Abstract
Background
We assessed whether a high-resolution impedance manometry (HRIM) metric, bolus flow time (BFT) across the esophagogastric junction (EGJ), was abnormal in achalasia patients subtyped by the Chicago Classification and compared BFT to other HRM metrics.
Methods
HRIM studies were performed in 60 achalasia patients (14 type I, 36 type II and 10 type III) and 15 healthy controls. Studies were analyzed with a MATLAB program to calculate BFT using a virtual HRIM sleeve. Integrated relaxation pressure (IRP) and basal end-expiratory EGJ pressure were also calculated. The relationship between BFT and dysphagia symptom scores was assessed using the impaction dysphagia questionnaire (IDQ).
Key Results
Median BFT was significantly lower in achalasia patients (0.5 s, range 0.0 to 3.5 s) compared to controls (3.5 s, range 2.0 to 5.0 s) (P<0.05). BFT was significantly lower in types I and II than in type III achalasia in both the supine and upright positions (p<0.0001). BFT was the only HRIM metric significantly associated with IDQ score in both the supine (R2 =0.20, p=0.0046) and upright positions (R2 =0.27, p=0.0002).
Conclusions & Inferences
BFT was significantly reduced in all subtypes of achalasia and complementary to the IRP as a diagnostic discriminant in equivocal achalasia cases. Additionally, BFT had a more robust correlation with dysphagia severity compared to other metrics of EGJ function.
Keywords: achalasia, impedance, manometry, dysphagia, esophagus
INTRODUCTION
The introduction of high-resolution manometry (HRM) and esophageal pressure topography (EPT) has improved our ability to visualize pressurization patterns and define their relationship to contractile activity and manometric landmarks1. This added detail facilitated the development of a new classification of achalasia that can inform treatment efficacy based on the presence or absence of panesophageal pressurization and premature spastic contractions2. However, issues regarding an optimal panesophageal pressurization cut-off value for type II achalasia and the potential for false negative results related to limitations of the integrated relaxation pressure (IRP) remain important limitations of the classification scheme2, 3. Intraluminal impedance monitoring provides a surrogate for bolus transit that adds a dimension to HRM. However, its implementation as a dichotomous variable hampered its use in clinical practice, as it does not detail flow dynamics beyond documentation of incomplete bolus transit.
Combining impedance monitoring with HRM and applying new approaches to visualizing bolus presence through the EGJ is a logical next step in the evolution of esophageal function testing that could fill the current gaps in each technology 4–6. This approach was first attempted in the assessment of bolus passage through the pharyngo-esophageal segment using a combined automated impedance manometry (AIM) approach. Subsequently, AIM was further modified to evaluate non-achalasia esophageal dysphagia,7 e.g. cases in which there was a propagated contraction. Using an alternative approach for analyzing impedance changes through the EGJ, Hong et al. explored the mechanisms of pressurization and emptying of the esophagus by combining HRM with impedance and simultaneous intraluminal ultrasound evaluation8. Their findings suggested that impedance changes through the EGJ could help delineate EGJ opening. We recently developed a new approach building on the work of the AIM group and Hong et al. that defined bolus opening and flow through the EGJ using a virtual high-resolution impedance manometry (HRIM) sleeve. This approach utilizes nadir impedance as a surrogate of bolus presence within the EGJ. An additional criterion for flow was that the trans-EGJ pressure gradients be flow-permissive 9. The correlation between trans-EGJ bolus flow times defined on fluoroscopy and bolus flow times (BFT) defined using the virtual HRIM sleeve was excellent9.
We hypothesize that BFT can be applied to achalasia to better understand the pathogenesis of impaired bolus transit and further refine our diagnostic classification scheme. In particular, this information may prove useful when the IRP is equivocal and when the diagnosis is uncertain. Hence, the aim of this study was to compare BFT to our current standard HRM metrics utilized to assess abnormal EGJ function in achalasia. Additionally, we also sought to determine whether BFT was associated with dysphagia severity.
