Sir,
In India where tuberculosis still remains unabated, we often encounter a variety of other pulmonary disorders being mislabeled as tuberculosis.[1] Occasionally, erroneous labeling of pulmonary tuberculosis as some other disease occurs. Herein, we report the case of a 30-year-old female, who was erroneously diagnosed and treated for allergic bronchopulmonary aspergillosis (ABPA). She was subsequently found to have pulmonary tuberculosis. This case provided us an opportunity to discuss the current approach to diagnosis of ABPA. Diseases such as ABPA, which were once considered to be a rarity, have now been recognized to be a significant problem, because of the availability of better diagnostic technology and increasing awareness among pulmonary physicians.[2,3] With approximately one-third of the individuals with ABPA being mislabeled as tuberculosis in the past,[1,4] the current situation in India seems to be much better, owing to the significant research on this topic. However, whether these diseases are being diagnosed appropriately, remains a matter of serious concern.
A 30-year-old female presented to her physician four months ago, with a two-week history of dry cough and minimal mucoid expectoration. There was no fever, anorexia, weight loss, hemoptysis, wheeze, chest pain or breathlessness. She denied a past history of any medical illness, tuberculosis or bronchial asthma. A chest radiograph revealed opacity in the right lower lobe [Figure 1]. The tuberculin skin test and sputum for acid-fast bacillus (AFB) were negative. The skin prick test for Aspergillus fumigatus and Aspergillus flavus were positive. The total IgE and eosinophil count were 235 IU/mL and 650 cells/μL, respectively. Computed tomography (CT) of the chest showed patchy consolidation and subsegmental atelectasis. She was labeled as ABPA and oral methylprednisolone was started at a dose of 16 mg per day. No significant improvement was noted in her symptoms after two weeks, hence, the patient visited our chest clinic. She was further investigated. A. fumigatus specific IgE was negative (0.03 kUA/L), eosinophil count was 220 cells/μL, and the total IgE level was 310 IU/mL. Glucocorticoids were tapered and stopped. Sputum for AFB was repeated twice, and was negative. Radiological worsening was observed in the CT chest, with areas of consolidation, centrilobular nodules, and tree-in-bud appearance in the right lower lobe [Figure 2]. Centrilobular nodules were also seen in left lower lobe. The patient underwent flexible bronchoscopy and bronchoalveolar lavage (BAL). Acid-fast bacilli were detected in the BAL fluid, Xpert MTB/Rif was positive for Mycobacterium tuberculosis with no rifampin resistance. The patient was started on anti-tuberculosis therapy and significant improvement was noted after two weeks.
Figure 1.

Chest radiograph showing homogenous opacity in the right lower zone
Figure 2.
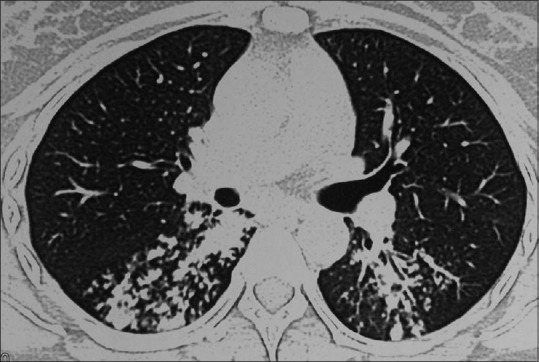
Computed tomography of the chest showing patchy consolidation, centrilobular nodules, and tree-in-bud opacities in both the lower lobes
The index case illustrates that several lessons need to be learnt in the diagnosis of ABPA. ABPA is an immunological disease, arising as a result of hypersensitivity to the antigens of A. fumigatus usually occurring in individuals with asthma (and cystic fibrosis).[5] The index patient lacked any predisposing factor for ABPA. Although ABPA does occur in patients without asthma, such an occurrence is rare.[6] Hence, in the absence of asthma, the diagnosis of ABPA should be made carefully.[5] Another caveat is, offering undue importance to the skin prick test in the diagnosis of ABPA. Immediate cutaneous hypersensitivity to the A. fumigatus antigen has a sensitivity of about 90% in the diagnosis of ABPA, whereas, demonstration of specific IgE against A. fumigatus >0.35 kUA/L is 100% sensitive.[7] Lack of standardization and improper techniques of performing the skin prick test for Aspergillus must also be considered as causes for the false negativity and positivity of this test.
The total eosinophil count in our patient was elevated; however, parasitic infestation and drugs are common causes of peripheral blood eosinophilia. Furthermore, the IgE levels were less than 500 IU/mL and this finding ruled out active ABPA as the cause of the patient's current symptoms.[8] In recent times, evidence-based, cut-off values have been found to differentiate asthmatics with and without ABPA, with 100% specificity (combination of total IgE > 2347 IU/mL, A. fumigatus specific IgE > 1.91 kUA/L, and eosinophil count > 507 cells/μL).[9] Several features that pointed toward an alternate diagnosis in the index patient have thus been overlooked. Finally, in patients with non-resolving pulmonary opacities and negative sputum microbiology, it is imperative that a flexible bronchoscopy (with BAL and lung biopsy) be performed in the diagnostic workup. Strict adherence to the currently available criteria to diagnose ABPA [Table 1] and a proper algorithmic approach [Figure 3] can avoid such problems in future.[5,10]
Table 1.
