BACKGROUND
In the United States, approximately 14% of children are diagnosed with asthma.1 The burden of asthma varies nationwide, and some communities have a higher prevalence of the chronic lung disease. For example, among the approximately 2,000 students in Kennett Public Schools (KPS) in southeast Missouri, about 18% have asthma. In 2008, KPS started addressing students’ health needs through a five-year Missouri Foundation for Health grant to implement an asthma management program. District staff developed the program in collaboration with the Missouri Department of Health and Senior Services, University of Missouri School of Medicine, and the Missouri Foundation for Health. In addition, the Centers for Disease Control and Prevention (CDC)-funded Missouri Asthma Prevention and Control Program contributed expertise in school-based asthma-related programming.
Between 2011–2012, a team from CDC and ICF International evaluated the KPS asthma program to examine program activities and their impact on students’ asthma outcomes. CDC evaluated this program because it used school-based activities to connect students to and potentially enhance outcomes of clinical asthma care, recognized as necessary for achieving and maintaining asthma control.2, 3 Findings revealed the program led to improvements in asthma control among students with poorly-controlled asthma.4 Given that the KPS program has evidence of effectiveness and provides a model for the role of school staff in enhancing clinical care, the purpose of this paper is to provide a more detailed program description of the multicomponent approaches used in order to offer school health services staff in other districts ideas for replication and incorporation into their asthma management programs. This paper will help to translate evaluation findings into clear programmatic activities for districts that wish to make use of these asthma program components.
PROGRAM OVERVIEW
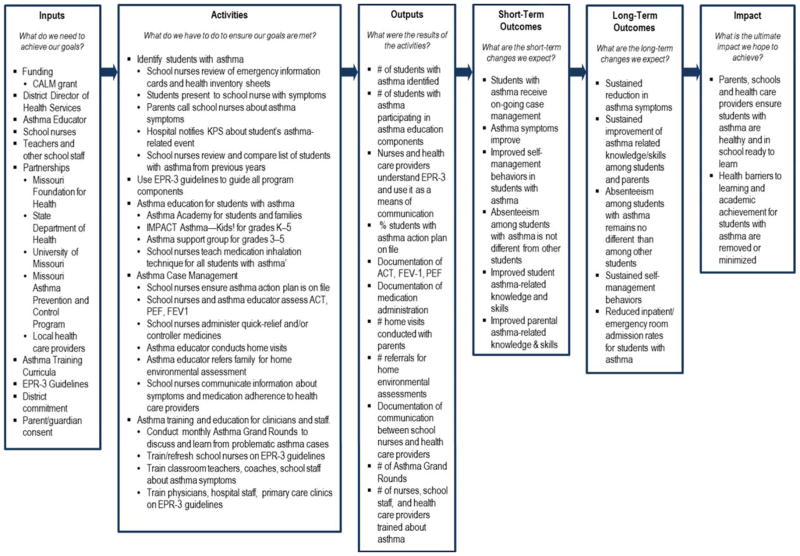
The KPS asthma program is a model for school districts interested in helping students with asthma. This paper provides a program overview and emphasizes activities that facilitate strong connections to clinical care (see Figure 1 for the program logic model). We start by describing foundational program characteristics: types of program activities; use of the National Asthma Education and Prevention Program’s (NAEPP) Expert Panel Report 3 (EPR-3) guidelines; and staffing structure.
Figure 1. Logic Model of the Kennett Public Schools Asthma Management Program.
Abbreviations: CALM, Childhood Asthma Linkages in Missouri. EPR-3, Expert Panel Report 3. ACT, Asthma Control Test. PEF, peak expiratory flow. FEV1, forced expiratory volume in 1 second.
The program consisted of several key activities—identification of students with asthma; case management and care coordination; asthma-related training for school staff and community health care providers; and education for students and their families. Some activities were provided to all students; others were reserved for students experiencing the greatest asthma control difficulty. Furthermore, several activities reflect approaches that have, to date, appeared less frequently in the literature on school-based asthma management but help fill gaps researchers have identified in many school-based programs, particularly related to helping students secure appropriate medical care.3 Additional activities, consistent with those routinely seen in the literature for school-based asthma management programs,5–7 rounded out program offerings.
