Abstract
Air pollution has become the world's single biggest environmental health risk, linked to around 7 million deaths in 2012 according to a recent World Health Organisation (WHO) report. The new data further reveals a stronger link between, indoor and outdoor air pollution exposure and cardiovascular diseases, such as strokes and ischemic heart disease, as well as between air pollution and cancer. The role of air pollution in the development of respiratory diseases, including acute respiratory infections and chronic obstructive pulmonary diseases, is well known. While both indoor and outdoor pollution affect health, recent statistics on the impact of household indoor pollutants (HAP) is alarming. The WHO factsheet on HAP and health states that 3.8 million premature deaths annually - including stroke, ischemic heart disease, chronic obstructive pulmonary disease (COPD) and lung cancer are attributed to exposure to household air pollution. Use of air cleaners and filters are one of the suggested strategies to improve indoor air quality. This review discusses the impact of air pollutants with special focus on indoor air pollutants and the benefits of air filters in improving indoor air quality.
KEY WORDS: Air filters, air pollution, cardiorespiratory health, enhancing indoor air quality, HEPA
INTRODUCTION
In order to extract 420 litres of oxygen that is crucial for human survival and function, a total of 10,000 litres of air enters the lungs every day. The quality of air we breathe determines the health of the lungs as well as other organs. Indeed clean air is considered to be a basic requirement of human health and well-being. However, air pollution continues to pose a significant threat to health worldwide. The World Health organization (WHO) reports that in 2012 around 7 million people died as a result of air pollution exposure confirming that air pollution is now the world's largest single environmental health risk.[1]
The impact of pollution on respiratory health is well known. The WHO factsheet reveal that, there exists a stronger link between air pollution exposure and cardiovascular diseases, such as strokes and ischemic heart disease, as well as between air pollution and cancer.[2] In the last decade, literature on the detrimental impacts of air pollution on brain, cognition and behavior has also exponentially increased.[3]
The multicenter European Study of Cohorts for Air Pollution Effects (ESCAPE) study- one of the largest ongoing studies initiated to assess the impact of air pollution on population health, involving 367,251 subjects, has generated significant data over the last 6 years. The results from the study, published in more than 25 publications, offers an insight into the correlation between air pollution and increases in cerebrovascular[4] and coronary[5] events besides an increase in respiratory illnesses.[6,7]
In the recently published analysis of the largest ever population based study on the distribution, causes and risk factors of a wide array of major diseases across the world, the Global Burden of Disease (GBD) study, exposure to air pollution and particulate matter was globally ranked as one of the top 10 risk factors for disease. More significant was the fact that household air pollution (HAP) was the leading risk factor for poor health in south Asia.[8]
The quality of air inside homes, offices, schools, day care centers, public buildings, health care facilities or other private and public buildings where people spend a large part of their life is an essential determinant of healthy life and people's well-being, says the WHO Guidelines for Indoor Air Quality.[9] Hazardous substances emitted from buildings, construction materials and indoor equipment or due to human activities indoors, such as combustion of fuels for cooking or heating, lead to a broad range of health problems.[9]
Air pollution and impact on health in India
As one of the world's most populous countries, India too has seen a significant rise in incidence of respiratory diseases such as asthma and COPD over the last decade. The burden of COPD in India has been estimated to be about 15 million cases (males and females contributing to 9.02 and 5.75 million, respectively), causing about 500,000 deaths per year.[10] The actual numbers are, however expected to be much higher. Most epidemiological studies in India have been based on respiratory symptom questionnaire. Use of spirometry to define COPD has shown a two-fold higher prevalence of COPD.[11]
India has 20-28 million asthmatics, with a prevalence of 10-15% among children, aged 5-11 years.[12] Indian study on epidemiology of asthma, respiratory symptoms and chronic bronchitis in adults (INSEARCH), a landmark epidemiological study conducted by the Indian Council of Medical Research (ICMR) found the overall prevalence of asthma and chronic bronchitis to be 2.05% (adults aged ≥15 years) and 3.49% (adults aged ≥35 years), respectively. The national burden of asthma and chronic bronchitis in this study was estimated at 17.23 and 14.84 million, respectively.[13]
Epidemiological survey in hospitals over three decades (1979-2009) in children under the age of 18 years, showed a steady rise in asthma prevalence from 9% to 25.5% -attributed not only to genetic predisposition but, more significantly to urbanization, air pollution and environmental tobacco smoke.[14] As with COPD, these numbers may not truly reflect the actual numbers.