METHODS
Subjects
Sixty patients with newly diagnosed achalasia (58% male, mean age 49, range 19–82 years) underwent HRIM and symptom assessment before intervention. These patients were being referred for definitive therapy (pneumatic dilation, per-oral endoscopic myotomy or Heller myotomy) and the diagnosis was confirmed using a combination of endoscopy, manometry and, in equivocal cases, a timed barium esophagram. Additionally, 15 healthy asymptomatic subjects (47% male, mean age 33, range 20–50 years) recruited from our previous validation study were utilized as a comparator group 9. Volunteers were recruited by advertisement or word of mouth and had no history of gastrointestinal symptoms or surgery. The study protocol was approved by the Northwestern University Institutional Review Board and informed consent was obtained from each study participant.
Symptom Assessment
Symptoms of dysphagia, chest pain and regurgitation were assessed with the Impaction-Dysphagia Questionnaire (IDQ) using the cumulative score as a descriptor of difficulty eating, pain with swallowing and food impaction. Ten questions with a six-point Likert score rating the frequency (0=none to 5=daily) and severity (0=none to 5=severe) of symptoms was utilized with a scoring range of 0 to 50.
Study protocol
HRIM studies were done after at least a six-hour fast. The HRIM catheter was a 4.2 mm outer diameter solid-state assembly with 36 circumferential pressure sensors at 1-cm intervals and also incorporated 18 impedance segments at 2 cm intervals (Medtronic Inc, Shoreview, MN). Transducers were calibrated at 0 and 300 mmHg using externally applied pressure. The HRIM assembly was placed transnasally and positioned to record from the hypopharynx to the stomach with about three intragastric pressure sensors. The HRIM protocol included a 5-minute baseline recording, ten 5-ml swallows in a supine position, and five 5-ml swallows in the upright position using 50% saline for test swallows at 20–30 s intervals. Measurements of integrated relaxation pressure IRP and baseline end-expiratory EGJ pressure (EE-EGJP) were performed using Manoview 3.0 (Medtronic Inc, Shoreview, MN).
Data analysis
Manometry studies were analyzed using ManoView 3.0 analysis software. The key metric in cases of achalasia is the IRP, which quantifies EGJ relaxation both in completeness and persistence. The upper limit of normal of the mean IRP for the 10-swallow protocol with this manometric system is <15mmHg. Additional measures of EGJ function analyzed were the mean resting EE-EGJP during the baseline recording using the isobaric contour tool on the ManoView 3.0 software. A measure of intrabolus pressure (IBP) using the isobaric contour tool was also made in the supine and upright position by determining the magnitude of pressure at which the isobaric contour break first occurred along the length of the esophagus. In type I and II achalasia, this represented the magnitude of panesophageal pressurization.
The virtual HRIM sleeve for calculating BFT through the EGJ
An automated virtual HRIM sleeve was created using 3 impedance and 3 manometry sensors placed through the EGJ with the distal manometry and impedance sensor positioned within the hiatus (identified by the crural contraction) to calculate BFT using the criteria developed for bolus presence in the EGJ as previously described 9. This allowed an assessment of duration and direction of bolus flow and delineated periods of a flow-permissive EGJ pressure gradient using a gastric pressure reference.
The automated HRIM virtual sleeve was created by exporting HRIM data from each subject from ManoView to MATLAB™ (The MathWorks Inc., Natick, MA, U.S.A.). Four functional analytic steps were performed in the MATLAB analysis as previously described 9 (Figures 1A and 1B): 1) interpolation to optimize and match the resolution of the impedance and manometry signals; 2) define the spatial and temporal region of interest; 3) identify potential regions of bolus presence within the EGJ defined as the intervals during which there was at least a 50% drop in impedance; if the impedance drop was not greater than 50% at each axial location, BFT was considered to be 0; the onset of actual bolus presence was taken as the point at which the impedance dropped 90% to nadir; offset bolus presence with return to 50% impedance baseline; 4) deriving BFT as the sum of all periods meeting the criteria of both bolus presence and manometrically defined flow-permissive time, subtracting any time period during a crural contraction.
Figure 1.