Activities were based on NAEPP’s EPR-3 guidelines8 outlining scientific recommendations for management and treatment of asthma. EPR-3 guidelines provided parameters for assessing asthma control, educating students, administering medications, and training staff and community providers. Use of the guidelines also facilitated effective communication among program staff, parents, and providers by giving staff specific and clinically relevant language and messages, allowing more targeted conversations about students’ asthma.
Primary staff involved in implementation were the health services director, school nurses, and an asthma educator. The director provided oversight across schools and coordinated activities. School nurses, one in each of four K-12 schools, conducted routine, ongoing activities (e.g., identifying students with asthma, administering medications, assessing asthma control). The asthma educator, a grant-funded position, provided more intensive case management services and supported educational activities. Since the evaluation, KPS has eliminated the asthma educator position and shifted associated responsibilities to school nurses; this coincided with the end of the 5-year grant.
Identification of Students with Asthma
Identifying students with asthma is the foundation for providing asthma management services. In KPS, the process for identifying students with asthma is consistent with recommendations in the literature: reviewing student emergency information cards and health inventories completed by parents and noting students who presented to nurses with asthma-like symptoms or whose parents talk to nurses about asthma.9 Additionally, after securing parent/guardian consent, KPS received notification from local hospital staff when students visited the emergency room or were hospitalized due to asthma.
Case Management and Care Coordination
Several program activities were offered as case management and care coordination for students with asthma. A few activities were similar to those implemented in other school-based asthma programs (e.g., keeping asthma action plans for students with asthma, administering quick-relief medications). In addition, program staff maintained asthma action plans and written permissions from physicians and parents/guardians for students to carry and self-administer their inhalers at school. Several activities, however, reflected approaches less common in the literature and facilitated staff’s ability to enhance clinical care for students—particularly those with poorly-controlled asthma.
Clinical assessment of asthma control
One key program activity was routine clinical assessment of asthma control (typically performed at least annually). Program staff received in-depth, EPR-3 guidelines-based training on assessment procedures (see description of the training component of this program) and then individually met all students with asthma to assess lung function through forced expiratory volume in one second (FEV1) and peak expiratory flow (PEF) using hand-held spirometers and peak flow monitors; staff interpreted results using EPR-3 guidelines to classify students’ asthma severity and control. Staff also administered the Asthma Control Test (ACT), a validated asthma assessment questionnaire.10, 11 These school-conducted assessments were in addition to assessments students received from health care providers in clinical settings. Assessments allowed program staff to identify students with the greatest asthma difficulties so they could receive more individualized, intensive program activities. Assessments also provided valuable information for engaging students’ families and physicians.
Controller medication administration
Administration of asthma controller medications was another key activity. If students had asthma difficulties related to inconsistent controller medication use that could not be addressed through other means, staff oversaw medication administration at school for those students (approximately 8% of students with asthma). This allowed staff to ensure proper, consistent medication use while reinforcing the importance of controller medications.
Home visits
Staff also conducted home visits for a subset of students experiencing asthma management difficulties (approximately 42% of students with asthma). Program staff, often the asthma educator, used home visits to help families better manage students’ asthma. During typical home visits, staff reviewed students’ clinical assessments, asthma triggers, and medications. In addition, staff usually conducted brief observational assessments to identify possible environmental triggers (including secondhand tobacco smoke) and reviewed the U.S. Environmental Protection Agency’s Asthma Home Environment Checklist, including action steps for identifying and remediating asthma triggers commonly found in and around homes.12, 13
Home environmental assessments
Depending on environmental triggers identified during home visits, staff sometimes referred families for free environmental assessments conducted by experts from Southeast Missouri State University. These in-depth assessments, provided to fewer than 5% of KPS students with asthma, entailed searching homes for crevices where rodents/pests could enter, examining for mold and mildew, and assessing indoor air quality. After receiving recommendations from basic home visits and intensive home environmental assessments, KPS staff occasionally helped remediate triggers (e.g., provided air conditioning filters, allergy-free pillow cases, and mattress covers; secured pest control services).
