Abstract
Background
Whether there are systematic sex differences in posttraumatic stress disorder (PTSD) symptom expression remains debated. Using methods based on item response theory (IRT), we aimed at examining differences in the likelihood of reporting DSM-IV symptoms of PTSD between women and men, while stratifying for major trauma type and equating for PTSD severity.
Method
We compared data from women and men in a large nationally representative adult sample, the National Epidemiologic Survey on Alcohol and Related Conditions. Analyses were conducted in the full population sample of individuals who met the DSM-IV criterion A (n = 23,860) and in subsamples according to trauma types.
Results
The clinical presentation of the 17 DSM-IV PTSD symptoms in the general population did not substantially differ in women and men in the full population and by trauma type after equating for levels of PTSD severity. The only exception was the symptom “foreshortened future”, which was more likely endorsed by men at equivalent levels of PTSD severity.
Limitations
The retrospective nature of the assessment of PTSD symptoms could have led to recall bias. Our sample size was too small to draw conclusions among individuals who experienced war-related traumas.
Conclusions
Our findings suggest that the clinical presentation of PTSD does not differ substantially between women and men. We also provide additional psychometric support to the exclusion of the symptom “foreshortened future” from the diagnostic criteria for PTSD in the DSM-5.
Keywords: posttraumatic stress disorder, symptoms, criteria, sex differences, item response theory (IRT), differential item functioning (DIF), national study
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) has moved posttraumatic stress disorder (PTSD) from the chapter on anxiety disorders to a new class of "trauma and stressor-related disorders" (American Psychiatric Association et al., 2013). This revision has brought to the fore considerations regarding expressions of distress as a result of traumatic experiences. These considerations are crucial because the nosological status of PTSD has important implications for the assessment and clinical management of patients with this disorder (Andreasen, 2010; Kilpatrick et al., 2013).
Epidemiological studies in general population samples have generally found that the prevalence of PTSD is higher in women than in men (Kessler et al., 1995; Pietrzak et al., 2011), leading several authors to hypothesize that sex may influence PTSD symptom expression (Carmassi et al., 2014; McLean et al., 2011; Stein et al., 2000; Weissman et al., 2005). Despite the clinical and research importance of this issue, studies examining the phenomenology of PTSD by sex are limited (Ditlevsen and Elklit, 2012; Peters et al., 2006; Stein et al., 2000). Determining whether there are sex differences in PTSD symptom expression could yet have potentially far-reaching implications for the clinical assessment and management of patients with PTSD, which still remains an underdiagnosed and undertreated condition (Bernardy et al., 2013; Felmingham and Bryant, 2012; Stenmark et al., 2014) .
While some studies have suggested that PTSD symptom expression in women and men are more similar than different (Chung and Breslau, 2008), others indicate that certain PTSD symptoms may differ between women and men (Breslau et al., 1999; He et al., 2014; Palm et al., 2009; Peters et al., 2006). Specifically, women may be more likely to endorse “memory lapses” of the stressful event (He et al., 2014), “feeling of detachment ” (He et al., 2014; Palm et al., 2009), “emotionally numb” (Breslau et al., 1999), “avoid conversations/places/people” (Breslau et al., 1999), “avoid thoughts” (Breslau et al., 1999; Peters et al., 2006), “difficulty sleeping” (Peters et al., 2006) and “exaggerated startled” (Palm et al., 2009; Peters et al., 2006), while men may be more likely to report a sense of “foreshortened future” (He et al., 2014; Palm et al., 2009), “intrusive thoughts” (He et al., 2014; Palm et al., 2009), “nightmares” (Palm et al., 2009) and “irritability” (Breslau et al., 1999; Palm et al., 2009). In addition, women may express more distress than men across almost all PTSD symptoms except for “hypervigilance” (Hourani et al., 2015).
However, prior research has often been limited by methodological constraints such as reliance on samples of convenience, incomplete assessment of full range of DSM-IV PTSD criteria, or lack of control for symptoms severity between groups. This last point is critical because sex differences in PTSD symptom expression reported in the literature may either reflect true phenomenological sex differences or result from differences in overall symptom severity between women and men (Peters et al., 2006). To our knowledge, only two studies (He et al., 2014; Palm et al., 2009) based on data from the National Comorbidity-Study Replication (NCS-R) (Kessler and Merikangas, 2004) have examined sex differences in PTSD symptom expression while adjusting for potential differences in PTSD severity between sexes. Their results suggest that women were more likely than men to endorse “feeling of detachment” (He et al., 2014; Palm et al., 2009) and “exaggerated startle » (Palm et al., 2009), whereas men were more likely to report a sense of “foreshortened future” (He et al., 2014; Palm et al., 2009), “intrusive thoughts” (He et al., 2014; Palm et al., 2009), “nightmares” (Palm et al., 2009) as well as “irritability” (Palm et al., 2009). However, prior work supports that PTSD symptom expression may vary according to trauma types (Breslau and Kessler, 2001; Cloitre et al., 2009; Stein et al., 2000). Because prevalence rates of several trauma types substantially differ between men and women (Tolin and Foa, 2006), these results support the need to examine whether PTSD symptom expression differ between women and men while stratifying by major trauma type.
