Abstract
Background
Neisseria gonorrhoeae (N. gonorrhoeae) is one of the most prevalent non-ulcerative sexually transmitted infections (STIs) in China, however, the data about N. gonorrhoeae infections are limited in this population. The objective of this study is to determine N. gonorrheae incidence and associated risk factors among female sex workers (FSWs) in China.
Methods
This serial cross-sectional study was conducted semi-annually among FSWs in a City of Yunnan Province, which constituted an open cohort study. Participants were interviewed and tested for N. gonorrhoeae every 6 months.
Results
During 3 years of follow-up, 64 incident cases of N. gonorrhoeae infection were diagnosed, yielding an overall incidence of 5.9 per 100 person years (PY) (95% confidence interval (CI), 4.53–7.41). Working in higher risk commercial sex venue (adjusted hazard ratio (AHR)=2.7, 95% CI, 1.56–4.55), inconsistently use condom with clients in previous week (AHR=1.9, 95% CI, 1.07–3.35) and being infected with C. trachomatis (AHR=1.9, 95% CI, 1.06–3.26) were independent risk factors for incident N. gonorrhoeae infection.
Conclusions
A relatively high prevalence and incidence of N. gonorrhoeae among a prospective cohort of FSWs underscore the urgency for traditional HIV/STIs prevention methods among FSWs, such as condom promotion, screening and treatment of STIs, considering the high prevalence of STIs. Significant attention should focus on FSWs working in higher risk commercial sex venues as they are at higher risk for N. gonorrhoeae and transmission than those in lower risk commercial sex venues.
Keywords: N. gonorrhoeae, sexually transmitted infections, female sex workers, China
Background
Sexual transmission has become the primary mode of human immunodeficiency virus (HIV) transmission in China, and heterosexual transmission through commercial sex is recognized as one of the main modes1. Female sex workers (FSWs), who are not only at high risk for HIV infection, but also a “core population” who may be responsible for a large proportion of HIV transmission in China. It has been well studied that sexually transmitted infections (STIs) may facilitate the spread of HIV2, 3.
Neisseria gonorrhoeae (N. gonorrhoeae) which is one of the most prevalent non-ulcerative STIs in China, act as facilitating factors in transmission of HIV4–6, and if left untreated, can cause long-term debilitating effects, such as chronic pelvic pain, pelvic inflammatory disease, ectopic pregnancy, and tubal infertility4, 7. Surveillance of syphilis infection among FSWs has been integrated into the national HIV surveillance system in China, but N. gonorrhoeae surveillance activities were mainly based on passive case reporting8. There have been many studies on HIV and syphilis9, 10, but the data about N. gonorrhoeae infections are limited in this population in China8, 11–13. These cross-sectional studies conducted between 2005 and 2013 revealed the range of N. gonorrhoeae prevalence among FSWs being 1.8–37.8% in different regions across the country (median = 7.8%)8, 11–14.
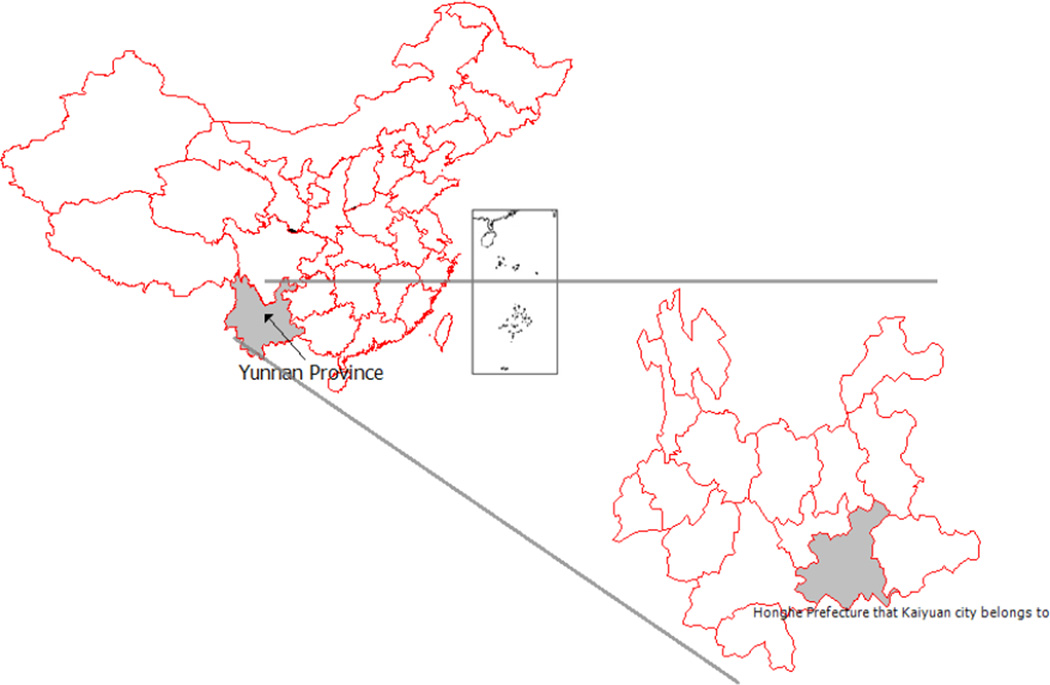
HIV/STIs prevalence are highest among FSWs in Yunnan Province in southern China, near the borders with Vietnam, Thailand, and Myanmar15, as many of the FSWs are illegal drug users and may serve commercial sex as a means to financially support their drug habits5. Most of the studies related with FSWs are cross-sectional design in Yunnan Province5, 11, 16–20, therefore there are limited data about N. gonorrhoeae incidence and associated risk factors. The aim of this study was to determine the incidence and risk factors for incident N. gonorrhoeae infection among FSWs in Yunnan Province, China. This study was conducted in moderately-sized city of Yunnan Province, with a population of 292,000 and large numbers of sex workers (Figure 1).
