Summary
Background
The laboratory interpretation of blood film morphology is frequently a rapid, accurate, and cost-effective final-stage of blood count analysis. However, the interpretation of findings often rests with a single individual, and errors can carry significant impact. Cell identification and classification skills are well supported by existing resources, but the contribution and importance of other skills are less well understood.
Methods
The UK external quality assurance group in haematology (UK NEQAS(H)) runs a Continued Professional Development scheme where large digital-images of abnormal blood smears are presented using a web-based virtual microscope. Each case is answered by more than 800 individuals. Morphological feature selection and prioritisation, as well as diagnosis and proposed action, are recorded. We analysed the responses of participants, aiming to identify successful strategies as well as sources of error.
Findings
The approach to assessment by participants depended on the affected cell type, case complexity or skills of the morphologist. For cases with few morphological abnormalities, we found that accurate cell identification and classification were the principle requirements for success. For more complex films however, feature recognition and prioritisation had primary importance. Additionally however, we found that participants employed a range of heuristic techniques to support their assessment, leading to associated bias and error.
Interpretation
A wide range of skills together allow successful morphological assessment and the complexity of this process is not always understood or recognised. Heuristic techniques are widely employed to support or reinforce primary observations and to simplify complex findings. These approaches are effective and are integral to assessment; however they may also be a source of bias or error. Improving outcomes and supporting diagnosis require the development of decision-support mechanisms that identify and support the benefits of heuristic strategies while identifying or avoiding associated biases.
Funding
The CPD scheme is funded by participant subscription.
Keywords: Blood cell morphology, Diagnosis, Cell recognition, Heuristics, Errors
Highlights
-
•
Morphological assessment of blood films at all levels requires complex problem-solving skills
-
•
In all cases morphologists apply heuristic approaches; these differ according to case complexity
-
•
Biases related to heuristics are evident in many errors, avoiding them requires specific strategies
When a large group of healthcare professionals examined the same blood films using a digital “virtual microscope”, we found that individuals supported their knowledge-based decisions using a range of additional techniques to reinforce or simplify their analyses. These skills are similar to those used in many different areas of human decision-making and support rapid and accurate choices. However, the approaches may also lead to unrecognised bias (as we have found in our study). To reduce errors in diagnosis, we suggest that training and support systems should identify and reinforce these choice-skills, while seeking to identify and avoid associated bias.
1. Introduction
The United Kingdom National External Quality Assurance Scheme for Haematology (UK NEQAS(H)) provides a Continued Professional Development (CPD) scheme serving more than 2000 individuals within the UK and internationally, with around 1000 individuals completing each release. The scheme presents participants with large digital images of blood films within a software environment that mirrors elements of the microscope, and tests skills of feature identification and interpretation (Brereton et al., 2008). The outcome of interpreting morphology presented as digital slides is comparable with results using conventional microscopy of blood smears on glass slides (Burthem et al., 2005). The cases vary in complexity, and the level of skill or experience of participants differs, so the outcome of interpretation often varies markedly. We have assumed that errors of interpretation reflect lower levels of experience or knowledge, and that similar principles of interpretation and error apply across all cases. However, we have not previously tested whether these assumptions are correct. Drawing on evidence from other spheres of medicine, the present paper examines how our participants approach interpretation of blood film morphology and why that interpretation is sometimes incorrect.
Interpretation of blood films is a complex process: the first and central skill is the assignment of identities to the cells that are present (recognition and classification). If more than one cellular element is abnormal then the different features must be prioritised relative to each other (weighting). The goal in all cases involves an interpretation of the findings (decision), but the nature of that decision may depend on level of skill and responsibility of the morphologist (expectation). In the laboratory setting, the time devoted to blood film examination is strongly influenced by the requirement to finish and move to next piece of work (completion). To help manage this complex decision process we consciously and unconsciously apply strategies that enable us to simplify and focus our analysis. The unconscious strategies are encompassed by the term “heuristics” (Shah and Oppenheimer, 2008). When they work well, heuristic approaches permit rapid and accurate interpretation: For example small children can readily and very rapidly identify different animals presented in pictures; by contrast computers struggle to reproduce this level of accuracy (Zhang et al., 2011). However, the “fast and frugal” heuristics that allow humans to outperform computers in many contexts can also be a source of bias (Marewski and Gigerenzer, 2012; Tversky and Kahneman, 1974). This bias frequently goes unrecognised by the individual, but may lead to mistaken conclusions and sometimes to serious error (Klein, 2005; Gunderman, 2009).
In the present study we have analysed the submissions of UKNEQAS(H) CPD participants assessing a range of representative cases, to examine the processes of decision making by individuals with varying levels of skill or experience. We have compared the submissions of morphologists arriving either at correct or incorrect diagnostic conclusions. Our analysis has revealed common patterns of approach to interpretation, but has also highlighted patterns of error shared by groups of participants. We suggest that our findings have relevance to the design of support mechanisms designed to improve the interpretation of haematological morphology.
2. Materials and Methods
2.1. Case Construction and Review
Cases were selected initially by members of the UK NEQAS(H) Morphology Scientific Advisory Group (Morphology SAG). Selection was based on blood smear quality, the range of morphological features, and the underlying diagnosis. Images were captured using a Zeiss Axio Imager M1 microscope and HRc camera (x63 Plan Apo Chromat 1.4 Oil immersion lens). At least 50 adjacent fields were manually focussed then formed into a single continuous image (photomerge function of Adobe Photoshop CS5). Post-processing included adjustment to image brightness and contrast, colour balance (Curves function) and sharpness (Unsharp mask) to ensure that reproduction matched the corresponding glass slide appearances, then images were uploaded to the viewing software (Digital SlideBox, Leica Biosystems).
2.2. Software System and Data Collection
Using the software virtual microscope as described (Burthem et al., 2005), participants were given brief clinical data, and viewed the image using magnification and navigation functions. Using a structured menu system, participants used a list of 74 features to select up to 5 morphological descriptors that they judged to best describe the blood film appearances then placed them in priority order. Participants were asked an additional single best-answer multiple choice question (most frequently “what would you do now?”); then had the option to suggest their preferred diagnosis using free-text entry.
