Abstract
Background
Chronic obstructive pulmonary disease (COPD) imposes a large public health burden internationally and in the United States. The objective of this study was to examine trends in mortality from COPD among US adults from 1968 to 2011.
Methods
Data from the National Vital Statistics System from 1968 to 2011 for adults aged ≥25 years were accessed, and trends in mortality rates were examined with Joinpoint analysis.
Results
Among all adults, age-adjusted mortality rose from 29.4 per 100,000 population in 1968 to 67.0 per 100,000 population in 1999 and then declined to 63.7 per 100,000 population in 2011 (annual percentage change [APC] 2000–2011: −0.2%, 95% confidence interval [CI]: −0.6, 0.2). The age-adjusted mortality among men peaked in 1999 and then declined (APC 1999–2011: −1.1%, 95% CI: −1.4, −0.7), whereas the age-adjusted mortality rate among women peaked in 2008 and subsequently increased slowly (APC 2000–2011: 0.4%, 95% CI: 0.0, 0.9). Despite a narrowing of the gender gap, mortality rates in men continued to exceed those in women. Evidence of a decline in the APC was noted for African American (1999–2011: −1.5%, 95% CI: −2.1, −1.0) and white men (1999–2011: −0.9%, 95% CI: −1.3, −0.6), adults aged 55–64 years (1989–2011: −1.0%, 95% CI: −1.2, −0.8), and adults aged 65–74 years (1999–2011: −1.2%, 95% CI: −1.6, −0.9).
Conclusions
In the United States, the mortality rate from COPD has declined since 1999 in men and some age groups but appears to be still rising in women, albeit at a reduced pace.
Introduction
Chronic obstructive pulmonary disease (COPD) is a major source of morbidity and mortality internationally.1,2 In 1997, COPD was predicted to become the third leading cause of global death by 2020,3 but a subsequent analysis found that COPD had become the third leading cause of global death by 2010.2 In the United States, deaths from chronic lower respiratory diseases, of which COPD comprises the bulk, rose to become the third leading cause of death in 2008.4 In international comparisons, the mortality rate from COPD in the United States ranks high;5 therefore, understanding trends in COPD mortality is of utmost importance in formulating appropriate public health initiatives to ease the burden of this disease.
A recent report showed that age-adjusted mortality rates from COPD declined substantially from 1994 to 2010 in the European Community and in most countries.6 In comparison, the age-adjusted mortality rate from COPD in the United States generally rose from 1970 to 2000 and then leveled off afterwards.7,8,9,10,11 To provide more detailed insights into the trend of the COPD mortality rate in the United States, the author examined national vital statistics data from 1968 to 2011 among adults aged ≥25 years.
Methods
Mortality data for adults aged 25 years or older were obtained from the Wide-ranging Online Data for Epidemiologic Research (WONDER) system developed and maintained by the Centers for Disease Control and Prevention.12 WONDER is an interactive web-based tool built with data from the National Vital Statistics System. Institutional Review Board approval was not required for this analysis of publically available data.
Deaths from COPD as the underlying cause of death were tabulated by using Eighth Revision of the International Classification of Diseases, Adapted for Use in the United States (ICDA-8) codes 490, 491, 492, and 519.3 (introduced in 1969) from 1968 to 1978, ICD-9 codes 490-492, 496 from 1979 to 1998, and ICD-10 codes J40-J44 from 1999 to 2011. Population estimates produced by the Bureau of the Census in collaboration with the National Center for Health Statistics provided the denominators needed to calculate rates for each year. Age-adjustment was done using the direct method to the projected year 2000 US population. Age-adjusted rates using the age-groups shown below were generated for all adults aged ≥25 years, men, women, whites, African Americans, other race, gender by race groups, and age-specific rates were generated for the age groups 25–34, 35–44, 45–54, 55–64, 65–74, 75–84, and ≥85 years.
