Abstract
Splenic artery pseudoaneurysm is a rare entity. Clinical diagnosis is challenging because presentation is often varied. It can range from an incidental finding to hemodynamic collapse from sudden rupture and bleeding. The most common cause of this condition is pancreatitis. We report an unusual case of a young man not known to have pancreatitis who presented with hematemesis with normal esophagogastroduodenoscopy. Imaging modalities did not lead to a definitive diagnosis, and he underwent emergency laparotomy with surgical ligation of splenic artery pseudoaneurysm for hemodynamic instability, without a definitive preoperative diagnosis.
Key words: Splenic artery pseudoaneurysm
Splenic artery pseudoaneurysm (SAP) is a rare entity. Fewer than 200 cases of SAP have been reported in the literature.1 Clinical diagnosis remains challenging because presentation is often varied. It can range from an incidental finding to hemodynamic collapse from sudden rupture and bleeding.2 Therefore, a high index of suspicion is required. The most common cause of SAP is chronic pancreatitis.1 We report an unusual case of a young man not known to have pancreatitis who presented with hematemesis and hemodynamic instability not amenable to endoscopic hemostasis. He underwent emergency laparotomy and surgical ligation of SAP.
Case Report
A 24-year-old man was admitted with hematemesis. He had had two previous episodes of epigastric pain, which were attributed to gastritis. During the past admission for pain, he underwent an esophagogastroduodenoscopy (OGD) and abdomen ultrasound, which were normal. He was a nonsmoker and not an alcoholic. During this admission, he was in hypovolemic shock and underwent an urgent OGD. OGD was normal and he underwent a computerized tomography (CT) scan of the abdomen. CT scan revealed pancreatic cystic lesion with an exophytic lesion in the stomach (Fig. 1). Magnetic resonance cholangiopancreatography (MRCP) scan revealed dilated pancreatic duct with a cystic lesion in the pancreatic tail suspicious of main duct type of cystic lesion. MRCP also revealed an exophytic lesion at the greater curvature suspicious of gastrointestinal stromal tumor (Fig. 2). He developed further hematemesis while awaiting endoscopic ultrasound. OGD failed to visualize the bleeding spot, and he was scheduled for emergency exploratory laparotomy due to unstable hemodynamics. Intraoperatively, an SAP was found and ligated. Spleen was preserved. Postoperatively he recovered uneventfully and was discharged well.
Fig. 1.
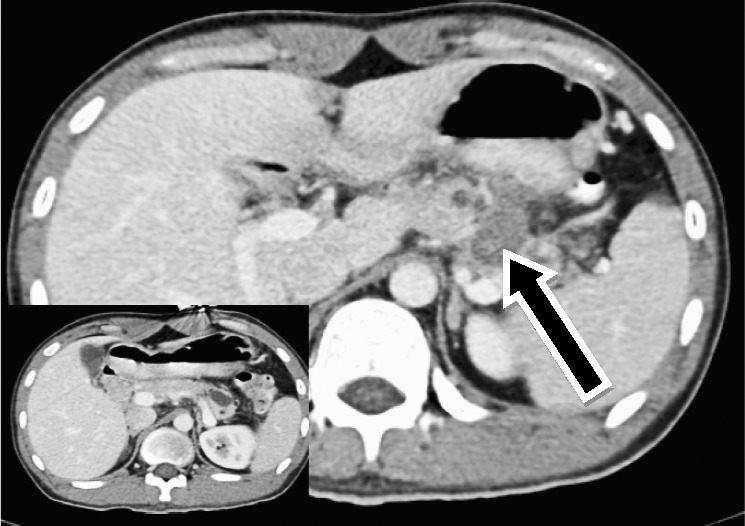
CT scan showing an exophytic lesion along the greater curvature of the stomach, along with a pancreatic cystic lesion at the tail. Inset: contrast filled stomach.
Fig. 2.

MRCP showing an exophytic lesion along the greater curvature of the stomach, along with the main duct type of pancreatic cystic lesion.
Discussion
Splenic artery is the most common artery known to form a pseudoaneurysm, with pancreatitis being the most common etiology. The mechanism behind pseudoaneurysm formation in pancreatitis is thought to occur via pancreatic enzymatic autodigestion of the splenic arterial wall, causing fragmentation of elastic tissue and weakening of the vessel wall architecture.3
Other causes of SAP include blunt abdominal trauma, peptic ulcer disease, and iatrogenic injury to splenic artery.1 Our patient is, to the best of our knowledge, the youngest patient reported in the literature with this condition and with no apparent risk factors. This case study also reinforced a frequently encountered diagnostic dilemma,4 with the underlying lesion masquerading as a possible gastrointestinal stromal tumor lesion on CT scan and cystic lesion of the pancreas on MRCP scan.
The mean age of patients with SAP was 51.2 years (range, 35–78 years) in the Tessier et al study.1 Few pseudoaneurysms are asymptomatic, and size is not a predictor of rupture.1 The common symptoms of SAP are abdominal pain, hematemesis, melena, flank pain, and chest pain. Hemorrhage from pseudoaneurysm can occur in the pseudocyst, stomach, pancreatic duct, peritoneal cavity, or retroperitoneum.5 Up to 58% of patients with bleeding are hemodynamically unstable at presentation.1 Correspondingly, this was also seen in our patient, who had repeated bleeding episodes with hemodynamic instability, which often hampered attempts to obtain a more definitive diagnosis.