Figure 1.
Location of study site in Yunnan Province, China.
Methods
Survey methods
From March 2009 to May 2012, cross-sectional studies were carried out every 6 months and totally 7 surveys were conducted by the Chinese Center for Disease Control and Prevention (China CDC) in Beijing with provincial and local staff in Yunnan. Subjects who completed two or more surveys constituted an open cohort. Local CDC outreach workers explained study purpose, procedures, and the risks and benefits of participation to all commercial sex venues and bosses and invited women working as sex workers to participate in. The inclusion criteria were women aged ≥16 years, self-reported to have sold sex for money within the previous 3 months, willing to provide written informed consent and who agreed to testing and counseling for HIV/STIs. Study protocol received approval from the institutional review boards of the National CDC and the Yunnan Provincial CDC.
In order to maximize participant retention, the study schedule was thoroughly explained during informed consent procedure and was re-emphasized at subsequent follow up surveys. Detailed contact information of FSWs and their representatives was collected and was reviewed at each study visit. Additionally, FSWs were compensated 50 RMB (8 USD) upon each survey completion.
Data Collection
Specialists from China CDC and the Yunnan Provincial CDC trained local staff members from CDC on protection of human subjects, obtaining informed consent, safeguarding confidentiality, and HIV/STIs pre and post-test counseling.
After providing written informed consent, participants were asked a series of questions regarding their demographics, basic medical history, and sexual and drug use behavior. All subjects were contacted through provided contact information and reminded to return to future survey and testing periods. After survey completion, endocervical swabs were collected and tested for N. gonorrhoeae and Chlamydia trachomatis by polymerase chain reaction (PCR, AMPLICOR, Roche, USA); the sensitivity and specificity of PCR were 93% and 100% for Chlamydia trachomatis and 95% and 99% for N. gonorrhoeae respectively. Blood was collected and tested for HSV-2 antibody (HSV-2, HerpeSelect-2 ELISA IgG, Focus, USA), HIV-1 antibodies (enzyme-linked immunosorbent assay (ELISA), Vironostika HIV Uni-Form plus O, bioMerieux, Holland), and syphilis (rapid plasma reagin (RPR) test, Diagnosis kit, Xinjiang Xindi company, China). Positive HIV-1 ELISAs were confirmed by western blot (Diagnostics HIV Blot 2.2, Genelabs, USA) and positive RPR tests for syphilis were confirmed by the Treponema pallidum particle assay (TPPA) test (Serodia-P·PA- Fujirebio, Fuji, Japan). Vaginal swabs were collected and a wet mount was prepared to detect Trichomonas vaginalis (TV). Urine was tested for traces of illicit drugs. FSWs were classified as using illegal drugs if they self-reported drug use or tested positive through urine screening. To protect confidentiality, all subjects, subject surveys and collected specimens were assigned a corresponding participant identity number. Subjects were scheduled for follow-up visits 4–6 weeks after the initial visit to receive test results and post-test counseling. FSW participants with STIs were referred to Local Dermatology Hospital, where participants were entitled to receive a 60% discount on STI treatment. Those who tested HIV-positive were referred to Local People’s Hospital, where antiretroviral therapy was offered (when applicable) through the support of the Clinton Foundation. Special efforts were made to contact and notify all subjects who tested positive for HIV/STIs, but did not return at the 4–6 week follow-up.
Statistical Analysis
Statistical tests were performed using SAS™ 9.1 software (SAS Institute Inc, Cary, NC, USA). Chi-square tests were used to compare demographic and behavioral characteristics of participants who returned for follow-up and subjects who did not return. N. gonorrhoeae incidence density was calculated for subjects with N. gonorrhoeae negative result at baseline or during follow-up who completed at least one follow-up following negative result. N. gonorrhoeae incident infection was defined as the subsequent follow-up positive test following negative result (at baseline or during follow-up) and it was estimated to occur midway between the last N. gonorrhoeae negative test result and the first N. gonorrhoeae positive test result. N. gonorrhoeae incidence density was calculated by dividing the number of events (N. gonorrhoeae incident infection) by the number of person years of follow up. The follow-up time for each FSW was calculated from the date of negative result at baseline or during follow-up until the date for visit of N. gonorrhoeae infection in the study (incident or repeat infection), or date of last visit with a negative test result. Poisson 95% confidence intervals (CI) were calculated for overall incidence density.
Eligible for analyses on incidence of repeat N. gonorrhoeae infection were subjects who at baseline, or at subsequent visits, were diagnosed with a N. gonorrhoeae infection, had a negative test result after treatment. Time of repeat infection was estimated from date of negative testing in study until a repeat infection (subsequent follow-up positive test) or date of last visit in study with a negative test result.
