal synapses. Nat Neurosci. 2001;4(2):129–136. doi: 10.1038/83949. [DOI] [PubMed] [Google Scholar]
- 17.Taheri S, et al. What solvent best represents the site of action of inhaled anesthetics in humans, rats, and dogs? Anesth Analg. 1991;72(5):627–634. doi: 10.1213/00000539-199105000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Kim SH, Ryan TA. CDK5 serves as a major control point in neurotransmitter release. Neuron. 2010;67(5):797–809. doi: 10.1016/j.neuron.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoppa MB, Lana B, Margas W, Dolphin AC, Ryan TA. α2δ expression sets presynaptic calcium channel abundance and release probability. Nature. 2012;486(7401):122–125. doi: 10.1038/nature11033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tian L, et al. Imaging neural activity in worms, flies and mice with improved GCaMP calcium indicators. Nat Methods. 2009;6(12):875–881. doi: 10.1038/nmeth.1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ariel P, Ryan TA. Optical mapping of release properties in synapses. Front Neural Circuits. 2010;4:1–10. doi: 10.3389/fncir.2010.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schneggenburger R, Meyer AC, Neher E. Released fraction and total size of a pool of immediately available transmitter quanta at a calyx synapse. Neuron. 1999;23(2):399–409. doi: 10.1016/s0896-6273(00)80789-8. [DOI] [PubMed] [Google Scholar]
- 23.Dobie FA, Craig AM. Inhibitory synapse dynamics: Coordinated presynaptic and postsynaptic mobility and the major contribution of recycled vesicles to new synapse formation. J Neurosci. 2011;31(29):10481–10493. doi: 10.1523/JNEUROSCI.6023-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dittman J, Ryan TA. Molecular circuitry of endocytosis at nerve terminals. Annu Rev Cell Dev Biol. 2009;25:133–160. doi: 10.1146/annurev.cellbio.042308.113302. [DOI] [PubMed] [Google Scholar]
- 25.Meir A, et al. Ion channels in presynaptic nerve terminals and control of transmitter release. Physiol Rev. 1999;79(3):1019–1088. doi: 10.1152/physrev.1999.79.3.1019. [DOI] [PubMed] [Google Scholar]
- 26.Westphalen RI, Desai KM, Hemmings HC., Jr Presynaptic inhibition of the release of multiple major central nervous system neurotransmitter types by the inhaled anaesthetic isoflurane. Br J Anaesth. 2013;110(4):592–599. doi: 10.1093/bja/aes448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bragina L, et al. Analysis of synaptotagmin, SV2, and rab3 expression in cortical glutamatergic and GABAergic axon terminals. Front Cell Neurosci. 2011;5:32. doi: 10.3389/fncel.2011.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reid CA, Bekkers JM, Clements JD. Presynaptic Ca2+ channels: A functional patchwork. Trends Neurosci. 2003;26(12):683–687. doi: 10.1016/j.tins.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 29.Grønborg M, et al. Quantitative comparison of glutamatergic and GABAergic synaptic vesicles unveils selectivity for few proteins including MAL2, a novel synaptic vesicle protein. J Neurosci. 2010;30(1):2–12. doi: 10.1523/JNEUROSCI.4074-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moulder KL, et al. Vesicle pool heterogeneity at hippocampal glutamate and GABA synapses. J Neurosci. 2007;27(37):9846–9854. doi: 10.1523/JNEUROSCI.2803-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu J, Mashimo T, Südhof TC. Synaptotagmin-1, -2, and -9: Ca(2+) sensors for fast release that specify distinct presynaptic properties in subsets of neurons. Neuron. 2007;54(4):567–581. doi: 10.1016/j.neuron.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 32.Rahamimoff R, et al. Multitude of ion channels in the regulation of transmitter release. Philos Trans R Soc Lond B Biol Sci. 1999;354(1381):281–288. doi: 10.1098/rstb.1999.0379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vacher H, Mohapatra DP, Trimmer JS. Localization and targeting of voltage-dependent ion channels in mammalian central neurons. Physiol Rev. 2008;88(4):1407–1447. doi: 10.1152/physrev.00002.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Martire M, et al. Pre-synaptic BK channels selectively control glutamate versus GABA release from cortical and hippocampal nerve terminals. J Neurochem. 2010;115(2):411–422. doi: 10.1111/j.1471-4159.2010.06938.x. [DOI] [PubMed] [Google Scholar]