Accordingly, using item response theory (IRT) methods (Lord and Novick, 1968) in a large nationally representative sample, our aim was to examine sex differences in the likelihood of reporting DSM-IV PTSD symptoms by major trauma type, when equating for levels of PTSD severity. IRT methods provide significant improvements for exploring differential symptom expression over previous statistical techniques as IRT approaches allow examining the likelihood that a particular symptom will be reported given a particular level of PTSD severity (Nicolas Hoertel et al., 2015; Hoertel et al., 2014; Peyre et al., 2012; Weinstock et al., 2010, 2009). We hypothesized that symptom features of PTSD substantially differ between women and men after adjusting for levels of PTSD severity, even when stratifying by major trauma type.
Methods
Sample
Data were drawn from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a nationally representative face-to-face survey of the US adult population, conducted in 2004–2005 by the National Institute on Alcoholism and Alcohol Abuse (NIAAA) and described in detail elsewhere (Grant et al., 2009; N. Hoertel et al., 2015). The second wave of NESARC was a representative sample of the civilian, non-institutionalized United States population, aged 20 years and older. The overall survey response rate was 70.2%, reflecting 34,653 completed interviews (Grant et al., 2009). Weighted data were adjusted to be representative of the civilian population on socio-demographic variables including region, age, race/ethnicity and sex, based on the 2000 Decennial Census. The research protocol, including informed consent procedures, received full human subjects review and approval from the US Census Bureau and the Office of Management and Budget (Grant et al., 2009).
Measures
PTSD symptoms and diagnosis and traumatic events were assessed using the Alcohol Use Disorder and Associated Disabilities Interview Schedule, DSM-IV version (AUDADIS-IV), a structured diagnostic instrument administered face to face by trained lay interviewers.
Assessment of lifetime DSM-IV symptoms of PTSD and major types of traumatic events
Respondents were asked about lifetime exposure to 27 different traumatic events (e.g., kidnapping, rape) (Kessler et al., 1995; Pietrzak et al., 2011). Participants who endorsed experiencing a traumatic event were asked about symptoms related to that event. If they reported more than one event, participants were asked about symptoms related to the worst event (Kessler et al., 1995; Pietrzak et al., 2011). Based on prior research (Breslau et al., 2006, 2004; Roberts et al., 2011), the traumatic events were grouped into six major categories: (1) “child maltreatment” (three items); (2) “interpersonal violence” (six items); (3) “war-related traumas” (four items); (4) “other injury or shocking event” (five items); (5) “learning of a trauma to a close friend or relative” (three items); and (6) “learning of an unexpected death” (one item). A total of 23,860 participants met DSM-IV criterion A for PTSD (i.e., had been exposed to a traumatic event and their response involved intense fear, helplessness, and/or horror). PTSD was diagnosed when respondents endorsed during at least 1 month (criterion E) at least 1 symptom within criterion B, at least 3 within criterion C, and at least 2 within criterion D, subsequent to the worst event they experienced that involved intense fear, helplessness, or horror, and the belief that they or someone close to them might die or be seriously injured or permanently disabled (Kessler et al., 1995; Pietrzak et al., 2011). PTSD diagnosis also required that the DSM-IV clinical significance criterion of impairment or distress (criterion F) be met (Pietrzak et al., 2011). Test-retest reliability of lifetime PTSD diagnoses was good (kappa=0.64) (Ruan et al., 2008).
Analyses for this study focused on the 17 DSM-IV PTSD symptoms. These symptoms are presented in Table 1. Only individuals who met DSM-IV criterion A for PTSD (i.e., had been exposed to a traumatic event and their response involved intense fear, helplessness, and/or horror) were included in our analyses, reflecting 14,632 women and 9,228 men.
TABLE 1.
Prevalence of DSM-IV symptoms of post-traumatic stress disorder (PTSD) by sex in the full sample, and in the subsample of individuals with a DSM-IV diagnosis of PTSD.
| DSM PTSD Symptoms | Full sample | Individuals with a DSM-IV diagnosis of PTSD | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Women N = 14632 |
Men N = 9228 |
p-value | Women N = 2644 |
Men N = 977 |
p-value | |
| % | % | % | % | |||
|
|
|
|
|
|
||
| Intrusive thoughts | 75.1 | 63.3 | <0.001 | 95.7 | 94.4 | 0.182 |
| Nightmares | 36.8 | 26.3 | <0.001 | 78.2 | 73.9 | 0.036 |
| Flashbacks | 29.8 | 19.6 | <0.001 | 69.7 | 64.8 | 0.020 |
| Distress by reminders/thoughts | 49.7 | 36.0 | <0.001 | 89.9 | 87.3 | 0.076 |
| Physiological reactivity | 22.0 | 13.9 | <0.001 | 63.0 | 56.6 | 0.017 |
| Avoid thoughts | 49.2 | 38.6 | <0.001 | 88.4 | 88.0 | 0.743 |
| Avoid conversations/places/people | 33.6 | 27.6 | <0.001 | 84.6 | 88.1 | 0.046 |
| Memory lapses | 15.8 | 11.7 | <0.001 | 47.1 | 45.5 | 0.456 |
| Anhedonia | 22.5 | 14.0 | <0.001 | 75.1 | 69.2 | 0.009 |
| Feeling of detachment | 20.5 | 12.5 | <0.001 | 76.6 | 71.7 | 0.010 |
| Emotionally numb | 13.1 | 8.4 | <0.001 | 56.8 | 58.3 | 0.534 |
| Foreshortened future | 7.1 | 5.6 | <0.001 | 31.1 | 41.1 | <0.001 |
| Difficulty sleeping | 32.6 | 20.0 | <0.001 | 83.7 | 80.42 | 0.095 |
| Irritability | 18.6 | 13.0 | <0.001 | 62.8 | 65.9 | 0.187 |
| Difficulty concentrating | 30.7 | 18.6 | <0.001 | 82.6 | 78.6 | 0.035 |
| Hypervigilance | 31.2 | 25.8 | <0.001 | 71.8 | 72.9 | 0.628 |
| Exaggerated startle | 17.3 | 10.9 | <0.001 | 57.4 | 51.9 | 0.025 |
|
| ||||||
| Diagnosis of PTSD | 17.2 | 9.4 | <0.001 | - | - | - |
Percentages are weighted values.