Trends were analyzed using the Joinpoint (version 4.1.0) statistical program.13 This program identifies years when changes in the estimated annual percentage change (APC) in the mortality rate occurs by performing a Monte Carlo permutation test and proceeds to fit the simplest model with the fewest number of trend segments.14 The APC is calculated as APCi = [(Exp(bi) − 1)] × 100 where bi represents the slope of the period segment.15 As many as 5 trend segments were allowed, and mortality rates were log-transformed. Differences in the slopes for adjacent trend segments were tested with t-tests.
Results
Overall, the age-adjusted mortality rate from COPD rose steadily from 29.4 per 100,000 population in 1968 to 67.0 per 100,000 population in 1999 and then declined gradually to 63.7 per 100,000 population in 2011 (Figure 1). The APC was 3.0% (95% CI: 2.7, 3.4) from 1968 to 1987, 1.9% (95% CI: 1.4, 2.3) from 1987 to 2000, and −0.2% (95% CI: −0.6, 0.2) from 2000 to 2011 (Table 1). Thus, there was a deceleration in the age-adjusted mortality rate during successive periods. The slope for the two latter periods was significantly different from that of each preceding period. The mortality rate in 2011 (63.7 per 100,000 population) was 5.0% lower than in 1999 (67.0 per 100,000 population).
Figure 1.
Age-adjusted mortality rate from chronic obstructive pulmonary disease among US adults aged ≥25 years, United States 1968–2011
Table 1.
Annual percentage change (APC) of age-adjusted and age-specific mortality rates from chronic obstructive pulmonary disease among US adults aged ≥25 years, 1968 to 2011
| Period 1 | Period 2 | Period 3 | Period 4 | Period 5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Period | APC (%, 95% CI) | Period | APC (%, 95% CI) | Period | APC (%, 95% CI) | Period | APC (%, 95% CI) | Period | APC (%, 95% CI) | |
| Total | 1968–1987 | 3.0a (2.7, 3.4) | 1987–2000 | 1.9a (1.4, 2.3)b | 2000–2011 | −0.2 (−0.6, 0.2)b | — | — | — | — |
| Women | 1968–1988 | 7.1a (6.6, 7.5) | 1988–2000 | 3.7a (3.2, 4.3)b | 2000–2011 | 0.4a (0.0, 0.9)b | — | — | — | — |
| Men | 1968–1985 | 2.1a (1.8, 2.4) | 1985–1999 | 0.1 (−0.2, 0.5)b | 1999–2011 | −1.1a (−1.4, −0.7)b | — | — | — | — |
| African Americans | 1968–1982 | 2.7a (2.0, 3.4) | 1982–1985 | 8.5 (−2.9, 21.4) | 1985–1999 | 1.9a (1.4, 2.4) | 1999–2011 | −0.3 (−0.8, 0.1)b | — | — |
| Other | 1968–1978 | 2.2 (−0.2, 4.6) | 1978–1981 | −9.7 (−30.4, 17.1) | 1981–1984 | 12.8 (−9.4, 40.5) | 1984–1999 | 1.3a (0.6, 2.0) | 1999–2011 | −1.6a (−2.1, −1.0)b |
| White | 1968–1986 | 3.1a (2.7, 3.5) | 1986–2000 | 2.0a (1.6, 2.4)b | 2000–2011 | −0.1 (−0.5, 0.4)b | — | — | — | — |
| African American women | 1968–1989 | 6.8a (6.2, 7.4) | 1989–1999 | 4.3a (3.2, 5.4)b | 1999–2011 | 1.1a (0.5, 1.6)b | — | — | — | — |