2.3. Data Sorting and Analysis
If a single feature had a high diagnostic significance this was considered as a single element, otherwise observations reflecting the same pathological process were considered as a combined group (expressed as the mean number of selections and standard error of the mean (SEM)). A “priority score” was generated from the rank assigned: for single elements this was the rank assigned by the participant, for feature-groups this was the highest rank for any element of that group. Statistical evaluation employed GraphPad Prism software (v6.04): a comparison of feature selection or diagnosis employed contingency table analysis (Chi-square test: Fisher's exact test, two tailed analysis); priority scores for frequency of choice were compared between multiple groups using a non-parametric ANOVA test (Kruskal–Wallis test with multiple comparisons of means); for two sets of observations a two tailed Mann–Whitney test was employed. Significance is indicated in figures as follows: *p < 0.05, **p < 0.01, and ***p < 0.001.
Funding: the CPD system was funded by participant subscription.
3. Results
3.1. Participants, Cases and Software
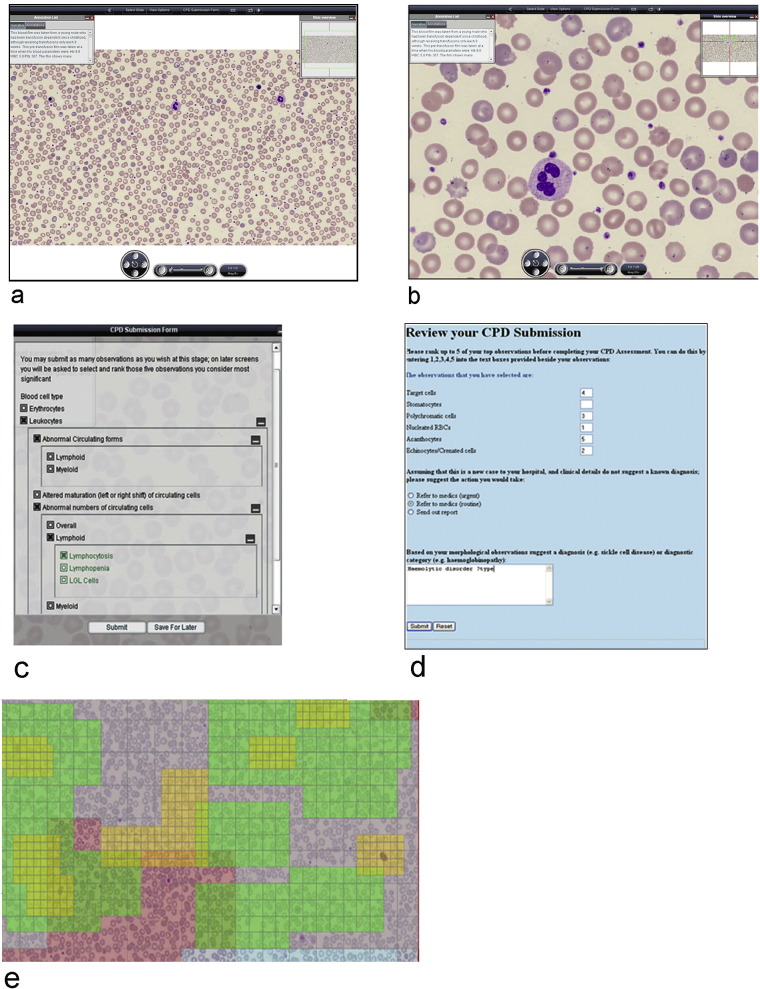
All participants were registered with the UK-NEQAS(H) Digital Morphology CPD scheme and principally comprised qualified UK Biomedical Scientists. Digital images presented in the virtual microscope software (Fig. 1a and b) were viewed by 715-1028 (mean 842) individuals with answers submitted using defined on-line criteria (Fig. 1c and d). Heat map analysis was employed in some studies; this analysis demonstrated that the users scanned the film area at low magnification before selecting specific areas for detailed examination at high magnification (Fig. 1e). This pattern is consistent with approaches to whole slide viewing previously shown by others (Raghunath et al., 2012). Five selected cases were analysed (Fig. 2a to e and Table 1).
Fig. 1.
The virtual microscope and question system. Panel a: the digital microscope interface at low power showing the case information provided (generally brief clinical details and selected values from the automated blood count), field size, and basic navigation controls. Panel b: high power view of the same image showing the magnification, resolution of cellular detail, and colour representation achieved. Panel c: heat map representation tracking the user viewing behaviour. The regions overlaid in colour represent areas viewed by the user; box size indicates the magnification used (the smallest boxes shown in yellow represent highest magnification). Panel d: morphological feature selection panel with the decision tree used by participants to select important features from the list of possible cell appearances. Panel e: answer submission panel requiring users to refine their selections by limiting their selections to a maximum of five selections most relevant to diagnosis and placing these in order of importance; this is followed by a single best answer multiple choice question and a separate free text question.
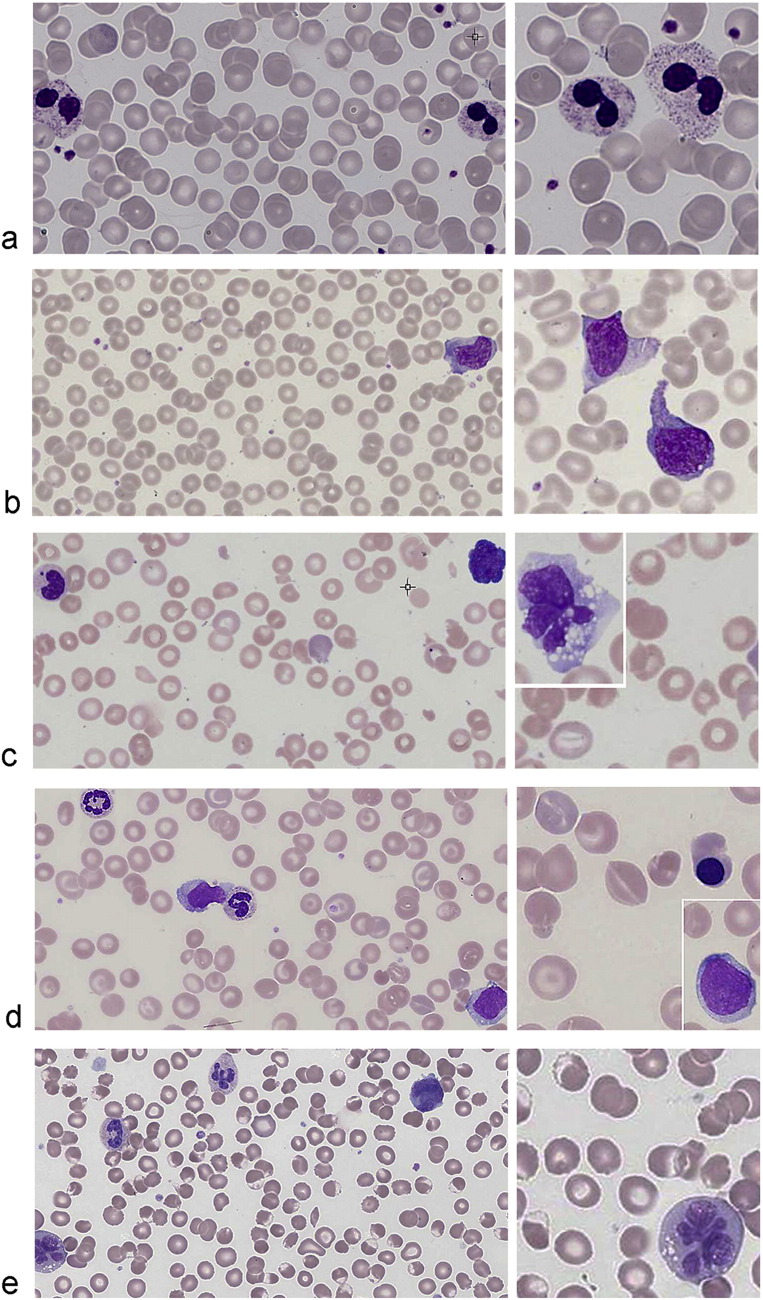
Fig. 2.