Indeed, the rising prevalence of asthma, allergies, and COPD over the past few decades, has been attributed to an increase in environmental pollution- a price being paid for rapid industrialization, socio-economic development, urbanization, and changing lifestyles.[15]
THE SHORT- AND LONG-TERM EFFECTS OF AIR POLLUTION
Exposure to air pollution can lead to a wide range of short- and long-term effects [Figure 1]. Temporary short-term effects include discomfort such as irritation to the nose, throat, eyes, or skin or headaches, dizziness, and nausea. Air pollution can also cause respiratory conditions such as pneumonia or bronchitis.[16]
Figure 1.
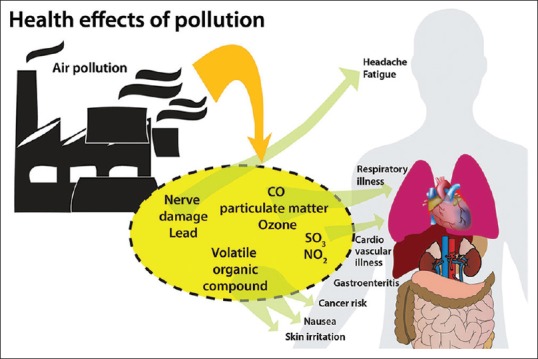
Health effects of air pollutants
Long-term effects of air include heart disease, lung cancer, and respiratory diseases. That air pollution can cause exacerbations of pre-existing asthma is supported by accumulating evidence over several decades. Particulate matter in air pollutants cause oxidative injury to the airways, leading to inflammation, remodelling, and increased risk of sensitization. On the other hand, while several pollutants have been linked to new-onset asthma, the strength of the evidence is variable.[17]
Consequently, persistent symptoms and frequent exacerbations, lead to increased medication use and considerable morbidity. Increased respiratory mortality has also been found in countries across the world, including Asian cities where researchers have demonstrated excess respiratory mortality risk with increases in particulate matter in the air.[18]
Several large studies suggest that pollutants exert significant effects on the cardiovascular system. It has been shown that for any increase in mortality caused by pollutants, two-thirds of the effect was accounted for by cardiovascular diseases.[18]
Chronic exposure to pollutants results in vascular inflammation leading to atherosclerosis. Acute exposure causes changes in coagulation and platelet activation. Increase in pollution has been linked to increased hospital admissions for congestive heart failure and ischemic heart disease [Figure 2].[18]
Figure 2.
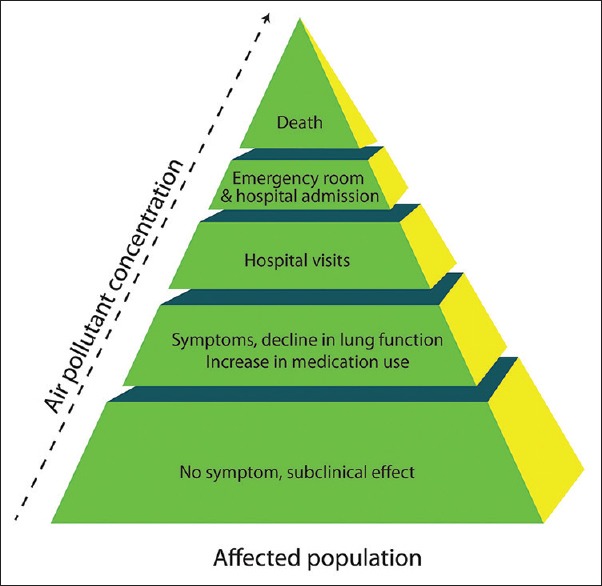
The burden of air pollutants on healthcare
Air pollution can also cause long-term damage to nerves, brain, kidneys, liver, and other organs. It is also believed that air pollutants cause birth defects.[16]
CONTAMINANTS OF INDOOR AIR
Indoor air pollution is a complex mixture of pollutants migrating indoors from outdoor air and pollutants generated by indoor sources.[19]