p-values in bold are statistically significant with p < .01.
Analyses
Comparing prevalence of PTSD symptoms
Sex differences in lifetime prevalence of each DSM-IV symptom of PTSD were tested using chi-square tests in both the full sample and the subsample of participants with a lifetime DSM-IV diagnosis of PTSD.
Assessing unidimensionality
Prior to IRT modeling, including testing for differential item functioning (DIF), it is necessary to confirm the unidimensionality of the set of symptoms, i.e., to assess whether all symptoms are part of the same underlying PTSD factor. Eigenvalue analysis of the tetrachoric correlation matrices of the 17 DSM-IV symptoms of PTSD (Table 1) was performed separately in women and men. A scree plot with an elbow after the first eigenvalue and a well-fitting one-factor model according to standard goodness of fit tests (RMSEA<.05, TLI>.95 and CFI>.95) were used to indicate unidimensionality.
Item response theory (IRT)
The IRT modeling was conducted to examine whether the DSM-IV symptoms of PTSD were endorsed similarly in women and men after adjusting for differences in underlying PTSD severity (Harford et al., 2013). A severity and a discrimination parameter are estimated for each symptom of PTSD indicating where along the latent severity continuum a symptom has a probability of 50% of being endorsed (for the severity parameter), and how rapidly the probability of observing the symptom changes across increasing levels of the latent severity continuum (for the discrimination parameter).
All factor analyses were conducted in Mplus Version 7.0 (Muthén and Muthén, 2007) which takes into account the NESARC sampling weights and design effects, in the parameter and standard error estimation as well as model fit calculations. The default estimator for the analysis was the variance adjusted weighted least squares (WLSMV), a robust estimator that does not assume normally distributed variables and provides the best option for modeling dichotomous observed variables such as the ones used in the present study (Muthén and Muthén, 2007).
Testing differential item functioning (DIF)
Multisample confirmatory factor analysis (MCFA) was used to test DIF across groups of (a) factor loadings (i.e., item discrimination parameters) and (b) thresholds (i.e., severity parameters). The different models varied in terms of the parameters constrained to be equal between groups (Millsap and Yun-Tein, 2004). Initially, an unconstrained model was fit allowing all parameters to differ between sexes (Table 2). Following a method previously described by McBride et al. (McBride et al., 2010), analyses were conducted iteratively to determine which IRT parameters differ between both groups. Nested models were compared using the chi-square difference test (implemented using the DIFFTEST option in Mplus (Muthén and Muthén, 2007). To detect DIF in IRT parameters of each item, the discrimination and severity parameters of the others items were constrained to be equal between groups. For each item, a chi-square difference test DIF comparing models with and without the discrimination parameter of the item constrained to be equal between groups was used to identify DIF in the discrimination parameter. To identify DIF in the severity parameter, a chi-square difference test DIF was used to compare models with and without the severity parameter of the item constrained to be equal between groups. Finally, Spearman’s correlation coefficients were calculated to examine whether the ranking of IRT severity and discrimination parameters was similar between sexes (Peyre et al., 2014).
TABLE 2.
Differential item functioning (DIF) of DSM-IV post-traumatic stress disorder (PTSD) symptoms by sex in the full sample and for 6 major trauma types.