Diagnosing SAP can be a difficult task, even with the advancement of adjunctive imaging techniques. CT scan is often used in the acute clinical setting to exclude other life-threatening conditions and can usually diagnose SAP, but small pseudoaneurysms may be missed.6 The gold standard for diagnosis is via direct catheter visceral angiography,4 which has the dual advantage of being both diagnostic and therapeutic. However, our patient did not have this window of opportunity, because he was hemodynamically unstable. Nevertheless, there have been reports of successful transcatheter embolization in hemodynamically unstable patients, suggesting that this may be a viable option in select patients.1 Other imaging modalities that are helpful for diagnosis include ultrasound Doppler, CT angiography, and magnetic resonance imaging. However, they do not offer concurrent therapeutic options and may mistake SAP for pancreatic pseudocyst or peripancreatic fluid collection. This was evident in our patient, who on MRCP was initially thought to have a cystic lesion of pancreas. Importantly, endoscopic ultrasound and drainage of suspected pancreatic pseudocyst can be catastrophic and are contraindicated when SAP is a possible differential diagnosis.
A variety of therapeutic interventions are available to treat SAP. Current guidelines advocate the treatment of all pseudoaneurysms to prevent sudden rupture and massive hemorrhage. Transarterial embolization of pseudoaneurysm using coils, thrombin injections, or gelfoam is the standard treatment when the patient is hemodynamically stable and diagnosis certain. Ligation of pseudoaneurysm with or without pancreatectomy (distal, partial, or total) and splenectomy is the standard treatment when the patient is hemodynamically unstable or embolization has failed.1,3,5,7 Good surgical judgment and early consultation with a vascular surgeon should be undertaken because surgical intervention has been reported to carry mortality and morbidity risks of 1.3% and 9%, respectively.8 Our patient had to undergo surgical treatment because of diagnostic dilemma and hemodynamic instability, and he recovered well postoperatively.
Conclusion
SAP is difficult to diagnose, and presentation can be varied. OGD can be normal even in patients with acute bleeding. Imaging modalities may not help to reach a confirmatory diagnosis. Prompt diagnosis is required so that definitive management with transarterial embolization can be attempted. If a patient is unstable or fails angioembolization, open surgical ligation of SAP should be performed.
References
- 1.Tessier DJ, Stone WM, Fowl RJ, Abbas MA, Andrews JC, Bower TC. Clinical features and management of splenic artery pseudoaneurysm: case series and cumulative review of literature. J Vasc Sug. 2003;38(5):969–974. doi: 10.1016/s0741-5214(03)00710-9. [DOI] [PubMed] [Google Scholar]
- 2.Nicaise N, Golzarian J, van Gansbeke D, Cremer M, Struyven J, Devière J. Rupture of pseudoaneurysm: a cause of delayed hemorrhage after endoscopic cystoenterostomy; angiographic diagnosis and treatment. Gastrointest Endosc. 1998;47(2):186–189. doi: 10.1016/s0016-5107(98)70356-6. [DOI] [PubMed] [Google Scholar]
- 3.Golzarian J, Nicaise N, Deviere J, Ghysels M, Wery D, Dussaussois L. Transcatheter embolization of pseudoaneurysms complicating pancreatitis. Cardiovasc Intervent Radiol. 1997;20(6):435–440. doi: 10.1007/s002709900189. [DOI] [PubMed] [Google Scholar]
- 4.Varshney P, Songra B, Mathur S, Gothwal S, Malik P, Rathi M. Splenic artery pseudoaneurysm presenting as massive hematemesis: a diagnostic dilemma. Case Rep Surg. 2014;2014:501937. doi: 10.1155/2014/501937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agarwal GA, Johnson PT, Fishman EK. Splenic artery aneurysms and pseudoaneurysms: clinical distinctions and CT appearances. Am J Roentgenol. 2007;188(4):992–999. doi: 10.2214/AJR.06.0794. [DOI] [PubMed] [Google Scholar]
- 6.Savastano S, Feltrin GP, Antonio T, Miotto D, Chiesurs-Corona M, Castellian L. Arterial complications of pancreatitis: diagnostic and therapeutic role of radiology. Pancreas. 1993;8(6):687–692. doi: 10.1097/00006676-199311000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Loffroy R, Guiu B, Cercueil JP, Lepage C, Cheynel N, Steinmetz E. Transcatheter arterial embolization of splenic artery aneurysms and pseudoaneurysms: short- and long-term results. Ann Vasc Surg. 2008;22(5):618–626. doi: 10.1016/j.avsg.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 8.Guillon R, Garcier JM, Abergel A, Mofid R, Garcia V, Chahid T. Management of splenic artery aneurysms and false aneurysms with endovascular treatment in 12 patients. Cardiovasc Intervent Radiol. 2003;26(3):256–260. doi: 10.1007/s00270-003-1948-y. [DOI] [PubMed] [Google Scholar]


