Abstract
Increases in marijuana use in recent years highlight the importance of understanding how marijuana affects mental health. Of particular relevance is the effect of marijuana use on anxiety and depression given that marijuana use is highest among late adolescents/early adults, the same age range in which risk for anxiety and depression is the highest. Here we examine how marijuana use moderates the effects of temperament on level of anxiety and depression in a prospective design in which baseline marijuana use and temperament predict anxiety and depression one year later. We found that harm avoidance (HA) is associated with higher anxiety and depression a year later, but only among those low in marijuana use. Those higher in marijuana use show no relation between HA and symptoms of anxiety and depression. Marijuana use also moderated the effect of novelty seeking (NS), with symptoms of anxiety and depression increasing with NS only among those with high marijuana use. NS was unrelated to symptoms of anxiety and depression among those low in marijuana use. The temperament dimension of reward dependence was unrelated to anxiety and depression symptoms. Our results suggest that marijuana use does not have an invariant relationship with anxiety and depression, and that the effects of relatively stable temperament dimensions can be moderated by other contextual factors.
Keywords: Marijuana, Harm Avoidance, Novelty Seeking, Reward Dependence, Anxiety, Depression
Marijuana is the third most commonly used drug in the U.S. (after alcohol and tobacco), and the leading illicit drug in states where its recreational use is currently illegal (Gallup, 2013; National Institute of Drug Abuse [NIDA], 2014). It is estimated that more than a third of the American population has used marijuana and that roughly 7% of Americans currently are regular users (Gallup, 2013). The perception that marijuana is dangerous has been decreasing since 2007, corresponding with increasing use among young people (NIDA, 2014) and increasing legalization for recreational and medical purposes (Colorado Amendment 64, 2012; Washington Initiative 502, 2012).
In the face of such high levels of use and rapid changes to laws and perceptions, it is critically important to better understand the consequences of marijuana use. One issue in particular need of further exploration is the relation of marijuana use to mental health. Anxiety and depression are the most common mental health conditions in the U.S. (National Institute of Mental Health [NIMH], 2014a; NIMH, 2014b), making understanding the factors that affect them of particular clinical significance. Adding to the clinical relevance, the risk of developing anxiety and depression is highest within the same age range in which marijuana use is the highest. That is, 75% of all lifetime cases of anxiety and depression start by age 24 (Kessler et al., 2005) and among adolescents, roughly 32% have had lifetime prevalence of anxiety disorders and roughly 14% have had lifetime prevalence of mood disorders (Merikangas et al., 2010). At the same time, marijuana use is typically the highest in the teens through early twenties as compared to all other age ranges (Degenhardt et al., 2008; Kessler et al., 2005), and about 52% of 18–25 year olds have used marijuana in their lifetime (NIDA, 2014).
Here we take the approach that understanding anxiety and depression within this population at heightened risk can be improved by examining whether behaviors that are frequent within this same age range relate to symptoms of anxiety and depression. That is, given the relatively high rate of marijuana use within late adolescence/early adulthood and the possibility that it may increase in the face of increasing legalization, there is public health relevance in knowing the relation of marijuana use to the risk of anxiety and depression within this age range. This can improve our understanding of whether increases in marijuana legalization might affect rates of anxiety and depression, and whether anxiety and depression prevention and treatment strategies could benefit by targeting marijuana use.
There is relatively little relevant co-morbidity data speaking to the relation between marijuana and anxiety/depression as most large epidemiological studies collapse marijuana use into a broader substance use disorder category (for review, see Degenhardt, Hall, & Lynskey, 2003). Those studies that do separately examine marijuana use focus only on marijuana dependence and/or examine a wide age range (Chen, Wagner, & Anthony, 2002; Degenhardt, Hall, & Lynskey, 2001). Results from studies that have focused on recreational users and/or young adults are quite variable; some show a negative association between marijuana use and anxiety/depression (e.g., Denson & Earleywine, 2006; Sethi et al., 1986; Stewart et al., 1997), others a positive association (e.g., Bonn-Miller et al., 2005; Hayatbakhsh et al., 2007; Scholes-Balog et al., 2013), and still others no association (e.g., Green & Ritter, 2000; Musty & Kaback, 1995). Such a diverse pattern of results suggests that other factors may also interact with marijuana use to affect anxiety and depression. Unfortunately, there has been a great deal of diversity in the extant research along multiple dimensions (e.g., community vs. college samples, samples unselected vs. selected for marijuana use, different types of marijuana, anxiety, and depression measures), making it difficult to identify variables that explain the different patterns of associations obtained. Here we begin the process of identifying factors that affect the relation between marijuana use and anxiety and depression by examining a variable that is itself known to relate to anxiety and depression. We specifically examine relatively stable aspects of temperament whose relation to anxiety and depression have been frequently studied and ask whether marijuana use interacts with temperament in its relationship with anxiety and depression.
Temperament, Anxiety, and Depression
According to the biosocial model (Cloninger, Svrakic, & Przybeck, 1993), temperament affects mental health via genetically determined biases that influence automatic responses to novelty, punishment, and reward. The temperament dimension of harm avoidance (HA) is particularly relevant for understanding anxiety and depression as it is characterized by heightened apprehension, shyness, pessimism, and inhibition of behaviors. Given these biases, it is not surprising that HA is positively associated with both anxiety and depression (Hansenne et al., 1998; Jiang et al., 2003; Matsudaira et al., 2006; Manfredi et al., 2011).
While HA likely increases anxiety and depression, marijuana can have anxiolytic and euphoriant effects. Such positive mood effects are reported among the top motives for marijuana use (Lee et al., 2009; Newcomb et al., 1998; Simons et al., 1998). Marijuana use may also facilitate social contact (Green & Ritter, 2000) which could, in turn, improve mood and ultimately mental health. Animal research suggests a direct anxiolytic effect of cannabis administration (e.g., Guimaraes et al., 1990; Soares et al., 2010; for a review, see Mechoulam, Parker, & Gallily, 2002). The exact mechanism of these effects has not been determined, although they seem to be restricted to the effects of cannabidiol and not Δ9-tetrahydrocannabinol (e.g., Zuardi et al., 2006) and likely involve serotonergic receptors in the dorsal periaqueductal gray matter as the basis for anxiolytic effects (Soares et al., 2010). The potential for marijuana use to affect mood suggests a possible moderating role of marijuana on the relation of HA to anxiety and depression. Specifically, to the degree that marijuana produces anxiolytic and/or euphoriant effects – either directly through its biochemical effects on neurotransmitters and receptors or indirectly through expectations and/or the facilitation of mood and beneficial social interactions – marijuana use may buffer individuals high in HA from increased risk for anxiety and depression.
The other major temperament dimensions in the biosocial model have shown no consistent associations with anxiety or depression. Novelty seeking (NS) is thought to bias individuals toward impulsivity and exploration in response to novelty; reward dependence (RD) reflects a tendency to maintain previously rewarded behaviors. While these dimensions have been associated with anxiety and depression in some samples (with occasional negative associations of NS and RD with depression, Farmer et al., 2003; Hansenne et al., 1998), they most often show no association with anxiety and depression (Copeland et al., 2004; Starcevic et al., 1996; Strakowski et al., 1995; Young et al., 1995). Given the behavioral biases linked with the temperament dimensions, the lack of associations with anxiety and depression are theoretically sensible (i.e., the biases associated with these temperament dimensions would not seem to increase risk for anxiety and depression). At the same time, these relations have most often been examined in studies with relatively small samples (fewer than 100 participants), making small effects difficult to detect. More importantly for the present analyses, the moderating effect of marijuana use has never to our knowledge been tested.
Current Study
The present study seeks to better understand how marijuana use relates to anxiety and depression within late adolescents/early adults by examining how it might moderate the effects of temperament on symptoms of anxiety and depression. We also examine, in a larger sample than past studies, the relation of temperament to anxiety and depression. We did this in a prospective design in which marijuana use and temperament assessed at baseline were used to predict anxiety and depression symptoms assessed one year later in a relatively large (n = 338) sample of 18 – 21 year old male and female college students. Roughly equal numbers of men and women allow us to test whether relations among temperament, marijuana use, and anxiety/depression differ for men and women.
Hypotheses
Given past research and the nature of the behavioral biases associated with HA, we predict that baseline HA will positively predict both anxiety and depression symptoms assessed one year later. However, given potential anxiolytic and euphoriant effects, we expect marijuana to moderate this relationship, such that the positive association of HA with anxiety and depression symptoms will be most evident when marijuana use is low. Marijuana may itself show a simple relation to anxiety and depression, with fewer symptoms of anxiety and depression among those who use marijuana more frequently. We assess these relations while also controlling for baseline anxiety and depression. If HA and its interaction with marijuana use have effects independent of current anxiety and depression, we expect these relations to be evident even after controlling for baseline levels of psychopathology.