| Other women | 1968–1999 | 3.4a (2.9, 4.0) | 1999–2011 | −0.6 (−1.4, 0.2)b | — | — | — | — | — | — |
| White women | 1968–1988 | 7.2a (6.7, 7.6) | 1988–2000 | 3.8a (3.3, 4.4)b | 2000–2011 | 0.6a (0.2, 1.0)b | — | — | — | — |
| African American men | 1968–1988 | 3.5a (3.1, 3.9) | 1988–1999 | 0.7 (0.0, 1.5)b | 1999–2011 | −1.5a (−2.1, −1.0)b | — | — | — | — |
| Other men | 1968–1999 | 1.3a (0.9, 1.7) | 1999–2011 | −2.2a (−3.0, −1.5)b | — | — | — | — | — | — |
| White men | 1968–1985 | 2.1a (1.7, 2.4) | 1985–1999 | 0.1 (−0.3, 0.4)b | 1999–2011 | −0.9a (−1.3, −0.6)b | — | — | — | — |
| Age groups (years) | ||||||||||
| 25–34 | 1968–1983 | −7.7a (−9.1, −6.3) | 1983–2011 | 1.0a (0.3, 1.6)b | — | — | — | — | — | — |
| 35–44 | 1968–1970 | 3.7 (−7.8, 16.6) | 1970–1983 | −6.6a (−7.4, −5.8) | 1983–1995 | −0.8 (−1.8, 0.2)b | 1995–2002 | 7.3a (5.1, 9.5)b | 2002–2011 | −1.6a (−2.6, −0.5)b |
| 45–54 | 1968–1998 | −1.5a (−1.7, −1.3) | 1998–2011 | 2.9a (2.4, 3.4)b | — | — | — | — | — | — |
| 55–64 | 1968–1981 | 0.1 (−0.4, 0.7) | 1981–1989 | 1.9a (0.7, 3.2)b | 1989–2011 | −1.0a (−1.2, −0.8)b | — | — | — | — |
| 65–74 | 1968–1985 | 2.5a (2.2, 2.8) | 1985–1999 | 1.2a (0.9, 1.6)b | 1999–2011 | −1.2a (−1.6, −0.9)b | — | — | — | — |
| 75–84 | 1968–1986 | 4.3a (4.0, 4.7) | 1986–1999 | 2.2a (1.8, 2.6)b | 1999–2011 | −0.1 (−0.4, 0.3)b | — | — | — | — |
| ≥85 | 1968–1985 | 5.8a (5.0, 6.6) | 1985–2001 | 4.1a (3.7, 4.6)b | 2001–2011 | 0.6a (0.1, 1.1)b | — | — | — | — |
P-value for APC <0.05.
Slope is significantly different from slope of preceding trend segment.
Among men, the mortality rate from 1968 (56.4 per 100,000 population) to its peak in 1999 (88.2 per 100,000 population) increased by about 60% and then decreased by 16.6% by 2011 (73.5 per 100,000 population). The APC increased by 2.1% per years (95% CI: 1.8, 2.4) from 1968 to 1985, changed little from 1985 to 1999 (0.1%, 95% CI: −0.2, 0.5), and decreased by −1.1% per years (95% CI: −1.4, −0.7) from 1999 to 2011 (Table 1). Among women, the age-adjusted mortality rate from 1968 (9.4 per 100,000 population) to its peak in 2008 (59.1 per 100,000 population) increased by 530%. The APC decreased progressively in three successive periods: 7.1% (95% CI: 6.6, 7.5) from 1968 to 1988, 3.7% (95% CI: 3.2, 4.3) from 1988 to 2000, and 0.4% (95% CI: 0.0, 0.9) from 2000 to 2011 (Table 1). Nevertheless, the APC in the latter period was positive and significant indicating that rates may still be rising among women. Rates in 1968 were approximately 6-fold higher in men than women, but the gap between men and women narrowed substantially so that by 2008 the rate in men was only 1.3 times higher in men than women. The gender difference in rates reached a maximum of 54.4 per 100,000 population in 1976 and declined to 16.2 per 100,000 population in 2011.