Univariate Cox proportional hazards regression model with time dependent variables was used to measure the associations between independent variables and N. gonorrhoeae incident infection. Most factors could change during follow-up and were treated as time-dependent variables. Some characteristics, such as education level, nationality, and age at initiation of sex work, were treated as time-independent variables. Factors that were significantly associated in univariate analysis were included in a stepwise Cox proportional hazards multiple regression model with entry criteria of p<0.2 and exit criteria of p<0.05. All tests were 2-tailed and P<0.05 was considered the cut-off level for statistical significance for all analyses. Higher risk sex worker venues were defined as locations where FSWs generally charged less than 100 Yuan (about $16USD) for sex services, including beauty salons, temporary sublets, and street walkers; these FSWs attracted the less wealthy and less educated clients potentially at higher risk of HIV infection, such as drug users. Lower sex worker risk venues were defined as locations where FSWs generally charged 100 Yuan or more for sex, including karaoke clubs, night clubs, saunas and hotels21.
Results
Characteristics of Study Participants
By the end of the seventh survey in May 2012, there were 2053 FSWs with valid N. gonorrhoeae testing cumulatively recruited in the study cohort. A total of 1888 (92.0%) participants were N. gonorrhoeae negative prior to the baseline survey and of these 1888 participants, 792 (41.9%) FSWs returned for at least one follow-up visit.
Table 1 shows the demographic and behavioral characteristics of FSWs at baseline. Among the initially N. gonorrhoeae negative FSWs cohort who completed at least one follow-up visit, the majority were of Han ethnicity (70.1%), had registered residence in other cities in Yunnan (53.3%), with poor education level (34.8% had less than 6 years of education). Most participants worked out of low-risk commercial sex venues (61.1%) and reported that they had always used condoms with the previous week’s clients (84.7%).
Table 1.
Comparison of demographic and behavioral characteristics of FSWs in cohort and lost to follow-up
| Demographic and behavioral characteristics | Lost to follow up (N=1096) |
At least one follow up (N=792) |
P | |
|---|---|---|---|---|
| Age (years) | 16–20 | 387 (35.3) | 224 (28.3) | <.0001 |
| 21–25 | 306 (27.9) | 196 (24.7) | ||
| 26–52 | 403 (36.8) | 372 (47.0) | ||
| Ethnicity | Han | 752 (68.6) | 555 (70.1) | 0.4968 |
| Other | 344 (31.4) | 237 (29.9) | ||
| Place of registered permanent residence | Local city | 272 (24.8) | 214 (27.0) | 0.0424 |
| Other cities in Yunnan | 645 (58.9) | 422 (53.3) | ||
| Outside Yunnan | 179 (16.3) | 156 (19.7) | ||
| Education level | ≤6 years | 395 (36.0) | 276 (34.8) | 0.5934 |
| >6 years | 701 (64.0) | 516 (65.2) | ||
| Marital status | Married or cohabitation | 332 (30.3) | 244 (30.8) | 0.8101 |
| Single, separated, divorced, or widowed | 764 (69.7) | 548 (69.2) | ||
| Commercial sex venue | Lower risk | 636 (58.0) | 484 (61.1) | 0.1785 |
| Higher risk | 460 (42.0) | 308 (38.9) | ||
| Residence type | Apartment | 637 (58.1) | 551 (69.6) | <.0001 |
| Family home | 108 (9.9) | 101 (12.7) | ||
| Brothel or other working location | 351 (32.0) | 140 (17.7) | ||
| Drug use (ever) | Injection drug user | 97 (8.8) | 113 (14.3) | 0.0003 |
| Non-injection illegal drug user | 62 (5.7) | 56 (7.1) | ||
| Non-drug user | 937 (85.5) | 623 (78.6) | ||
| Drinks alcohol | No | 411 (37.5) | 254 (32.1) | 0.0148 |
| Yes | 685 (62.5) | 538 (67.9) | ||
| Duration of commercial sex work (years) | <2 | 721 (65.8) | 437 (55.2) | <.0001 |
| 2–5 | 226 (20.6) | 188 (23.7) | ||
| ≥5 | 149 (13.6) | 167 (21.1) | ||
| Age at sexual debut | <18 | 447 (40.8) | 309 (39.0) | 0.4387 |
| ≥18 | 649 (59.2) | 483 (61.0) | ||
| Age at initiation of commercial sex work | <20 | 392 (35.8) | 257 (32.4) | 0.1343 |
| ≥20 | 704 (64.2) | 535 (67.6) | ||
| Number of clients in previous week | <7 | 829 (75.6) | 647 (81.7) | 0.0017 |
| ≥7 | 267 (24.4) | 145 (18.3) | ||
| Always used condom with clients in previous week | Yes | 917 (83.7) | 671 (84.7) | 0.5363 |
| No | 179 (16.3) | 121 (15.3) | ||
| Has regular sexual partner | No | 547 (49.9) | 383 (48.4) | 0.5061 |
| Yes | 549 (50.1) | 409 (51.6) | ||
| Always used condom with regular partner in previous week | Yes | 91 (16.6) | 82 (20.1) | 0.1669 |
| No | 458 (83.4) | 327 (79.9) | ||
| Fee-per-service | ≥$16 | 679 (61.9) | 527 (66.5) | 0.0406 |
| <$16 | 417 (38.1) | 265 (33.5) | ||
| Vaginal douching | No | 233 (21.3) | 148 (18.7) | 0.1694 |
| Yes | 863 (78.7) | 644 (81.3) | ||
| HIV sero-positivity | No | 1001 (91.3) | 702 (88.6) | 0.0519 |
| Yes | 95 (8.7) | 90 (11.4) | ||
| HSV-2 sero-positivity | No | 434 (39.6) | 265 (33.5) | 0.0064 |
| Yes | 662 (60.4) | 527 (66.5) | ||
| C. trachomatis positive | No | 851 (77.6) | 643 (81.2) | 0.0617 |
| Yes | 245 (22.4) | 149 (18.8) | ||
| T. vaginalis positive | No | 1023 (93.3) | 720 (90.9) | 0.0503 |
| Yes | 73 (6.7) | 72 (9.1) | ||
| Syphilis positive | No | 1044 (95.3) | 731 (92.3) | 0.0075 |
| Yes | 52 (4.7) | 61 (7.7) | ||
Compared with FSWs lost to follow-up, the subjects who completed at least one follow-up survey were older, generally living in apartment, more likely to use illegal drug and drink alcohol, with longer duration of commercial sex work. This subset of participants also had fewer clients in the previous week, and charged a higher fee-per-service, but had a higher HSV-2 and syphilis prevalence.