Given the lack of consistent relations of NS and RD with anxiety and depression, we had no specific predictions for these analyses but we nevertheless tested them to provide a comprehensive assessment of the relations among temperament dimensions, marijuana use, and risk for anxiety and depression. We have no a priori expectations that these relations will differ for men and women, but given gender differences in rates of anxiety and depression (Kessler, McGonagle, Swartz, Blazer, & Nelson, 1993; McLean, Asnaani, Litz, & Hofmann, 2011), it is important to assess whether factors that relate to anxiety and depression differ for men and women.
Method
Participants
Potential participants were recruited via email invitations to their university account and advertisements on campus to take part in a three-year longitudinal study of marijuana use. Those who were interested in the study were initially interviewed on the phone by study personnel to determine whether their marijuana use fit into one of three categories: never users (i.e., never tried marijuana), relatively infrequent marijuana users (i.e., used marijuana four times or less per month for less than three years), and regular frequent marijuana users (i.e., used marijuana an average of five days a week or more for at least the past year). Both quantity and frequency criteria were implemented to ensure that variability in marijuana use reflected relatively stable tendencies. Because the full protocol also included electroencephalography measures, individuals who reported a history of head trauma, neurological disorder, or the use of prescription medication (with the exception of oral contraceptives or medical marijuana) were excluded from the study. One of the interests in the larger study was on change in marijuana use over time, so we oversampled participants with lower levels of use, whom we expected to be more likely to change their use over time. We continued sampling within each use category until we had roughly equal numbers of men and women. Participants who met criteria for inclusion were invited to participate in two sessions a year for three total years. Data in the present analyses come from the first sessions in years 1 and 2.
Our final sample consisted of 375 University of Colorado primarily freshman (see Table 1 for sample characteristics). Of the 337 participants who provided racial information, 1 identified as Black, 12 as Asian, 11 as Hispanic, 1 as Pacific Islander, 2 as East Indian, 1 as Middle Eastern, 63 as multi-racial, and 246 as White. Four additional participants were initially enrolled but later found to have provided inaccurate information at the time of recruitment and so were dropped from the study. Thirty-seven individuals did not return to complete Year 2, so analyses are based on the 338 with complete data. Those who failed to return in Year 2 did not differ from those who did in gender, age, race, marijuana use group, temperament, or psychopathology (all p’s > .13). Only the measures of interest to our current hypotheses will be described in detail, but where appropriate (e.g., when they preceded the measures of interest), other measures collected will be noted.
Table 1.
Sample Characteristics by Marijuana Use Group
| Never | Infrequent | Frequent | F or χ2 Value | |
|---|---|---|---|---|
| Demographics | ||||
| N (Year 1/Year 2) | 126/114 | 146/133 | 103/91 | |
| Gender (% female) | 57 (50%) | 72 (54.1%) | 47 (51.6%) | 0.43 |
| Age | 18.30 (0.46) | 18.38 (0.52) | 18.34 (0.50) | 0.76 |
| Ethnicity (% White) | 81 (71.1%) | 93 (69.9%) | 72 (80%) | 3.10 |
|
| ||||
| Substance Use Year 1 | ||||
| Total Days of Marijuana Use (0–30) | 0.00a | 1.65 (1.88)b | 26.07 (3.52)c | 4475.48*** |
| Total Grams of Marijuana Use | 0.00a | 0.87 (1.43)a | 24.45 (16.57)b | 256.76*** |
| Avg Grams per Use Day | 0.00a | 0.32 (0.44)b | 0.92 (0.56)c | 134.33*** |
|
| ||||
| Temperament Year 1 | ||||
| Harm Avoidance | 2.49 (0.66) | 2.58 (0.64) | 2.52 (0.51) | 0.67 |
| Novelty Seeking | 2.91 (0.42)a | 3.08 (0.37)b | 3.38 (0.40)c | 36.59*** |
| Reward Dependence | 3.55 (0.58) | 3.57 (0.53) | 3.58 (0.46) | 0.10 |
|
| ||||
| Psychopathology Year 1 | ||||
| Anxiety Symptoms | 4.40 (2.60) | 4.67 (3.39) | 4.91 (3.08) | 0.71 |
| Anxiety % at risk | 4.39 a | 15.04 b | 13.19 b | 7.79* |
| Depression Symptoms | 3.64 (2.67)a | 4.73 (3.90)b | 5.29 (4.00)b | 5.81** |
| Depression % at risk | 0.88 a | 8.27 b | 14.29 b | 13.53*** |
|
| ||||
| Psychopathology Year 2 | ||||
| Anxiety Symptoms | 3.90 (2.79) | 4.66 (3.45) | 4.40 (2.86) | 1.88 |
| Anxiety % subclinical or greater | 7.02 | 11.28 | 6.59 | 2.05 |
| Depression Symptoms | 3.80 (3.28)a | 4.99 (4.28)b | 4.84 (4.00)ab | 3.23* |
| Depression % subclinical or greater | 5.26 | 12.03 | 10.99 | 3.62 |
Note. Gender shows number of females. Ethnicity shows number of Whites. Numbers in parentheses are standard deviations. Possible ranges are 1–5 for Harm Avoidance, Novelty Seeking, and Reward Dependence, 0–14 for ASR Anxiety Symptoms, and 0–24 for ASR Depression Symptoms. Higher values indicate greater marijuana use, HA, NS, RD, anxiety, and depression. Anxiety and Depression Symptoms reflect total number of symptoms endorsed. % at risk shows percentage of participants who scored at or above the ASR “at-risk” threshold for clinical levels of anxiety or depression (T score >=65). F and χ2 values reflect the test of the omnibus Marijuana Use Group main effect (df = 2, 335 and 2, respectively). χ2 = 2. Marijuana Use Group means within the same row with different subscripts differ at p < .05. For omnibus Marijuana Use Group effects,
p ≤ .05,
p ≤ .01,
p ≤ .001
Self-Report Measures
Temperament and Character Inventory (TCI) (Year 1 and Year 2)
HA, NS, and RD were measured with the TCI (Cloninger et al., 1993). HA was assessed with 33 items that assess anticipatory worry, fear of uncertainty, shyness with strangers, and fatigability (e.g., “Usually I am more worried than most people that something might go wrong in the future,” “I usually feel tense and worried when I have to do something new and unfamiliar,” “When I meet a group of strangers, I am more shy than most people,” “I have less energy and get tired more quickly than most people,”) (α = .93). NS was assessed with 35 items that assess exploratory excitability, impulsivity, extravagance, and disorderliness (e.g., “When nothing new is happening, I usually start looking for something that is thrilling or exciting,” “I often do things based on how I feel at the moment without thinking about how they were done in the past,” “I often spend money until I run out of cash or get into debt from using too much credit,” “I like when people can do whatever they want without strict rules and regulations,”) (α = .85). RD was assessed with 30 items that assess sentimentality, openness to warm communication versus aloofness, attachment, and dependence (e.g., “I am strongly moved by sentimental appeals [like when asked to help crippled children],” “I like other people to know that I really care about them,” “I like to discuss my experiences and feelings openly with friends instead of keeping them to myself,” “I don’t care very much whether other people like me or the way I do things,” [reverse-coded]) (α = .88).
All items were answered with respect to how the participants usually or generally act and feel using a 5-point scale (1=definitely false to 5=definitely true). Separate mean scores were created for overall HA, NS, and RD, with higher scores reflecting greater HA, NS, and RD. The biosocial model currently includes a fourth temperament dimension of Persistence (P) that was previously included as part of RD (Cloninger et al. 1993). P is associated with determination and industriousness. It has been much less frequently measured in association with anxiety and depression, and when it has been, shows inconsistent relations (Cloninger et al., 2006; Hansenne et al., 1999). Measures of P were omitted from the present study out of space considerations.
Marijuana use (Year 1)
Self-reported marijuana use during the past 30 days was assessed using the Time-Line Follow Back (TLFB; Sobell & Sobell, 1992), a calendar-assisted structured interview in which participants were asked to indicate over the past 30 days the quantity of marijuana used on each day. Frequency and quantity reports were highly correlated (r =0.82, p < .0001). Relative to other substances such as alcohol and nicotine, where individuals might consume an entire beer or cigarette, marijuana users might just take a few hits. There are also many different ways to consume marijuana (joints, vaporizers, edibles). Because of this potential for variability, our main analyses used marijuana use frequency as our measure of marijuana use. However, secondary analyses were also conducted with marijuana quantity measures and yielded identical results (see Supplement Tables S1, S2, and S3).