Documented evidence on indoor pollutants in the urban Indian environment is somewhat limited. It is however, very apparent that there has been continuous deterioration of ambient air and human health with the increase in population, industrialization, and urbanization.[20] Improper management of transport, primitive roads, high construction activity, and unplanned distribution of industries –all have led to an increase in the pollution levels.[20] Residential complexes adjacent to industries related to dyes, textiles, timber and furniture, handicrafts, metals, chemicals, sandstone quarries, steel rolling mills, guar gum, pulses and oil mills, etc., are responsible for a rise in a variety of indoor pollutants.[20] Increasing emission of toxic pollutants such as particulate matter (PM2.5, PM10) and green house gases like ozone (O3), sulphur dioxide (SO2), nitrous oxide (NO2), etc., has been reported from various cities. Burning of fossil fuels by humans also adds up to pollute the atmosphere.[20] Tobacco smoke has been well recognized as an indoor pollutant, with severe health risks to children and elderly.[21,22] There are also high levels of indoor pollutants in residential areas including emissions from cooking (biomass fuels), smoking, burning of mosquito coils, cigarettes, incense sticks, etc.[23] During festival days, such as Diwali, extensive burning of firecrackers takes place, especially in the evening hours, constituting a significant source of aerosols, black carbon (BC), organics, and trace gases.[24] Allergens from dust mites, cockroaches, fungi, pollens, pets cats/dogs, rodents are common in households.[23]
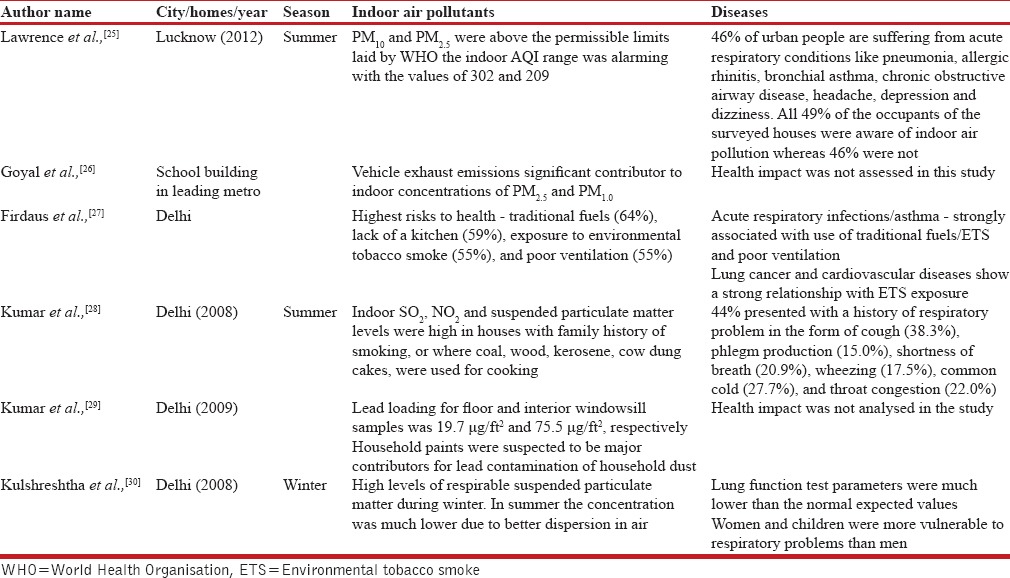
Table 1 provides an overview of a cross-section of studies on indoor pollutants conducted in Indian metros over the last decade and offers an insight into the health effects of indoor air pollution.
Table 1.
A summary of cross-section of studies from Indian metros on health impact of indoor air pollution
Classification of contaminants –Size matters
Pollutants are essentially particulate matter and are described by the “aerodynamic equivalent diameter” (AED). Particles of the same AED tend to have the same settling velocity. Particulate matter is subdivided into AED fractions based on how the particles are generated and where they deposit in human airways e.g: <10, <2.5, and <0.1 μm (PM10, PM2.5, and PM0.1, respectively).[18]
Particles with a diameter greater than 10 μm have a relatively small suspension half-life and are largely filtered out by the nose and upper airway.[18]
Those with a diameter between 2.5 and 10 μm (PM2.5-10) are classified as “coarse,” less than 2.5 μm as “fine,” and less than 0.1 μm as “ultrafine” particles.[18] Particles <10 μm in diameter (PM10) are capable of entering the respiratory system, and particles <2.5 μm (PM2.5) are capable of reaching the alveoli [Figure 3].[19] Ultrafine particles or nanoparticles which translocate to the circulation directly after inhalation, may systemically affect the blood, vasculature and organs such as the heart and even the brain.[31,32]
Figure 3.