| DSM PTSD Symptoms | Full sample | Child maltreatment | Interpersonal violence | War-related trauma | Other injury or shocking event | Learning of a trauma to a close friend or relative | Learning of an unexpected death | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Women: N=14632 Man: N=9228 |
Women: N=406 Man: N=211 |
Women: N=1648 Man: N=490 |
Women: N=54 Man: N=588 |
Women: N=4628 Man: N=3398 |
Women: N=4366 Man: N=2509 |
Women: N=3530 Man: N=2032 |
||||||||
|
| ||||||||||||||
| DIFa | DIFb | DIFa | DIFb | DIFa | DIFb | DIFa | DIFb | DIFa | DIFb | DIFa | DIFb | DIFa | DIFb | |
| Intrusive thoughts | − 0,01 | −0,13 | −0,34 | −0,35 | −0,20 | − 0,11 | 0,27 | 0,37 | − 0,03 | − 0,16 | −0,05 | −0,08 | 0,09 | −0,20 |
| Nightmares | −0,04 | 0,00 | −0,24 | 0,09 | −0,38 | − 0,02 | − 0,36 | 0,32 | − 0,04 | 0,01 | −0,06 | −0,04 | 0,00 | −0,08 |
| Flashbacks | − 0,09 | −0,01 | −0,35 | −0,05 | −0,36 | 0,20 | − 0,03 | 0,29 | − 0,02 | − 0,05 | − 0,27* | 0,09 | −0,05 | −0,18 |
| Distress by reminders/thoughts | 0,05 | −0,09 | −0,30 | −0,01 | −0,26 | 0,10 | 2,98 | 0,00 | 0,13 | − 0,07 | −0,05 | −0,08 | 0,12 | −0,24 |
| Physiological reactivity | 0,03 | −0,04 | −0,40 | −0,05 | −0,10 | 0,00 | 0,62 | 0,14 | 0,11 | −0,04 | −0,15 | 0,08 | 0,08 | −0,13 |
| Avoid thoughts | − 0,11 | 0,00 | −0,16 | 0,07 | − 0,35* | − 0,29 | 1,88 | 0,29 | − 0,16 | − 0,03 | −0,07 | −0,03 | −0,17 | 0,07 |
| Avoid conversations/places/people | − 0,05 | 0,17 | −0,34 | −0,19 | − 0,40* | − 0,19 | − 0,02 | 0,12 | − 0,09 | 0,08 | 0,02 | 0,31** | −0,18 | 0,36** |
| Memory lapses | 0,04 | 0,00 | −0,06 | 0,01 | −0,13 | 0,14 | −0,19 | 0,86 | 0,10 | 0,00 | −0,06 | 0,04 | 0,03 | −0,13 |
| Anhedonia | 0,09 | −0,08 | −0,03 | 0,28 | −0,44 | 0,32 | 1,70 | −0,77 | 0,09 | −0,01 | 0,13 | −0,14 | 0,12 | −0,09 |
| Feeling of detachment | 0,08 | −0,02 | −0,21 | 0,02 | −0,67 | 0,06 | 0,54 | − 0,11 | 0,12 | 0,03 | 0,09 | 0,03 | −0,07 | 0,09 |
| Emotionally numb | − 0,02 | 0,09 | −0,94 | 0,23 | −0,62 | 0,06 | 2,53 | − 0,26 | − 0,01 | 0,18 | 0,23 | 0,08 | −0,08 | 0,31** |
| Foreshortened future | − 0,23 | 0,35** | −1,62 | 0,63 | −0,17 | 0,52 * | 3,56 | − 0,54 | − 0,28 | 0,32 | −0,07 | 0,32** | −0,04 | 0,35** |
| Difficulty sleeping | − 0,08 | −0,09 | −0,01 | 0,12 | −0,04 | − 0,06 | − 0,45 | − 0,32 | 0,19 | − 0,08 | 0,01 | −0,15 | −0,19 | −0,15 |
| Irritability | − 0,04 | 0,10 | −0,90 | 0,21 | −0,26 | 0,14 | 0,24 | − 0,36 | − 0,04 | 0,16 | 0,05 | 0,05 | −0,29* | 0,30* |
| Difficulty concentrating | 0,03 | −0,12 | −0,62 | −0,07 | −0,60 | 0,06 | 1,29 | − 0,44 | 0,17 | − 0,20 | 0,10 | −0,07 | −0,15 | 0,02 |
| Hypervigilance | 0,04 | 0,10 | −0,19 | −0,22 | −0,08 | 0,13 | − 0,24 | − 0,11 | 0,03 | 0,05 | −0,05 | 0,22 | −0,03 | 0,23 |
| Exaggerated startle | 0,08 | −0,04 | −0,01 | −0,24 | −0,22 | − 0,02 | − 0,22 | 0,31 | 0,00 | − 0,09 | −0,03 | −0,07 | 0,05 | −0,11 |
| Spearman correlation | 0.82 | 0,98 | 0,50 | 0,97 | 0,85 | 0,97 | 0,27 | 0,87 | 0,81 | 0,99 | 0,87 | 0,96 | 0,86 | 0,94 |
| Cohen’s d (Man vs. Woman) | −0.381 | −0.174 | −0.966 | −0.111 | −0.201 | −0.380 | −0.475 | |||||||
Note: a = discrimination parameter estimate, b = severity parameter estimate.
Values in bold are statistically (*p < .05, **p < .01) and clinically significant (DIF > .25) (method described in the article).
Sampling weights and design effects of the NESARC were taken into account.
DIFFTEST a = comparing models with the factor loading free and fixed for the corresponding item.
DIFFTEST b = comparing models with the threshold respectively free and fixed for the corresponding it
Small differences in severity between groups could be statistically significant but may not be clinically meaningful (Strong et al., 2009). To minimize the number of false positives that could derive from the multiple comparisons conducted in this study, we decided a priori that only differences greater than 0.25 in symptom discrimination and severity, would be considered as clinically meaningful and would be tested (Steinberg and Thissen, 2006). Such differences in symptom severity can be interpreted as one quarter of the “standard unit difference between the values of the (underlying) trait necessary to have a 50–50 chance of responding positively in one group compared to another” (Steinberg and Thissen, 2006). Because graphical display is helpful in placing the “effect sizes in a practical and theoretical context” (Wilkinson, 1999), we present the item response curves (IRC) for all symptom parameters that reached our a priori threshold of both statistical and clinical significance. Minimum sample size for DIF analyses is usually considered in the range of 100–200 subjects per group. Based on a simulation study, Scott et al. (Scott et al., 2010) recommended a minimum of 200 participants per group to ensure adequate performance (i.e., 80% power).