Adult Self-report (ASR) (Year 1 and Year 2)
Symptoms of anxiety and depression were measured with the Achenbach System of Empirically Based Assessment Adult Self-report (Achenbach & Rescorla, 2003), a self-report measure of current internalizing and externalizing psychopathology that is the adult parallel to the Child Behavior Checklist. These internalizing and externalizing scales on the ASR have been well validated and have adequate psychometric characteristics (Achenbach & Rescorla, 2003). Of interest were anxiety problems and depressive problems. Participants were asked how well each item described them over the past six months, with responses ranging from 0 = not true, 1 = somewhat or sometimes true, and 2 = very true or often true. Anxiety problems were assessed with 7 items (e.g., “I am nervous or tense,” Year 1: α = .76; Year 2: α = .77). Depressive problems were assessed with 14 items (e.g., “I am unhappy, sad, or depressed,” Year 1: α = .77; Year 2: α = .80). A total score was created for each construct with higher scores reflecting a continuous measure of greater endorsement of anxiety and depressive problems. Because of the conceptual similarity between HA and anxiety and depression, we conducted factor analyses to confirm that HA was distinct from anxiety and depression (see Supplement).
Procedure
Participants who met criteria for inclusion were invited to participate in a total of six laboratory sessions over three years. Data in the present analyses come from the first sessions in Years 1 and 2 at which marijuana use, temperament, and psychopathology were assessed. The assessments occurred approximately 12 months apart (M = 356.98 days, SD = 19.78 days).
Participants were instructed to abstain from alcohol for 24 hours, recreational drugs (including marijuana) for 6 hours, and caffeine and cigarettes for 1 hour prior to each laboratory session. In both sessions, participants were breathalyzed to ensure a breath alcohol concentration of zero. Adherence to other abstinence requirements was verified verbally. Although it would have been preferable to assess abstinence biochemically, it was prohibitively expensive. While failure to meet the requirements could add variability to the responses, none of the participants were visibly impaired and we have no reason to think failure to conform to the abstinence requirements introduced any systematic artifact (i.e., failure to meet the abstinence requirement seems unlikely to have created the pattern of relationships among the variables that we observed). Participants next completed the TLFB followed by a questionnaire including demographics, the ASR, and the TCI. Prior to the ASR, participants completed measures of handedness, ADHD symptoms (Barkley & Murphy, 1998), the Beck Depression Index (Beck, Steer, & Garbin, 1988) and the Beck Anxiety Index (Beck, Epstein, Brown, & Steer, 1988). Prior to completing the TCI, participants completed the Shortened Self-Regulation Questionnaire (Carey, Neal, & Collins, 2004). Participants received $25 at each session.
Analysis Strategy
We first performed preliminary descriptive analyses to assess the relation between marijuana use, temperament, and anxiety and depression symptoms, with separate analyses representing marijuana use either categorically or continuously. Categorical analyses were done with one-way analyses of variance (ANOVAs) using a 3-level Marijuana Use Group variable based on the participant’s use at time of study enrollment (i.e., never, infrequent, frequent). Continuous analyses consisted of bivariate correlations between number of days marijuana was used in past 30 days from the baseline Year 1 TLFB and temperament and psychopathology variables.
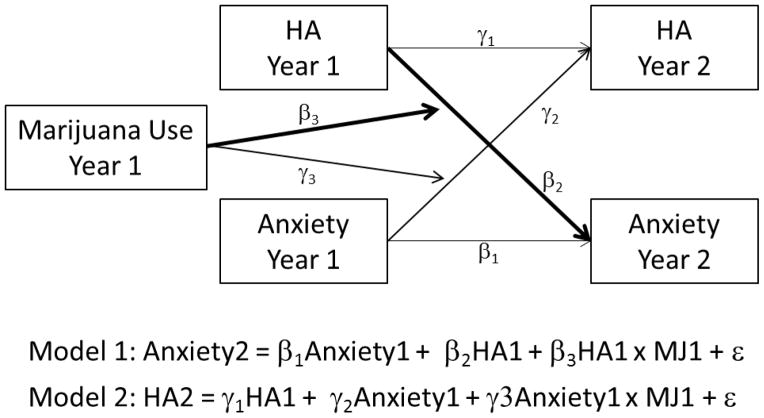
Our primary analyses assessed whether Year 1 HA, NS, and RD predict Year 2 anxiety and depression symptoms, and whether this relationship is moderated by marijuana use. This was tested using a cross-lag structural regression approach (Rogosa, 1980). Under this approach, two multiple regression equations are used to test the relations shown in Figure 1, illustrated using HA and anxiety symptoms as an example. Model 1 tests our hypothesized relations that Year 2 anxiety is predicted by Year 1 HA, and that the relation between HA and anxiety is moderated by marijuana use. More specifically, β1 assesses the autoregressive or lagged effect of Year 1 anxiety predicting Year 2 anxiety. Because we assume that initial anxiety and depression symptoms will be a strong predictor of subsequent anxiety and depression, including this lagged effect provides a strong test of the degree to which temperament and marijuana use predict anxiety and depression over and above baseline anxiety and depression. Of primary theoretical interest are β2 and β3. β2 tests the effects of Year 1 HA on Year 2 anxiety, reflecting a simple crossed effect, whereas β3 assesses whether the simple crossed effect of HA on Year 2 anxiety is moderated by Year 1 marijuana use. As described by Baron and Kenny (1986), this predicted moderation is tested by assessing the interaction between Year 1 HA and Year 1 marijuana use. Although our data are correlational, given the temporal precedence of the variables (i.e., that HA and marijuana use in Year 1 are predicting anxiety in Year 2), significant coefficients for β2 and β3 are consistent with the possibility that initial HA affects subsequent anxiety, and that the relation of initial HA on subsequent HA is moderated by initial marijuana use, respectively (Rogosa, 1980).
Figure 1.
Sample cross-lag structural regression model. Hypothesized relations were tested with two multiple regression models. Heavier lines indicate the two paths of primary theoretical interest assessing the cross-lagged effect of initial temperament on subsequent psychopathology (β2) and the degree to which initial marijuana use moderates the cross-lagged effect of initial temperament on subsequent psychopathology (β3).
To further test our hypothesized relations, additional autoregressive, cross-lagged, and cross-lagged moderation effects are tested in Model 2 in which Year 2 HA is the outcome. Specifically, γ1 assesses the autoregressive or lagged effect of Year 1 HA predicting Year 2 HA. These relations are not of particular theoretical interest here, but because this tests the temporal stability of temperament, we expect the autoregressive effects in these second models to be significant. Of primary theoretical interest are γ2 and γ3. γ2 tests the effect of Year 1 anxiety symptoms on Year 2 HA. Because we expect the relations between temperament and psychopathology to reflect the effect of the more stable temperament variables affecting subsequent psychopathology rather than initial symptoms of psychopathology affecting subsequent temperament, we do not expect initial anxiety symptoms to predict subsequent HA. Thus, we expect γ2 to be non-significant. Similarly, we have no theoretical expectation that the impact of initial anxiety symptoms on subsequent temperament will be moderated by marijuana use, so we do not expect γ3 to be significant. In this way, non-significant coefficients for γ2 and γ3, coupled with significant coefficients for β2 and/or β3, provide additional evidence for our hypothesized relations. In sum, to the degree that relations between temperament and anxiety reflect the effect of initial temperament on subsequent anxiety and not the effect of initial anxiety on subsequent temperament, we expect significant effects in β2 and/or β3, but not γ2 and γ3.
This framework just described was repeated six times to test the relation of each aspect of temperament (HA, NS, and RD) on each outcome variable (symptoms of anxiety and depression). Figure 1 shows a simplified model highlighting the autoregressive, cross-lagged, and moderated cross-lagged relations. In addition to these three variables, each model also contained five additional predictors. First, given the presence of marijuana use in the interaction term to test for moderation (e.g., Year 1 HA x Year 1 marijuana use), all models also included the simple effect of Year 1 marijuana use as a predictor. This variable is also of theoretical interest because it assesses the simple effect of marijuana on anxiety and depression symptoms. We also included gender and its interactions with temperament and marijuana use (e.g., HA x Gender, Marijuana Use x Gender, HA x Marijuana Use x Gender) to test whether interrelations among temperament, marijuana use, and symptoms of anxiety and depression differ for males and females.
All continuous variables were mean-centered before analyses, and gender was coded as 1 = male and −1 = female. All model assumptions (e.g., homoscedasticity, normality of distributions) were met. When the predicted interaction between temperament and marijuana use reflecting our primary test of moderation was significant, we explored the form of the interaction by plotting and testing the simple effects of temperament on anxiety or depression symptoms at lower and higher levels of marijuana use following Aiken and West (1991). The values of lower and higher marijuana use selected to test the simple effects were based on examination of the distribution of marijuana use reported in the TLFB in Year 1 with the goal of assessing effects at values that reflect actual levels of low and high use in our sample. Based on use within our sample, we plot and statistically test the effects of temperament on anxiety and depression at 0 days (low use) and 25.80 days (high use) of marijuana use, with the latter reflecting the mean level of use reported by frequent users on the TLFB in Year 1. The low marijuana use group included all participants recruited as never users (i.e., they all reported 0 days of use in the past 30 days on the TLFB) as well as 48 infrequent users who also happened to have no days of use in the 30 days prior to completion of the Year 1 TLFB. We also conducted ancillary simple effects tests using −/+ .5 standard deviations to represent low (M = 2.07 days) and high (M = 13.47 days) levels of marijuana use. Results were identical to those reported here.