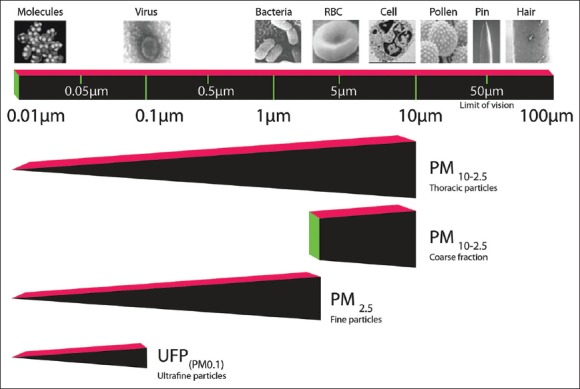
Characterization of particulate matter (PM) based on size. Particulate matter <10 μm (PM10) can enter the human thorax, whereas PM <2.5 μm (PM2.5) can reach the alveoli. RBC = Red blood cell
Contaminants of biological origin
Infectious pathogens, such as fungi, bacteria, and viruses, can be dispersed into the air in drops of moisture after coughing or sneezing. Droplet nuclei- small drops of moisture carrying infectious pathogens about 1-5μm in diameter remain suspended in the air for several hours by virtue of their size and are carried by air currents over considerable distances. When inhaled, they are small enough to bypass the protective mechanisms of the respiratory tract and settle in the lung where they may cause infection.[33]
Droplet nuclei are responsible for the airborne transmission of infectious diseases like tuberculosis (TB), influenza virus, chicken pox (varicella), measles (rubeola), and dessiminated herpes zoster.[33]
WAYS TO IMPROVING HEALTH – FILTRATION OF INDOOR AIR
Several measures are recommended to reduce exposure to contaminants of biological origin (e.g., dust mites, household pets, cockroaches, mould, and mice) and non-biological origin (e.g., environmental tobacco smoke, wood smoke, volatile organic compounds). With a better understanding of indoor pollutants, new and effective measures have evolved, including the development of indoor air filters.[34]
Air filtration is frequently recommended as a component of environmental control measures. Indoor air filtration can be provided by whole house filtration via the home's heating, ventilation, or air conditioning system, by portable room air cleaners, or a combination of the two.[3,34]
The key attribute of any air filter, is a balance of the following:[34]
Air flow to assure adequate ventilation
Efficiency to filter out a range of small particle sizes, and
Capacity to allow for reasonable cost-effective maintenance schedules without adversely affecting airflow and efficiency.
Currently available air purifiers usually use a multilayer filter system composed, often of a prefilter, a carbon filter, an antibacterial filter, and a HEPA filter.
The use of HEPA filters traditionally used in hospitals, has indeed been a significant inclusion to home air purifiers. A HEPA filter uses mechanical filtration to remove airborne particles. A HEPA filter is standardized at a minimum 99.97% efficiency rating for removing particles greater than or equal to 0.3μm (1/83,000 of an inch) in diameter. This means that for every 10,000 particles that are 0.3μm in diameter, 3 will pass through the filter, and the rest will be trapped by the filter.[33]
Efficacy of indoor air filters
A study by van der Heide et al.,[35] assessed the efficacy of air-cleaners with respect to their capacity to capture airborne allergen particles. Over a 6-month period, the efficacy of air filters to capture particulate matter and allergens was measured. The study included three interventions -application of active air-cleaners in living-rooms and bedrooms, placebo air-cleaners used in combination with allergen-impermeable mattress covers or active air-cleaners used in combination with allergen-impermeable mattress covers.
Allergen levels in mattress and floor dust were measured before, and 3 and 6 months after the interventions. After 6 months, the air-cleaners were dismantled and the filters were analysed for the amount of dust collected and allergen content.
In the air-cleaners, the air was filtered first by a coarse pre-filter, followed by a Rota-filter, in which small dust particles were captured by rotation at high speed. The last filter consisted of a high efficiency particulate air (HEPA)-type filter, filtering 70% of 0.3-μm particles and 95% of 1.0-μm particles. The air cleaners in this study clearly showed the capacity to capture substantial amounts of airborne dust particles and airborne allergens.
Another study, a randomized controlled trial, evaluated the effectiveness of free-standing air filters and window air conditioners (ACs) in 126 low-income households of children with asthma. Indoor air quality (IAQ) was monitored for week-long periods over three to four seasons. High concentrations of particulate matter (PM) and carbon dioxide were frequently seen.[36] When IAQ was monitored, filters reduced PM levels in the child's bedroom by an average of 50%. A similar study by Du et al.[37] found reduction in PM, by an average of 69 to 80% suggesting that while PM levels in homes with asthmatic children can be high, levels can be dramatically reduced using filters.
The benefits of capturing large amount of allergens and dust particles by the air cleaners reflect in improved respiratory function.
Air filters improve respiratory health
In a year-long, randomized, parallel-group study, Francis et al., measured the clinical outcomes for the use of indoor HEPA air cleaners of 30 adult asthmatics who were sensitized to, yet lived with an indoor cat or dog.[38] Primary end points in combined asthma outcomes (bronchial reactivity and treatment requirements) were statistically improved in the treatment group over the controls.
