Abstract
Multiple myeloma is a malignant neoplasm of plasma cell origin that mainly affects bone marrow and skeletal system, producing large amount of light chain immunoglobulins. Pleural involvement in multiple myeloma is a rare complication which carries very poor prognosis. We report a case of multiple myeloma who presented with recurrent pleural effusion that was evaluated by means of thoracoscopy.
KEY WORDS: Multiple myeloma, pleural effusion, rigid thoracoscopy
INTRODUCTION
Multiple myeloma (MM) is a malignant proliferation of β-type of plasma cells, that mainly affects bone marrow and skeletal system, replacing the normal bone marrow with production of large amount of light chain immunoglobulins.[1] Accumulation of these proteins in vital organs such as kidneys and heart resulting in disease manifestation.
Pleural effusion in MM is a rare manifestation of the disease carrying grave prognosis and is mainly due to benign causes such as cardiac failure, renal failure, hypoalbuminemia, amyliodiosis, etc.[2] Myelomatous pleural involvement is a very rare manifestation of the disease and present in <1% of the cases.[3]
We present a case of multiple myeloma, who presented to us with recurrent exudative pleural effusion.
CASE REPORT
A 45-year-old male smoker was referred to our center with recurrent lymphocytic exudative pleural effusion. He was already on antitubercular treatment for past 2 months but was not responding to it. He had already been aspirated for effusion thrice before he was referred to our center.
He was having complains of loss of appetite, weight loss and fatigue since 4 months. Pulmonary symptoms of breathlessness, dull aching chest pain on right side and dry cough since 3 months. Otherwise the patient was normotensive and non-diabetic. There was no history of fever, hemoptysis or trauma to chest.
On examination, the patient was breathless with modified medical research council (MMRC) dyspnea scale of III with oxygen saturation of 93% at room air. His general physical examination was within normal except for subnormal body mass index (18.1 kg/m2). His jugular venous pressure was not raised. Respiratory system examination revealed reduced intensity of breath sounds on right side with dullness on percussion and decreased vocal resonance. Fine crepitations were present on lower lung fields of opposite lung. Other systemic examinations were unremarkable except for non-tender hepatomegaly.
Chest radiography confirmed that he had large right-sided pleural effusion [Figure 1]. Routine laboratory hematological tests revealed hemoglobin 11.1 mg/dl, slightly elevated WBCs (15300 cells/mm3) and raised ESR (89 mm/hr). His renal function tests were within normal limits. ECG revealed sinus tachycardia and ECHO was normal. Subsequent CECT thorax [Figure 2] showed right sided pleural effusion with marked pleural thickening, radiologically consistent with features of mesothelioma. Pleural fluid was thick, gelatinous and hemorrhagic in nature, which on re-evaluation showed high pleural fluid protein- 7.7 g/dl, sugar- 66 mg/dl and ADA- 33 U/L. Pleural fluid hematocrit was 1.2%. After risk benefit analysis, patient was considered for thoracoscopy and informed consent was taken before the procedure.
Figure 1.
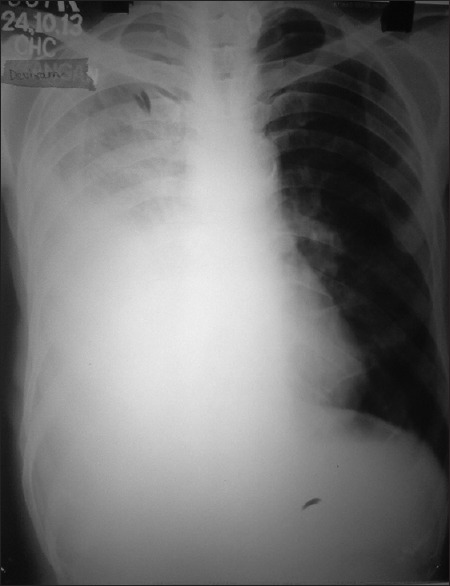
Chest radiograph showing homogenous opacity on right side with blunt CP angle, suggestive of massive right-sided pleural effusion
Figure 2.

