Abstract
Left colon perforation usually occurs in complicated diverticulitis or cancer. The most frequent signs are intraperitoneal abscess or peritonitis. In cases of retroperitoneal colonic perforation, diagnosis may be difficult. A 59-year-old woman presented with left thigh pain and with abdominal discomfort associated with mild dyspnea. Computed tomography scan showed air bubbles and purulent collection in the retroperitoneum, with subcutaneous emphysema extending from the left thigh to the neck. Computed tomography scan also revealed portal vein gas and thrombosis with multiple liver abscesses. An emergency laparotomy revealed a perforation of the proximal left colon. No masses were found. A left colectomy was performed. The retroperitoneum was drained and washed extensively. A negative pressure wound therapy was applied. A second-look laparotomy was performed 48 hours later. The retroperitoneum was drained and an end colostomy was performed. Intensive Care Unit postoperative stay was 9 days, and the patient was discharged on the 32nd postoperative day. Pneumoretroperitoneum and pneumomediastinum are rare signs of colonic retroperitoneal perforation. The diagnosis may be delayed, especially in the absence of peritoneal irritation. Clinical, laboratory, and especially radiologic parameters might be useful. Surgical treatment must be prompt to improve prognosis.
Key words: Pneumomediastinum, Retroperitoneum, Colonic, Perforation
Colonic perforation can be caused by either benign or malignant diseases. Left colon perforation is generally due to diverticular disease or cancer.1–3 Uncommon causes are iatrogenic ischemia, colonic ischemia, trauma, or toxic megacolon.1,3,4 Symptoms are usually due to abscesses or peritonitis. However, retroperitoneal ruptures can be difficult to diagnose because their presentation can vary widely.1,2,4–6
Through this case of retroperitoneal colonic perforation we aim to describe the presentation and therapeutic management of this entity.
Case Report
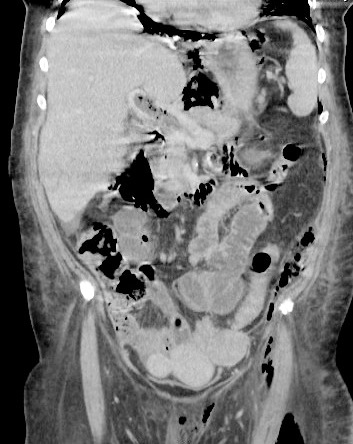
A 59-year-old woman presented with left thigh and back pain, asthenia, and abdominal discomfort associated with mild dyspnea. The woman had no significant past medical history. The abdomen was slightly distended without signs of peritoneal irritation. Full blood count revealed a raised white blood cell count (14.7 × 109/L), anemia (10.2 g/dL), prolonged prothrombin time (43%), and elevated procalcitonin (17.7 μg/L). A computed tomography (CT) scan showed air bubbles in the retroperitoneum, and subcutaneous emphysema extending from the left thigh to the neck (Figs. 1 and 2). No pneumoperitoneum was present. CT scan also revealed portal vein gas and thrombosis with multiple liver abscesses, in the left and right sides of the liver (Figs. 3 and 4). These CT images aroused suspicion of an underlying necrotizing fasciitis and a bowel perforation.
Fig. 1.
CT scan showing septic thrombophlebitis of the portal vein.
Fig. 2.

CT scan showing air in the portal vein.
Fig. 3.
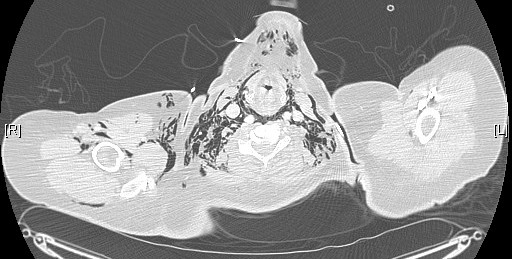
Axial CT images showing subcutaneous emphysema and pneumomediastinum.
Fig. 4.