Because PTSD symptom expression can be influenced by the type of traumatic exposure (Breslau and Kessler, 2001; Cloitre et al., 2009; Stein et al., 2000), we conducted these analyses in the full sample and in six subsamples according to major trauma types (i.e., “child maltreatment”, “interpersonal violence”, “war-related trauma”, “other injury or shocking event”, “learning of a trauma to a close friend or relative” and “learning of an unexpected death”).
Results
Symptoms of PTSD endorsement rates
In the full sample, the prevalence rates of all PTSD symptoms and DSM-IV PTSD diagnosis were significantly higher in women compared to men (Table 1). In the subsample of participants with a DSM-IV diagnosis of PTSD, the prevalence rates of “anhedonia” and “feeling of detachment” were significantly higher in women compared to men, whereas “foreshortened future” was significantly more frequently endorsed in men than in women (all p < .01) (Table 1). PTSD severity was significantly higher in women compared to men (Cohen’s d = 0.38 in the full sample and ranged from 0.11 (for “war-related traumas”) to 0.97 (for “interpersonal violence”) in subsamples) (Table 2).
Unidimensionality of symptoms of PTSD
In the full sample, fit indices indicated a very good fit of a single factor to the data (in men: first factor eigenvalue = 12.9, second factor eigenvalue = 1.1, CFI = 0.97, TLI = 0.97, RMSEA = 0.039; in women: first factor eigenvalue = 12.8, second factor eigenvalue = 1.0, CFI = 0.97, TLI = 0.97, RMSEA = 0.044). After stratifying by major trauma type, fit indices also indicated a good fit of a single factor to the data in the 6 subsamples (see Supplementary Table S1). We determined that these fit statistics were adequate to proceed to fitting IRT models.
IRT item parameters
In the full sample, the ranking of IRT parameters was similar between sex groups. Spearman’s correlation coefficients were 0.97 for severity parameters (differences of rank ≤3) and 0.90 for discrimination parameters (differences of rank ≤10) (Table 2). In the 6 trauma type subsamples, the ranking of IRT parameters was similar between sex groups for severity parameters (mean Spearman’s correlation coefficients were 0.95 (min = 0.87, max = 0.99)), and to a lesser extent for discrimination parameters (mean = 0.69, less than 0.80 for two trauma types, i.e., “child maltreatment” and “war-related trauma”).
Differential item functioning
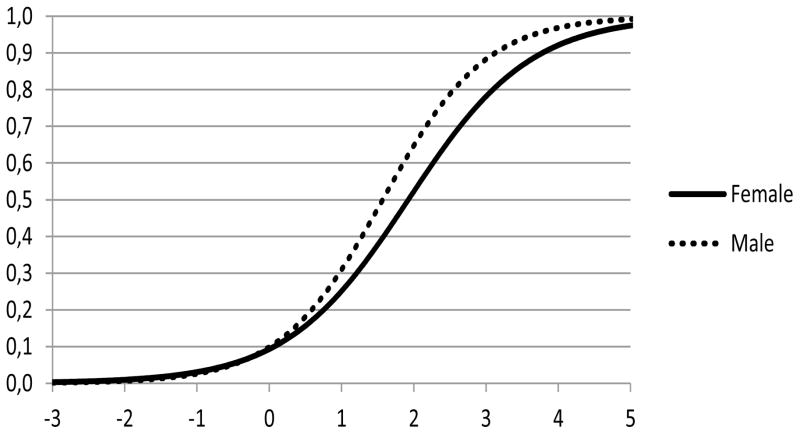
In the full sample, only one item out of 17 (i.e., “foreshortened future”) reached our a priori threshold for statistical and clinical significance in symptom severity (Table 2). Visual inspection of the item response curves (IRC) for this item indicated that men were consistently more likely than women to experience a sense of a “foreshortened future” at equivalent levels of PTSD severity (Figure 1). For 3 out of 6 trauma types (i.e., “interpersonal violence”, “learning of a trauma to a close friend or relative” and “learning of an unexpected death”), men were also more likely than women to experience a feeling of “foreshortened future” at equivalent levels of PTSD severity, in a clinically meaningful way (eFigures S1, S2 and S3). For the two trauma types “learning of a trauma to a close friend or relative” and “learning of an unexpected death”, men were more likely than women to “avoid conversations, places and/or people” at equivalent levels of PTSD severity (eFigures S4 and S5). There were no other items for these trauma types that reached our a priori threshold for statistical and clinical significance or whose item response curves displayed graphically substantial differences (eFigures S6 to S10).
FIGURE 1.
Differences in the probability of endorsing the symptom “foreshortened future” across levels of PTSD severity between women and men in the full sample of individuals (N = 23,860).
For the three other trauma types (i.e., “child maltreatment”, “war-related trauma” and “other injury or shocking event”), there were no significant DIF in symptom severity and discrimination parameters between women and men.
Discussion
The aim of the current study was to evaluate sex differences in the likelihood of reporting DSM-IV PTSD symptoms in a nationally representative sample using an IRT-based methodology, while stratifying by major trauma type. The benefit of the IRT-based approach is that it accounts for the potential confounding effect of PTSD severity in evaluating potential sex differences in symptom expression. Additional strengths of the present study include (i) the use of a large nationally representative sample, (ii) the incorporation in our analyses of information from the sampling methods of the survey design which has been suggested to substantially improve standard error estimates and tests of model fit (Asparouhov, 2005), (iii) the use of an a priori defined threshold of clinical significance so that emphasis was placed on differences that can be considered substantively clinically meaningful, and (iv) the stratification of analyses by major trauma type.