- 35.Debanne D, Bialowas A, Rama S. What are the mechanisms for analogue and digital signalling in the brain? Nat Rev Neurosci. 2013;14(1):63–69. doi: 10.1038/nrn3361. [DOI] [PubMed] [Google Scholar]
- 36.Pittson S, Himmel AM, MacIver MB. Multiple synaptic and membrane sites of anesthetic action in the CA1 region of rat hippocampal slices. BMC Neurosci. 2004;5:52. doi: 10.1186/1471-2202-5-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bieda MC, MacIver MB. Major role for tonic GABAA conductances in anesthetic suppression of intrinsic neuronal excitability. J Neurophysiol. 2004;92(3):1658–1667. doi: 10.1152/jn.00223.2004. [DOI] [PubMed] [Google Scholar]
- 38.Oose Y, et al. Imbalanced suppression of excitatory and inhibitory synaptic transmission onto mouse striatal projection neurons during induction of anesthesia with sevoflurane in vitro. Eur J Neurosci. 2012;35(9):1396–1405. doi: 10.1111/j.1460-9568.2012.08065.x. [DOI] [PubMed] [Google Scholar]
- 39.Mashour GA. Top-down mechanisms of anesthetic-induced unconsciousness. Front Syst Neurosci. 2014;8:115. doi: 10.3389/fnsys.2014.00115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sonner JM, et al. Inhaled anesthetics and immobility: Mechanisms, mysteries, and minimum alveolar anesthetic concentration. Anesth Analg. 2003;97(3):718–740. doi: 10.1213/01.ANE.0000081063.76651.33. [DOI] [PubMed] [Google Scholar]
- 41.Jurd R, et al. General anesthetic actions in vivo strongly attenuated by a point mutation in the GABA(A) receptor beta3 subunit. FASEB J. 2003;17(2):250–252. doi: 10.1096/fj.02-0611fje. [DOI] [PubMed] [Google Scholar]
- 42.Zhang Y, et al. Gamma-aminobutyric acidA receptors do not mediate the immobility produced by isoflurane. Anesth Analg. 2004;99(1):85–90. doi: 10.1213/01.ANE.0000118108.64886.42. [DOI] [PubMed] [Google Scholar]
- 43.Liao M, et al. Beta3-containing gamma-aminobutyric acidA receptors are not major targets for the amnesic and immobilizing actions of isoflurane. Anesth Analg. 2005;101(2):412–418. doi: 10.1213/01.ANE.0000154196.86587.35. [DOI] [PubMed] [Google Scholar]
- 44.Herold KF, Hemmings HC., Jr Sodium channels as targets for volatile anesthetics. Front Pharmacol. 2012;3:50. doi: 10.3389/fphar.2012.00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Franks NP, Honoré E. The TREK K2P channels and their role in general anaesthesia and neuroprotection. Trends Pharmacol Sci. 2004;25(11):601–608. doi: 10.1016/j.tips.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 46.Study RE. Isoflurane inhibits multiple voltage-gated calcium currents in hippocampal pyramidal neurons. Anesthesiology. 1994;81(1):104–116. doi: 10.1097/00000542-199407000-00016. [DOI] [PubMed] [Google Scholar]
- 47.Westphalen RI, Hemmings HC., Jr Effects of isoflurane and propofol on glutamate and GABA transporters in isolated cortical nerve terminals. Anesthesiology. 2003;98(2):364–372. doi: 10.1097/00000542-200302000-00016. [DOI] [PubMed] [Google Scholar]
- 48.Cechova S, Zuo Z. Inhibition of glutamate transporters increases the minimum alveolar concentration for isoflurane in rats. Br J Anaesth. 2006;97(2):192–195. doi: 10.1093/bja/ael152. [DOI] [PubMed] [Google Scholar]
- 49.Nagele P, et al. Volatile anesthetics bind rat synaptic snare proteins. Anesthesiology. 2005;103(4):768–778. doi: 10.1097/00000542-200510000-00015. [DOI] [PubMed] [Google Scholar]
- 50.Wu XS, Sun JY, Evers AS, Crowder M, Wu LG. Isoflurane inhibits transmitter release and the presynaptic action potential. Anesthesiology. 2004;100(3):663–670. doi: 10.1097/00000542-200403000-00029. [DOI] [PubMed] [Google Scholar]
- 51.Ouyang W, Hemmings HC., Jr Depression by isoflurane of the action potential and underlying voltage-gated ion currents in isolated rat neurohypophysial nerve terminals. J Pharmacol Exp Ther. 2005;312(2):801–808. doi: 10.1124/jpet.104.074609. [DOI] [PubMed] [Google Scholar]