The five morphological cases analysed in the study: low power image (left) and high power image (right). Panel a: case 1, reactive lymphocytes in viral infection (EBV), showing typical abnormal polymorphic reactive T lymphocytes in an otherwise normal cellular background. Panel b: case 2, inherited Pelger–Huet disorder, showing neutrophils with typical spectacle-like bi-lobed nuclei and condensed chromatin. The neutrophil granulation and cellular background were normal making myelodysplasia less likely. Panel c: case 3, microangiopathic haemolysis, showing thrombocytopenia, keratocytes, fragmentation and general haemolysis. Reactive lymphocytes are shown at low power and in the inset panel. Panel d: case 4, haemoglobin SC disease, with target cells, contracted cells, polychromasia, nucleated erythrocytes and boat-shaped cells. There is also an acute leukaemia with primitive blast cells (inset and low power panels) and abnormal neutrophils. Panel e: case 5, oxidative haemolysis, shown principally by bite cells, but accompanied by other erythrocyte damage. Also present are lymphoid cells of adult T-cell leukaemia lymphoma, including the example with basophilic cytoplasm and typical lobulated and unfolded nuclei (inset panel), and a further example with folded convoluted nuclei visible on the low power image.
Table 1.
Cases and case characteristics of analysed group.
| Case | Total participants | Morphological syndrome | Principle diagnostic features present on film | Major diagnostic subgroups analysed | Group numbers |
|---|---|---|---|---|---|
| 1 | 715 | Reactive lymphocytes (EBV virus infection) | Reactive lymphocytes | a. Reactive lymphocytes | 460 |
| b. Neoplastic lymphocytes | 137 | ||||
| c. Reactive or neoplastic | 54 | ||||
| 2 | 1028 | Typical Pelger–Huet neutrophils (inherited Pelger–Huet anomaly) | Pelger–Huet neutrophils | a. Pelger–Huet anomaly | 584 |
| b. Myelodysplastic syndrome | 142 | ||||
| c. Reactive changes | 54 | ||||
| 3 | 747 | Microangiopathic haemolytic anaemia associated with viral infection (HIV) | Thrombocytopenia Red cell fragmentation General haemolytic features Reactive lymphocytes |
a. MAHA and viral illness | 125 |
| b. MAHA | 385 | ||||
| c. Haemolysis (other) | 157 | ||||
| 4 | 948 | Acute myeloid leukaemia with haemoglobin SC disease | Leukaemic blast cells Target erythrocytes Abnormal erythrocytes (various) |
a. Acute leukaemia diagnosed | 205 |
| b. Leukaemia not diagnosed | 268 | ||||
| c. No white cell diagnosis made | 283 | ||||
| 5 | 772 | Adult T-cell leukaemia lymphoma with oxidative haemolysis | Typical abnormal ATLL lymphocytes Changes of oxidative haemolysis affecting erythrocytes |
a. Biomedical scientists regularly reporting blood films | 505 |
| b. Biomedical scientists not reporting blood films | 58 |
3.2. Cases With a Predominant Single Morphological Feature
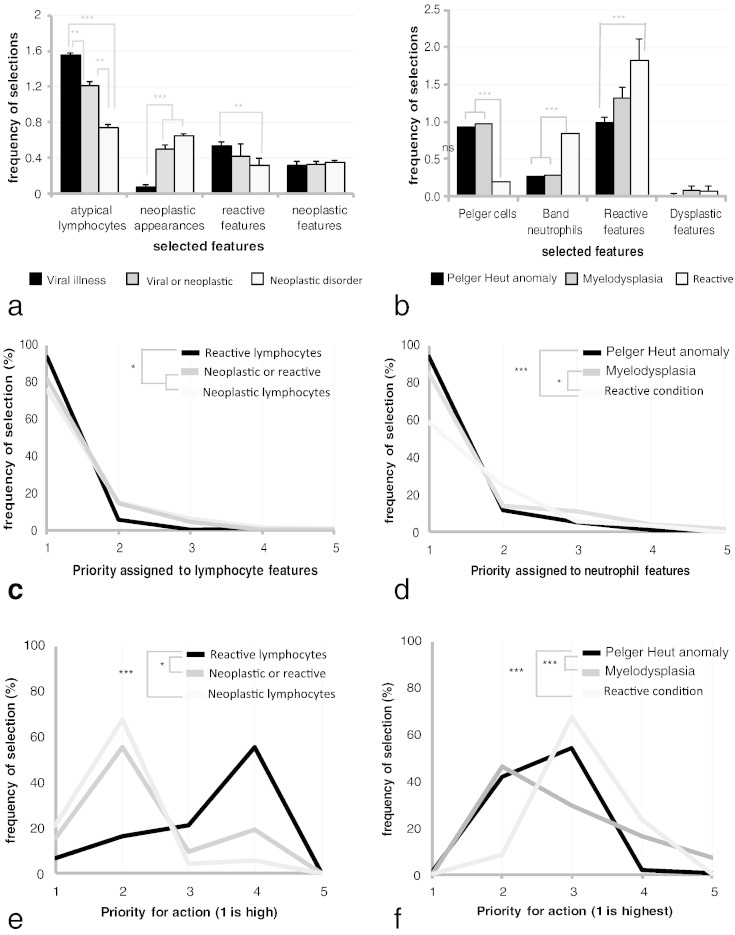
The morphological features present in cases 1 and 2 (Fig. 2a and b) affected a single cell type. Almost all participants correctly identified and prioritised the affected lineage (Fig. 3a and b). However, within that lineage the classification of the abnormal cells differed significantly between participants, and could be divided into distinct subgroups that were linked to the classification of the abnormal cell type (Table 1). For case 1, those answering the case correctly identified the abnormal cells as reactive lymphocytes, but other subgroups incorrectly reported the abnormal cells to be neoplastic, or reported the presence of both of neoplastic and reactive cells (Fig. 3c). Case 2 showed similar findings, with abnormal neutrophils being identified as the most significant feature by almost all participants. Those participants correctly interpreting the case classified the cells as having Pelger–Huet morphology, while incorrect groups selected either pseudo Pelger morphology (diagnosing myelodysplasia), or “left-shifted” morphology (assigning a reactive condition) (Fig. 3d).