The age-adjusted rates for African Americans, whites, and adults of a race other than African American and white peaked in 1999 and were from 3.1% to 19.2% lower in 2011 (Figure 2). Only among adults of a race other than African American or white did the APC decrease significantly from 1999–2011 (Table 1). The ratio of rates in whites to African Americans ranged between 1.5 and 1.8 and did not vary greatly during the study period, but the absolute difference in age-adjusted rates increased from 12.8 per 100,000 population in 1970 to 27.3 per 100,000 population in 2008.
Figure 2.
Age-adjusted mortality rate from chronic obstructive pulmonary disease among US adults aged ≥25 years, by race, United States 1968–2011
The age-adjusted mortality rates among white and African American men peaked in 1999 and the rate of men of a race other than African American and white peaked in 2000. The mortality rates among white and African American women peaked in 2008, and the rate of women of a race other than African American and white peaked in 1999. The age-adjusted rates in white adults were substantially higher than those in African American adults and adults of a race other than African American and white (Figure 3). From 1999 to 2011, significant decreases in the APC were present among African American men, white men, and men of races other than white and African American (Table 1). In contrast, significant increases in the APC were noted among African American and white women. Among women, the white/African American ratio fluctuated between 1.7 and 2.3 with no clear trend. In contrast, the white/African American ratio among men tended to decrease from 1.8 in 1968 to about 1.2–1.3 in 1988 and beyond. The absolute difference between white and African American women increased from 4.4 per 100,000 population in 1968 to 31.1 per 100,000 population in 2003, remaining high in subsequent years. In contrast, the absolute difference in rates between white and African American men narrowed from a high of 31.4 per 100,000 population in 1975 to 15.6 per 100,000 population in 2005.
Figure 3.
Age-adjusted mortality rate from chronic obstructive pulmonary disease among US adults aged ≥25 years, by race and gender, United States 1968–2011
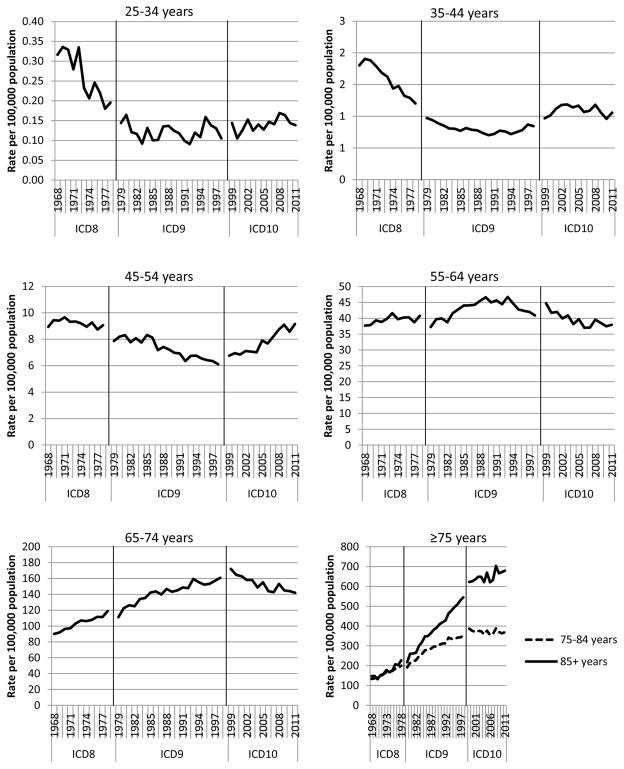
The age-specific rates showed a powerful gradient: the rate among adults aged ≥85 years was as much as approximately 6000-fold higher than adults aged 25–34 years and as much as 700-fold higher than adults aged 35–44 years (Figure 4, 5). The age-specific rates among adults aged 25–34 years, 35–44 years, 45–54 years, and 55–64 years were at their peaks in 1969, 1969, 1971, and 1989, respectively, and at their lows during 1992, 1990, 1998, and 2006, respectively. In the three youngest age groups, rates in 2011 were approximately 50% higher than the ones at their nadir. In the older age groups, the pattern was reversed: the lowest rates among adults aged 65–74 years, 75–84 years, and ≥85 years occurred during 1968, 1968, and 1970, respectively, whereas the highest rates occurred during 1999, 2008, and 2008, respectively. The APC decreased significantly among adults aged 35–44 years since 2002, 55–64 years since 1989, and 65–74 years since 1999, but increased among those aged 25–34 years since 1983 and 45–54 years since 1998, and ≥85 years since 2001 (Table 1).