CT scan showing bilateral pneumoretroperitoneum spreading to the thigh.
Airway obstruction due to subcutaneous emphysema in the neck required emergency orotracheal intubation. Emergency laparotomy was performed. The abdominal exploration found less than 300 mL of intraperitoneal fluid and the presence of hepatic abscess, and a perforation of the proximal left colon with no obvious masses was identified. A left colectomy was performed and retroperitoneal necrotic tissues were removed. Retroperitoneum was extensively washed and a negative pressure wound therapy (ABthera system, KCI, San Antonio, Texas) was applied.
A second-look laparotomy was performed after 48 hours. At the reopening of the laparostomy, the abdominal cavity appeared clean. There was a minor biliary leak from the necrotic parenchyma surrounding liver abscesses. Drains were placed in the retroperitoneum, in the Douglas sac, and in the right and left paracolic spaces. An end colostomy was performed.
An adapted multiple-antibiotic therapy and heparin therapy were administered.
Orotracheal tube was removed on the third postoperative day and the patient was discharged by the intensive care unit on the ninth postoperative day.
On the 11th postoperative day, the patient developed a biliary cutaneous fistula. A CT scan showed bile leaks in proximity to the left hepatic abscess (Fig. 5). Biliary cutaneous fistula was managed conservatively and no interventions were required.
Fig. 5.

CT scan showing the bile leakage and a left hepatic abscess.
Histologic examination of the surgical specimen confirmed a perforated diverticulum.
The patient was discharged on the 32nd postoperative day.
Discussion
Colonic retroperitoneal perforation is a rare clinical condition, and any age and sex can be affected by this condition. The most common cause of colonic retroperitoneal perforation is diverticular disease.1–6 Other causes can be cancer, colonic ischemia, toxic megacolon, iatrogenic perforation, or trauma.1–6 The diagnosis can be challenging for surgeons, and it may be delayed, especially in the absence of peritoneal signs and abdominal pain. The presence of thigh cellulites (more frequent is the involvement of the left thigh in diverticular perforation), psoas irritation, and pylephlebitis can suggest a clinical presentation of an intra-abdominal infection.5 The mechanism of the spread of abscess, gas, and necrosis along the retroperitoneum and mediastinum, for the anatomic connection between regions, was reported by Choi in 2011.1
No biochemical markers are currently available to detect this condition, unlike radiologic techniques, which can be very useful in these cases.6 In particular, CT scan, in stable patients, can be useful to detect the indirect signs of colonic perforation, such as pneumoretroperitoneum, pneumomediastinum, and subcutaneous emphysema, and gravity signs of abdominal infections, like pylephlebitis, portal vein gas and hepatic abscesses. However, it is not rare for diagnosis to be confirmed only intraoperatively or at histologic examination.
A rapid progression of infection and gas within tissues should raise the suspicion of necrotizing fasciitis. Most necrotizing soft tissue infections are caused by a mixture of aerobic and anaerobic bacteria (aerobic and anaerobic streptococci, coagulase-negative and coagulase-positive staphylococci, facultative and anaerobic Gram-negative rods, Bacteroides species, and Clostridium species) that act synergistically to cause fulminant infection.7 Many factors, including all septic parameters, clinical conditions, and laboratory results, such as leukocyte count, C-reactive protein, interleukin 6, lactate, base deficit, and procalcitonin (the optimal cutoff value was calculated at 1.14 for the procalcitonin ratio between postoperative days 1 and 2), can be taken into account for the decision to increase or decrease surgical aggressiveness.8
Surgery may be lifesaving in acute events and in most cases, but in the absence of necrotizing fasciitis, a radical colonic resection should be avoided in asymptomatic patients with multiple comorbidities.7–9 In these cases, the conservative approach might be possible, but there is a lack of published evidence regarding this topic.10 In cases of necrotizing fasciitis a targeted antibiotic treatment and a radical surgical treatment are necessary to improve the outcomes.7,8,11
Surgical procedures proposed in the literature were: Hartmann procedure, double-barrel colostomy, sigmoidectomy and coloproctectomy, segmental resection and anastomosis with or without covering loop ileostomy, and radical debridement.