CECT Chest showing right-sided massive pleural effusion with pleural thickening
During thoracoscopy, we found thickened non-smooth parietal pleura, dense pleuro-parenchymal adhesions along with red membranous glistening surface of the pleura and gelatinous nature of the fluid and septae [Figure 3]. Parietal pleural biopsy was taken and sent for histopathological analysis. On doing specific investigations, liver function tests revealed very high serum protein level (10.1 g/dl) with reversed albumin/globulin ratio of 0.2:1 (albumin 1.7 g/dl; globulin 8.4 g/dl). Urine for Bence-Jones proteins was positive. On serum electrophoresis, myeloma band was detected with high M-spike (6.95). Bone marrow aspirate was also thick and gelatinous, which constituted 30% of plasma cells. On cytological evaluation of pleural fluid, revealed presence of atypical plasma cells. Pleural biopsy revealed monotonous distribution of atypical plasma cells with basophilic cytoplasm, eccentric nuclei and prominent nucleoli, features were suggestive of pleural myeloma [Figure 4].
Figure 3.
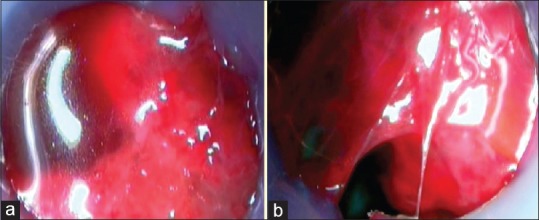
Thoracoscopic appearance of pleural cavity. (a) Gelatinous nature of pleural fluid (b) Glistening pleura and septae
Figure 4.
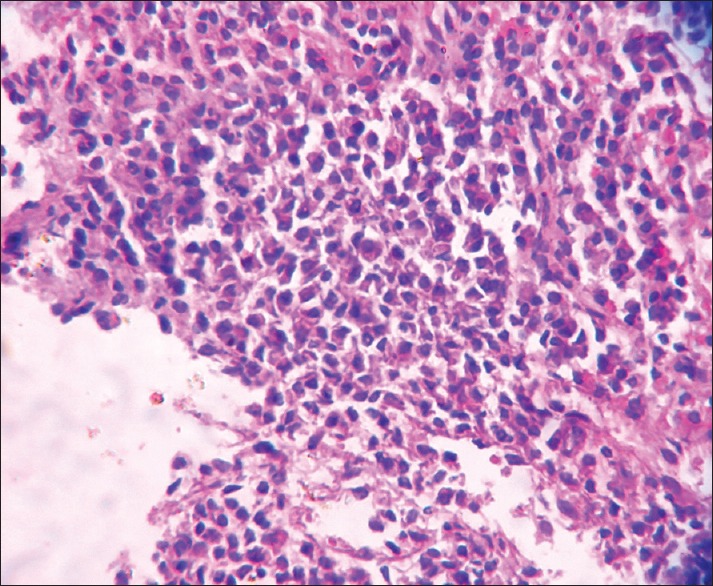
Photomicrograph of pleural biopsy showing monotonous distribution of plasma cells within the pleura (H and E, ×40)
DISCUSSION
Multiple myeloma is a neoplastic disorder caused by the proliferation of monoclonal plasma cells, associated with production of large amount of monoclonal immunoglobulins. Involvement of serous cavities in MM is very rare and documented sites of involvement are pleural cavity, peritoneal cavity and pericardium.[4]
Pleural effusion is a rare manifestation of MM. The first case of pleural effusion and involvement of serous cavities in multiple myeloma was reported in the Chest Journal in 1994 by Rodriguez et al.[5] Pleural effusion in MM is very unusual, occurs approximately in 6% of the cases during the natural course of disease, mainly due to benign and treatable causes. Malignant myelomatous involvement of the pleura is very rare, occurs in less than 1% of the cases[3] and less than 100 cases having been reported worldwide.[6] This can be due to direct extension from chest wall, invasion from adjacent skeletal structures or direct pleural involvement.
A diagnostic criteria was formed in 1994 by Rodriguez et al.,[5] three parameters were defined to confirm a myelomatous pleural effusion (a) Demonstration of a monoclonal protein in pleural fluid electrophoresis, (b) Detection of atypical plasma cells in the pleural fluid, and (c) Histologic confirmation with a pleural biopsy or by autopsy.
In our case, the atypical thoracocopic view which we had never encountered earlier along with high pleural fluid protein made us to rethink the initial clinical diagnosis of pleural tuberculosis for which he was kept on ATT. On searching the literature, we got the similar picture of bone marrow aspirate in a case of multiple myeloma.[7] Hence we went for specific investigations to confirm the diagnosis. Liver function tests revealed reversed Albumin: Globulin ratio, presence of Bence-Jones proteins in urine, myeloma band in serum electrophoresis, along with atypical plasma cells in pleural fluid and positive pleural biopsy confirmed the diagnosis of MM.