Figure 4.
Age-specific mortality rate from chronic obstructive pulmonary disease among US adults aged ≥25 years, United States 1968–2011
Figure 5.
Age-specific mortality rate from chronic obstructive pulmonary disease among US adults aged ≥25 years graphed on a log-scale, United States 1968–2011
Discussion
The findings from this study document changes in the mortality rate from COPD among US adults aged ≥25 years over a 44-year period and illustrate several points. First, rates are no longer rising in all adults. Since 1999, the APC has decreased significantly in men but is still rising, albeit at a much slower rate, in women. Two, rates in men continue to exceed those in women, but there has been a substantial narrowing of the gender gap. Third, rates in whites are greater than those in African Americans, and the difference in absolute rates between the two groups has widened driven by the divergence in rates among white and African American women. Fourth, the patterns of the trends differed markedly among the age groups.
Several recent publications have described changes in mortality from COPD in Europe, Australia, and Japan.5,6,16 In the European Union, the age-adjusted rates of mortality from COPD among adults aged ≥40 years from 1994 to 2010 declined continuously in men with relatively stable rates in women.6 However, the rate aggregated over 27 countries masked considerable variation among countries. The pattern in the United States was similar to that in Sweden where the rate in men peaked around 2000 before declining, and the rate in women continued to increase but at a slower pace during the tail end of the study period. In Australia, the age-adjusted rate in men aged ≥55 years increased sharply from 1965 to 1970 and thereafter started a continuous decline that was particularly steep from 1988 to 2006.5 In women, however, the age-adjusted rate increased from 1965 to 1997 before starting a moderate decline. In Japan, the age-adjusted rate of mortality from COPD in adults aged ≥40 years decreased from 71.3 per 100,000 population in 1950 to 19.7 per 100,000 population in 2004 in men and from 41.7 to 4.3 per 100,000 population in women.16
The current analysis shows that the mortality rate among men continues to exceed that in women. A previous analysis of mortality data from 1968 to 1999 in the United States reported a narrowing of the gender gap in mortality rates.8 The current analysis shows a further narrowing of this gap through 2011. National data show interesting gender differences in COPD statistics. Men have higher mortality rates and a higher prevalence of obstructive lung function than women, yet women are more likely to report having COPD in surveys.7,11,17,18
Despite substantial declines in the prevalence of smoking in the United States since 1965,19 mortality from COPD has remained intractably high reflecting the lingering burden of tobacco use from decades past and the long lag period between tobacco use and its effect on mortality. The declining rate in men since 1999 is a welcome development, and given the continuing decline in tobacco use, further declines in the mortality rate in men can be anticipated. There is also a suggestion in the data that the increase in COPD mortality in women may be leveling off, but additional data are required to bear this contention out. Furthermore, the age-specific rates in adults younger than 65 years suggest that future declines in the rate of COPD mortality are likely. However, it should be noted that the year when the rates reached a minimum generally occurred during the 1990s (2006 for adults aged 55–64 years), and the rates among adults aged 25–34 years and 45–54 years have increased significantly since reaching their nadirs. Thus, the mortality rate in these age cohorts should continue to be carefully monitored. Reasons for these apparent increases are unclear as the prevalence of current smokers has been declining in all age groups as well as in the 1960 and 1980 birth cohorts although the downturn for the latter cohort started only about a decade ago.20
Because tobacco use is the single biggest contributor to the development of COPD,20 continued public health efforts to prevent the initiation of tobacco use and smoking cessation among those who continue to smoke are needed to further lower the prevalence of tobacco use. Although the prevalence of cigarette smoking among US adults was 19.0% in 2011, considerable interstate variation in the prevalence in 2012 existed with a range of 10.6% to 28.6%.21 These estimates suggest that substantial advances in reducing the prevalence of current smoking are feasible.