Fig. 3.
Participant responses to case 1 (features of Epstein–Barr infection) and case 2 (Pelger–Huet anomaly). Panels a and b: features selected by participants for each case according to the diagnosis made. Bars represent the mean number of selections for the indicated feature or feature group (for groups, variability is indicated by bars representing SEM). Significant differences of selection frequency are indicated on the panels (Chi-square test). Panels c and d: priority score for first selected feature of each indicated morphological group divided according to the diagnosis made (1 is the highest priority and significant differences are indicated on the figure (Mann–Whitney test)). Panels e and f: priority for action ascribed to case according to diagnosis (1 is highest priority). Statistical differences between cases are indicated on the figure (ANOVA).
In addition however, morphological features affecting other lineages also were consistently reported. Those correctly diagnosing the case made the fewest additional selections. Those participants diagnosing a reactive process more frequently (but incorrectly) reported reactive changes affecting other cell lineages. Where a neoplastic disorder was diagnosed, participants selected a higher number of morphological features, but did not identify supporting evidence from other cell lineages (Fig. 3c and d). For both cases, the preferred action selected by participants was clearly linked to their morphological interpretation, and the diagnosis of neoplasia was associated with a higher perceived importance for action (Fig. 3e and f).
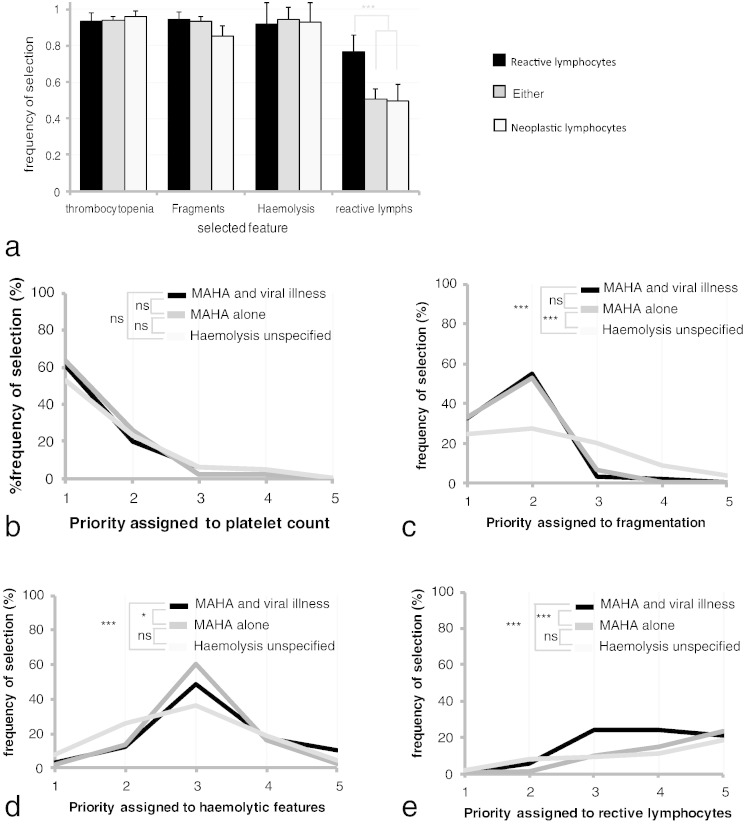
3.3. Cases Combining Complex Morphological Features
Cases 3 and 4 had greater morphological complexity. Case 3 demonstrated a microangiopathic haemolytic anaemia (MAHA) together with reactive lymphocytes, reflecting an actual pathological diagnosis of thrombotic thrombocytopenic purpura (TTP) arising during acute human immunodeficiency virus (HIV) infection (Fig. 2c and Table 1). Consistent with this increased complexity, participants reported a greater number of morphological feature selections (mean 4.75/5). Three separate diagnostic groups were identified: microangiopathic haemolysis (MAHA) with concurrent viral infection, MAHA alone, and haemolysis without specifying a microangiopathic process (Table 1). The morphological triad associated with MAHA (thrombocytopenia, red cell fragmentation, and general features of haemolysis) was consistently identified by all participant groups (Fig. 4a). The major difference lay in the priority ascribed to those features. Thus all groups agreed that thrombocytopenia was the most important aspect of the case (even for those not diagnosing MAHA) (Fig. 4b); however, where non-specific haemolysis was diagnosed a significantly lower priority was attached to erythrocyte fragmentation and higher priority to general haemolytic features (Fig. 4c and d). Lymphocyte abnormalities were reported significantly less frequently than when present as a sole abnormality (p < 0.001 vs. case 1, Chi-square test). Similarly, lymphocyte-related features were included in the suggested diagnosis more frequently than when they were a sole abnormality (p < 0.001 vs. case 1, Chi-square test) (Fig. 4a and e).
Fig. 4.
Participant responses to case 3 (microangiopathic haemolytic anaemia associated with viral illness: acute HIV infection). Panel a: major morphological feature groups shown as the mean number of selections for the indicated feature. Features are divided according to diagnosis and variability is represented by error bars (SEM). Significant differences are indicated on the figure (Chi-square test) Panels b to e: priority score given to the first selection of any feature from a feature group (1 is the highest priority), selections are divided according to the given diagnosis. Significant differences are indicated on the figure (Mann–Whitney test). Figures represent each major morphological feature groups: platelets (A), fragmentation (B), haemolytic features (C), and reactive lymphocytes (D).