To our knowledge, although two studies (He et al., 2014; Palm et al., 2009) examined the specific contribution of sex to the expression of PTSD symptoms in a general population sample using IRT-based methodology, this study is the first to examine this issue while stratifying by major trauma type. Our findings suggest that the clinical presentation of PTSD symptoms does not differ substantially between women and men. Indeed, only one of the 17 PTSD symptoms (i.e., “foreshortened future”) reached our criteria for both clinical and statistical significance in the full sample. Ranging in size from small to medium in magnitude (Steinberg and Thissen, 2006), the direction of association suggested that men were more likely than women to experience a feeling of “foreshortened future” at equivalent levels of PTSD severity in a clinically meaningful way. This difference was also found in three trauma type subsamples (i.e., “interpersonal violence”, “learning of a trauma to a close friend or relative” and “learning of an unexpected death”), suggesting the robustness of this result. This finding, in line with those of two previous studies (He et al., 2014; Palm et al., 2009), suggests either a true sex difference in expression of PTSD or a sex-bias towards reporting this specific PTSD symptom. For example, while certain individuals may refer to a negative evaluation of what will happen in the future and are still able to distinguish past, present and future, others may experience an altered sense of time itself and temporal passage (Ratcliffe et al., 2014). As previously suggested (He et al., 2014; Palm et al., 2009), the interpretation of this item may vary by sex, supporting that a different severity cut-off score should be used in women and in men. This result also gives psychometric support to the exclusion of this symptom from the diagnostic criteria for PTSD in the DSM-5.
The symptom “avoid conversations/places/people” also reached our a priori threshold of both statistical and clinical significance for severity parameter in two trauma type subsamples (i.e., “learning of a trauma to a close friend or relative” and “learning of an unexpected death”). However, several lines of evidence argue against the clinical impact of this difference. First, there were no significant differences in severity parameter for this item in the full sample. Second, the sex differences in the ranking of the severity parameters for this symptom in the two subsamples were small (differences of rank ≤ 4). Last, the visual examination of the item response curves for the symptom “avoid conversations/places/people” in these two subsamples revealed a small nonuniform DIF (Figure S4 and S5), supporting that this difference is unlikely to be clinically meaningful.
Finally, we found that the prevalence rates of all PTSD symptoms as well as DSM-IV PTSD diagnosis were higher in women than in men. This finding is consistent with prior research derived from clinical or general population samples (Kawakami et al., 2014; Perkonigg et al., 2000; Pietrzak et al., 2011; Stein et al., 2000). Our results argue against the hypothesis that the higher prevalence of PTSD symptoms in women can be due to sex differences in the report of PTSD symptoms.
Our results should be interpreted in light of some limitations. A first limitation involves the retrospective nature of the assessment of PTSD symptoms that could have led to recall bias. Our findings should be further confirmed in national studies comparing prospectively PTSD symptoms by sex. Another limitation was that our sample size was too small to draw firm conclusions on sex differences in PTSD symptoms among individuals who experienced war-related traumas (Scott et al., 2010). Finally, our study examined specifically sex differences in the likelihood of reporting DSM-IV PTSD symptoms and the symptoms recently introduced in the DSM-5 (such as “persistent, distorted cognitions about the cause or consequences of the traumatic event that lead the individual to blame himself/herself or others”, “persistent negative emotional state (e.g., fear, horror, anger, guilt, or shame)” and “reckless or self-destructive behavior”) were not available in NESARC.
Conclusion
Despite these limitations, by addressing several constraints of prior research and using IRT-based methods, the present study suggests that the clinical presentation of PTSD symptoms does not substantially differ between women and men after stratifying by major trauma type and equating for levels of PTSD severity. The only exception was the symptom “foreshortened future” that was more likely endorsed by men at equivalent levels of PTSD severity. These findings give additional psychometric support to the exclusion of this symptom from the diagnostic criteria for PTSD in the DSM-5.
Supplementary Material
Highlights.
Examining differences in PTSD symptoms, between females and males, at same level of PTSD severity.
US adult sample: the National Epidemiologic Survey on Alcohol and Related Conditions.
Use of Item Response Theory.
The clinical presentation of PTSD symptoms does not substantially differ between genders.
The only exception was “foreshortened future”, more likely endorsed by men but removed from DSM-5.
Acknowledgments
Funding/support: supported by NIH grants MH076051 and MH082773 (Dr. Blanco), the New York State Psychiatric Institute (Drs. Blanco and Hoertel) and a fellowship grant from Public Health Expertise (Dr. Hoertel).