Results
Preliminary Analyses
Table 1 presents descriptive statistics from our sample by categorical Marijuana Use Group classification at time of study enrollment (never, infrequent, frequent). Age, ethnicity, and gender measured in Year 1 did not differ across groups. One-way ANOVAs on the temperament variables revealed a significant effect of Marijuana Use Group only on NS, with more frequent marijuana use associated with higher novelty seeking. One-way ANOVAs also revealed significant differences in depression among the Marijuana Use Groups in both Year 1 and Year 2, with those who use marijuana reporting more depression symptoms. Marijuana users were also more likely to meet or exceed the “at risk” threshold for clinical levels of depression in Year 1 (ASR T score greater than or equal to 65). While there was no marijuana use group effect on anxiety symptoms, those who use marijuana were more likely to meet or exceed the “at-risk” threshold for clinical levels of anxiety in Year 1.
In addition to examining marijuana use categorically based on use at study enrollment, we can also examine marijuana use continuously based on TLFB via bivariate correlations (See Table 2). When examined continuously, marijuana use was only weakly associated with Year 1 depression symptoms, but not with Year 2 depression symptoms. It was unrelated to anxiety. More frequent marijuana use was associated with higher NS. Of theoretical interest, HA was positively correlated with Year 1 and Year 2 anxiety and depression symptoms. Neither Marijuana Use frequency, NS, nor RD were correlated with anxiety or depression symptoms.
Table 2.
Bivariate Correlations Among Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Year 1 Marijuana Use | ___ | ||||||
| 2. Harm Avoidance | −.01 | ___ | |||||
| 3. Novelty Seeking | .40** | −.32** | ___ | ||||
| 4. Reward Dependence | .01 | −.14* | .12* | ___ | |||
| 5. Year 1 Anxiety | .05 | .57** | −.06 | .03 | ___ | ||
| 6. Year 1 Depression | .13* | .55** | .04 | .02 | .68** | ___ | |
| 7. Year 2 Anxiety | .01 | .46** | −.04 | .00 | .68** | .50** | ___ |
| 8. Year 2 Depression | .05 | .42** | .05 | −.06 | .51** | .63** | .69** |
Note.
p < .05
p < .01
+p < 0.10
Main Analyses
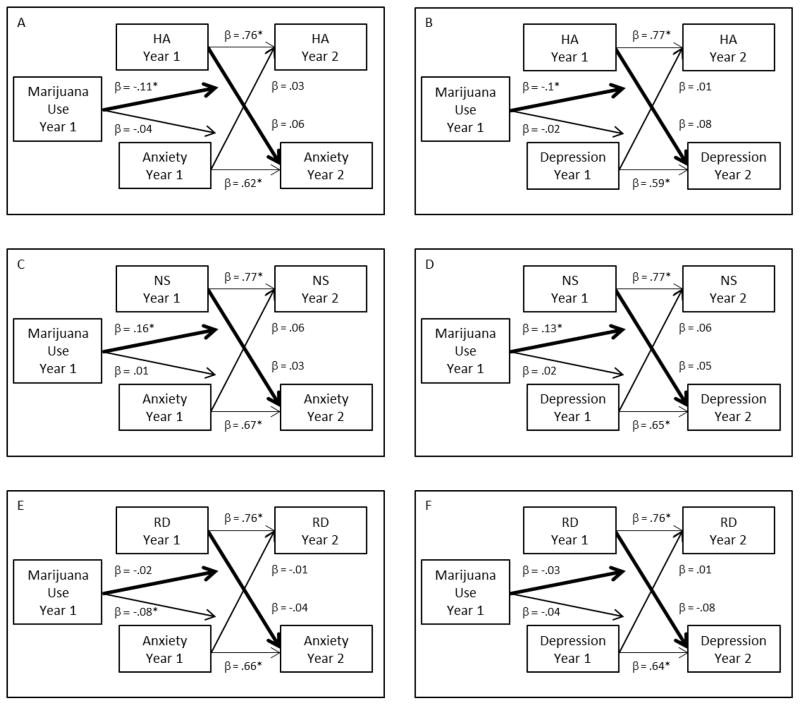
The preliminary correlational analyses (see Table 2) show consistent simple relations between HA and anxiety and depression symptoms in both Years 1 and 2. To more specifically test our hypotheses about the relation of temperament to subsequent anxiety and depression symptoms, as well as the moderating effect of marijuana on this relation, we conducted a series of cross-lag regression models, as described in the Analysis Strategy. To facilitate interpretation, Figure 2 presents the coefficients of greatest interest in testing our hypotheses (cf. Figure 1) while Table 3 presents full model output including all predictors.
Figure 2.
Cross-lag structural regression models assessing the relation of Harm Avoidance and Marijuana Use to levels of Anxiety (Panel A) and Depression (Panel B), Novelty Seeking and Marijuana Use to levels of Anxiety (Panel C) and Depression (Panel D), and Reward Dependence and Marijuana Use to levels of Anxiety (Panel E) and Depression (Panel F). Heavier lines indicate the cross-lagged and moderated cross-lagged relations of primary theoretical significance. * p < .05 (see Table 3 for exact significance levels).
Table 3.
Full Regression Models
| Harm Avoidance | |||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| HA and Anxiety | HA and Depression | ||||||
|
| |||||||
| Model 1: DV = Anxiety | β | t | p | Model 1: DV = Depression | β | t | p |
| Year 1 Anxiety | 0.62 | 12.76 | <0.001 | Year 1 Depression | 0.59 | 11.30 | <0.001 |
| Year 1 HA | 0.06 | 1.24 | 0.22 | Year 1 HA | 0.08 | 1.52 | 0.13 |
| Marijuana Use Frequency | −0.02 | −0.54 | 0.59 | Marijuana Use Frequency | −0.03 | −0.65 | 0.52 |
| Gender | −0.09 | −2.31 | 0.02 | Gender | 0.01 | 0.17 | 0.87 |
| HA X Marijuana Use | −0.11 | −2.69 | 0.01 | HA X Marijuana Use | −0.10 | −2.22 | 0.03 |
| Marijuana Use x Gender | 0.01 | 0.20 | 0.84 | Marijuana Use x Gender | −0.02 | −0.50 | 0.62 |
| HA X Gender | 0.00 | −0.09 | 0.93 | HA X Gender | 0.00 | 0.07 | 0.94 |
| HA X Marijuana Use X Gender | −0.02 | −0.35 | 0.73 | HA X Marijuana Use x Gender | 0.02 | 0.49 | 0.63 |
|
| |||||||
| Model 2: DV = HA | β | t | p | Model 2: DV = HA | β | t | p |
|
| |||||||
| Year 1 HA | 0.76 | 18.88 | <0.001 | Year 1 HA | 0.77 | 19.24 | <0.001 |
| Year 1 Anxiety | 0.03 | 0.79 | 0.43 | Year 1 Depression | 0.01 | 0.28 | 0.78 |
| Marijuana Use Frequency | −0.05 | −1.59 | 0.11 | Marijuana Use Frequency | −0.05 | −1.38 | 0.17 |
| Gender | −0.05 | −1.39 | 0.17 | Gender | −0.05 | −1.53 | 0.13 |
| Anxiety X Marijuana Use | −0.04 | −1.19 | 0.23 | Depression X Marijuana Use | −0.02 | −0.43 | 0.67 |
| Marijuana Use x Gender | 0.01 | 0.17 | 0.86 | Marijuana Use x Gender | 0.01 | 0.24 | 0.81 |
| Anxiety x Gender | −0.07 | −2.24 | 0.03 | Depression X Gender | −0.06 | −1.82 | 0.07 |
| Anxiety X Marijuana Use x Gender | −0.01 | −0.26 | 0.80 | Depression X Marijuana Use X Gender | 0.03 | 0.89 | 0.37 |
| Novelty Seeking | |||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| NS and Anxiety | NS and Depression | ||||||
|
| |||||||
| Model 1: DV = Anxiety | β | t | p | Model 1: DV = Depression | β | t | p |
| Year 1 Anxiety | 0.67 | 16.67 | <0.001 | Year 1 Depression | 0.65 | 14.84 | <0.001 |
| Year 1 NS | 0.03 | 0.58 | 0.56 | Year 1 NS | 0.05 | 1.18 | 0.24 |
| Marijuana Use Frequency | −0.10 | −2.22 | 0.03 | Marijuana Use Frequency | −0.12 | −2.46 | 0.02 |
| Gender | −0.08 | −1.78 | 0.08 | Gender | 0.04 | 0.76 | 0.45 |
| NS X Marijuana Use | 0.16 | 3.80 | <.001 | NS X Marijuana Use | 0.13 | 2.93 | 0.00 |
| Marijuana Use x Gender | 0.09 | 1.87 | 0.06 | Marijuana Use x Gender | 0.07 | 1.41 | 0.16 |
| NS X Gender | −0.05 | −1.26 | 0.21 | NS X Gender | −0.05 | −1.06 | 0.29 |
| NS X Marijuana Use X Gender | −0.04 | −0.91 | 0.36 | NS X Marijuana Use x Gender | −0.07 | −1.51 | 0.13 |
|
| |||||||
| Model 2: DV = NS | β | t | p | Model 2: DV = NS | β | t | p |
|
| |||||||
| Year 1 NS | 0.77 | 20.61 | <0.001 | Year 1 NS | 0.77 | 20.59 | <0.001 |