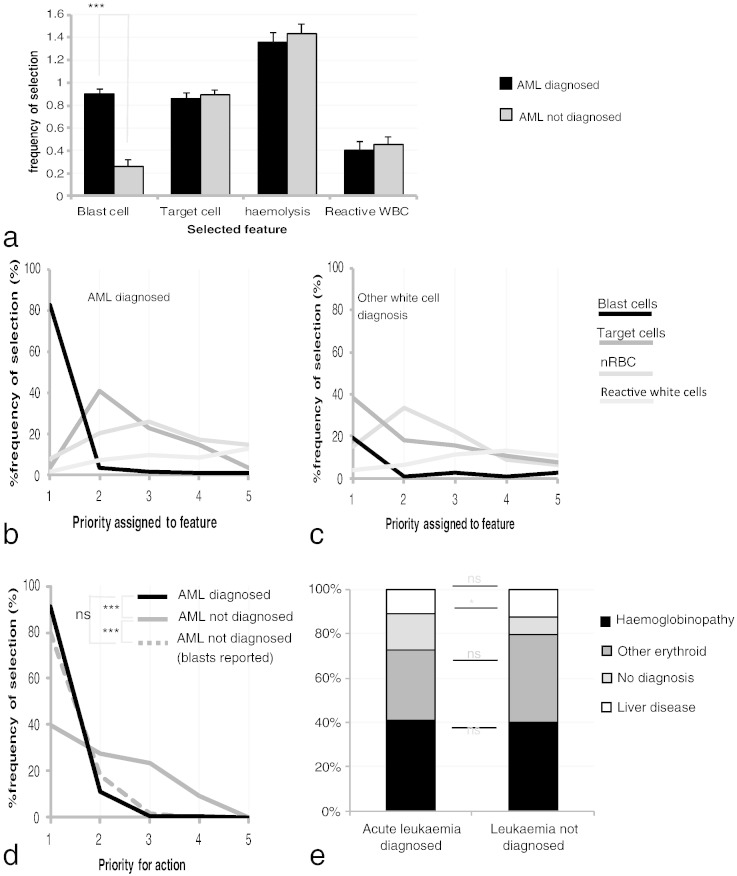
In case 4, an acute myeloid leukaemia (AML) arose in an individual with an inherited abnormal-haemoglobin (haemoglobin SC disease) (Fig. 2d and Table 1). Again there was a high use of permitted choices (4.7/5). Three diagnostic subgroups were analysed: acute leukaemia, white-cell changes noted but acute leukaemia not reported, and white cells not considered in the diagnosis (Table 1). Similar to case 3, the reported red cell features did not significantly differ between the groups (Fig. 5a), but for white cells the recognition and classification of the abnormal cells were crucial: those diagnosing acute leukaemia reported blast cells with high frequency, while their presence was not (in general) reported by those diagnosing a different white cell disorder or offering no white cell diagnosis (Fig. 5a). In terms of priority, if blast cells were reported they were assigned the highest level of importance (Fig. 5b, c, d), and this was irrespective of whether leukaemia was diagnosed (Fig. 5d) or not. There was no link between the abnormal white features reported by participants and their interpretation of red cell abnormalities (Fig. 5e).
Fig. 5.
Participant responses to case 4 (haemoglobin SC disease and acute myeloid leukaemia). Panel a: major morphological feature groups represented according to whether a diagnosis of acute leukaemia was made, bars represent mean selection number with error bars (SEM) and significant differences are indicated on the figure (Chi-square test). Panels b and c: priority score given to the first selection of any feature each feature group (1 is the highest priority); charts reflect whether acute leukaemia was diagnosed (B) or not diagnosed (C). Panel d: priority for action taken according to diagnosis suggested (1 is highest priority). Priorities indicated reflect whether acute leukaemia was diagnosed, a third broken line represents the subset of participants who recorded the presence of blast cells but did not diagnose acute leukaemia. Panel e: red cell diagnoses offered according to whether acute leukaemia was diagnosed. Statistically significant differences are indicated on the figure (Chi-square test).
3.4. Effect of Experience on Morphological on Reporting Skills
For this analysis participants were asked to specify their level of reporting responsibility. Two groups were selected for analysis: biomedical scientists who regularly issued morphological reports (R-BMS) and those who did not (NR-BMS). A complex morphological case was used: abnormal lymphoid cells of adult T-cell leukaemia lymphoma together with features of treatment-induced oxidative haemolysis (underlying glucose-6-phosphate dehydrogenase deficiency) (Fig. 2e and Table 1 case 5).
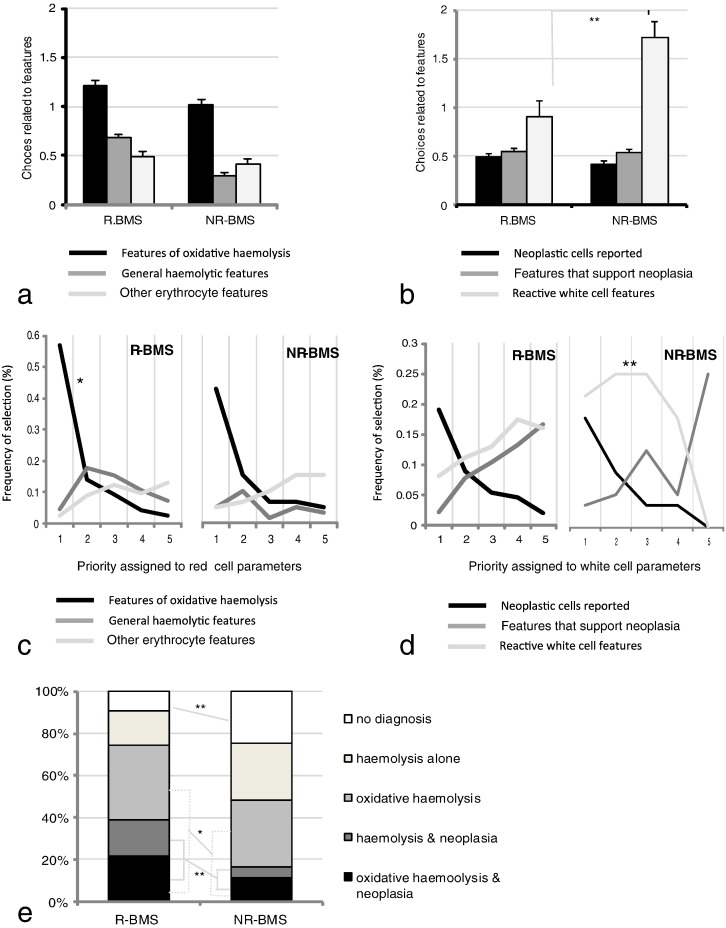
Overall the participants made a high number of morphological selections (4.9/5), reflecting the large number of features present. A correct diagnosis of lymphoid malignancy was made by 176/772 (23%), and of oxidative haemolysis by 358/772 (46%), with an entirely correct diagnosis including both disorders made by 104/772 (13%). For both red cells and white cells, R-BMS showed a trend to report features more relevant to diagnosis than NR-BMS groups, with a statistically significant difference demonstrated for white cell forms (Fig. 6a and b). For prioritisation, R-BMS again demonstrated more effective prioritisation of abnormal forms; this was significant for both white and red cell features (Figs. 6c and d). These skills were linked to a higher overall rate of diagnosis both of oxidative haemolysis and of neoplasia by the R-BMS group (Fig. 6e). However, consistent with cases 3 and 4, some participants from each group failed to identify the neoplastic white cells. Analysis suggested that (at least for the R-BMS group) the features were missed rather than being misinterpreted as reactive cells.