Communication with health care providers
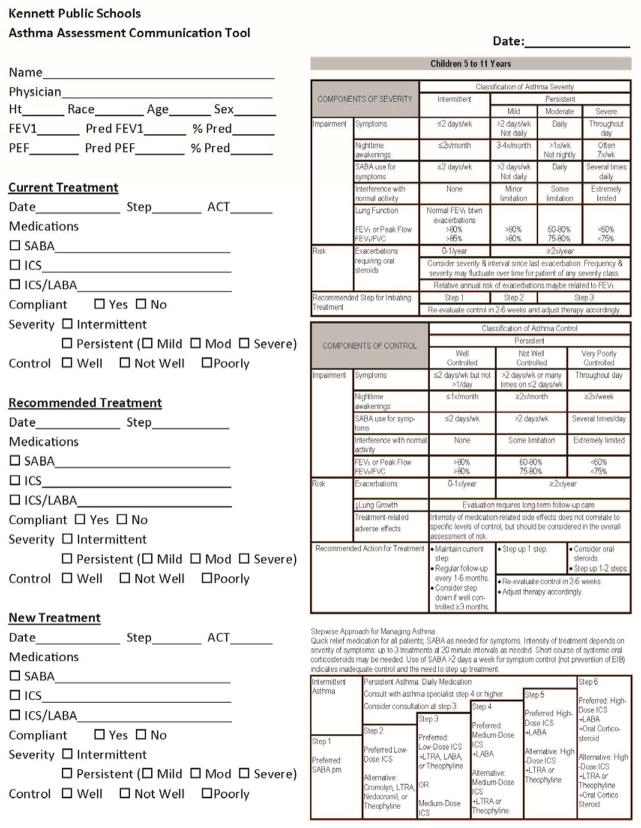
Another key case management activity was staff communication with community health care providers about students’ asthma; this has been highlighted in the literature as a valuable approach for school involvement in improving asthma among children.9 Asthma action plans on file for students with asthma already provided lines of communication from providers to school staff, but additional strategies opened lines of communication from school staff back to providers. When initiating communication with health care providers, school staff most often shared asthma assessment results (e.g., FEV1 and PEF measures) and medication information, but they also provided contextual information about students’ asthma-related experiences during school. Information could be easily shared with clinicians using the program’s Asthma Assessment Communication Tool (see Figure 2), which summarized EPR-3 guidelines and facilitated staff reports of assessment data, symptoms, and information about medication compliance. The tool was designed to help staff and health care providers easily identify asthma severity and distinguish between current, recommended, and new treatment plans based on EPR-3 principles of stepwise therapy in children. Health care providers could use the same form to document changes to students’ care (e.g., medication changes) and return it to the school. Program staff requested signed waivers from parents/guardians to allow sharing information with physicians in accordance with Health Insurance Portability and Accountability Act and Family Educational Rights and Privacy Act regulations.
Figure 2. Asthma Assessment Communication Tool.
Note: Tables in this tool were created based on tables in the EPR-3 Guidelines.8
Training for Health Care Providers and School Staff
KPS, in partnership with the director of Asthma Ready Communities14 at the University of Missouri School of Medicine, coordinated trainings for school nurses, health care providers, and their staff on both EPR-3 guidelines and educating families about asthma. In these trainings, staff and providers received updates on science-based asthma care, and KPS program staff received clinical training on asthma triggers, symptoms, EPR-3 guidelines, FEV1 measurement, teaching inhalation technique, and asthma medications. Program staff also met the district’s consulting physician monthly for “Asthma Grand Rounds” to discuss problematic asthma cases and lessons learned.