Authors report high mortality rates (34%–93%) in patients with emphysema of the thigh complicating a colonic perforation, especially in cases of conservative management. This rate decreases to 34% in patients treated also for the perforation.10
Conclusions
Pneumoretroperitoneum and pneumomediastinum are rare signs of colonic perforation. The diagnosis may be delayed, especially in the absence of peritoneal irritation. Clinical parameters, laboratory parameters, and CT scan might be useful. A timely and correct diagnosis associated with a rapid surgical treatment may be essential for improved prognosis.
Acknowledgments
An earlier version of this manuscript was presented at the 2nd World Congress of the World Society of Emergency Surgery, July 7–9, 2013, Bergamo, Italy.
References
- 1.Choi PW. Pneumomediastinum caused by colonic diverticulitis perforation. J Korean Surg Soc. 2011;80(suppl 1):S17–S20. doi: 10.4174/jkss.2011.80.Suppl1.S17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yaşar NF, Kebapçı M, Ihtiyar E. Pneumomediastinum and subcutaneous emphysema caused by sigmoid diverticulum perforation secondary to blunt abdominal trauma: report of a case. Ulus Travma Acil Cerrahi Derg. 2011;17(1):93–95. doi: 10.5505/tjtes.2011.69783. [DOI] [PubMed] [Google Scholar]
- 3.Biondo S, Parés D, Martí Ragué J, De Oca J, Toral D, Borobia FG, et al. Emergency operations for nondiverticular perforation of the left colon. Am J Surg. 2002;183(3):256–260. doi: 10.1016/s0002-9610(02)00780-8. [DOI] [PubMed] [Google Scholar]
- 4.Mogan GR, Sachar DB, Bauer J, Salky B, Janowitz HD. Toxic megacolon in ulcerative colitis complicated by pneumomediastinum: report of two cases. Gastroenterology. 1980;79(3):559–562. [PubMed] [Google Scholar]
- 5.Mailleux P, Maldague P, Coulier B. Pylephlebitis complicating peridiverticulitis without hepatic abscess: early detection with contrast-enhanced CT of the abdomen. JBR-BTR. 2012;95(1):13–14. [PubMed] [Google Scholar]
- 6.Sivarajah V, Jones C, Pittathankal A. Radiological evidence of subcutaneous emphysema leading to a diagnosis of retroperitoneal perforated diverticulum. Int J Surg Case Rep. 2013;4(6):531–533. doi: 10.1016/j.ijscr.2013.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Urschel JD. Necrotizing soft tissue infections. Postgrad Med J. 1999;75(889):645–649. doi: 10.1136/pgmj.75.889.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Friederichs J, Hutter M, Hierholzer C, Novotny A, Friess H, Bühren V. Procalcitonin ration as a predictor of successful surgical treatment of severe necrotizing soft tissue infections. Am J Surg. 2013;206(3):368–373. doi: 10.1016/j.amjsurg.2012.11.024. [DOI] [PubMed] [Google Scholar]
- 9.Rees JR, Burgess P. Conservative management of complex diverticular disease causing a retroperitoneal perforation. BMJ Case Rep. 20092009 doi: 10.1136/bcr.03.2009.1692. bcr03.2009.1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ioannidis O, Kakoutis E, Paraskevas G, Chatzopoulos S, Kotronis A, Papadimitriou N. Emphysematous cellulitis of the left thigh caused by sigmoid diverticulum perforation. Ann Ital Chir. 2011;82(3):217–220. [PubMed] [Google Scholar]
- 11.Elliott DC, Kufera JA, Myers RA. Necrotizing soft tissue infections: risk factors for mortality and strategies for management. Ann Surg. 1996;224(5):672–683. doi: 10.1097/00000658-199611000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]