Criteria for diagnosis of allergic bronchopulmonary aspergillosis
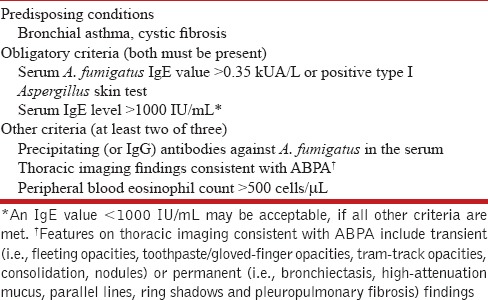
Figure 3.
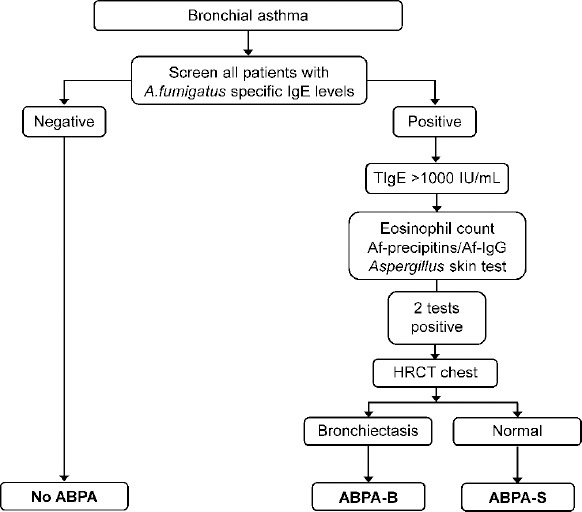
Suggested algorithm for the diagnosis of allergic bronchopulmonary aspergillosis
REFERENCES
- 1.Agarwal R, Gupta D, Aggarwal AN, Behera D, Jindal SK. Allergic bronchopulmonary aspergillosis: Lessons from 126 patients attending a chest clinic in north India. Chest. 2006;130:442-8. doi: 10.1378/chest.130.2.442. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal R, Chakrabarti A. Allergic bronchopulmonary aspergillosis in asthma: Epidemiological, clinical and therapeutic issues. Future Microbiol. 2013;8:1463-74. doi: 10.2217/fmb.13.116. [DOI] [PubMed] [Google Scholar]
- 3.Agarwal R, Denning DW, Chakrabarti A. Estimation of the burden of chronic and allergic pulmonary aspergillosis in India. PLoS One. 2014;9:e114745. doi: 10.1371/journal.pone.0114745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agarwal R, Gupta D, Aggarwal AN, Saxena AK, Chakrabarti A, Jindal SK. Clinical significance of hyperattenuating mucoid impaction in allergic bronchopulmonary aspergillosis: An analysis of 155 patients. Chest. 2007;132:1183–90. doi: 10.1378/chest.07-0808. [DOI] [PubMed] [Google Scholar]
- 5.Agarwal R, Chakrabarti A, Shah A, Gupta D, Meis JF, Guleria R, et al. Allergic bronchopulmonary aspergillosis: Review of literature and proposal of new diagnostic and classification criteria. Clin Exp Allergy. 2013;43:850–73. doi: 10.1111/cea.12141. [DOI] [PubMed] [Google Scholar]
- 6.Agarwal R, Aggarwal AN, Gupta D, Bal A, Das A. Case report: A rare cause of miliary nodules – allergic bronchopulmonary aspergillosis. Br J Radiol. 2009;82:e151–4. doi: 10.1259/bjr/20940804. [DOI] [PubMed] [Google Scholar]
- 7.Agarwal R, Maskey D, Aggarwal AN, Saikia B, Garg M, Gupta D, et al. Diagnostic performance of various tests and criteria employed in allergic bronchopulmonary aspergillosis: A latent class analysis. PLoS One. 2013;8:e61105. doi: 10.1371/journal.pone.0061105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agarwal R. Allergic bronchopulmonary aspergillosis. Chest. 2009;135:805–26. doi: 10.1378/chest.08-2586. [DOI] [PubMed] [Google Scholar]
- 9.Agarwal R, Aggarwal AN, Garg M, Saikia B, Chakrabarti A. Cut-off values of serum IgE (total and A. fumigatus -specific) and eosinophil count in differentiating allergic bronchopulmonary aspergillosis from asthma. Mycoses. 2014;57:659-63. doi: 10.1111/myc.12214. [DOI] [PubMed] [Google Scholar]
- 10.Dhooria S, Agarwal R. Diagnosis of allergic bronchopulmonary aspergillosis: A case-based approach. Future Microbiol. 2014;9:1195–208. doi: 10.2217/fmb.14.74. [DOI] [PubMed] [Google Scholar]