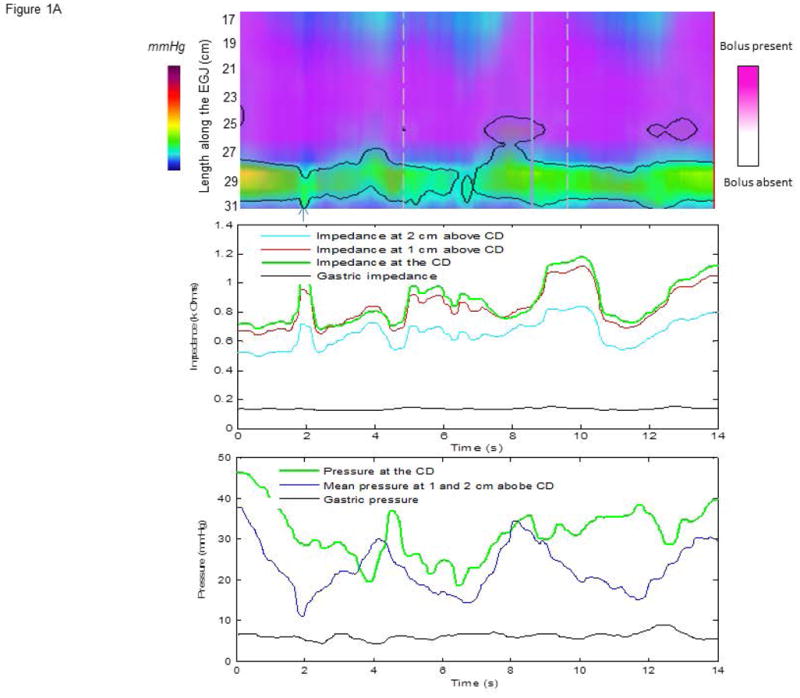
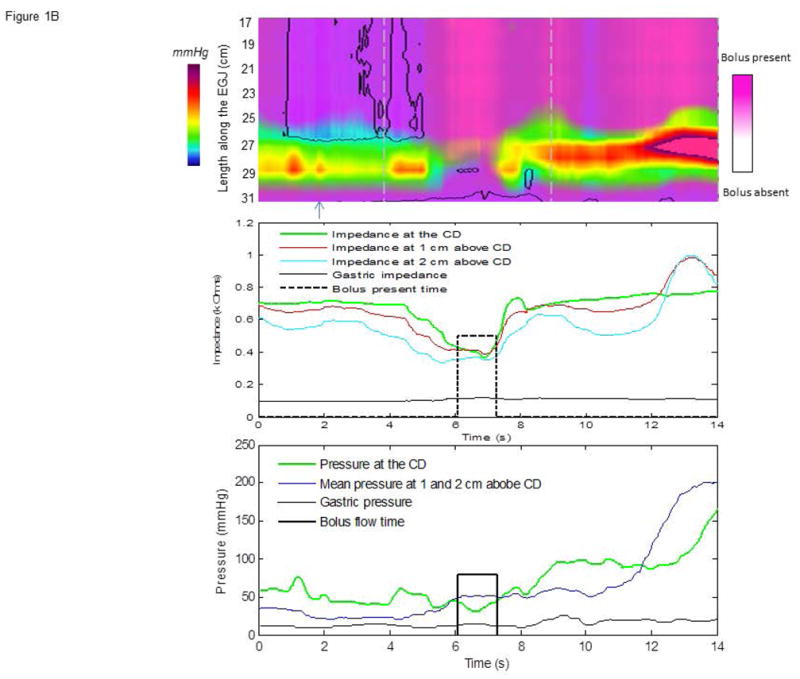
Examples of: (A) type I achalasia with a BFT of zero and (B) type II achalasia with a BFT of 1.25 s. The top panels show the EPT plot with overlying impedance topography. In Figure 1A, there is no period of 50% drop in impedance (middle panel) and no period of relaxation to <15 mmHg (bottom panel, crural diaphragm (CD) line). This suggests poor relaxation and no opening. There are limited time periods during which the mean pressure above the CD (bottom panel, blue pink line) exceeds pressure at the crural diaphragm (green line) suggesting a flow-permissive gradient. However, since both impedance and manometric criteria are requisite, the BFT is 0. In Figure 1B (middle panel) there is a 50% drop in each impedance recording suggesting EGJ opening. The BFT algorithm defines the onset of opening as the time at which the impedance drop achieves 90% of its nadir value at all three impedance loci and the offset as return to the 50% point indicated by the black dashed line. In the lower panel, a preferential flow gradient is noted when mean pressure above the CD (blue line) are greater than the CD (green line) and gastric pressure (black line). The solid black line indicates the interval that all BFT criteria are met, totaling 1.25 s in this case.