| Year 1 Anxiety | 0.06 | 1.80 | 0.07 | Year 1 Depression | 0.06 | 1.68 | 0.09 |
| Marijuana Use Frequency | 0.03 | 0.91 | 0.36 | Marijuana Use Frequency | 0.01 | 0.35 | 0.73 |
| Gender | −0.05 | −1.31 | 0.19 | Gender | −0.03 | −0.96 | 0.34 |
| Anxiety X Marijuana Use | 0.01 | 0.37 | 0.72 | Depression X Marijuana Use | 0.02 | 0.61 | 0.54 |
| Marijuana Use x Gender | −0.04 | −1.04 | 0.30 | Marijuana Use x Gender | −0.02 | −0.64 | 0.52 |
| Anxiety x Gender | −0.05 | −1.60 | 0.11 | Depression X Gender | −0.02 | −0.49 | 0.63 |
| Anxiety X Marijuana Use x Gender | 0.02 | 0.57 | 0.57 | Depression X Marijuana Use X Gender | −0.04 | −1.11 | 0.27 |
| Reward Dependence | |||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| RD and Anxiety | RD and Depression | ||||||
|
| |||||||
| Model 1: DV = Anxiety | β | t | p | Model 1: DV = Depression | β | t | p |
| Year 1 Anxiety | 0.66 | 16.19 | <0.001 | Year 1 Depression | 0.64 | 14.49 | <0.001 |
| Year 1 RD | −0.04 | −1.08 | 0.28 | Year 1 RD | −0.08 | −1.91 | 0.06 |
| Marijuana Use Frequency | −0.01 | −0.14 | 0.89 | Marijuana Use Frequency | −0.02 | −0.46 | 0.65 |
| Gender | −0.12 | −2.97 | <.0.01 | Gender | −0.03 | −0.60 | 0.55 |
| RD X Marijuana Use | −0.02 | −0.49 | 0.62 | RD X Marijuana Use | −0.03 | −0.65 | 0.52 |
| Marijuana Use x Gender | 0.02 | 0.59 | 0.56 | Marijuana Use x Gender | 0.00 | −0.09 | 0.93 |
| RD X Gender | −0.02 | −0.60 | 0.55 | RD X Gender | −0.06 | −1.35 | 0.18 |
| RD X Marijuana Use X Gender | 0.06 | 1.47 | 0.14 | RD X Marijuana Use x Gender | 0.06 | 1.38 | 0.17 |
|
| |||||||
| Model 2: DV = RD | β | t | p | Model 2: DV = RD | β | t | p |
|
| |||||||
| Year 1 RD | 0.76 | 22.44 | <0.001 | Year 1 RD | 0.76 | 22.26 | <0.001 |
| Year 1 Anxiety | −0.01 | −0.36 | 0.72 | Year 1 Depression | 0.00 | 0.06 | 0.96 |
| Marijuana Use Frequency | 0.05 | 1.51 | 0.13 | Marijuana Use Frequency | 0.05 | 1.56 | 0.12 |
| Gender | −0.14 | −3.92 | <0.001 | Gender | −0.14 | −3.89 | <0.001 |
| Anxiety X Marijuana Use | −0.08 | −2.44 | 0.02 | Depression X Marijuana Use | −0.04 | −0.98 | 0.33 |
| Marijuana Use x Gender | −0.10 | −3.03 | <0.01 | Marijuana Use x Gender | −0.10 | −2.86 | <0.01 |
| Anxiety x Gender | −0.02 | −0.58 | 0.56 | Depression X Gender | −0.02 | −0.51 | 0.61 |
| Anxiety X Marijuana Use x Gender | −0.01 | −0.21 | 0.83 | Depression X Marijuana Use X Gender | 0.02 | 0.62 | 0.53 |
Note. All regression coefficients are standardized.
Harm avoidance and anxiety
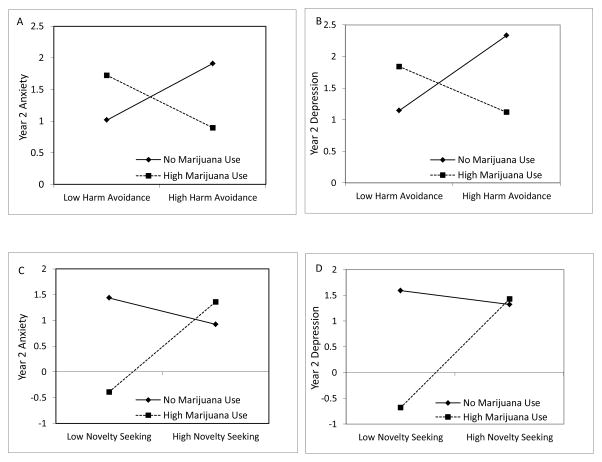
The first model we ran tests our primary hypotheses that initial temperament predicts subsequent psychopathology, and that this relation may be moderated by marijuana use (i.e., Model 1 in Figure 1). This was done by regressing Year 2 Anxiety on Year 1 HA, Year 1 Marijuana Use, Year 1 Anxiety, the HA x Marijuana Use interaction term, Gender, and all interaction terms involving Gender. This model revealed three significant effects (Table 3). Not surprisingly, Year 1 Anxiety symptoms significantly predicted Year 2 Anxiety symptoms. There was also a significant Gender effect, with women reporting more Year 2 Anxiety symptoms than men. Of interest, when these other variables were included in the model, HA was not an independent predictor of Year 2 Anxiety symptoms. However, consistent with hypotheses, HA did interact with Marijuana Use in predicting Anxiety symptoms (Figure 2, Panel A). To understand this interaction, we conducted simple slope analyses separately assessing the relation between HA and Year 2 Anxiety for those low and high in Marijuana Use (Aiken & West, 1991). As can be seen in Figure 3, Panel A, when frequency of Marijuana Use was low, increases in Year 1 HA were associated with greater anxiety in Year 2 (β=.15, t(329)=2.69, p<.01). By contrast, as predicted, Marijuana Use had a buffering effect as reflected in a non-significant relation between HA and Anxiety when Marijuana Use frequency was high (β=−.14, t(329)=−1.40, p=.16).
Figure 3.
Simple effects of Harm Avoidance and Novelty Seeking on levels Anxiety and Depression as a function of Marijuana Use.
To further evaluate our hypotheses, we also tested a second model assessing the other possible cross-lagged effect – that initial psychopathology predicts subsequent temperament (Model 2 in Figure 1). This was tested by regressing Year 2 HA on Year 1 HA, Year 1 Anxiety, Year 1 Marijuana Use, the Anxiety x Marijuana Use interaction term, Gender, and all interaction terms involving gender. Not surprisingly, Year 1 HA predicted Year 2 HA (Table 3). Of primary theoretical relevance, neither the simple cross-lagged effect of Year 1 Anxiety nor the moderated cross-lagged effect of Year 1 Anxiety x Marijuana Use were significant (Figure 2, Panel A). The only other significant effect in this model was the Anxiety x Gender interaction. Tests of simple slopes showed that Year 1 Anxiety was associated with greater Year 2 HA for women (β=.11, t(329)=2.15, p=.03) but not men (β=−.04, t(329)=−.79, p=.43).
Harm Avoidance and depression
Figure 2, Panel B shows the relations of primary theoretical interest in the cross-lag model assessing the relation between HA and Depression symptoms. Considering the first regression model that tests whether initial temperament predicts subsequent psychopathology, Year 1 Depression symptoms were a significant predictor of Year 2 Depression symptoms (see Table 3). The only other significant effect was the predicted HA x Marijuana Use interaction. Simple effects tests revealed a pattern of effects very similar to that obtained for anxiety (Figure 3, Panel B): HA was significantly positively associated with Depression symptoms when Marijuana Use frequency was low (β=.15, t(329)=2.69, p<.01), but Marijuana Use appeared to have a buffering effect as reflected in a non-significant negative relation between HA and Depression symptoms at high levels of Marijuana Use frequency (β=−.09, t(329)=−.92, p=.36).
In the second model predicting Year 2 HA, the only significant predictor was Year 1 HA (see Table 3). Of importance, Year 1 Depression symptoms did not predict Year 2 HA, nor did the Year 1 Depression x Marijuana Use interaction.