N. gonorrhoeae prevalence, incidence and repeat infection
As shown in table 2, N. gonorrhoeae prevalence was average 8.0% among all the enrollees, and N. gonorrhoeae prevalence rate among FSWs in higher risk commercial sex venue was significant higher than in lower risk venue in the overall population. Of the 792 FSWs who were N. gonorrhoeae negative at enrollment and returned for at least one follow-up visit had been followed for a mean of 1.38 (±0.90) years. During the three years of the study, 64 incident cases of N. gonorrhoeae infection were diagnosed, yielding an overall incidence 5.9 per 100 person years (PY) (95% CI, 4.53–7.41).
Table 2.
N. gonorrhoeae prevalence among new enrollees in FSWs cohort by survey round and commercial sex venue
| Survey round |
New enrollees§ | Lower risk commercial sex venue |
Higher risk commercial sex venue |
P value |
|---|---|---|---|---|
| 1 | 8.3% (61/737) | 7.2% (33/458) | 10.0% (28/279) | 0.1761 |
| 2 | 7.0% (28/403) | 5.5% (13/238) | 9.1% (15/165) | 0.1589 |
| 3 | 7.9% (21/266) | 5.3% (8/152) | 11.4% (13/114) | 0.0661 |
| 4 | 8.1% (13/161) | 4.3% (4/93) | 13.2% (9/68) | 0.0399 |
| 5 | 11.0% (30/273) | 9.9% (15/152) | 12.4% (15/121) | 0.5070 |
| 6 | 5.6% (12/213) | 4.8% (5/105) | 6.5% (7/108) | 0.5863 |
| 7 | 9.1% (16/176) | 8.1% (9/111) | 10.8% (7/65) | 0.5534 |
| Total ∮ | 8.0% (165/2053) | 6.5% (78/1198) | 10.2% (87/855) | 0.0026 |
The enrollees in the 7th survey were excluded from all the data analysis as no subsequent follow up was carried out.
The subjects at baseline, who were enrolled the study for the first time.
A total of 51 FSWs who had a negative test after being diagnosed with N. gonorrhoeae and returned for at least one follow-up were eligible for repeat infection analyses, including 25 prevalent N. gonorrhoeae cases detected at baseline and 26 incident N. gonorrhoeae cases detected during follow-up. These subjects were followed for a mean of 1.17 (±0.74) years. During the three years of follow-up, 8 repeat N. gonorrhoeae infection were diagnosed, yielding a cumulative rate of repeat infection 13.3 per 100 PY (95% CI, 5.93–24.59). There were insufficient follow-up data to assess repeat infection past 3 years of observation and there were too few incident cases of repeat infection to display risk factor distributions.
Factors associated with N. gonorrhoeae infection
Table 3 presents the demographic and behavioral characteristics associated with N. gonorrhoeae incidence in univariate analysis. Participants with the number of clients in previous week≥7 (HR 1.7, 95% CI 1.01–3.02), inconsistently use condom with clients in previous week (HR 2.7, 95% CI 1.57–4.60), working in higher risk commercial sex venue (HR 3.1, 95% CI 1.88–5.17), being infected with C. trachomatis (HR 1.8, 95% CI 1.02–3.11) had an increased risk of incident N. gonorrhoeae infection, while those with higher education level (HR 0.5, 95% CI 0.33–0.90), drinking alcohol (HR 0.5, 95% CI 0.29–0.78) were less likely to be infected with N. gonorrhoeae.
Table 3.