Statistical analysis
Descriptive statistics for all continuous and ordinal measures were presented as median and interquartile range (IQR). Analysis of variance tests (ANOVAs), and in the case of violations of normality assumptions (e.g., BFT), Kruskal-Wallis tests were utilized to compare mean (or median) values of continuous outcomes across classification types (and across categories of other potential predictors; e.g., gender). Tukey’s adjustment for multiple pairwise comparisons was employed to examine pairwise differences (e.g., type I vs. type III, type I vs. type II, and type II vs. type III). Bivariate associations between continuous variables were evaluated via Pearson’s sample correlation coefficients and/or Spearman’s sample correlation coefficients in cases of possible violation of relevant statistical assumptions. Finally, multiple linear regression models were used to examine association between BFT and IDQ symptom score, controlling for potential confounders. Supine and upright BFT were examined separately for association with outcome. Analyses assumed a 5% level of statistical significance, and all statistical analyses were conducted in SAS version 9.4 (The SAS Institute; Cary, NC).
RESULTS
HRM metrics of EGJ function in achalasia and healthy controls
The median (IQR) BFT in 15 healthy control subjects was 3.5 s (2.3–3.9 s) in supine position and 3.2 s (2.3–3.6 s) in the upright position. The 5th percentile for normal controls was 2.0 s. The median BFT (IQR) in the 60 achalasia patients was 0.45 s (0.0–1.2s) in the supine position and 0.0s (0.0–1.1s) in the upright position. BFT was significant greater in the healthy controls compared to the achalasia patients as a whole in both the supine (P<0.0001) and upright (P<0.0001) positions. The median (IQR) IRP in the healthy controls in the supine position was 8.4 mmHg (6.0–9.1 mmHg) and 1.5 mmHg (0.7–5.3 mmHg) in the upright position. The median (IQR) IRP in the achalasia patients in the supine position was 31.1 mmHg (21.7–41.0 mmHg) and 28.4 mmHg (18.1–40.7 mmHg) in the upright position. IRP was significant lower in the healthy controls compared to the achalasia patients as a whole in both the supine (P<0.0001) and upright (P<0.0001) position.
HRIM metrics among achalasia subtypes
Comparisons of demographic data and HRIM variables among achalasia subtypes are presented in Table 1. There was a significant difference in age across the three subtype classifications, with type III being older on average than both type I and II (P<0.0001). Mean IDQ score was significantly lower in type III compared to type II patients (adjusted p=0.0120) and there was a trend toward lower mean IDQ score for type III patients when compared to type I (adjusted p=0.0842). There were no statistically significant differences noted among the subtypes in terms of mean IRP or mean EE-EGJP in either the supine or upright position. The median BFT was significantly lower in types I and II when compared to type III in both the supine (Kruskal-Wallis p=0.0005) and upright positions (Kruskal-Wallis p=0.0089). Using a cutoff of 1 s for BFT as a dichotomous endpoint, 93% (13 of 14) of type I, 72% (26 of 36) of type II and 10% (1 of 10) of type III patients had a value less than 1.0 s in the supine position (Fisher’s exact p<0.0001) while 93% (13 of 14) of type I, 72% (26 of 36) of type II and 30% (3 of 10) of type III patients had a value less than 1.0 s in the upright position (Fisher’s exact p=0.0035).
Table 1.
HRM metrics of EGJ Function in Achalasia Subtype
| Type I (n=14) | Type II (n=36) | Type III (n=10) | |
|---|---|---|---|
| Age* | 41.0 (35.0–55.0) | 47 (26.8–57.5) | 69 (64–80.3) |
| Sex | 8M/6F | 21M/15F | 6M/4F |
| BMI | 23.9 (22.3–26.45) | 25.2 (22.4–28.2) | 27.3 (22.4–28.2) |
| IDQ* | 22.5 (21.0–31.0) | 26.0 (17.5–35.5) | 17.5 (9.2–23.0) |
| Supine-BFT (s)* | 0.0 (0.0–0.5) | 0.2 (0.0–1.3) | 1.3 (1.2–2.4) |
| Supine-IRP (mmHg) | 25.0 (15.0–32.0) | 32.7 (23.2–46.0) | 31.0 (22.0–42.0) |
| Supine-EE-EGJP (mmHg) | 19.0 (13.0–25.0) | 27.5 (20.5–38.5) | 27.0 (21.0–40.0) |
| Upright-BFT (s)* | 0.0 (0.0–0.0) | 0.0 (0.0–1.1) | 1.1 (0.8–1.6) |
| Upright-IRP (mmHg) | 18.3 (10.8–29.9) | 31.1 (22.4–43.0) | 31.4 (24.0–45.4) |
| Upright-EE- EGJP(mmHg) | 16.0 (12.0–26.0) | 25.0 (17.0–38.5) | 27.0 (20.0–42.0) |
Note:
P<0.05 for comparison amongst the classification groups;
BFT, bolus flow time; IRP, integrated relaxation pressure; EE-EGJP, end-expiratory esophagogastric junction pressure
Predictors of IDQ score
Spearman’s sample correlation revealed that BFT in the supine position had a significant negative correlation with IDQ score (r=−0.42 with 95% CI [−0.61, −0.18]; p=0.0008). Similarly, BFT in the upright position was also significantly negatively correlated with IDQ (r=−0.53, 95% CI [−0.69. −0.31]; p<0.0001).