Another study by Sulser et al., compared sham versus HEPA portable room air cleaners (PRACs) in 36 asthmatic children sensitized to cat or dog.[39] A significant reduction in nocturnal symptoms including stuffy nose was observed in the HEPA filter group. There was also a trend toward an improvement in bronchial hyper-responsiveness- seen as a decrease in delta FEV1 (comparing FEV1 before and after cold air challenge) as opposed to an increase in the sham group.
Another double blind, placebo-controlled, cross-over study by Van der Heide et al.[40] compared the effects of air cleaners for 3 months with that of sham air cleaners. Within a short period of intervention of 3 months with active air cleaners, airway hyper-responsiveness, expressed by PC20 adenosine, was significantly diminished compared with baseline values. Peak flow amplitude also decreased (P =0.045).
Pedroletti et al.[41] studied 22 patients (12 to 33 years) with mild to moderate asthma, sensitized to cat or dog, dust mite, birch tree pollen, or a combination of these allergens. The device tested, provided laminar airflow of cooled, HEPA-filtered air directed to the sleep breathing zone (SBZ). At the end of 10 weeks, the treatment group showed improvement in the mini-Asthma Quality of Life Questionnaire (P < 0.05) –with benefits seen within the first 2 weeks of treatment.
Air filters have a positive impact on vascular health
Exposure to particulate matter is associated with risk of cardiovascular events, as a consequence of oxidative stress and systemic inflammation leading to endothelial dysfunction.[42,43]
The effects of controlled exposure to indoor air particles on micro vascular function (MVF) were studied in a healthy elderly population, of 21 non-smoking couples.[42] In this study the participants were subjected to two consecutive 48-hour exposures to either particle-filtered or non-filtered air (2,533-4,058 and 7,718-12,988 particles/cm3, respectively) in their homes.
MVF was assessed non-invasively by measuring digital peripheral artery tone after arm ischemia. Indoor air filtration significantly improved MVF by 8.1% (95% confidence interval, 0.4-16.3%). The study suggested that MVF was significantly associated with personal exposure to iron, potassium, copper, zinc, arsenic, and lead in the fine fraction. Reduction of particle exposure by filtration of recirculated indoor air for only 48 hours improved MVF in healthy elderly citizens, suggesting that this may be a feasible way of reducing the risk of cardiovascular disease
To assess the impact of portable air filters on particle exposures and endothelial function among healthy adults in a woodsmoke-impacted community, 45 healthy adults were exposed to consecutive 7-day periods of filtered and non-filtered air, in a randomized cross-over intervention study.[43]
Air filters reduced indoor fine particle concentrations by 60%. Filtration was associated with a 9.4% (95% confidence interval, 0.9-18%) increase in reactive hyperemia index and a 32.6% (4.4-60.9%) decrease in C-reactive protein. These two studies by Brauner et al. and Allen et al., support the hypothesis that systemic inflammation and impaired endothelial function, both predictors of cardiovascular morbidity, can be favorably influenced by reducing indoor particle concentrations.
In one of the recent studies by Weichenthal et al.[44] the benefits of an electrostatic air filter was assessed in 37 residents from 20 homes. The indoor PM2.5 decreased substantially during the period when air filter was used relative to placebo (mean difference: 37 μg/m3, 95% CI: 10, 64). On average, air filter use was associated with a 7.9 mmHg (95% CI: -17, 0.82) decrease in systolic blood pressure, and a 4.5-mm Hg (95% CI: -11, 2.4) decrease in diastolic blood pressure.
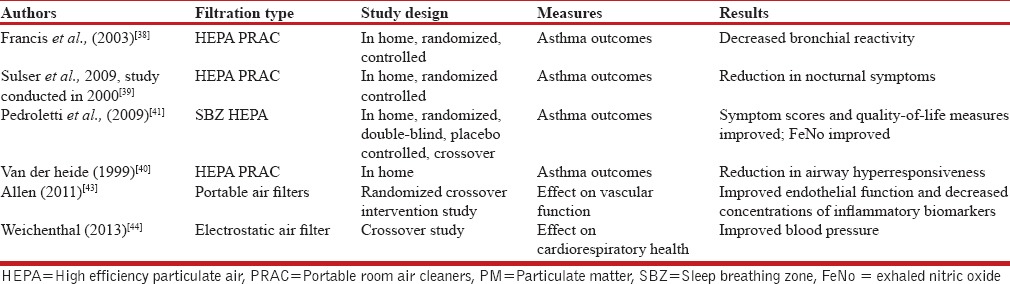
Table 2 summarizes the studies on impact of air filters on cardiac and respiratory health.