Presence of myelomatous pleural effusions is either a late complication of the disease in the natural course or an aggressive behavior of the disease and is associated with poor prognosis, with previous studies reporting median survival of less than 4 months.[8,9] This characteristic glistening pleura and gelatinous nature of fluid observed by thoracoscopy is probably being reported for the first time, as we could not get in literature. This gelatinous nature of the fluid is said to be because of increased levels of circulating serum immunoglobulins. The hyperviscosity seen in multiple myeloma is not due to myeloma cells in the blood stream. Proteins do not dissolve in a solution; they form a colloid which suspends the proteins within the moving bloodstream like sediment in a river. The more protein in a liquid, the more likely it is that the liquid will be viscous. The proteins (or protein parts) found in myeloma can vary in size. IgG, IgE, or IgD are thought of as single units, whereas IgA is a double unit and IgM is a pentamer. Hyperviscosity in multiple myeloma is mostly because of excess IgM and least likely if there is an excess IgG, IgE or IgD.[10]
CONCLUSIONS
In conclusion, the incidence of myelomatous pleural effusion is very rare, often signifying a poor prognostic outlook and this alarming thoracoscopic view which must be further explored on a larger case series, keeping multiple myeloma as one of the differential diagnosis.
Points to remember
Pleural myeloma is a rare entity (<1%) and <100 cases having been reported worldwide
Whenever suspected, serum and pleural fluid electrophoresis should be combined with pathological studies
Thoracoscopy showing ‘red membranous glistening pleura along with gelatinous nature of fluid and septae’, which has never been mentioned in the literature before
Increased viscocity of the body fluids is mainly because of high IgM, produced by plasma cells.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Kyle RA, Rajkumar SV. Plasma cell disorders. In: Goldman L, Ausiello DA, editors. Cecil Textbook of Medicine. 22nd ed. Philadelphia: WB Saunders; 2004. pp. 1184–95. [Google Scholar]
- 2.Miller J, Alton PA. Myelomatous pleural effusion - A case report. Respir Med Case Rep. 2012;5:59–61. doi: 10.1016/j.rmedc.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kintzer JS, Jr, Rosenow EC, 3rd, Kyle RA. Thoracic and pulmonary abnormalities in multiple myeloma: A review of 958 cases. Arch Intern Med. 1978;138:727–30. [PubMed] [Google Scholar]
- 4.Palmer HE, Wilson CS, Bardales RH. Cytology and flow cytometry of malignant effusions of multiple myeloma. Diagn Cytopathol. 2000;22:147–51. doi: 10.1002/(sici)1097-0339(20000301)22:3<147::aid-dc3>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 5.Rodríguez JN, Pereira A, Martínez JC, Conde J, Pujol E. Pleural effusion in multiple myeloma. Chest. 1994;105:622–4. doi: 10.1378/chest.105.2.622. [DOI] [PubMed] [Google Scholar]
- 6.Oudart JB, Maquart FX, Semouma O, Lauer M, Arthuis-Demoulin PA, Ramont L. Pleural effusion in a patient with multiple myeloma. Clin Chem. 2012;58:672–4. doi: 10.1373/clinchem.2010.160994. [DOI] [PubMed] [Google Scholar]
- 7.Kumar V, Abbas AK, Fausto N, Aster J. Diseases of white blood cells, lymph nodes, spleen and thymus. In: Kumar V, Abbas AK, Fausto N, Aster J, editors. Robbins and Cotran Pathologic Basis of Disease. 8th ed. Philadelphia: Saunders; 2010. p. 610. [Google Scholar]
- 8.Kamble R, Wilson CS, Fassas A, Desikan R, Siegel DS, Tricot G, et al. Malignant pleural effusion of multiple myeloma: Prognostic factors and outcome. Leuk Lymphoma. 2005;46:1137–42. doi: 10.1080/10428190500102845. [DOI] [PubMed] [Google Scholar]
- 9.Dhingra KK, Singhal N, Nigam S, Jain S. Unsuspected multiple myeloma presenting as bilateral pleural effusion-a cytological diagnosis. Cytojournal. 2007;4:17. doi: 10.1186/1742-6413-4-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Did You Know: What Causes Viscosity in Multiple Myeloma. [Last accessed on 08/May/15];International Myeloma Foundation. 2005 6:14. Available from: http://myeloma.org/ArticlePageaction?tabId = 1&menuId%20 = 0& queryPageId = 0&articleId = 1589 . [Google Scholar]