KPS also offered education sessions every other year for teachers and other school staff, and annually for sports coaches and physical education (PE) teachers. The Initiating Change: Creating an Asthma-Friendly School toolkit and companion video15 were used in broader staff training, and coaches and PE teachers received more detailed trainings to better recognize signs of asthma exacerbations. School staff learned how to help students having difficulty breathing, remind students to use medication before exercise, and communicate observations of possible asthma-related problems to program staff.
Asthma Education for Students
Program staff educated students with asthma and their families. KPS provided school-based group education and support programs for elementary students, off-site education events for students and their families, and one-on-one education on medication inhalation technique.
School-based group education and support programs
Group education and support programs focused on elementary school students with asthma and were offered annually. IMPACT Asthma—Kids! was a 30- to 60-minute, computer-based program that taught students in grades K–5 about topics such as quick-relief and controller medicines, triggers, and what to do during asthma exacerbations. In addition, KPS offered a support group for students in grades 3–5 to discuss asthma and encourage one another while learning management techniques.
Asthma Academy
KPS also offered an all-day workshop called the Asthma Academy, which was typically offered 1–4 weekend days a year in a local healthcare provider’s office. For this workshop, KPS brought in a well-known expert on guidelines-based treatment of asthma to work alongside community healthcare providers and school asthma program staff to educate a small group of students and their families about asthma. Activities included physical assessments, interpretation of assessment results, explanation of asthma triggers, and education about medications and proper medication inhalation technique. Through these activities, the Academy provided opportunities for students to receive expert care (e.g., allergy testing) that can be difficult to obtain in rural areas.
One-on-one education on medication inhalation technique
Another key asthma education approach was tailored one-on-one education on medication inhalation technique, provided as-needed. Program staff taught most students with asthma (83%) how to use spacers, and used handheld inspiratory flow measurement devices to show students correct inhalation needed for optimal medication deposition into the lungs.
IMPLICATIONS FOR SCHOOL HEALTH
Although the evaluation did not examine effectiveness of individual activities, findings suggested the program as a whole helped improve asthma control among students with poorly-controlled asthma.4 This program offers a replicable model with evidence of effectiveness for other school districts aiming to better support students with asthma, and may be particularly valuable for districts with low nurse-to-student ratios (to support the program’s workload).
Although several program activities are common among school-based programs, a number of KPS activities illustrate potential roles for school staff in enhancing clinical care, as has been called for—though less frequently reported—in the literature on school-based asthma management.3 By basing the program on EPR-3 guidelines, KPS established common language with which staff could communicate meaningfully and efficiently with students, families, and health care providers. Furthermore, by sharing asthma control assessment data with health care providers, staff provided a more complete set of information on which health care providers could base clinical decisions, thus potentially enhancing the care students received. Program staff further supported clinical care by educating students and families about medications, administering medications at school as necessary, and teaching students proper inhalation technique to maximize medication effectiveness. In addition, staff helped students and families understand the importance of asthma management and empowered them to achieve better asthma control. Program replication in other school districts may facilitate better coordination among school staff, families, and health care providers to improve asthma control among students.
Acknowledgments
The authors would like to thank Ngozi Kamalu and Doryn Chervin for their assistance in this project—particularly in evaluation design and data collection oversight. We also thank Blair Dean for her assistance in data collection coordination, and Eric Armbrecht, Ben Francisco, and Peggy Gaddy for their consultation and support throughout the evaluation. And last, but certainly not least, we thank the school district for its willingness to participate in this evaluation.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributor Information
Karen Cheung, Email: karen.cheung@icfi.com, Manager, ICF International, 710 Second Ave, Suite 550, Seattle, WA 98104, Phone: 206-801-2821, Fax: 206-801-2899.
Catherine N. Rasberry, Email: CRasberry@cdc.gov, Health Scientist, Centers for Disease Control and Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Division of Adolescent Health.
Richard L. Dunville, Email: RDunville@cdc.gov, Research Officer, Centers for Disease Control and Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Division of Adolescent Health.
Rebekah Buckley, Email: eut9@cdc.gov, Health Scientist, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health.
Deborah Cook, Email: dcook@kennett.k12.mo.us, Director of Health Services, Kennett Public Schools.