Pearson’s sample correlation coefficient suggested a significant negative linear correlation between age and IDQ score (r=−0.33, [−0.54, −0.08]; p=0.0096), while there was no significant association noted between IDQ score and body mass index (BMI) (Pearson’s r, p=0.3088) or gender (t-test; p=0.2275). In addition, there were no statistically significant associations between IDQ score and supine/upright IRP or supine/upright EE-EGJ, and there was evidence of a marginal association between achalasia subtype and IDQ (p=0.0413).
Given the associations of age and achalasia subtype with IDQ score, linear models for IDQ involving BFT controlled for these two potential covariates. The adjusted R-squared in the model revealed that the upright BFT was slightly more predictive (R2 =0.27, model-adjusted Wald p-value for BFT = 0.0002) than the supine BFT (R2 =0.20, p=0.0046).
Concordance between IDQ, BFT and IRP
Overall, there was no significant correlation between BFT and IRP (Spearman’s r=−0.14. p=0.2878 upright; Spearman’s r=−0.15; p=0.2544 supine). Almost half of the patients (47%, 28 of 60) had a median supine BFT of 0 s. In the supine position, there were seven patients with an IRP ≤15 mmHg and an IDQ score >10. Of these, six patients had a BFT <2.0 s (5th percentile), suggesting limited opening despite a normal IRP. There was one patient with supine BFT >3.0 s, and this patient had a supine IRP of 12.4 mmHg.
DISCUSSION
The aim of this study was to determine whether a new metric devised using HRIM could be utilized to assess esophageal function and dysphagia severity in achalasia. Our findings suggest that BFT provides information above and beyond the Chicago Classification measures of EGJ function devised for HRM. In this dataset, BFT was significantly lower in achalasia patients compared to controls and it was also significantly lower in type I and II compared to type III achalasia. Furthermore, the correlation between BFT and IDQ score was significant which was not the case with either the IRP or the EE-EGJP. More importantly, the BFT was abnormal in patients with a clinical diagnosis of achalasia despite an IRP <15 mmHg suggesting that this metric had discriminant diagnostic utility.
The widespread adoption of HRM elicited a new appreciation of the problems associated with measuring lower esophageal sphincter (LES) relaxation. Well before HRM, Dent et al recognized the movement artifact associated with swallowing and developed the Dent Sleeve to circumvent the problem of ‘pseudorelaxation’ related to axial movement of the LES10. This principle was enhanced and adapted to HRM by the work of Staiano and Clouse with the description of an electronic sleeve11. Those investigators determined that the optimal measure of deglutitive LES relaxation was the mean pressure during the 3-s post-swallow interval, with maximal relaxation measured using an electronic sleeve. Using the 3-s mean maximized the discriminant value of the metric by minimizing error attributable to movement artifact and spurious pressure transients. Notably, that same investigation reported that the trans-sphincteric pressure gradient was also helpful in diagnosing achalasia, as this was another important determinant of EGJ flow.