Several limitations of the present analysis merit consideration. First, the validity of COPD codes on death certificates is unknown. A few studies in the United States suggest that death from COPD is underreported on death certificates.22,23 Second, the study period covered several ICD transitions raising the prospect of abrupt artificial changes in mortality rates. The comparability ratio for ICD codes 490-491 in ICD8 and ICD9 was 0.9383, whereas the comparability ratio for code 492 was 0.9770.24 The comparability ratio for the category chronic lower respiratory disease for the transition from ICD9 to ICD10 was 1.0478.25 Third, this study, like many other mortality studies, examined only COPD as the underlying cause of death. Studies using multiple cause of death provide a fuller picture of the burden associated with COPD. Fourth, separating out persons of Hispanic heritage was not possible for the entire study period.
In conclusion, the age-adjusted mortality rate from COPD peaked in 1999 and has decreased nonsignificantly since then reflecting a significant decline in men and a significant increase among women. Men continue to die at higher rates than women although the gap has narrowed, and whites die at higher rates than African Americans with a widening mortality gap. Although it continues to be asserted that mortality from COPD has been rising, the findings from the present study make clear that the mortality rate from COPD among US adults has stopped rising and has even started to decline in some demographic groups.
Abbreviations
- APC
annual percentage change
- COPD
chronic obstructive pulmonary disease
- ICD
International Classification of Diseases
- WONDER
Wide-ranging Online Data for Epidemiologic Research
Footnotes
Work was performed at the Centers for Disease Control and Prevention
Conflict of interest: None
Earl S. Ford: None
Author contributions: Dr Ford had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the analysis.
Dr Ford: responsible for the study concept and design, acquisition of data, analysis and interpretation of data, and manuscript preparation.
Financial/nonfinancial disclosures: Dr Ford has reported to CHEST that no potential conflicts of interest exist.
Disclaimer: The findings and conclusions in this article are those of the author and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Role of Sponsors: None
Funding: None
Funding/Support: None
References
- 1.World Health Organization. Global surveillance, prevention and control of chronic respiratory diseases. Geneva, Switzerland: World Health Organization; 2007. [Google Scholar]
- 2.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet. 1997;349(9064):1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 4.Miniño AM, Murphy SL, Xu J, Kochanek KD. Deaths: Final Data for 2008. National Vital Statistics Reports. 2011;59(10):1–157. [PubMed] [Google Scholar]
- 5.Australian Institute of Health and Welfare. Poulos LM, Cooper SJ, Ampon R, Reddel HK, Marks GB. [Accessed August 21, 2014];Mortality from asthma and COPD in Australia. http://apo.org.au/files/Resource/aihw_mortalityfromasthmaandcopdinaustralia_aug_2014.pdf.