Fig. 6.
Analysis of case 5 (adult T cell leukaemia lymphoma and acute oxidative haemolysis) comparing responses according to the reporting experience of participants. Panels a and b: comparison of erythroid (A) or white cell (B) features selected according to the level of reporting experience; error bars represent SEM. No significant differences were detected in selections for either cell type (Chi-square test). Panels c and d: a comparison of the priority assigned to erythroid features (C) or white cell features (D), separated according to the reporting experience of participants. Significant differences are indicated on the plot (Mann–Whitney test). Panel e: comparison between the suggested diagnosis and experience of the reporter.
4. Discussion
Recognition skills depend on two related processes: the perception of familiarity or unfamiliarity (a rapid intuitive process based on previous experience), and recollection (a slower conscious recall of knowledge) (Henson et al., 1999; Wagner et al., 1998). In morphological evaluation, familiarity is likely to drive the initial recognition of abnormality, and in this study there was generally a substantial agreement on the affected cell lineage irrespective of the diagnosis reached. However, subsequent evaluation of the precise abnormality requires active recollection, and this conscious process revealed an interesting variability: for abnormal erythrocyte forms there was a considerable agreement in classification; however for white cells the classification assigned differed markedly between participants. It is probable that these differences arise from the different nature of the cell types. Abnormal erythrocytes are often present in large number and have simple forms that are often geometric — such forms are known to be rapidly and accurately recognised and classified by the human brain (Larson et al., 2009; Bar, 2003). By contrast, abnormal white cells are often infrequent and individually complex — the recognition of these subtle and highly specific features depends strongly on conscious evaluation (DiCarlo et al., 2012). However, despite the more consistent classification of erythroid cells found in this study, this did not translate to greater diagnostic accuracy, suggesting that additional factors were also involved in reaching a conclusion.
Irrespective of the nature or frequency of the abnormalities present, the data obtained through morphological assessment of a blood film is inevitably complex. Each of the five films studied showed 3000–4000 cells with many possible morphological descriptions: in the final case participants made 63 different morphological selections (of the 74 available). Deriving a conclusion from this complexity therefore presents a problem: there are simply too many cells for each to be considered individually (confirmed by the heat map analysis in this study showing that participants viewed the slide selectively). Arriving at a timely and accurate conclusion therefore depends on strategies that simplify and direct analysis. Specific conscious evaluations such as cell classification and prioritisation are central to assessment; additionally however the often unconscious mechanisms of heuristics are employed. These techniques may be highly effective (fast and frugal decision making) (Goldstein and Gigerenzer, 2002), or may introduce bias. Heuristic processes have been widely reported in other areas of medicine (Croskerry, 2013; Dawson and Arkes, 1987), and are recognised to be prevalent in image based interpretation in radiology (Gunderman, 2009), but have not been studied in haematology. Heuristic processes that are potentially relevant to haematological morphology, and their associated cognitive biases are summarised in Table 2 (Shah and Oppenheimer, 2008; Tversky and Kahneman, 1974; Blumenthal-Barby and Krieger, 2015).
Table 2.
A summary of the processes employed by morphologists to arrive at a decision and the linked forms of bias or error that may arise from these processes.
| A. Classification (knowledge-based organisation of data) | |
| Classification (simplification function) | Assigning related observations to a discreet “class”. The cells comprising that class are then considered together as a single feature: e.g. the class ‘target cells’ or a combined larger class of related observations ‘features of haemoglobinopathy’. |
| Classification (directing function) | Using the known pathological significance of an identified class to direct examination to seek evidence of a specific disease state e.g. the presence of target cells may direct a search of liver disease or haemoglobinopathy. |
| B. Simplification heuristics (techniques employed to reduce the complexity of datasets) | |
| i. Weighting | Attributing a relative importance to each individual class based on the perception of its diagnostic significance, e.g. frequency of forms belonging to that class, or the perceived pathological importance of the features. |
| ii. Elimination | Using the class assigned, and the weighting attributed to them to identify those feature considered to have low importance to diagnosis and excluding them from further analysis. |
| iii. Sources of bias | a. Bias of imaginability: complex findings are simplified by the morphologist to remove elements considered less important for diagnosis: this may not follow objective criteria. b. Inattention error: being distracted by the many elements in a complex picture and therefore failing to notice or consider specific important features. c. Associative thinking: the belief that events occurring together are likely to be linked; leading to morphologists placing unlinked observations into a single class. |
| C. Context heuristics (actively seeking other data that supports a particular decision) | |
| i. Framing | Reinforcing a diagnostic impression through the identification of supporting features or other classes that are consistent with the same pathological process. |
| ii. Availability | Interpreting features based on a perceived likelihood for a particular disease process, e.g. clinic of origin, age of patient, previous experience. |
| iii. Sources of bias | a. Framing bias and inattention error: the preconceived diagnosis is inappropriately favoured by overemphasising features that support the diagnosis and giving less weight to features that do not fit. b. Availability bias: “common things are common” so less likely explanations are given less consideration. c. Anchoring bias: becoming rooted in an idea (e.g. “this is a leukaemia”) this interpretation is then maintained even where no further evidence is present. Anchoring is often associated with “loss aversion”: observations with high potential significance (e.g. “features of possible neoplasm”) are not eliminated even where the observer considers the diagnosis unlikely. |
| D. Completion heuristics (techniques that support completion of task) | |
| i. Attribute substitution | Simplifying the question from the objective “what is the diagnosis?” to the subjective “do the features fit with my preferred diagnosis?” |
| ii. Sources of bias | Premature completion of task: when a conclusion has been reached that is deemed sufficient to stop examination (“satisficing”), this may lead to a premature conclusion before all evidence has been discovered or considered. |
The two initial cases affected a single lineage with no accompanying abnormalities. The error pattern in these cases differed from those in more complex cases. Essentially, Knowledge-based skills of recognition and classification had primary importance, and diagnosis/action was strongly linked to cell classification. However, participants additionally sought to support their decision through context heuristic processes (Table 2C). In particular, incorrect diagnoses were associated with reporting a greater number of morphological selections and with evidence of biases associated with seeking supportive context: for reactive diagnoses the use of “framing bias” led to the incorrect reporting of reactive features in other lineages, while malignant diagnoses were associated with “anchoring” to a neoplastic interpretation despite lack of supporting evidence, and with “loss aversion” where participants reported both reactive and neoplastic features on the film (Table 3a).