As HRM evolved, it became evident that the continuous 3-s measure of residual EGJ pressure was suboptimal because of the potential for crural contractions to be incorporated into the measurement. The next logical step was to eliminate periods of crural contraction from the measurement. Hence, the development of the IRP, which reported the mean value of the lowest residual pressure through the electronic sleeve for four seconds, not requiring that they be contiguous12. This modification reduced false positive results and became the standard for diagnosing achalasia. However, new issues arose regarding instances of clinically-evident achalasia with an IRP <15 mmHg. Most commonly this occurred in type I achalasia patients with low intra-esophageal pressures and type II achalasia patients with short periods of panesophageal pressurizations. Subsequently, a classification and regression tree model suggested that the IRP cutoff value should be modified based on the esophageal contractile and pressurization pattern. This was logical because the IRP is partially dependent on the intrabolus pressure developed within the esophagus13.
To improve on the detection of EGJ dysfunction beyond what is achieved with current HRM metrics, we now incorporate concepts from recent literature on simultaneous impedance and manometry 5–8 and developed a new complex metric, the BFT, that requires both impedance-defined EGJ opening and manometrically-defined flow-permissive time. Using a three cm virtual HRIM sleeve through the EGJ, we developed a paradigm that accurately determined the time points where the EGJ was open and flow was occurring as validated by fluoroscopy9. The recognition that the nadir impedance through the EGJ made us revisit our original work focused on using impedance manometry to assess flow through the EGJ14. We realized that the nadir impedance value through the EGJ during a swallow was more accurate marker of bolus presence and that although the 50% drop in impedance was required, it more likely reflects a change in contact pressure with the impedance sensors during relaxation9.
Given the excellent agreement between BFT and bolus flow on fluoroscopy, we hypothesized that the BFT measure could be helpful in equivocal cases of achalasia as it defines the conversion of the sphincter from a state of isometric relaxation to a state of passive distention and opening related to trans-EGJ flow15. The BFT bypasses the confounding issue of low intra-esophageal pressure and also provides a more comprehensive analysis of EGJ function, complementing the IRP which is only reflective of isometric relaxation. Our findings suggest that the BFT was significantly lower in achalasia and, most interesting, that it was much lower in type I and type II when compared to type III achalasia. This likely reflects the fact that type III achalasia patients can generate sufficient intrabolus pressure to open the EGJ during swallows. Additionally, the data suggest that the BFT was reduced in cases in which the IRP was <15 mmHg despite a clinical presentation consistent with achalasia. We hypothesize that the BFT could act as an arbiter of such equivocal cases and that this would be more objective approach than modifying the IRP cutoff values based on achalasia subtype.
Another aspect of the BFT supporting its clinical utility was its strong relationship to dysphagia severity. Previous investigations suggest that measures of EGJ function are not strongly associated with symptom severity16. This is likely related to the fact that the relationship between these measures is not linear and modified by other factors such as intra-esophageal pressure and the trans-sphincteric pressure gradient. In contrast, the BFT calculation utilizes intra-esophageal pressure and the trans-sphincteric pressure gradient making it is a much more comprehensive assessment of esophageal emptying dynamics.
This work has limitations as it requires both HRIM recordings and MATLAB programming thereby making it not widely available. Although automated, the technique still requires identification of appropriate landmarks and will be subject to the expertise of the interpreter in localizing the hiatus. Additionally, the HRIM sleeve may need to be positioned within the LES zone in cases of hiatus hernia. Although a significant hiatus hernia is unusual in achalasia, this consideration may be important in other disease states and further study is required. Furthermore, there is also no diagnostic cutoff value for achalasia as some achalasia patients had values in the normal range. Of course, this is no different than what is found with the IRP, nadir LES relaxation, and trans-sphincteric gradients. The thought that a heterogeneous disorder such as achalasia can be uniformly detected with a perfect diagnostic cut-off using a single measurement is unreasonable. Rather, we would propose that the BFT act as an adjudicator of equivocal cases, similar to the timed barium esophagram.
In conclusion, we developed a technique that extends the measure of deglutitive EGJ function from a metric purely focused on assessing the level of resistance to flow during deglutitive relaxation to one that incorporates a measure of opening. Our findings suggest that the BFT can be utilized as a diagnostic discriminant in equivocal achalasia cases. Additionally, we think that the BFT may be an important post-treatment outcome measure as it is a more comprehensive metric of forces that are both driving and resisting emptying. Future studies are required to test this role and further work will be needed to adapt this approach into a more user-friendly analysis package.
Figure 2.