Table 2.
The impact of air filters on cardiorespiratory health
SUMMARY AND CONCLUSIONS
Despite the rapid rise in environmental pollutants, the causal pathways leading to adverse health effects is often complex and poorly understood.
Children, the elderly, and women are most vulnerable to potential indoor air pollution health effects because they spend more time in the home environment.
There are many sources of indoor air pollution. Air pollution inside homes consists of a complex mixture of agents penetrating from ambient (outdoor) air and agents generated by indoor sources. Indoor pollutants can vary in their potential health effects and intensity, as well as in their distribution across geographic areas, cultural backgrounds, and socioeconomic status. Exposure to indoor air pollutants can cause health effects ranging from sneezing and coughing to exacerbation of chronic respiratory disorders such as asthma and outcomes such as cardiovascular disease and even cancer.
Studies appear to suggest, that reduction in particulate matter and allergens results in reducing symptoms and in certain cases, preventing disease progression across all age groups, including the elderly and children. The evidence is apparent, in chronic respiratory diseases, such as asthma and in cardiovascular health.
Reduction in particulate matter and allergens is achieved successfully through efficient air filters. The British Guideline on Asthma Management from the British Thoracic Society recommends use of air filters for removal of pet and other allergens.[45]
Technologically advanced air filter systems are now available which efficiently remove particulate matter, resulting in significant health benefits to patients of asthma and cardiovascular disease. Cost-benefit studies are currently not available; however, such studies are required in countries like India for assessing the utility of universal application of these devices.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ambient (outdoor) Air Quality and Health, Fact Sheet No. 313. World Health Organisation. [Last accessed on 2015 Aug 20]. Available from: http://www.who.int/mediacentre/factsheets/fs313/en/
- 2.Household Air Polluton and Health, Fact Sheet No. 292. World Health Organisation. [Last accessed on 2015 Aug 20]. Available from: http://www.who.int/mediacentre/factsheets/fs292/en/
- 3.Suades-González E, Gascon M, Guxens M, Sunyer J. Air Pollution and Neuropsychological Development: A Review of the Latest Evidence. Endocrinology. 2015 doi: 10.1210/en.2015-1403. en20151403 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stafoggia M, Cesaroni G, Peters A, Andersen ZJ, Badaloni C, Beelen R, et al. Long-term exposure to ambient air pollution and incidence of cerebrovascular events: Results from 11 european cohorts within the escape project. Environ Health Perspect. 2014;122:919–25. doi: 10.1289/ehp.1307301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cesaroni G, Forastiere F, Stafoggia M, Andersen ZJ, Badaloni C, Beelen R, et al. Long term exposure to ambient air pollution and incidence of acute coronary events: Prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE project. BMJ. 2014;348:f7412. doi: 10.1136/bmj.f7412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.MacIntyre EA, Gehring U, Mölter A, Fuertes E, Klümper C, Krämer U, et al. Air pollution and respiratory infections during early childhood: An analysis of 10 European birth cohorts within the ESCAPE Project. Environ Health Perspect. 2014;122:107–13. doi: 10.1289/ehp.1306755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gehring U, Gruzieva O, Agius RM, Beelen R, Custovic A, Cyrys J, et al. Air pollution exposure and lung function in children: The ESCAPE project. Environ Health Perspect. 2013;121:1357–64. doi: 10.1289/ehp.1306770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO Guidelines for indoor air quality: Selected pollutants. [Last accessed on 2014 Sep 12]. Available from: http://www.euro.who.int/__data/assets/pdf_file/0009/128169/e94535.pdf .
- 10.Gupta D, Agarwal R, Aggarwal AN, Maturu VN, Dhooria S, Prasad KT, et al. S.K. Jindal for the COPD Guidelines Working Group. Guidelines for diagnosis and management of chronic obstructive pulmonary disease: Joint ICS/NCCP (I) recommendations. Lung India. 2013;30:228–67. doi: 10.4103/0970-2113.116248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salvi S, Agrawal A. India needs a national COPD prevention and control programme. J Assoc Physicians India. 2012;60(Suppl):5–7. [PubMed] [Google Scholar]
- 12.Gaude GS, Hattiholi J, Chaudhury A. Role of health education and self-action plan in improving the drug compliance in bronchial asthma. J Family Med Prim Care. 2014;3:33–8. doi: 10.4103/2249-4863.130269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jindal SK, Aggarwal AN, Gupta D, Agarwal R, Kumar R, Kaur T, et al. Indian study on epidemiology of asthma, respiratory symptoms and chronic bronchitis in adults (INSEARCH) Int J Tuberc Lung Dis. 2012;16:1270–7. doi: 10.5588/ijtld.12.0005. [DOI] [PubMed] [Google Scholar]
- 14.Paramesh H. Epidemiology of asthma in India. Indian J Pediatr. 2002;69:309–12. doi: 10.1007/BF02723216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Upadhyay RP. An overview of the burden of non-communicable diseases in India. Iran J Public Health. 2012;41:1–8. [PMC free article] [PubMed] [Google Scholar]
- 16. [Last accessed on 2015 Mar 6]. Available from: http://www.education.nationalgeographic.com/education/encyclopedia/air-pollution/?ar_a=1 .