Brandy Daniels, Email: Brandy.Daniels@icfi.com, Senior Associate, ICF International.
Leah Robin, Email: LRobin@cdc.gov, Lead Health Scientist, Centers for Disease Control and Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Division of Adolescent Health.
References
- 1.Bloom B, Cohen RA, Freeman G. Vital Health Stat. Vol. 10. Hyattsville, MD: 2012. Summary health statistics for U.S. children: National Health Interview Survey, 2011; pp. 1–80. [PubMed] [Google Scholar]
- 2.Rossier Markus A, Lyon M, Rosenbaum S. Changing pO2licy: The elements for improving childhood asthma outcomes. The George Washington University School of Public Health and Health Services; 2010. [Accessed October 28, 2013]. Available at: http://www.mcanonline.org/files/ChangingpO2licyReport.pdf. [Google Scholar]
- 3.Wheeler LS, Merkle SL, Gerald LB, Taggart VS. Managing asthma in schools: Lessons learned and recommendations. J Sch Health. 2006;76(6):340–344. doi: 10.1111/j.1746-1561.2006.00125.x. [DOI] [PubMed] [Google Scholar]
- 4.Rasberry CN, Cheung K, Buckley R, et al. Indicators of asthma control among students in a rural, school-based asthma management program. J Asthma. doi: 10.3109/02770903.2014.913620. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brasler M, Lewis M. Teens: Taking control of asthma. J Sch Health. 2006;76(6):269–272. doi: 10.1111/j.1746-1561.2006.00110.x. [DOI] [PubMed] [Google Scholar]
- 6.Gerald LB, Redden D, Wittich AR, et al. Outcomes for a comprehensive school-based asthma management program. J Sch Health. 2006;76(6):291–296. doi: 10.1111/j.1746-1561.2006.00114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McLaughlin T, Maljanian R, Kornblum R, Clark P, Simpson J, McCormack K. Evaluating the availability and use of asthma action plans for school-based asthma care: A case study in Hartford, Connecticut. J Sch Health. 2006;76(6):325–328. doi: 10.1111/j.1746-1561.2006.00121.x. [DOI] [PubMed] [Google Scholar]
- 8.National Asthma Education and Prevention Program. Expert panel report 3: Guidelines for the diagnosis and management of asthma. National Heart, Lung, and Blood Institute; 2007. [Accessed June 14, 2013]. Available at: http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.pdf. [Google Scholar]
- 9.Wheeler L, Buckley R, Gerald LB, Merkle S, Morrison TA. Working with schools to improve pediatric asthma management. Pediatr Asthma Allergy Immunol. 2009;22(4):197–207. [Google Scholar]
- 10.Liu AH, Zeiger R, Sorkness CA, Mahr T, Ostrom N, Burgess S. Development and cross-sectional validation of the Childhood Asthma Control Test. J Allergy Clin Immunol. 2007;119(4):817–825. doi: 10.1016/j.jaci.2006.12.662. [DOI] [PubMed] [Google Scholar]
- 11.Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: A survey for assessing asthma control. J Allergy Clin Immunol. 2004;113(1):59–65. doi: 10.1016/j.jaci.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 12.United States Environmental Protection Agency. Asthma Home Environment Checklist. United States Environmental Protection Agency; 2004. [Accessed October 28, 2013]. Available at: http://www.epa.gov/asthma/pdfs/home_environment_checklist.pdf. [Google Scholar]
- 13.United States Environmental Protection Agency. Home Visits. United States Environmental Protection Agency; 2013. [Accessed October 28, 2013]. Available at: http://www.epa.gov/asthma/homevisits.html. [Google Scholar]
- 14.University of Missouri Health System, Child Health, Pulmonary Department. Asthma Ready Communities. Columbia, MO: 2013. [Accessed October 28, 2013]. Available at: http://asthmaready.org. [Google Scholar]
- 15.Centers for Disease Control and Prevention. Initiating change: Creating an asthma-friendly school. Centers for Disease Control and Prevention; Atlanta, GA: 2008. [Google Scholar]