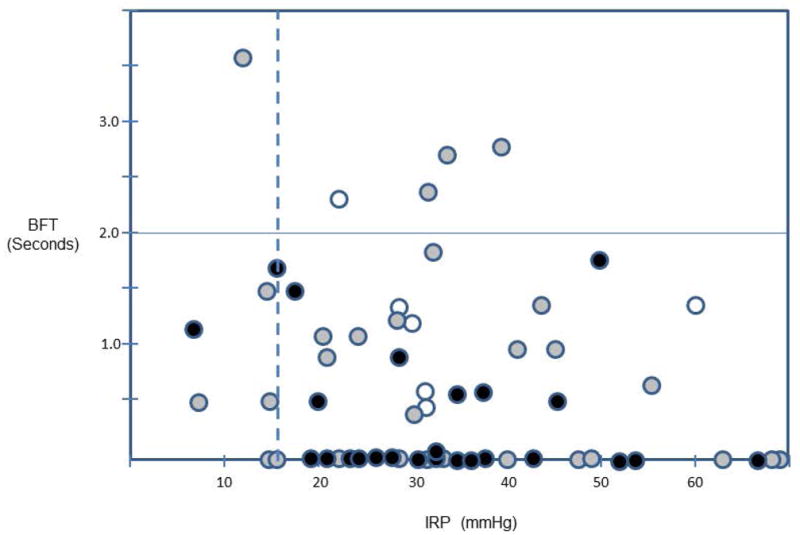
Concordance of HRM metrics in the context of dysphagia severity. IRP is on the X-axis, BFT is on the y-axis, and the corresponding supine values of the 60 achalasia patients are plotted. The circles are colored to represent gradations of IDQ score (white <10, gray 10–25, black >25). There are 5 instances in which the IRP is within the normal range (<15 mmHg), whom BFT values are < 2 s.
Key Messages.
A new metric, bolus flow time (BFT) across the EGJ was significantly reduced in all subtypes of achalasia and complementary to the IRP as a diagnostic discriminant in equivocal achalasia cases. Additionally, BFT had a more robust correlation with dysphagia severity compared to other metrics of EGJ function.
The goal of this study was to determine whether BFT devised using HRIM could be utilized to assess esophageal function and dysphagia severity in achalasia.
HRIM studies were performed in 60 achalasia patients and 15 healthy controls and were analyzed with a MATLAB program to calculate BFT using a virtual HRIM sleeve. The relationship between BFT and dysphagia symptom scores was assessed using the impaction dysphagia questionnaire (IDQ).
In this dataset, BFT was significantly lower in achalasia patients compared to controls and it was also significantly lower in type I and II compared to type III achalasia. Furthermore, BFT was the only HRIM metric significantly associated with IDQ score.
Acknowledgments
Financial support: This work was supported by R01 DK079902 (JEP) from the National Institutes of Health, USA.
Abbreviations
- BFT
bolus flow time
- EE-EGJP
end expiratory esophagogastric junction pressure
- EPT
esophageal pressure topography
- EGJ
esophagogastric junction
- HRM
high resolution manometry
- HRIM
high-resolution impedance manometry
- IDQ
Impaction Dysphagia Questionnaire
- IRP
integrated relaxation pressure
- LES
lower esophageal sphincter
Footnotes
Specific author contributions: Zhiyue Lin contributed to data analysis and interpretation, manuscript revision and final approval. Peter J. Kahrilas contributed to the study design, data interpretation, manuscript editing, critical revision and final approval. Jody Ciolino contributed to the data analysis and the manuscript drafting. Joel Sternbach, Dusty Carlson, Eric Hungness and Kristina Dykstra contributed to the organization of data and recruitment of patients. John E. Pandolfino contributed to the conception and study design, obtained funding, data analysis and interpretation, manuscript drafting, editing, critical revision and final approval.
Potential competing interests: John E. Pandolfino [Given Imaging, Sandhill Scientific (consulting, educational)]; No relevant competing financial and other interests exist for other authors (Z.L., J.C., E.H., K.D., D.C, J.S., P.J.K.).