- 52.Joksovic PM, et al. Isoflurane-sensitive presynaptic R-type calcium channels contribute to inhibitory synaptic transmission in the rat thalamus. J Neurosci. 2009;29(5):1434–1445. doi: 10.1523/JNEUROSCI.5574-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rama S, Zbili M, Debanne D. Modulation of spike-evoked synaptic transmission: The role of presynaptic calcium and potassium channels. Biochim Biophys Acta. 2014;1853(9):1933–1939. doi: 10.1016/j.bbamcr.2014.11.024. [DOI] [PubMed] [Google Scholar]
- 54.Hochbaum DR, et al. All-optical electrophysiology in mammalian neurons using engineered microbial rhodopsins. Nat Methods. 2014;11(8):825–833. doi: 10.1038/nmeth.3000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hoppa MB, Gouzer G, Armbruster M, Ryan TA. Control and plasticity of the presynaptic action potential waveform at small CNS nerve terminals. Neuron. 2014;84(4):778–789. doi: 10.1016/j.neuron.2014.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Verhage M, et al. Differential release of amino acids, neuropeptides, and catecholamines from isolated nerve terminals. Neuron. 1991;6(4):517–524. doi: 10.1016/0896-6273(91)90054-4. [DOI] [PubMed] [Google Scholar]
- 57.Elliott EM, Malouf AT, Catterall WA. Role of calcium channel subtypes in calcium transients in hippocampal CA3 neurons. J Neurosci. 1995;15(10):6433–6444. doi: 10.1523/JNEUROSCI.15-10-06433.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Balaji J, Ryan TA. Single-vesicle imaging reveals that synaptic vesicle exocytosis and endocytosis are coupled by a single stochastic mode. Proc Natl Acad Sci USA. 2007;104(51):20576–20581. doi: 10.1073/pnas.0707574105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Solt K, Forman SA. Correlating the clinical actions and molecular mechanisms of general anesthetics. Curr Opin Anaesthesiol. 2007;20(4):300–306. doi: 10.1097/ACO.0b013e32816678a5. [DOI] [PubMed] [Google Scholar]
- 60.Akeju O, et al. Effects of sevoflurane and propofol on frontal electroencephalogram power and coherence. Anesthesiology. 2014;121(5):990–998. doi: 10.1097/ALN.0000000000000436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.MacIver MB. Anesthetic agent-specific effects on synaptic inhibition. Anesth Analg. 2014;119(3):558–569. doi: 10.1213/ANE.0000000000000321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhang Y, et al. Bidirectional modulation of isoflurane potency by intrathecal tetrodotoxin and veratridine in rats. Br J Pharmacol. 2010;159(4):872–878. doi: 10.1111/j.1476-5381.2009.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jinks SL, Bravo M, Hayes SG. Volatile anesthetic effects on midbrain-elicited locomotion suggest that the locomotor network in the ventral spinal cord is the primary site for immobility. Anesthesiology. 2008;108(6):1016–1024. doi: 10.1097/ALN.0b013e3181730297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lukatch HS, Kiddoo CE, Maciver MB. Anesthetic-induced burst suppression EEG activity requires glutamate-mediated excitatory synaptic transmission. Cereb Cortex. 2005;15(9):1322–1331. doi: 10.1093/cercor/bhi015. [DOI] [PubMed] [Google Scholar]
- 65.Kenny JD, Westover MB, Ching S, Brown EN, Solt K. Propofol and sevoflurane induce distinct burst suppression patterns in rats. Front Syst Neurosci. 2014;8:237. doi: 10.3389/fnsys.2014.00237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ratnakumari L, Hemmings HC., Jr Inhibition of presynaptic sodium channels by halothane. Anesthesiology. 1998;88(4):1043–1054. doi: 10.1097/00000542-199804000-00025. [DOI] [PubMed] [Google Scholar]
- 67.Ryan TA. Inhibitors of myosin light chain kinase block synaptic vesicle pool mobilization during action potential firing. J Neurosci. 1999;19(4):1317–1323. doi: 10.1523/JNEUROSCI.19-04-01317.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Miesenböck G, De Angelis DA, Rothman JE. Visualizing secretion and synaptic transmission with pH-sensitive green fluorescent proteins. Nature. 1998;394(6689):192–195. doi: 10.1038/28190. [DOI] [PubMed] [Google Scholar]
- 69.Kim SH, Ryan TA. A distributed set of interactions controls mu2 functionality in the role of AP-2 as a sorting adaptor in synaptic vesicle endocytosis. J Biol Chem. 2009;284(47):32803–32812. doi: 10.1074/jbc.M109.039149. [DOI] [PMC free article] [PubMed] [Google Scholar]