Factors associated with N. gonorrhoeae incidence in univariate analysis (N=792)
| Demographic and behavioral characteristics | HR (95% CI) | |
|---|---|---|
| Age (years) | 16–20 | 1.0 |
| 21–25 | 0.5 (0.22–1.07) | |
| 26–52 | 1.0 (0.54–1.69) | |
| Ethnicity | Han | 1.0 |
| Other | 1.3 (0.76–2.18) | |
| Place of registered permanent Residence | Local city | 1.0 |
| Other cities in Yunnan | 1.2 (0.65–2.10) | |
| Outside Yunnan | 0.9 (0.44–2.03) | |
| Education level | ≤6 years | 1.0 |
| >6 years | 0.5 (0.33–0.90) | |
| Marital status | Married or cohabitation | 1.0 |
| Single, separated, divorced, or widowed | 1.0 (0.61–1.77) | |
| Commercial sex venue | Lower risk | 1.0 |
| Higher risk | 3.1 (1.88–5.17) | |
| Residence type | Apartment | 1.0 |
| Family home | 0.7 (0.30–1.64) | |
| Brothel or other working location | 1.5 (0.81–2.71) | |
| Drug use (ever) | Non-drug user | 1.0 |
| Non-injection illegal drug user | 1.0 (0.42–2.63) | |
| Injection drug user | 0.9 (0.44–1.82) | |
| Drinks alcohol | No | 1.0 |
| Yes | 0.5 (0.29–0.78) | |
| Duration of commercial sex work (years) | <2 | 1.0 |
| 2–5 | 1.1 (0.60–1.86) | |
| ≥5 | 0.7 (0.36–1.43) | |
| Age at sexual debut (years) | <18 | 1.0 |
| ≥18 | 0.6 (0.37–1.01) | |
| Age at initiation of commercial sex work (years) | ≥20 | 1.0 |
| <20 | 0.9 (0.54–1.55) | |
| Number of clients in previous week | <7 | 1.0 |
| ≥7 | 1.7 (1.01–3.02) | |
| Always used condom with clients in previous week | Yes | 1.0 |
| No | 2.7 (1.57–4.60) | |
| Had regular sexual partner | No | 1.0 |
| Yes | 0.8 (0.50–1.36) | |
| Always used condom with regular partner in previous week | Yes | 1.0 |
| No | 0.8 (0.35–1.77) | |
| Fee per service | ≥100 RMB | 1.0 |
| <100 RMB | 1.6 (0.95–2.56) | |
| Vaginal douching | No | 1.0 |
| Yes | 1.1 (0.55–2.14) | |
| HIV sero-positivity | No | 1.0 |
| Yes | 1.5 (0.79–2.90) | |
| HSV-2 sero-positivity | No | 1.0 |
| Yes | 1.8 (0.97–3.41) | |
| C. trachomatis positive | No | 1.0 |
| Yes | 1.8 (1.02–3.11) | |
| T. vaginalis positive | No | 1.0 |
| Yes | 1.0 (0.38–2.38) | |
| Syphilis positive | No | 1.0 |
| Yes | 1.0 (0.39–2.40) | |
Table 4 displays the results from multivariate Cox proportional hazards regression model of N. gonorrhoeae incident infection. Working in higher risk commercial sex venue (AHR=2.7, 95% CI 1.56–4.55), inconsistently use condom with clients in previous week (AHR=1.9, 95% CI 1.07–3.35) and being infected with C. trachomatis (AHR=1.9, 95% CI 1.06–3.26) were independent risk factors for N. gonorrhoeae infection.
Table 4.
Factors associated with N. gonorrhoeae infection in multivariate analysis (N=792)
| Risk factors | Adjusted HR (95% CI) | P |
|---|---|---|
| Higher risk commercial sex venue | 2.7 (1.56–4.55) | 0.0003 |
| Inconsistent condom use with clients in previous week | 1.9 (1.07–3.35) | 0.0283 |
| C. trachomatis positive | 1.9 (1.06–3.26) | 0.0295 |
Discussion
To our knowledge, this is the first paper to report the incidence of N. gonorrhoeae infection among FSWs in China. This study found a relatively high incidence (5.9 per 100 PY, 95% CI: 4.53–7.41) and prevalence (average 8.0% among the whole study population) of N. gonorrhoeae among FSWs in a City of Yunnan Province. N. gonorrhoeae prevalence measured in this study was similar to that in Guangxi and Guangzhou Province14, 22, but higher than the results in the eastern and southern parts of China8, 13. However, a lower N. gonorrhoeae prevalence was reported among FSWs in other countries, from 0.31% in Melbourne23, 1·6% in Peru24, 1.9% in west Africa25, 4.4% in Hong Kong26, to 5.1% in Côte d’Ivoire27. The differences in the observed burden might have been resulted from sampling techniques, laboratory testing methods and different epidemic situations in the source population of FSWs. The high incidence and prevalence among FSWs identified in our study is an important public health concern as STIs including N. gonorrhoeae may facilitate HIV transmission4, 5. Understanding the prevalence and incidence of STIs, including N. gonorrhoeae, is key to characterizing the Chinese HIV epidemic and will aid in informing policy and prevention efforts20.
In this cohort of FSWs in Yunnan Province, we found that there was a significant higher risk of incident N. gonorrhoeae infection among women working in higher risk commercial sex venues. This is consistent with previously reported findings of risk factors for other STIs infection among FSWs in the studies of other countries28, 29. FSWs from higher risk commercial sex venues generally work in smaller and hidden venues such as, guesthouses, beauty salons, temporary sublets, on the street, and self-rented rooms etc8, 30. Those women are a special segment of FSWs population with more vulnerable nature in terms of socio-demographic characteristics (including older age, less education), employment and economic status, access to health care, risky behavior, and relationship with clients8. It was reported that FSWs working in higher risk commercial sex venues had more clients per week, had worked as an FSW for a longer time, and more reported not consistently using condoms with all clients in the previous week19, 20, 31. In addition, the clients who patronize FSWs in higher risk venues may also be at potentially higher risk of HIV infection, such as drug users. Intervention efforts should target FSWs working in higher risk commercial sex venues as they are more likely to be infected with HIV/STIs and may transmit these infections to their clients.