Novelty seeking and anxiety
The cross-lag model in Figure 2, Panel C shows the coefficients of primary theoretical interest in assessing the relation between NS and Anxiety. Considering the first regression model that tests whether initial temperament predicts subsequent psychopathology, three effects were significant. Year 1 Anxiety symptoms significantly predicted Year 2 Anxiety symptoms, and greater Marijuana Use frequency in Year 1 was associated with less Anxiety in Year 2 (see Table 3). While NS did not have a direct effect on Anxiety levels, its effect was moderated by Marijuana Use, as reflected in the NS x Marijuana Use interaction. Simple effects displayed in Figure 3, Panel C show that the relation between NS and Anxiety occurs among those with high Marijuana Use frequency. That is, when Marijuana Use frequency was high, Year 1 NS was positively associated with Anxiety symptoms (β=.28, t(329)=3.46, p=.001). There was no relation between NS and Anxiety symptoms when Marijuana Use frequency was low (β=−.08, t(329)=−1.61, p=.11).
In the second model predicting Year 2 NS, the only significant predictor was Year 1 NS (see Table 3). Year 1 Anxiety did not predict Year 2 NS, nor did the Year 1 Anxiety x Marijuana Use interaction.
Novelty seeking and depression
The regression models predicting Year 2 Depression from NS revealed effects very similar to those in the models predicting anxiety from NS (See Figure 2, Panel D). In the first regression model that tests whether initial temperament predicts subsequent psychopathology, there were three significant predictors of Year 2 Depression symptoms (see Table 3). Year 1 Depression was positively associated with Year 2 Depression symptoms, and Year 1 Marijuana Use was negatively associated with Year 2 Depression. The NS x Marijuana Use interaction was also significant. The simple effects in Figure 3, Panel D show that greater Year 1 NS was associated with greater Depression in Year 2 for those with high Marijuana Use frequency (β=.26, t(329)=3.06, p<.01). By contrast, there was no relation between NS and Depression when Marijuana Use was low (β=−.03, t(329)=−.62, p=.54).
In the second model predicting Year 2 NS, the only significant predictor was Year 1 NS (see Table 3). Year 1 Depression levels did not predict Year 2 NS, nor did the Year 1 Depression x Marijuana Use interaction.
Reward dependence and anxiety
Figure 2, Panel E shows the cross-lag relations of primary theoretical interest in assessing the relation between RD and Anxiety levels. The first regression model testing whether initial temperament predicts subsequent psychopathology revealed only two significant effects: greater Year 1 Anxiety was associated with more Year 2 Anxiety and females reported more Anxiety in Year 2 than males (see Table 3). There were no effects of RD on Anxiety symptoms, either independently or moderated by Marijuana Use.
The second regression model predicting Year 2 RD revealed 4 significant effects (see Table 3). Greater Year 1 RD and being female were both associated with higher Year 2 RD. There was also an Anxiety x Marijuana Use interaction. Tests of simple slopes showed a significant negative relation between Year 1 Anxiety levels and Year 2 RD among those who more frequently use marijuana (β=−.14, t(329) =−.2.26, p=.02). The relation between Year 1 Anxiety and Year 2 RD was not significant for low frequency marijuana users (β=.04, t(329)=1.06, p=.29). Finally, the Marijuana Use x Gender interaction was significant. Among women, Marijuana Use was positively associated with greater RD (β=.15, t(329)=3.19, p=.002), but the relation was non-significant for men (β=−.05, t(329)=−1.08, p=.28).
Reward dependence and depression
The first regression model predicting later psychopathology from initial temperament revealed only that Year 1 Depression symptoms predicted Year 2 Depression symptoms (Figure 2, Panel F). In the second model predicting later temperament from initial psychopathology, three effects were significant. Year 1 RD predicted Year 2 RD, and females reported higher Year 2 RD. There was also a Marijuana Use x Gender interaction which showed the same pattern as this same interaction in the model predicting Anxiety from RD. That is, among women, Marijuana Use frequency was positively associated with greater RD (β=.15, t(329)=3.05, p=.002), but the relation was non-significant for men (β=−.05, t(329)=−.94, p=.35).
Discussion
Given the elevated rates of anxiety and depression within late adolescence and early adulthood, the present study examined how another behavior that occurs with relatively high frequency in this age range – marijuana use – is associated with anxiety and depression. There has to date been no clear picture of how marijuana relates to anxiety and depression; thus, we examined how temperament may impact these relations. Of particular interest was HA, which is associated with greater anxiety and depression. One question that has not yet been examined is whether marijuana use moderates the impact of the behavioral biases associated with HA on anxiety and depression.
The temperament dimension of HA is associated with apprehension, pessimism, and inhibition and has been associated with both anxiety and depression (Hansenne et al., 1998; Jianga et al., 2003; Manfredi et al., 2011; Matsudaira et al., 2006). Our prospective analyses show a similar relation, but importantly demonstrate that it is moderated by level of marijuana use. Specifically, we find that HA measured at baseline is associated with more symptoms of both anxiety and depression measured a year later only for those low in marijuana use. By contrast, when marijuana use is high, HA is unrelated to anxiety and depression levels. Of importance, these analyses control for baseline anxiety or depression levels, so our results show the predictive effect of HA and marijuana use over and above levels of anxiety and depression exhibited a year earlier. While the present study cannot speak definitively to the mechanism of our effects, marijuana has been suggested to produce anxiolytic and mood elevating benefits (Sethi et al., 1986; Stewart et al., 1997; Denson & Earleywine, 2006). Such mood benefits could attenuate the greater risk toward anxiety and depression typically associated with HA. Using our cross-lag analysis approach, we see no evidence that initial symptoms of anxiety and depression predict subsequent HA (Model 2 in Figure 1), suggesting that the relations observed between HA, marijuana use, anxiety, and depression are likely due to effects of initial temperament and marijuana use on subsequent psychopathology rather than the converse.
Marijuana use also moderated the relation between NS and anxiety and depression symptoms but the pattern of modulation differed from that with HA. For NS, it was people higher in marijuana use who showed a positive association between NS and both anxiety and depression symptoms. Those low in marijuana use showed no relation between NS and levels of anxiety and depression. Further, the pattern of the interaction was such that levels of anxiety and depression were similarly high for those high in NS and high in marijuana use, as well as those low in NS at all levels of marijuana use. It was individuals low in NS and high in marijuana use that had the lowest anxiety and depression (see Figure 3, Panels C & D). This effect warrants further investigation as it is not clear what mechanism may account for the seemingly protective effect of low NS coupled with high marijuana use or why this benefit of marijuana use is not seen when NS is higher. As with HA, models assessing the relation of initial symptoms of anxiety and depression to subsequent NS fail to show effects of anxiety, depression, or marijuana use frequency, suggesting that the relations observed between NS, marijuana use, anxiety, and depression are likely due to effects of initial temperament and marijuana use on subsequent psychopathology rather than the converse.
Our results reveal no effect of RD on anxiety and depression symptoms. There were no zero-order correlations between RD and anxiety or depression, no independent effects of RD on Year 2 anxiety or depression, and no moderated effect on anxiety and depression. Unexpectedly, RD was the one aspect of temperament that was predicted by an aspect of psychopathology. Specifically, Year 1 Anxiety and Marijuana Use frequency interacted to predict Year 2 RD. Tests of the simple effects show that among those who use marijuana more frequently, reporting more symptoms of Anxiety in Year 1 predicted lower RD in Year 2. Temperament is considered to be relatively stable. Consistent with this, Year 1 temperament was always a significant and large predictor of Year 2 temperament in our models, a relation that was of similar magnitude for RD as compared to HA and NS (see Table 3). We are, therefore, uncertain what accounts for this sole effect of initial psychopathology predicting subsequent temperament. We interpret this relation cautiously and note that the analogous RD and marijuana use interaction was not significant for depression symptoms.
These results have a number of implications for understanding how marijuana affects anxiety and depression, and for how temperament affects anxiety and depression. We have noted that the relation between marijuana and anxiety/depression has been quite variable in past research. We think the present results demonstrate the importance of considering the impact of other factors known to influence anxiety and depression. The interactions we observed between HA and marijuana use and NS and marijuana use indicate that different relations between marijuana use and anxiety/depression levels will be observed depending on the levels of HA and NS within a sample. Consider, for example, the interaction between HA and marijuana use in predicting anxiety (Figure 3, Panel A). If a sample happened to be relatively low in HA, a positive relation between marijuana use and anxiety would be expected but if the sample happened to be high in HA, greater marijuana use might be associated with less anxiety. To our knowledge, no studies examining the effect of marijuana use on anxiety and depression have considered how these relations interact with pre-existing temperament.