Table 3.
Relevant skills and sources of error or bias observed in the case series.
| A. Cases 1 and 2 (simple morphological features) | ||
| Primary skills: recognition and classification Relevant heuristic group: context | ||
| Error group | Incorrect classification. Source: Knowledge/skills based error |
Cases 1 & 2 |
| Supporting bias 1 | Overemphasis of reactive features to support a reactive diagnosis. Source: Framing bias |
Cases 1 & 2 |
| Supporting bias 2 | Favouring malignant diagnosis without supporting evidence Source: Anchoring bias and consequence bias |
Cases 1 & 2 |
| B. Cases 3 to 5 (complex morphological features) | ||
| Primary skills: recognition classification, prioritisation Relevant heuristic groups: simplification and completion | ||
| Error group | Incorrect classification. Source: Knowledge/skills based error |
Cases 4 & 5 |
| Error group | Incorrect prioritisation and interpretation. Source: Knowledge-based error |
Case 3 |
| Supporting bias 1 | Failure to report significant feature. Source: inattention error, premature completion of task |
All cases |
| Supporting bias 2 | Failure to include an observed feature in the interpretation: Source: associative thinking, attribute substitution |
All cases |
Where the digital slides presented more complex combinations of features (cases 3 to 5), the participants' analyses predominantly employed strategies that simplified the observations. The knowledge-based stratification of findings and the elimination of less important features allowed many participants to deliver more relevant interpretation. Errors related to prioritisation were observed. For example in case 3, although there was a widespread agreement on features present, some participants failed to consider the low platelet count in their interpretation or gave low priority to fragmentation, resulting in an incorrect conclusion of general haemolysis rather than the more urgent diagnosis of microangiopathic haemolysis. Significant error also arose from the application of simplification heuristics (Table 2B): “Associative thinking” led to very significant morphological features being assumed to form part of an existing class rather than having independent significance. This could have a minor effect e.g. the failure to include viral disorder in the conclusion to case 3, or major effect e.g. the failure to include leukaemia in the conclusion to case 4 even when the participants identified that blast cells were present. Biases associated with the need or desire to complete their examination were also seen (Table 2C): in cases 4 and 5, a significant group of respondents failed to report the presence of neoplastic white cells at all. These errors were likely to derive from the complexity of the features and the requirement to finish the case and move on, resulting in “inattention error” or the associated bias “premature completion of task” (Table 3).
The reporting responsibilities and experience of participants in this CPD scheme varied. However, blood film analysis is always interpretive even when the decision concerns whether (or when) to seek a colleague's help. Cases 1 and 2 clearly showed that the action taken in response to morphological appearances is tightly linked to the perceived diagnosis. Getting this process right is an important facet of post-analytical quality (iso:15189, 2012). This study shows that while cell recognition is an important part of this process, the techniques of blood film interpretation also depend on accurate use of a range of heuristic techniques. Those techniques are hugely valuable in driving effective conclusion, and the study suggests that experienced morphologists apply these unconscious techniques more accurately than inexperienced morphologists. However, biases related to heuristics are also evident. As microscope-side teaching of skills becomes less widespread, and computer-driven decision-support methods are introduced (Ceelie et al., 2007; Lee et al., 2013; Crowley et al., 2013) it is important that we actively seek to identify, understand, and address how we arrive at rapid accurate conclusions or errors (Hamilton et al., 2009).
The present study shows that simple and complex films are processed differently, and that different heuristic approaches are applied. The later cases in this series in particular had a morphological complexity that would not commonly be faced by our participant group; moreover, the image size is not equivalent to a glass slide and this may have contributed to errors. Therefore our findings may not be transferable to the day-to-day practice in all respects. Nonetheless, our data demonstrates that in many cases, the errors by participants in these cases were significantly associated with heuristic processes rather than with knowledge-base. Therefore, as well as supporting knowledge-based decisions, approaches to clinical-decision support should adopt and make use of training techniques that increase awareness of the heuristic strategies in morphological diagnosis (Crowley et al., 2013; Wegwarth et al., 2009; Murray et al., 2015). At the microscope there remains a significant role for effective decision support: automated cell-recognition systems for white cells (Rezatofighi and Soltanian-Zadeh, 2011; Meintker et al., 2013) may reduce errors associated with premature completion or inattention, but address only part of the problem: morphological evaluation effectively requires the integration of findings of complex datasets and their application to a range of different diagnostic outcomes. Tools and approaches are presently being developed in many contexts to support decisions in complex data — improving outcome requires collaborative approaches to seek their appropriate application to morphology and other fields of medical diagnosis.
Declaration of Interests
The authors have no personal, academic or financial interests to declare.
Contribution of Authors
MB and JB designed the study, analysed the data and wrote the manuscript. BDS, KH and JA contributed to the study design and interpretation and helped in the editing of the manuscript.
Acknowledgements
We would like to thank the staff at UK NEQAS(H) and the participants in the CPD scheme for their continued enthusiasm and involvement. We thank SlidePath-Leica Digital Systems for hosting the system and providing access to anonymised responses of participants. The work contained in the paper was not externally funded.