Footnotes
Conflicts of interest: Prof. Limosin is a member of the speakers/advisory boards for Janssen, Euthérapie, Lundbeck and Roche. Other authors report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association, American Psychiatric Association, DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Association; Arlington, Va: 2013. [Google Scholar]
- Andreasen NC. Posttraumatic stress disorder: a history and a critique. Ann N Y Acad Sci. 2010;1208:67–71. doi: 10.1111/j.1749-6632.2010.05699.x. [DOI] [PubMed] [Google Scholar]
- Asparouhov T. Sampling weights in latent variable modeling. Struct Equ Model- Multidiscip J - STRUCT EQU Model. 2005;12 doi: 10.1207/s15328007sem1203_4. [DOI] [Google Scholar]
- Bernardy NC, Lund BC, Alexander B, Jenkyn AB, Schnurr PP, Friedman MJ. Gender differences in prescribing among veterans diagnosed with posttraumatic stress disorder. J Gen Intern Med. 2013;28(Suppl 2):S542–548. doi: 10.1007/s11606-012-2260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, Peterson EL, Lucia VC. Vulnerability to assaultive violence: further specification of the sex difference in post-traumatic stress disorder. Psychol Med. 1999;29:813–821. doi: 10.1017/s0033291799008612. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC. The stressor criterion in DSM-IV posttraumatic stress disorder: an empirical investigation. Biol Psychiatry. 2001;50:699–704. doi: 10.1016/s0006-3223(01)01167-2. [DOI] [PubMed] [Google Scholar]
- Breslau N, Lucia VC, Alvarado GF. Intelligence and other predisposing factors in exposure to trauma and posttraumatic stress disorder: a follow-up study at age 17 years. Arch Gen Psychiatry. 2006;63:1238–1245. doi: 10.1001/archpsyc.63.11.1238. [DOI] [PubMed] [Google Scholar]
- Breslau N, Wilcox HC, Storr CL, Lucia VC, Anthony JC. Trauma exposure and posttraumatic stress disorder: a study of youths in urban America. J Urban Health Bull N Y Acad Med. 2004;81:530–544. doi: 10.1093/jurban/jth138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi C, Akiskal HS, Bessonov D, Massimetti G, Calderani E, Stratta P, Rossi A, Dell osso L. Gender differences in DSM-5 versus DSM-IV-TR PTSD prevalence and criteria comparison among 512 survivors to the L Aquila earthquake. J Affect Disord. 2014;160C:55–61. doi: 10.1016/j.jad.2014.02.028. [DOI] [PubMed] [Google Scholar]
- Chung H, Breslau N. The latent structure of post-traumatic stress disorder: tests of invariance by gender and trauma type. Psychol Med. 2008;38:563–573. doi: 10.1017/S0033291707002589. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stolbach BC, Herman JL, van der Kolk B, Pynoos R, Wang J, Petkova E. A developmental approach to complex PTSD: childhood and adult cumulative trauma as predictors of symptom complexity. J Trauma Stress. 2009;22:399–408. doi: 10.1002/jts.20444. [DOI] [PubMed] [Google Scholar]
- Ditlevsen DN, Elklit A. Gender, trauma type, and PTSD prevalence: a re-analysis of 18 nordic convenience samples. Ann Gen Psychiatry. 2012;11:26. doi: 10.1186/1744-859X-11-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felmingham KL, Bryant RA. Gender differences in the maintenance of response to cognitive behavior therapy for posttraumatic stress disorder. J Consult Clin Psychol. 2012;80:196–200. doi: 10.1037/a0027156. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, Ruan WJ, Compton WM. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harford TC, Chen CM, Saha TD, Smith SM, Hasin DS, Grant BF. An item response theory analysis of DSM-IV diagnostic criteria for personality disorders: findings from the national epidemiologic survey on alcohol and related conditions. Personal Disord. 2013;4:43–54. doi: 10.1037/a0027416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Q, Glas CAW, Veldkamp BP. Assessing impact of differential symptom functioning on post-traumatic stress disorder (PTSD) diagnosis. Int J Methods Psychiatr Res. 2014 doi: 10.1002/mpr.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoertel N, Franco S, Wall MM, Oquendo MA, Kerridge BT, Limosin F, Blanco C. Mental disorders and risk of suicide attempt: a national prospective study. Mol Psychiatry. 2015;20:718–726. doi: 10.1038/mp.2015.19. [DOI] [PubMed] [Google Scholar]
- Hoertel N, López S, Peyre H, Wall MM, González-Pinto A, Limosin F, Blanco C. Are symptom features of depression during pregnancy, the postpartum period and outside the peripartum period distinct? Results from a nationally representative sample using item response theory (IRT) Depress Anxiety. 2015;32:129–140. doi: 10.1002/da.22334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoertel N, Peyre H, Wall MM, Limosin F, Blanco C. Examining sex differences in DSM-IV borderline personality disorder symptom expression using Item Response Theory (IRT) J Psychiatr Res. 2014;59:213–219. doi: 10.1016/j.jpsychires.2014.08.019. [DOI] [PubMed] [Google Scholar]
- Hourani L, Williams J, Bray R, Kandel D. Gender differences in the expression of PTSD symptoms among active duty military personnel. J Anxiety Disord. 2015;29:101–108. doi: 10.1016/j.janxdis.2014.11.007. [DOI] [PubMed] [Google Scholar]