It is also important to consider that the simple relations we observed between marijuana use and depression symptoms differed from those obtained in the more complex models. That is, when only marijuana use was considered, results suggest a positive association between marijuana use and depression. This was seen in the Marijuana Use Group main effects in the preliminary categorical analyses, and in a significant (but small) positive bivariate correlation between Year 1 marijuana use and Year 1 depression symptoms. However, in the regression models that prospectively predict anxiety/depression and also include HA or RD, the HA x marijuana use or RD x marijuana use interactions, and baseline anxiety or depression, marijuana use was not an independent predictor of depression symptoms. Moreover, in the models involving NS, marijuana use negatively predicted depression symptoms (and anxiety). These differing patterns of results first demonstrate the importance of measuring the effects of marijuana within the context of other factors known to affect anxiety and depression, as well as prior symptoms of anxiety and depression. The results might also indicate a complex causal relation between marijuana use and depression in which initial symptoms of depression facilitate marijuana use, which subsequently decreases depression. This conclusion, however, is speculative and warrants more explicit examination. At a minimum, our results suggest marijuana does not have an invariant effect of anxiety and depression, and that more research is needed to understand the possible mechanisms through which aspects of temperament and marijuana use affects anxiety and depression.
Another intriguing question raised by our results is whether temperament could affect marijuana use. HA is associated with negative affective states such as apprehension and pessimism, as well as social inhibition (Cloninger et al., 1993). Coping with negative affect, enhancing positive affect, and facilitating social interactions are among the top motivations reported for marijuana use (Lee et al., 2009; Newcomb et al., 1998; Simons et al., 1998), raising the possibility that people high in HA might use marijuana as a way to manage their temperamental predispositions. As marijuana use increases, studying not only the outcomes of its use but also the factors that motivate its use is of increasing relevance. Our results suggest additional specific relations that might be fruitful to examine.
Effects of Gender
Roughly equal numbers of men and women with similar rates of marijuana use were recruited in this sample, providing the opportunity to assess whether predictors of level of anxiety and depression in this age range differ for men and women. There were some gender main effects in the regression analyses predicting anxiety, with women reporting more symptoms of anxiety in Year 2 than men, even when controlling for Year 1 anxiety. This result indicates that anxiety increased more for women that for men in this sample, broadly consistent with higher prevalence rates of anxiety among women (e.g., McLean et al., 2011; NIMH, 2014c). However, gender did not moderate any of the effects of temperament, or the temperament x marijuana use interactions, suggesting that the way temperament relates to anxiety and depression – and how that relation is moderated by marijuana use – occurs similarly for men and women.
Limitations
While our prospective design, relatively large sample, and roughly equal numbers of men and women were strengths of our design, there are limitations to consider. We purposely focused our analyses on a college sample because of the high clinical significance of anxiety, depression, and marijuana use in this age range. However, it is important to interpret results with these contextual factors in mind; it is possible that the relation among these variables differs in other types of samples. Another factor to consider is our use of self-reported symptoms of anxiety and depression. Although the measure we used to assess anxiety and depression has demonstrated validity with clinical assessments (Achenbach & Rescorla, 2003), no independent clinical assessments were available for our participants. Moreover, we examined our hypotheses within the context of a broad range of anxiety and depression symptomology. While the number of participants meeting clinical thresholds for anxiety and depression was modest (Table 1), subclinical levels of anxiety and depression are associated with meaningful functional impairments (Dotson et al., 2014; Kessler et al., 1997; Karsten et al., 2011). Subclinical symptoms are also precursors to clinical conditions (Hill et al., 2014; Shankman et al., 2009).
A final important consideration is that our analyses are based on correlational data. Given the variables involved – temperament, substance use, and symptoms associated with psychopathology – true experiments are not feasible. We attempted to maximize our inferential power through methodological decisions such as the longitudinal design so that marijuana use and temperament were measured one year before anxiety and depression symptoms. Use of cross-lag analyses also allowed us to statically assess the plausibility of our proposed model that initial temperament and marijuana use affect subsequent and depression over the alternative model that initial anxiety/depression and marijuana use affect subsequent temperament. Nevertheless, our conclusions are ultimately correlational and the implications of the results must be interpreted with that limitation in mind. Moreover, that conclusions are based on only two points in time is another limitation to consider.
Conclusions
Our results highlight the importance of simultaneously assessing the effect of marijuana use on anxiety and depression within the context of other factors known to predict psychopathology by showing that marijuana use and temperament interact complexly in predicting risk for anxiety and depression. These results may help explain why marijuana’s effects on anxiety and depression have been variable in past research. They also show that even for a temperament dimension consistently linked with anxiety and depression (HA), other factors have important moderating influences on its effects. Another important implication of our results is that it is not only important to assess these complex relations among multiple factors, but also the causal mechanisms they imply. Our results suggest that marijuana’s anxiolytic and mood-enhancing effects (or perceived effects) may attenuate the effects of HA on risk for anxiety and depression, raising the question of whether such effects might motivate individuals high in HA to use marijuana. As marijuana use becomes more readily available and accepted, it will be important to consider these kinds of potential motivations for its use. Finally, from the perspective of treatment and intervention, the lack of simple effects of marijuana use on anxiety and depression argues against marijuana reduction interventions as strategies that will necessarily decrease risk for anxiety and depression within this age range. Instead, the benefits of decreasing marijuana use will depend on other characteristics, such as temperament.
Supplementary Material
Acknowledgments
This work was supported by NIH DA024002 to Tiffany Ito and NIH K23DA033302 to L. Cinnamon Bidwell.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA adult forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2003. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks: Sage Publications; 1991. [Google Scholar]
- Barkley R, Murphy K. A clinical workbook: Attention-deficit hyperactivity disorder. Guilford; New York: 1998. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years later. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ, Leen-Feldner EW, Feldner MT, Yartz AR. Marijuana use among daily tobacco smokers: Relationship to anxiety-related factors. Journal of Psychopathology and Behavioral Assessment. 2005;27(4):279–289. [Google Scholar]
- Carey KB, Neal DJ, Collins SE. A psychometric analysis of the self-regulation questionnaire. Addictive Behaviors. 2004;29:253–260. doi: 10.1016/j.addbeh.2003.08.001. [DOI] [PubMed] [Google Scholar]
- Chen CY, Wagner FA, Anthony JC. Marijuana use and the risk of Major Depressive Episode: Epidemiological evidence from the United States National Comorbidity Survey. Social Psychiatry and Psychiatric Epidemiology. 2002;37:199–206. doi: 10.1007/s00127-002-0541-z. [DOI] [PubMed] [Google Scholar]
- Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Archives of General Psychiatry. 1993;50(12):975–990. doi: 10.1001/archpsyc.1993.01820240059008. [DOI] [PubMed] [Google Scholar]
- Cloninger CR, Svrakic DM, Przybeck TR. Can personality assessment predict future depression? A twelve-month follow-up of 631 subjects. Journal of Affective Disorders. 2006;92(1):35–44. doi: 10.1016/j.jad.2005.12.034. [DOI] [PubMed] [Google Scholar]
- Colorado Amendment 64. Amendment 64: Use and Regulation of Marijuana. 2012 http://www.colorado.gov/cs/Satellite?blobcol=urldata&blobheader=application%2Fpdf&blobkey=id&blobtable=MungoBlobs&blobwhere=1251834064719&ssbinary=true.
- Copeland W, Landry K, Stanger C, Hudziak JJ. Multi-informant assessment of temperament in children with externalizing behavior problems. Journal of Clinical Child and Adolescent Psychology. 2004;33(3):547–556. doi: 10.1207/s15374424jccp3303_12. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Chiu WT, Sampson N, Kessler RC, Anthony JC, Angermeyer M, Bruffaerts R, de Girolamo G, Gureje O, Huang Y, Karam A, Kostyuchenko S, Lepine JP, Mora MEM, Neumark Y, Ormel JH, Pinto-Meza A, Posada-Villa J, Stein DJ, Takeshima T, Wells EJ. Toward a global view of alcohol, tobacco, cannabis, and cocaine use: Findings from the WHO World Mental Health Surveys. PLoS Medicine. 2008;5(7):e141. doi: 10.1371/journal.pmed.0050141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Hall W, Lynskey M. The relationship between cannabis use, depression and anxiety among Australian adults: findings from the National Survey of Mental Health and Well-Being. Social Psychiatry and Psychiatric Epidemiology. 2001;36:219–227. doi: 10.1007/s001270170052. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Hall W, Lynskey M. Exploring the association between cannabis use and depression. Addiction. 2003;98:1493–1504. doi: 10.1046/j.1360-0443.2003.00437.x. [DOI] [PubMed] [Google Scholar]
- Denson TF, Earleywine M. Decreased depression in marijuana users. Addictive Behaviors. 2006;31(4):738–742. doi: 10.1016/j.addbeh.2005.05.052. [DOI] [PubMed] [Google Scholar]
- Dotson VM, Szymkowicz SM, Kirton JW, McLaren ME, Green ML, Rohani JY. Unique and interactive effect of anxiety and depressive symptoms on cognitive and brain function in young and older adults. Journal of Depression and Anxiety. 2014;S1:1–10. doi: 10.4172/2167-1044.S1-003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer A, Mahmood A, Redman K, Harris T, Sadler S, McGuffin P. A sib-pair study of the Temperament and Character Inventory scales in major depression. Archives of General Psychiatry. 2003;60(5):490–496. doi: 10.1001/archpsyc.60.5.490. [DOI] [PubMed] [Google Scholar]
- Gallup, C.N.N., U.S.A. Today Poll. Poll questions. 2013 Aug 2; retrieved from: http://www.gallup.com/poll/163835/tried-marijuana-little-changed-80s.aspx.