References
- Bar M. A cortical mechanism for triggering top-down facilitation in visual object recognition. J. Cogn. Neurosci. 2003;15(4):600–609. doi: 10.1162/089892903321662976. [DOI] [PubMed] [Google Scholar]
- Blumenthal-Barby J.S., Krieger H. Cognitive biases and heuristics in medical decision making: a critical review using a systematic search strategy. Med. Decis. Mak. 2015;35(4):539–557. doi: 10.1177/0272989X14547740. [DOI] [PubMed] [Google Scholar]
- Brereton M.L., B DLS, Burthem J. Review of the UK NEQAS (H) digital morphology pilot scheme for continuing professional development accessed via the internet. Int. J. Lab. Hematol. 2008;30(5):365–371. doi: 10.1111/j.1751-553X.2008.01086.x. [DOI] [PubMed] [Google Scholar]
- Burthem J., Brereton M., Ardern J. The use of digital ‘virtual slides’ in the quality assessment of haematological morphology: results of a pilot exercise involving UK NEQAS(H) participants. Br. J. Haematol. 2005;130(2):293–296. doi: 10.1111/j.1365-2141.2005.05597.x. [DOI] [PubMed] [Google Scholar]
- Ceelie H., Dinkelaar R.B., van Gelder W. Examination of peripheral blood films using automated microscopy; evaluation of Diffmaster Octavia and Cellavision DM96. J. Clin. Pathol. 2007;60(1):72–79. doi: 10.1136/jcp.2005.035402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croskerry P. From mindless to mindful practice—cognitive bias and clinical decision making. N. Engl. J. Med. 2013;368(26):2445–2448. doi: 10.1056/NEJMp1303712. [DOI] [PubMed] [Google Scholar]
- Crowley R.S., Legowski E., Medvedeva O. Automated detection of heuristics and biases among pathologists in a computer-based system. Adv. Health Sci. Educ. Theory Pract. 2013;18(3):343–363. doi: 10.1007/s10459-012-9374-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson N.V., Arkes H.R. Systematic errors in medical decision making: judgment limitations. J. Gen. Intern. Med. 1987;2(3):183–187. doi: 10.1007/BF02596149. [DOI] [PubMed] [Google Scholar]
- DiCarlo J.J., Zoccolan D., Rust N.C. How does the brain solve visual object recognition? Neuron. 2012;73(3):415–434. doi: 10.1016/j.neuron.2012.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein D.G., Gigerenzer G. Models of ecological rationality: the recognition heuristic. Psychol. Rev. 2002;109(1):75–90. doi: 10.1037/0033-295x.109.1.75. [DOI] [PubMed] [Google Scholar]
- Gunderman R.B. Biases in radiologic reasoning. AJR Am. J. Roentgenol. 2009;192(3):561–564. doi: 10.2214/AJR.08.1220. [DOI] [PubMed] [Google Scholar]
- Hamilton P.W., van Diest P.J., Williams R., Gallagher A.G. Do we see what we think we see? The complexities of morphological assessment. J. Pathol. 2009;218(3):285–291. doi: 10.1002/path.2527. [DOI] [PubMed] [Google Scholar]
- Henson R.N., Rugg M.D., Shallice T., Josephs O., Dolan R.J. Recollection and familiarity in recognition memory: an event-related functional magnetic resonance imaging study. J. Neurosci. 1999;19(10):3962–3972. doi: 10.1523/JNEUROSCI.19-10-03962.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- iso:15189 . ISO (International Organization for Standardization); 2012. Medical Laboratories — Requirements for Competence and Quality; pp. 1–53. [Google Scholar]
- Klein J.G. Five pitfalls in decisions about diagnosis and prescribing. BMJ. 2005;330(7494):781–783. doi: 10.1136/bmj.330.7494.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson C.L., Aronoff J., Sarinopoulos I.C., Zhu D.C. Recognizing threat: a simple geometric shape activates neural circuitry for threat detection. J. Cogn. Neurosci. 2009;21(8):1523–1535. doi: 10.1162/jocn.2009.21111. [DOI] [PubMed] [Google Scholar]
- Lee L.H., Mansoor A., Wood B., Nelson H., Higa D., Naugler C. Performance of CellaVision DM96 in leukocyte classification. J. Pathol. Inform. 2013;4:14. doi: 10.4103/2153-3539.114205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marewski J.N., Gigerenzer G. Heuristic decision making in medicine. Dialogues Clin. Neurosci. 2012;14(1):77–89. doi: 10.31887/DCNS.2012.14.1/jmarewski. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meintker L., Ringwald J., Rauh M., Krause S.W. Comparison of automated differential blood cell counts from Abbott Sapphire, Siemens Advia 120, Beckman Coulter DxH 800, and Sysmex XE-2100 in normal and pathologic samples. Am. J. Clin. Pathol. 2013;139(5):641–650. doi: 10.1309/AJCP7D8ECZRXGWCG. [DOI] [PubMed] [Google Scholar]
- Murray D.J., Freeman B.D., Boulet J.R., Woodhouse J., Fehr J.J., Klingensmith M.E. Decision making in trauma settings: simulation to improve diagnostic skills. Simul. Healthc. 2015;10(3):139–145. doi: 10.1097/SIH.0000000000000073. [DOI] [PubMed] [Google Scholar]
- Raghunath V., Braxton M.O., Gagnon S.A. Mouse cursor movement and eye tracking data as an indicator of pathologists' attention when viewing digital whole slide images. J. Pathol. Inform. 2012;3:43. doi: 10.4103/2153-3539.104905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rezatofighi S.H., Soltanian-Zadeh H. Automatic recognition of five types of white blood cells in peripheral blood. Comput. Med. Imaging Graph. 2011;35(4):333–343. doi: 10.1016/j.compmedimag.2011.01.003. [DOI] [PubMed] [Google Scholar]
- Shah A.K., Oppenheimer D.M. Heuristics made easy: an effort-reduction framework. Psychol. Bull. 2008;134(2):207–222. doi: 10.1037/0033-2909.134.2.207. [DOI] [PubMed] [Google Scholar]
- Tversky A., Kahneman D. Judgment under uncertainty: heuristics and biases. Science. 1974;185(4157):1124–1131. doi: 10.1126/science.185.4157.1124. [DOI] [PubMed] [Google Scholar]
- Wagner A.D., Desmond J.E., Glover G.H., Gabrieli J.D. Prefrontal cortex and recognition memory. Functional-MRI evidence for context-dependent retrieval processes. Brain. 1998;121(Pt 10):1985–2002. doi: 10.1093/brain/121.10.1985. [DOI] [PubMed] [Google Scholar]
- Wegwarth O., Gaissmaier W., Gigerenzer G. Smart strategies for doctors and doctors-in-training: heuristics in medicine. Med. Educ. 2009;43(8):721–728. doi: 10.1111/j.1365-2923.2009.03359.x. [DOI] [PubMed] [Google Scholar]
- Zhang W., Sun J., Tang X. From tiger to panda: animal head detection. IEEE Trans. Image Process. 2011;20(6):1696–1708. doi: 10.1109/TIP.2010.2099126. [DOI] [PubMed] [Google Scholar]