Inconsistently using condom with clients in previous week was a significant risk factor for incident N. gonorrhoeae infection after adjusting for significant covariates (AHR=1.9, 95% CI 1.07–3.35). Condoms have been consistently shown to protect against HIV/STIs infection21, 32, so FSWs should be encouraged to use condoms to protect both their sex partners (including clients and regular sex partners) and themselves. As FSWs in higher risk commercial sex venues may be under more pressure to not use condoms when requested by a client due to lack self-perceived risk and knowledge of HIV/STIs, consistent condom use should be promoted through interventions that take into account the specific context of risk behavior for those women30. Condoms available on-site, negotiations skills of condom use and funding free condoms to FSWs may help decrease risky behavior33.
Multivariate analysis revealed that C. trachomatis infection increased the risk of N. gonorrhoeae acquisition in this study population. Adjusting for the key covariates, FSWs with C. trachomatis infection were at a 2-fold, statistically significant, greater risk of incident N. gonorrhoeae infection than FSWs who were negative for C. trachomatis. There are several possible explanations for the relationship between the two infections. Firstly, FSWs infected with STIs, including C. trachomatis, have the same behavioural risk factors, for example, inconsistent or incorrect condom use and more clients. However, C. trachomatis infection was associated with N. gonorrhoeae after adjusting for other risk factors. Secondly, biological factors may help explain the association between C. trachomatis and N. gonorrhoeae infections. C. trachomatis can cause pelvic inflammatory disease, cervical inflammation and other chronic inflammation of the urogenital tract and chronic urogenital tract inflammation can contribute to the susceptibility of other microbial pathogens, including N. gonorrhoeae34, 35. The interaction of co-infections is of particular concern in the context of disease control because STIs are known to be important co-factors in the transmission of HIV.
Several limitations of this study should be considered in the interpretation of the results. Firstly, the subjects recruited from a city of Yunnan Province could not represent the population in China, more unlikely to reflect the accrual situation in China. Secondly, cohort study might be the best designing method for investigating HIV/STIs incidence. However, as we know, there is a high mobility among FSWs16, maintaining a cohort among these women is difficult and expensive. Moreover, validity problems arise when participants are lost to follow-up. Whereas, serial cross-sectional surveys, the inferences from which are highly useful and reliable, might be an ideal option. Thirdly, Nearly 60% of eligible FSWs were lost to follow-up, and there were significant differences between the subjects who were retained in the cohort and those who were lost to follow-up. Participants in the cohort had a higher prevalence (in comparison with those lost to follow-up) of some factors that might increase their N. gonorrhoeae risk, including illicit drug use, prevalent HSV-2, and prevalent syphilis, but also had a lower prevalence of other risk behaviors including having less clients in the previous week; thus, it is difficult to determine whether N. gonorrhoeae incidence was overestimated or underestimated. Fourthly, antimicrobial susceptibility of N. gonorrhoeae was not tested in the current study, FSWs with a positive nucleic acid amplification tests should be further encouraged to provide a urethral swab for culture susceptibility testing in the future. Finally, most of our data were self-reported, which raises concern about social desirability bias, particularly those related to sexual behaviours.
Conclusions
This study identified a relatively high prevalence and incidence of N. gonorrhoeae among a prospective cohort of FSWs. The results of this study have significant implications for future research and health interventions. Traditional HIV/STIs prevention methods among FSWs such as condom promotion should be emphasized, considering the high prevalence of STIs. Screening and treatment of STIs are also an important strategy as the presence of STIs may facilitate HIV acquisition. Significant attention should focus on FSWs working in higher risk commercial sex venues as they are at higher risk for N. gonorrhoeae and transmission.
Highlights.
An open cohort study was conducted.
The incidence was 5.9 per 100 person-years;
Higher risk venue, inconsistently use condom and C. trachomatis were risk factors.
Acknowledgements
This study was funded by a grant from the National Institute of Allergy and Infectious Diseases, U.S. National Institutes of Health (U19 AI51915–05).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement
All the authors declare no conflict of interest.