- Green BE, Ritter C. Marijuana use and depression. Journal of Health and Social Behavior. 2000:40–49. [PubMed] [Google Scholar]
- Guimaraes F, Chiaretti T, Graeff F, Zuardi A. Antianxiety effect of cannabidiol in the elevated plus-maze. Psychopharmacology. 1990;100(4):558–559. doi: 10.1007/BF02244012. [DOI] [PubMed] [Google Scholar]
- Hansenne M, Pitchot W, Gonzalez Moreno A, Machurot P, Ansseau M. The tridimensional personality questionnaire (TPQ) and depression. European Psychiatry. 1998;13(2):101–103. doi: 10.1016/S0924-9338(98)80026-6. [DOI] [PubMed] [Google Scholar]
- Hansenne M, Reggers J, Pinto E, Kjiri K, Ajamier A, Ansseau M. Temperament and Character Inventory (TCI) and depression. Journal of Psychiatric Research. 1999;33(1):31–36. doi: 10.1016/s0022-3956(98)00036-3. [DOI] [PubMed] [Google Scholar]
- Hayatbakhsh MR, Najman JM, Jamrozik K, Mamun AA, Alati R, Bor W. Cannabis and anxiety and depression in young adults: A large prospective study. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(3):408–417. doi: 10.1097/chi.0b013e31802dc54d. [DOI] [PubMed] [Google Scholar]
- Hill RM, Pettit JW, Lewinsohn PM, Seeley JR, Klein DN. Escalation to Major Depressive Disorder among adolescents with subthreshold depressive symptoms: Evidence of distinct subgroups at risk. Journal of Affective Disorders. 2014;8:133–138. doi: 10.1016/j.jad.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang N, Sato T, Hara T, Takedomi Y, Ozaki I, Yamada S. Correlations between trait anxiety, personality and fatigue: Study based on the Temperament and Character Inventory. Journal of Psychosomatic Research. 2003;55(6):493–500. doi: 10.1016/s0022-3999(03)00021-7. [DOI] [PubMed] [Google Scholar]
- Karsten J, Nolen WA, Penninx BW, Hartman CA. Subthreshold anxiety better defined by symptom self-report than by diagnostic interview. Journal of Affective Disorders. 2011;129(1–3):236–43. doi: 10.1016/j.jad.2010.09.006. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey I: Lifetime prevalence, chronicity, and recurrence. Journal of Affective Disorders. 1993;29:85–96. doi: 10.1016/0165-0327(93)90026-g. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Zhao S, Blazer DG, Swartz M. Prevalence, correlates, and course of minor depression and major depression in the National Comorbidity Survey. Journal of Affective Disorders. 1997;45(1–2):19–30. doi: 10.1016/s0165-0327(97)00056-6. [DOI] [PubMed] [Google Scholar]
- Lee CM, Neighbors C, Hendershot CS, Grossbard JR. Development and preliminary validation of a comprehensive marijuana motives questionnaire. Journal of Studies on Alcohol and Drugs. 2009;70(2):279. doi: 10.15288/jsad.2009.70.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manfredi C, Caselli G, Rovetto F, Rebecchi D, Ruggiero GM, Sassaroli S, Spada MM. Temperament and parental styles as predictors of ruminative brooding and worry. Personality and Individual Differences. 2011;50(2):186–191. [Google Scholar]
- Matsudaira T, Kitamura T. Personality traits as risk factors of depression and anxiety among Japanese students. Journal of Clinical Psychology. 2006;62(1):97–109. doi: 10.1002/jclp.20215. [DOI] [PubMed] [Google Scholar]
- McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. Journal of Psychiatric Research. 2011;45:1027–1035. doi: 10.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechoulam R, Parker LA, Gallily R. Cannabidiol: An overview of some pharmacological aspects. The Journal of Clinical Pharmacology. 2002;42(S1):11S–19S. doi: 10.1002/j.1552-4604.2002.tb05998.x. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J-p, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in US adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musty RE, Kaback L. Relationships between motivation and depression in chronic marijuana users. Life Sciences. 1995;56(23):2151–2158. doi: 10.1016/0024-3205(95)00202-h. [DOI] [PubMed] [Google Scholar]
- National Institute of Drug Abuse (NIDA) DrugFacts: Marijuana. 2014 Retrieved from http://www.drugabuse.gov/publications/drugfacts/marijuana.
- National Institute of Mental Health (NIMH) Any anxiety disorder among adults. 2014a Retrieved from http://www.nimh.nih.gov/health/statistics/prevalence/any-anxiety-disorder-among-adults.shtml.
- National Institute of Mental Health (NIMH) Any mood disorder among adults. 2014b Retrieved from http://www.nimh.nih.gov/health/statistics/prevalence/any-mood-disorder-among-adults.shtml.
- National Institute of Mental Health (NIMH) Anxiety disorders. 2014c Retrieved from http://www.nimh.nih.gov/health/topics/anxiety-disorders/index.shtml.
- Newcomb MD, Chou CP, Bentler PM, Huba G. Cognitive motivations for drug use among adolescents: Longitudinal tests of gender differences and predictors of change in drug use. Journal of Counseling Psychology. 1988;35(4):426–438. [Google Scholar]
- Rogosa D. A critique of cross-lagged correlation. Psychological Bulletin. 1980;88(2):245. [Google Scholar]
- Scholes-Balog KE, Hemphill SA, Patton GC, Toumbourou JW. Cannabis use and related harms in the transition to young adulthood: A longitudinal study of Australian secondary school students. Journal of Adolescence. 2013;36(3):519–527. doi: 10.1016/j.adolescence.2013.03.001. [DOI] [PubMed] [Google Scholar]
- Sethi B, Trivedi J, Kumar P, Gulati A, Agarwal A, Sethi N. Antianxiety effect of cannabis: involvement of central benzodiazepine receptors. Biological Psychiatry. 1986;21(1):3–10. doi: 10.1016/0006-3223(86)90003-x. [DOI] [PubMed] [Google Scholar]
- Shankman SA, Lewinsohn PM, Klein DN, Small JW, Seeley JR, Altman SE. Subthreshold conditions as precursors for full syndrome disorders: A 15-year longitudinal study of multiple diagnostic classes. Journal of Child Psychology and Psychiatry. 2009;50:1485–1494. doi: 10.1111/j.1469-7610.2009.02117.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons J, Correia CJ, Carey KB, Borsari BE. Validating a five-factor marijuana motives measure: Relations with use, problems, and alcohol motives. Journal of Counseling Psychology. 1998;45(3):265–273. [Google Scholar]
- Soares VdP, Campos AC, Bortoli VCd, Zangrossi H, Jr, Guimaraes FS, Zuardi AW. Intra-dorsal periaqueductal gray administration of cannabidiol blocks panic-like response by activating 5-HT1A receptors. Behavioural Brain Research. 2010;213(2):225–229. doi: 10.1016/j.bbr.2010.05.004. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Follow-back: A technique for assessing self-reported ethanol consumption. In: Allen J, Litten RZ, editors. Measuring Alcohol Consumption: Psychosocial and Biological Methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Starcevic V, Uhlenhuth E, Fallon S, Pathak D. Personality dimensions in panic disorder and generalized anxiety disorder. Journal of Affective Disorders. 1996;37(2):75–79. doi: 10.1016/0165-0327(95)00058-5. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Karp J, Pihl RO, Peterson RA. Anxiety sensitivity and self-reported reasons for drug use. Journal of Substance Abuse. 1997;9:223–240. doi: 10.1016/s0899-3289(97)90018-3. [DOI] [PubMed] [Google Scholar]
- Strakowski SM, Dunayevich E, Keck PE, Jr, McElroy SL. Affective state dependence of the Tridimensional Personality Questionnaire. Psychiatry Research. 1995;57(3):209–214. doi: 10.1016/0165-1781(95)02655-g. [DOI] [PubMed] [Google Scholar]
- Washington Initiative 502. Summary of Initiative 502. 2012 http://www.leg.wa.gov/House/Committees/OPRGeneral/Documents/2012/I-502%20summary.pdf.
- Young LT, Bagby RM, Cooke RG, Parker JD, Levitt AJ, Joffe RT. A comparison of Tridimensional Personality Questionnaire dimensions in bipolar disorder and unipolar depression. Psychiatry Research. 1995;58(2):139–143. doi: 10.1016/0165-1781(95)02684-o. [DOI] [PubMed] [Google Scholar]
- Zuardi A, Crippa J, Hallak J, Moreira F, Guimaraes F. Cannabidiol, a Cannabis sativa constituent, as an antipsychotic drug. Brazilian Journal of Medical and Biological Research. 2006;39(4):421–429. doi: 10.1590/s0100-879x2006000400001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.