References
- 1.Clouse RE, Staiano A. Topography of normal and high-amplitude esophageal peristalsis. Am J Physiol. 1993;265:G1098–1107. doi: 10.1152/ajpgi.1993.265.6.G1098. [DOI] [PubMed] [Google Scholar]
- 2.Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–74. doi: 10.1111/nmo.12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lin Z, Kahrilas PJ, Roman S, et al. Refining the criterion for an abnormal Integrated Relaxation Pressure in esophageal pressure topography based on the pattern of esophageal contractility using a classification and regression tree model. Neurogastroenterol Motil. 2012;24:e356–63. doi: 10.1111/j.1365-2982.2012.01952.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Noll L, Rommel N, Davidson GP, et al. Pharyngeal flow interval: a novel impedance-based parameter correlating with aspiration. Neurogastroenterol Motil. 2011;23:551–e206. doi: 10.1111/j.1365-2982.2010.01634.x. [DOI] [PubMed] [Google Scholar]
- 5.Omari TI, Papathanasopoulos A, Dejaeger E, et al. Reproducibility and agreement of pharyngeal automated impedance manometry with videofluoroscopy. Clin Gastroenterol Hepatol. 2011;9:862–7. doi: 10.1016/j.cgh.2011.05.026. [DOI] [PubMed] [Google Scholar]
- 6.Omari TI, Rommel N, Szczesniak MM, et al. Assessment of intraluminal impedance for the detection of pharyngeal bolus flow during swallowing in healthy adults. Am J Physiol Gastrointest Liver Physiol. 2006;290:G183–8. doi: 10.1152/ajpgi.00011.2005. [DOI] [PubMed] [Google Scholar]
- 7.Rommel N, Van Oudenhove L, Tack J, et al. Automated impedance manometry analysis as a method to assess esophageal function. Neurogastroenterol Motil. 2014;26:636–45. doi: 10.1111/nmo.12308. [DOI] [PubMed] [Google Scholar]
- 8.Hong SJ, Bhargava V, Jiang Y, et al. A unique esophageal motor pattern that involves longitudinal muscles is responsible for emptying in achalasia esophagus. Gastroenterology. 2010;139:102–11. doi: 10.1053/j.gastro.2010.03.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin Z, Imam H, Nicodeme F, et al. Flow time through esophagogastric junction derived during high-resolution impedance-manometry studies: a novel parameter for assessing esophageal bolus transit. Am J Physiol Gastrointest Liver Physiol. 2014;307:G158–63. doi: 10.1152/ajpgi.00119.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Linehan JH, Dent J, Dodds WJ, et al. Sleeve device functions as a Starling resistor to record sphincter pressure. Am J Physiol. 1985;248:G251–5. doi: 10.1152/ajpgi.1985.248.2.G251. [DOI] [PubMed] [Google Scholar]
- 11.Staiano A, Clouse RE. Detection of incomplete lower esophageal sphincter relaxation with conventional point-pressure sensors. Am J Gastroenterol. 2001;96:3258–67. doi: 10.1111/j.1572-0241.2001.05323.x. [DOI] [PubMed] [Google Scholar]
- 12.Ghosh SK, Pandolfino JE, Rice J, et al. Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitative analysis of 400 patients and 75 controls. Am J Physiol Gastrointest Liver Physiol. 2007;293:G878–85. doi: 10.1152/ajpgi.00252.2007. [DOI] [PubMed] [Google Scholar]
- 13.Lin Z, Kahrilas PJ, Roman S, et al. Improving the Integrated Relaxation Pressure (IRP) cutoff value for the diagnosis of achalasia using a classification and regression tree (CART) model. Gastroenterology. 2012 Abstract. [Google Scholar]
- 14.Pandolfino JE, Shi G, Zhang Q, et al. Measuring EGJ opening patterns using high resolution intraluminal impedance. Neurogastroenterol Motil. 2005;17:200–6. doi: 10.1111/j.1365-2982.2004.00589.x. [DOI] [PubMed] [Google Scholar]
- 15.Lin Z, Yim B, Gawron A, et al. The four phases of esophageal bolus transit defined by high-resolution impedance manometry and fluoroscopy. Am J Physiol Gastrointest Liver Physiol. 2014;307:G437–44. doi: 10.1152/ajpgi.00148.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lazarescu A, Karamanolis G, Aprile L, et al. Perception of dysphagia: lack of correlation with objective measurements of esophageal function. Neurogastroenterol Motil. 2010;22:1292–7. e336–7. doi: 10.1111/j.1365-2982.2010.01578.x. [DOI] [PubMed] [Google Scholar]