- 17.Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014;383:1581–92. doi: 10.1016/S0140-6736(14)60617-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anderson JO, Thundiyil JG, Stolbach A. Clearing the air: A review of the effects of particulate matter air pollution on human health. J Med Toxicol. 2012;8:166–75. doi: 10.1007/s13181-011-0203-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diette GB, McCormack MC, Hansel NN, Breysse PN, Matsui EC. Environmental issues in managing asthma. Respir Care. 2008;53:602–17. [PMC free article] [PubMed] [Google Scholar]
- 20.Rumana HS, Sharma RC, Beniwal V, Sharma AK. A retrospective approach to assess human health risks associated with growing air pollution in urbanized area of Thar Desert, western Rajasthan. J Environ Health Sci Eng. 2014;12:23. doi: 10.1186/2052-336X-12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patra S, Sharma S, Behera D. Passive smoking, indoor air pollution and childhood tuberculosis: A case control study. Indian J Tuberc. 2012;59:151–5. [PubMed] [Google Scholar]
- 22.King BA, Mirza SA, Babb SD. GATS Collaborating Group. A cross-country comparison of secondhand smoke exposure among adults: Findings from the Global Adult Tobacco Survey (GATS) Tob Control. 2013;22:e5. doi: 10.1136/tobaccocontrol-2012-050582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singh P, Kaur M, John S. Assessment of human health effects associated with exposure to indoor air pollution. Int J Appl Engineer Res. 2012;7:1–5. [Google Scholar]
- 24.Yerramsetti VS, Sharma AR, Gauravarapu Navlur N, Rapolu V, Dhulipala NS, Sinha PR. The impact assessment of Diwali fireworks emissions on the air quality of a tropical urban site, Hyderabad, India, during three consecutive years. Environ Monit Assess. 2013;185:7309–25. doi: 10.1007/s10661-013-3102-x. [DOI] [PubMed] [Google Scholar]
- 25.Lawrence A, Fatima N. Urban air pollution and its assessment in Lucknow City--the second largest city of North India. Sci Total Environ. 2014:488–489. doi: 10.1016/j.scitotenv.2013.10.106. 447-55. [DOI] [PubMed] [Google Scholar]
- 26.Goyal R, Khare M. Indo air quality modelling for PM 10, PM 2.5, PM 2.5, and PM 1.0 in naturally ventilated classrooms of an urban Indian school building. Environ Monit Assess. 2011;176:501–16. doi: 10.1007/s10661-010-1600-7. [DOI] [PubMed] [Google Scholar]
- 27.Firdaus G, Ahmad A. Indoor air pollution and self-reported diseases - A case study of NCT of Delhi. Indoor Air. 2011;21:410–6. doi: 10.1111/j.1600-0668.2011.00715.x. [DOI] [PubMed] [Google Scholar]
- 28.Kumar R, Nagar JK, Kumar H, Kushwah AS, Meena M, Kumar P, et al. Indoor air pollution and respiratory function of children in Ashok Vihar, Delhi: An exposure-response study. Asia Pac J Public Health. 2008;20:36–48. doi: 10.1177/1010539507308248. [DOI] [PubMed] [Google Scholar]
- 29.Kumar A, Scott Clark C. Lead loadings in household dust in Delhi, India. Indoor Air. 2009;19:414–20. doi: 10.1111/j.1600-0668.2009.00605.x. [DOI] [PubMed] [Google Scholar]
- 30.Kulshreshtha P, Khare M, Seetharaman P. Indoor air quality assessment in and around urban slums of Delhi city, India. Indoor Air. 2008;18:488–98. doi: 10.1111/j.1600-0668.2008.00550.x. [DOI] [PubMed] [Google Scholar]
- 31.Sharman JE, Cockcroft JR, Coombes JS. Cardiovascular implications of exposure to traffic air pollution during exercise. QJM. 2004;97:637–43. doi: 10.1093/qjmed/hch104. [DOI] [PubMed] [Google Scholar]
- 32.Bonner JC. Nanoparticles as a potential cause of pleural and interstitial lung disease. Proc Am Thorac Soc. 2010;7:138–41. doi: 10.1513/pats.200907-061RM. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Health Quality Ontario. Air cleaning technologies: An evidence-based analysis. Ont Health Technol Assess Ser. 2005;5:1–52. [PMC free article] [PubMed] [Google Scholar]