- Kawakami N, Tsuchiya M, Umeda M, Koenen KC, Kessler RC World Mental Health Survey Japan. Trauma and posttraumatic stress disorder in Japan: Results from the World Mental Health Japan Survey. J Psychiatr Res. 2014;53:157–165. doi: 10.1016/j.jpsychires.2014.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS-R): background and aims. Int J Methods Psychiatr Res. 2004;13:60–68. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26:537–547. doi: 10.1002/jts.21848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord FM, Novick MR. Statistical theories of mental test scores. Addison-Wesley Pub. Co; 1968. [Google Scholar]
- McBride O, Strong DR, Kahler CW. Exploring the role of a nicotine quantity-frequency use criterion in the classification of nicotine dependence and the stability of a nicotine dependence continuum over time. Nicotine Tob Res Off J Soc Res Nicotine Tob. 2010;12:207–216. doi: 10.1093/ntr/ntp196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. 2011;45:1027–1035. doi: 10.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millsap RE, Yun-Tein J. Assessing Factorial Invariance in Ordered-Categorical Measures. Multivar Behav Res. 2004;39:479–515. doi: 10.1207/S15327906MBR3903_4. [DOI] [Google Scholar]
- Muthén L, Muthén B. User’s guide. Los Angeles: 2007. Mplus: Statistical analyses with latent variables. [Google Scholar]
- Palm KM, Strong DR, MacPherson L. Evaluating symptom expression as a function of a posttraumatic stress disorder severity. J Anxiety Disord. 2009;23:27–37. doi: 10.1016/j.janxdis.2008.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkonigg A, Kessler RC, Storz S, Wittchen HU. Traumatic events and post-traumatic stress disorder in the community: prevalence, risk factors and comorbidity. Acta Psychiatr Scand. 2000;101:46–59. doi: 10.1034/j.1600-0447.2000.101001046.x. [DOI] [PubMed] [Google Scholar]
- Peters L, Issakidis C, Slade T, Andrews G. Gender differences in the prevalence of DSM-IV and ICD-10 PTSD. Psychol Med. 2006;36:81–89. doi: 10.1017/S003329170500591X. [DOI] [PubMed] [Google Scholar]
- Peyre H, Hoertel N, Cortese S, Acquaviva E, De Maricourt P, Limosin F, Delorme R. Attention-deficit/hyperactivity disorder symptom expression: a comparison of individual age at onset using item response theory. J Clin Psychiatry. 2014;75:386–392. doi: 10.4088/JCP.13m08638. [DOI] [PubMed] [Google Scholar]
- Peyre H, Speranza M, Cortese S, Wohl M, Purper-Ouakil D. Do ADHD Children With and Without Child Behavior Checklist-Dysregulation Profile Have Different Clinical Characteristics, Cognitive Features, and Treatment Outcomes? J Atten Disord. 2012 doi: 10.1177/1087054712452135. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Anxiety Disord. 2011;25:456–465. doi: 10.1016/j.janxdis.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratcliffe M, Ruddell M, Smith B. What is a “sense of foreshortened future?” A phenomenological study of trauma, trust, and time. Front Psychol. 2014;5:1026. doi: 10.3389/fpsyg.2014.01026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychol Med. 2011;41:71–83. doi: 10.1017/S0033291710000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott NW, Fayers PM, Aaronson NK, Bottomley A, de Graeff A, Groenvold M, Gundy C, Koller M, Petersen MA, Sprangers MA. Differential item functioning (DIF) analyses of health-related quality of life instruments using logistic regression. Health Qual Life Outcomes. 2010;8:81. doi: 10.1186/1477-7525-8-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L, Thissen D. Using effect sizes for research reporting: examples using item response theory to analyze differential item functioning. Psychol Methods. 2006;11:402–415. doi: 10.1037/1082-989X.11.4.402. [DOI] [PubMed] [Google Scholar]
- Stein MB, Walker JR, Forde DR. Gender differences in susceptibility to posttraumatic stress disorder. Behav Res Ther. 2000;38:619–628. doi: 10.1016/s0005-7967(99)00098-4. [DOI] [PubMed] [Google Scholar]
- Stenmark H, Guzey IC, Elbert T, Holen A. Gender and offender status predicting treatment success in refugees and asylum seekers with PTSD. Eur J Psychotraumatology. 2014;5 doi: 10.3402/ejpt.v5.20803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong DR, Kahler CW, Colby SM, Griesler PC, Kandel D. Linking Measures of Adolescent Nicotine Dependence to a Common Latent Continuum. Drug Alcohol Depend. 2009;99:296–308. doi: 10.1016/j.drugalcdep.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull. 2006;132:959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- Weinstock LM, Strong D, Uebelacker LA, Miller IW. DSM-IV depressive symptom expression among individuals with a history of hypomania: A comparison to those with or without a history of mania. J Psychiatr Res. 2010;44:979–985. doi: 10.1016/j.jpsychires.2010.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstock LM, Strong D, Uebelacker LA, Miller IW. Differential item functioning of DSM-IV depressive symptoms in individuals with a history of mania versus those without: an item response theory analysis. Bipolar Disord. 2009;11:289–297. doi: 10.1111/j.1399-5618.2009.00681.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Neria Y, Das A, Feder A, Blanco C, Lantigua R, Shea S, Gross R, Gameroff MJ, Pilowsky D, Olfson M. Gender differences in posttraumatic stress disorder among primary care patients after the World Trade Center attack of September 11, 2001. Gend Med. 2005;2:76–87. doi: 10.1016/s1550-8579(05)80014-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson L. Statistical methods in psychology journals: Guidelines and explanations. Am Psychol. 1999;54:594–604. doi: 10.1037/0003-066X.54.8.594. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.