- 6.Lopez-Campos JL, Ruiz-Ramos M, Soriano JB. Mortality trends in chronic obstructive pulmonary disease in Europe, 1994–2010: a joinpoint regression analysis. Lancet Respir Med. 2014;2(1):54–62. doi: 10.1016/S2213-2600(13)70232-7. [DOI] [PubMed] [Google Scholar]
- 7.Mannino DM, Homa DM, Akinbami LJ, Ford ES, Redd SC. Chronic obstructive pulmonary disease surveillance--United States, 1971–2000. MMWR Surveill Summ. 2002;51(6):1–16. [PubMed] [Google Scholar]
- 8.Kazerouni N, Alverson CJ, Redd SC, Mott JA, Mannino DM. Sex differences in COPD and lung cancer mortality trends--United States, 1968–1999. J Womens Health (Larchmt) 2004;13(1):17–23. doi: 10.1089/154099904322836410. [DOI] [PubMed] [Google Scholar]
- 9.Jemal A, Ward E, Hao Y, Thun M. Trends in the leading causes of death in the United States, 1970–2002. JAMA. 2005;294(10):1255–1259. doi: 10.1001/jama.294.10.1255. [DOI] [PubMed] [Google Scholar]
- 10.Akinbami LJ, Liu X. Chronic obstructive pulmonary disease among adults aged 18 and over in the United States, 1998–2009. NCHS Data Brief. 2011;(63):1–8. [PubMed] [Google Scholar]
- 11.Ford ES, Croft JB, Mannino DM, Wheaton AG, Zhang X, Giles WH. COPD surveillance--United States, 1999–2011. Chest. 2013;144(1):284–305. doi: 10.1378/chest.13-0809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. [Accessed August 15, 2014];CDC wonder: Compressed Mortality File. http://wonder.cdc.gov/mortSQL.html.
- 13.National Cancer Institute. Statistical Methodology and Applications Branch, Surveillance Research Program. [Accessed August 21, 2014];Joinpoint Regression Program. http://surveillance.cancer.gov/joinpoint/
- 14.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 15.National Cancer Institute. [Accessed October 8, 2014];Average Annual Percent Change (AAPC) http://surveillance.cancer.gov/joinpoint/aapc.html.
- 16.Pham TM, Ozasa K, Kubo T, et al. Age-period-cohort analysis of chronic obstructive pulmonary disease mortality in Japan, 1950–2004. J Epidemiol. 2012;22(4):302–307. doi: 10.2188/jea.JE20110092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ford ES, Mannino DM, Wheaton AG, Giles WH, Presley-Cantrell L, Croft JB. Trends in the Prevalence of Obstructive and Restrictive Lung Function among Adults in the United States: Findings from the National Health and Nutrition Examination Survey from 1988–1994 to 2007–2010. Chest. 2013;143(5):1395–1406. doi: 10.1378/chest.12-1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Chronic obstructive pulmonary disease among adults--United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(46):938–943. [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. [Accessed May 3, 2012];Trends in Current Cigarette Smoking Among High School Students and Adults, United States, 1965–2007. http://www.cdc.gov/tobacco/data_statistics/tables/trends/cig_smoking/index.htm.
- 20.U.S. Department of Health and Human Services. The Health Consequences of Smoking--50 Years of Progress. A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Serices, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 21.Centers for Disease Control and Prevention. [Accessed August 20, 2014];Prevalence and Trends Data. http://apps.nccd.cdc.gov/brfss/
- 22.Mitchell RS, Walker SH, Silvers GW, Dart G, Maisel JC. The causes of death in chronic airway obstruction. I. The unreliability of death certificates and routine autopsies. Am Rev Respir Dis. 1968;98(4):601–610. doi: 10.1164/arrd.1968.98.4.601. [DOI] [PubMed] [Google Scholar]
- 23.Camilli AE, Robbins DR, Lebowitz MD. Death certificate reporting of confirmed airways obstructive disease. Am J Epidemiol. 1991;133(8):795–800. doi: 10.1093/oxfordjournals.aje.a115958. [DOI] [PubMed] [Google Scholar]
- 24.U.S. Department of Health Education and Welfare, Public Health Service, Office of Health Research Statistics and Technology, National Center for Health Statistics. Estimates of Selected Comparability Ratios Based on Dual Coding of 1976 Death Certificates by the Eighth and Ninth Revisions of the International Classification of Diseases. Monthly Vital Statistics Report. 1980;28(11) Supplement:1–19. [Google Scholar]
- 25.Anderson RN, Miniño AM, Hoyert DL, Rosenberg HM. Comparability of Cause of Death Between ICD–9 and ICD–10-Preliminary Estimates. National Vital Statistics Reports. 2001;49(2):1–32. [PubMed] [Google Scholar]