- 34.Sublett JL. Effectiveness of air filters and air cleaners in allergic respiratory diseases: A review of the recent literature. Curr Allergy Asthma Rep. 2011;11:395–402. doi: 10.1007/s11882-011-0208-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van der Heide S, Kauffman HF, Dubois AE, de Monchy JG. Allergen reduction measures in houses of allergic asthmatic patients: Effects of air-cleaners and allergen-impermeable mattress covers. Eur Respir J. 1997;10:1217–23. doi: 10.1183/09031936.97.10061217. [DOI] [PubMed] [Google Scholar]
- 36.Batterman S, Du L, Mentz G, Mukherjee B, Parker E, Godwin C, et al. Particulate matter concentrations in residences: An intervention study evaluating stand-alone filters and air conditioners. Indoor Air. 2012;22:235–52. doi: 10.1111/j.1600-0668.2011.00761.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Du L, Batterman S, Parker E, Godwin C, Chin JY, O’Toole A, et al. Particle concentrations and effectiveness of free-standing air filters in bedrooms of children with asthma in Detroit, Michigan. Build Environ. 2011;46:2303–13. doi: 10.1016/j.buildenv.2011.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Francis H, Fletcher G, Anthony C, Pickering C, Oldham L, Hadley E, et al. Clinical effects of air filters in homes of asthmatic adults sensitized and exposed to pet allergens. Clin Exp Allergy. 2003;33:101–5. doi: 10.1046/j.1365-2222.2003.01570.x. [DOI] [PubMed] [Google Scholar]
- 39.Sulser C, Schulz G, Wagner P, Sommerfeld C, Keil T, Reich A, et al. Can the use of HEPA cleaners in homes of asthmatic children and adolescents sensitized to cat and dog allergens decrease bronchial hyper responsiveness and allergen contents in solid dust? Int Arch Allergy Immunol. 2009;148:23–30. doi: 10.1159/000151502. [DOI] [PubMed] [Google Scholar]
- 40.van der Heide S, van Aalderen WM, Kauffman HF, Dubois AE, de Monchy JG. Clinical effects of air cleaners in homes of asthmatic children sensitized to pet allergens. J Allergy Clin Immunol. 1999;104:447–51. doi: 10.1016/s0091-6749(99)70391-x. [DOI] [PubMed] [Google Scholar]
- 41.Pedroletti C, Millinger E, Dahlén B, Söderman P, Zetterström O. Clinical effects of purified air administered to the breathing zone in allergic asthma: A double-blind randomized cross-over trial. Respir Med. 2009;103:1313–9. doi: 10.1016/j.rmed.2009.03.020. [DOI] [PubMed] [Google Scholar]
- 42.Bräuner EV, Forchhammer L, Møller P, Barregard L, Gunnarsen L, Afshari A, et al. Indoor particles affect vascular function in the aged: An air filtration-based intervention study. Am J Respir Crit Care Med. 2008;177:419–25. doi: 10.1164/rccm.200704-632OC. [DOI] [PubMed] [Google Scholar]
- 43.Allen RW, Carlsten C, Karlen B, Leckie S, van Eeden S, Vedal S, et al. An air filter intervention study of endothelial function among healthy adults in a woodsmoke-impacted community. Am J Respir Crit Care Med. 2011;183:1222–30. doi: 10.1164/rccm.201010-1572OC. [DOI] [PubMed] [Google Scholar]
- 44.Weichenthal S, Mallach G, Kulka R, Black A, Wheeler A, You H, et al. A randomized double-blind crossover study of indoor air filtration and acute changes in cardiorespiratory health in a First Nations community. Indoor Air. 2013;23:175–84. doi: 10.1111/ina.12019. [DOI] [PubMed] [Google Scholar]
- 45.British Guideline on the Management of Asthma, British Thoracic Society May 2008, revised May 2011. [Last accessed on 2014 Jul 21]. Available from: https://www.brit-thoracic.org.uk/document-library/clinical-information/asthma/btssign-asthma-guideline-2011 .