References
- 1.Wang N, Wang L, Wu Z, Guo W, Sun X, Poundstone K, Wang Y National Expert Group on HIVAE. Estimating the number of people living with HIV/AIDS in China: 2003–09. International journal of epidemiology. 2010;39(Suppl 2):21–28. doi: 10.1093/ije/dyq209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kenyon CR, Osbak K, Buyze J. The Prevalence of HIV by Ethnic Group Is Correlated with HSV-2 and Syphilis Prevalence in Kenya, South Africa, the United Kingdom, and the United States. Interdisciplinary perspectives on infectious diseases. 2014;2014:284317. doi: 10.1155/2014/284317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kenyon C, Buyze J, Colebunders R. Classification of incidence and prevalence of certain sexually transmitted infections by world regions. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases. 2014;18:73–80. doi: 10.1016/j.ijid.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 4.Folch C, Esteve A, Sanclemente C, Martro E, Lugo R, Molinos S, Gonzalez V, Ausina V, Casabona J. Prevalence of human immunodeficiency virus, Chlamydia trachomatis, and Neisseria gonorrhoeae and risk factors for sexually transmitted infections among immigrant female sex workers in Catalonia, Spain. Sexually transmitted diseases. 2008;35:178–183. doi: 10.1097/OLQ.0b013e31815a848d. [DOI] [PubMed] [Google Scholar]
- 5.Chen XS, Yin YP, Liang GJ, Gong XD, Li HS, Poumerol G, Thuy N, Shi MQ, Yu YH. Sexually transmitted infections among female sex workers in Yunnan, China. AIDS patient care and STDs. 2005;19:853–60. doi: 10.1089/apc.2005.19.853. [DOI] [PubMed] [Google Scholar]
- 6.Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sexually transmitted infections. 1999;75:3–17. doi: 10.1136/sti.75.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vall-Mayans M, Villa M, Saravanya M, Loureiro E, Merono M, Arellano E, Sanz B, Saladie P, Andreu A, Codina MG. Sexually transmitted Chlamydia trachomatis, Neisseria gonorrhoeae, and HIV-1 infections in two at-risk populations in Barcelona: female street prostitutes and STI clinic attendees. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases. 2007;11:115–122. doi: 10.1016/j.ijid.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Chen XS, Yin YP, Liang GJ, Wang QQ, Jiang N, Liu Q, Fu GF, Yang B, Zhou YJ, Shi MQ, Wang B. The prevalences of Neisseria gonorrhoeae and Chlamydia trachomatis infections among female sex workers in China. BMC public health. 2013;13:121. doi: 10.1186/1471-2458-13-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang C, Latkin C, Luan R, Wang C, Nelson K. HIV, syphilis, hepatitis C and risk behaviours among commercial sex male clients in Sichuan province, China. Sexually transmitted infections. 2010;86:559–564. doi: 10.1136/sti.2009.041731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liao M, Nie X, Pan R, Wang C, Ruan S, Zhang C, Kang D, Fu J, Qian Y, Tao X, Zhao J. Consistently low prevalence of syphilis among female sex workers in Jinan, China: findings from two consecutive respondent driven sampling surveys. PloS one. 2012;7:34085. doi: 10.1371/journal.pone.0034085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jin X, Chan S, Ding G, Wang H, Xu J, Wang G, Chang D, Reilly KH, Wang N. Prevalence and risk behaviours for Chlamydia trachomatis and Neisseria gonorrhoeae infection among female sex workers in an HIV/AIDS high-risk area. International journal of STD & AIDS. 2011;22:80–84. doi: 10.1258/ijsa.2010.010289. [DOI] [PubMed] [Google Scholar]
- 12.Zhu BY, Bu J, Huang PY, Zhou ZG, Yin YP, Chen XS, Wei WH, Zhong MY, Wang HC, Wang H, Gan Q. Epidemiology of sexually transmitted infections, HIV, and related high-risk behaviors among female sex workers in Guangxi Autonomous Region, China. Japanese journal of infectious diseases. 2012;65:75–78. [PubMed] [Google Scholar]
- 13.Tang W, Pan J, Jiang N, Hu HY, Mahapatra T, Yin YP, Mahapatra S, Wang XL, Chen XS, Lin N, Zhang X, Huan XP, Yang HT, Fu GF. Correlates of chlamydia and gonorrhea infection among female sex workers: the untold story of Jiangsu, China. PloS one. 2014;9:85985. doi: 10.1371/journal.pone.0085985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yin YP, Li HM, Xiang Z, Liang GJ, Shi MQ, Zhou YJ, Han Y, Wang GQ, Wang B, Chen XS. Association of sexually transmitted infections with high-risk human papillomavirus types: a survey with 802 female sex workers in china. Sexually transmitted diseases. 2013;40:493–495. doi: 10.1097/OLQ.0b013e31828b32b8. [DOI] [PubMed] [Google Scholar]
- 15.Xiao Y, Kristensen S, Sun J, Lu L, Vermund SH. Expansion of HIV/AIDS in China: lessons from Yunnan Province. Social science & medicine. 2007;64:665–75. doi: 10.1016/j.socscimed.2006.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang H, Chen RY, Sharp GB, Brown K, Smith K, Ding G, Jin X, Xu J, Dong R, Wang N. Mobility, risk behavior and HIV/STI rates among female sex workers in Kaiyuan City, Yunnan Province, China. BMC infectious diseases. 2010;10:198. doi: 10.1186/1471-2334-10-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang HB, Smith K, Brown KS, Wang GX, Chang DF, Xu JJ, Ding GW, Jin X, Reilly KH, Wang N. Prevalence, incidence, and persistence of syphilis infection in female sex workers in a Chinese province. Epidemiology and infection. 2011;139:1401–1409. doi: 10.1017/S0950268810002578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang JJ, Zhu ZB, Yang X, Wu J, Wang HB, Feng L, Ding GW, Norris JL, Wang N. Herpes simplex virus type 2 risks in female sex workers in the China-Vietnam border county of Hekou. Biomedical and environmental sciences : BES. 2012;25:706–710. doi: 10.3967/0895-3988.2012.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang H, Reilly KH, Brown K, Jin X, Xu J, Ding G, Zang C, Wang J, Wang N. HIV incidence and associated risk factors among female sex workers in a high HIV-prevalence area of China. Sexually transmitted diseases. 2012;39:835–841. doi: 10.1097/OLQ.0b013e318266b241. [DOI] [PubMed] [Google Scholar]
- 20.Wang H, Reilly KH, Smith MK, Brown K, Jin X, Xu J, Ding G, Zang C, Wang J, Wang N. Herpes simplex virus type 2 incidence and associated risk factors among female sex workers in a high HIV-prevalence area of China. International journal of STD & AIDS. 2013;24:441–446. doi: 10.1177/0956462412472800. [DOI] [PubMed] [Google Scholar]
- 21.Wang H, Chen RY, Ding G, Ma Y, Ma J, Jiao JH, Wu Z, Sharp GB, Wang N. Prevalence and predictors of HIV infection among female sex workers in Kaiyuan City, Yunnan Province, China. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases. 2009;13:162–169. doi: 10.1016/j.ijid.2008.05.1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van den Hoek A, Yuliang F, Dukers NH, Zhiheng C, Jiangting F, Lina Z, Xiuxing Z. High prevalence of syphilis and other sexually transmitted diseases among sex workers in China: potential for fast spread of HIV. Aids. 2001;15:753–759. doi: 10.1097/00002030-200104130-00011. [DOI] [PubMed] [Google Scholar]
- 23.Tang H, Hocking JS, Fehler G, Williams H, Chen MY, Fairley CK. The prevalence of sexually transmissible infections among female sex workers from countries with low and high prevalences in Melbourne. Sexual health. 2013;10:142–145. doi: 10.1071/SH12114. [DOI] [PubMed] [Google Scholar]
- 24.Carcamo CP, Campos PE, Garcia PJ, Hughes JP, Garnett GP, Holmes KK, Peru Pst Prevalences of sexually transmitted infections in young adults and female sex workers in Peru: a national population-based survey. The Lancet Infectious diseases. 2012;12:765–773. doi: 10.1016/S1473-3099(12)70144-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pepin J, Deslandes S, Khonde N, Kintin DF, Diakite S, Sylla M, Meda H, Sobela F, Asamoah-Adu C, Agyarko-Poku T, Frost E. Low prevalence of cervical infections in women with vaginal discharge in west Africa: implications for syndromic management. Sexually transmitted infections. 2004;80:230–235. doi: 10.1136/sti.2003.007534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wong HT, Lee KC, Chan DP. Community-based sexually transmitted infection screening and increased detection of pharyngeal and urogenital Chlamydia trachomatis and Neisseria gonorrhoeae infections in female sex workers in Hong Kong. Sexually transmitted diseases. 2015;42:185–191. doi: 10.1097/OLQ.0000000000000257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vuylsteke B, Semde G, Sika L, Crucitti T, Ettiegne Traore V, Buve A, Laga M. HIV and STI prevalence among female sex workers in Cote d’Ivoire: why targeted prevention programs should be continued and strengthened. PloS one. 2012;7:32627. doi: 10.1371/journal.pone.0032627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ford K, Wirawan DN, Reed BD, Muliawan P, Sutarga M. AIDS and STD knowledge, condom use and HIV/STD infection among female sex workers in Bali, Indonesia. AIDS care. 2000;12:523–534. doi: 10.1080/095401200750003716. [DOI] [PubMed] [Google Scholar]
- 29.Riono P, Jazant S. The current situation of the HIV/AIDS epidemic in Indonesia. AIDS education and prevention : official publication of the International Society for AIDS Education. 2004;16:78–90. doi: 10.1521/aeap.16.3.5.78.35531. [DOI] [PubMed] [Google Scholar]
- 30.Zhou C, Rou K, Dong WM, Wang Y, Dong W, Zhou Y, Chen X, Jia M, Liu W, Zheng J, Ma Y, Li Y, Wu Z, China National HIVPSG High prevalence of HIV and syphilis and associated factors among low-fee female sex workers in mainland China: a cross-sectional study. BMC infectious diseases. 2014;14:225. doi: 10.1186/1471-2334-14-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhou Y, Li X, Zhang C, Tan G, Stanton B, Zhang X, Cui Y. Rates of HIV, syphilis, and HCV infections among different demographic groups of female sex workers in Guangxi China: evidence from 2010 national sentinel surveillance data. AIDS care. 2013;25:1433–1441. doi: 10.1080/09540121.2013.772282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cayley WE., Jr Effectiveness of condoms in reducing heterosexual transmission of HIV. American family physician. 2004;70:1268–1269. [PubMed] [Google Scholar]
- 33.Ye X, Shang M, Shen T, Pei B, Jiang X, Cai Y. Social, psychological, and environmental-structural factors determine consistent condom use among rural-to-urban migrant female sex workers in Shanghai China. BMC public health. 2012;12:599. doi: 10.1186/1471-2458-12-599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Simms I, Stephenson JM, Mallinson H, Peeling RW, Thomas K, Gokhale R, Rogers PA, Hay P, Oakeshott P, Hopwood J, Birley H, Hernon M. Risk factors associated with pelvic inflammatory disease. Sexually transmitted infections. 2006;82:452–457. doi: 10.1136/sti.2005.019539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaur R, Mittal N, Bhalla P, Reddy BN, Baveja UK. Risk factors of herpes simplex virus type 2 among STD clinic attenders in Delhi, India. The Journal of communicable diseases. 2006;38:339–343. [PubMed] [Google Scholar]