Abstract
Background:
A diagnosis of femoroacetabular impingement (FAI) requires careful history and physical examination, as well as an accurate and reliable radiologic evaluation using plain radiographs as a screening modality. Radiographic markers in the diagnosis of FAI are numerous and not fully validated. In particular, reliability in their assessment across health care providers is unclear.
Purpose:
To determine inter- and intraobserver reliability between orthopaedic surgeons and musculoskeletal radiologists.
Study Design:
Cohort study (diagnosis); Level of evidence, 3.
Methods:
Six physicians (3 orthopaedic surgeons, 3 musculoskeletal radiologists) independently evaluated a broad spectrum of FAI pathologies across 51 hip radiographs on 2 occasions separated by at least 4 weeks. Reviewers used 8 common criteria to diagnose FAI, including (1) pistol-grip deformity, (2) size of alpha angle, (3) femoral head-neck offset, (4) posterior wall sign abnormality, (5) ischial spine sign abnormality, (6) coxa profunda abnormality, (7) crossover sign abnormality, and (8) acetabular protrusion. Agreement was calculated using the intraclass correlation coefficient (ICC).
Results:
When establishing an FAI diagnosis, there was poor interobserver reliability between the surgeons and radiologists (ICC batch 1 = 0.33; ICC batch 2 = 0.15). In contrast, there was higher interobserver reliability within each specialty, ranging from fair to good (surgeons: ICC batch 1 = 0.72; ICC batch 2 = 0.70 vs radiologists: ICC batch 1 = 0.59; ICC batch 2 = 0.74). Orthopaedic surgeons had the highest interobserver reliability when identifying pistol-grip deformities (ICC = 0.81) or abnormal alpha angles (ICC = 0.81). Similarly, radiologists had the highest agreement for detecting pistol-grip deformities (ICC = 0.75).
Conclusion:
These results suggest that surgeons and radiologists agree among themselves, but there is a need to improve the reliability of radiographic interpretations for FAI between the 2 specialties. The observed degree of low reliability may ultimately lead to missed, delayed, or inappropriate treatments for patients with symptomatic FAI.
Keywords: femoroacetabular impingement, hip, reliability, diagnosis, radiology
Femoroacetabular impingement (FAI) is a recognized cause of hip pain in the young adult that may lead to the premature development of osteoarthritis.11 It represents a morphologic disorder that results in abnormal contact between the femoral head/neck and acetabular rim.16 While an accurate diagnosis always depends on a careful history and physical examination, a proper radiologic evaluation remains equally essential.16 Particularly, accurate and reliable interpretations of plain radiographs are the preferred modality of choice to screen for FAI, despite the availability of advanced imaging, such as computed tomography (CT) scans and magnetic resonance imaging (MRI).9
Many different plain radiographic parameters have been previously described to diagnose FAI,3 but their reliability has not been thoroughly assessed.10,14 Particularly, the literature contains limited information about the reliability of these radiographic criteria across different health care providers who must evaluate and treat the young adult with hip pain. This is important when utilizing plain radiographs to screen for FAI and to avoid delays in treatment, as patients may seek advice from different health care professionals. In 1 series, patients saw an average of 3.3 health care providers for their hip symptoms prior to their definitive diagnosis.5 Thus, it is important that accurate and reliable radiographic interpretations are not limited to a particular specialty.
We identified orthopaedic surgeons and radiologists as key specialists who have a collaborative and influential role in directing the management of patients with symptomatic FAI. The current investigation aimed to evaluate the intra- and interobserver reliability of commonly used radiographic criteria to diagnose FAI and to determine the degree of agreement between musculoskeletal radiologists and orthopaedic surgeons. We hypothesized that there would be a good level of reliability between the 2 specialties, as they often collaborate when diagnosing and treating FAI.
Materials and Methods
Overview
A summary of the methods is presented in Figure 1. This study was approved by our institutional research ethics board. Briefly, 6 reviewers, including 3 orthopaedic surgeons and 3 radiologists, independently evaluated 51 hip radiographs for the presence of FAI based on several radiographic parameters. Assessments were completed on 2 separate occasions, at least 4 weeks apart. This information was subsequently used for data analysis.
Figure 1.
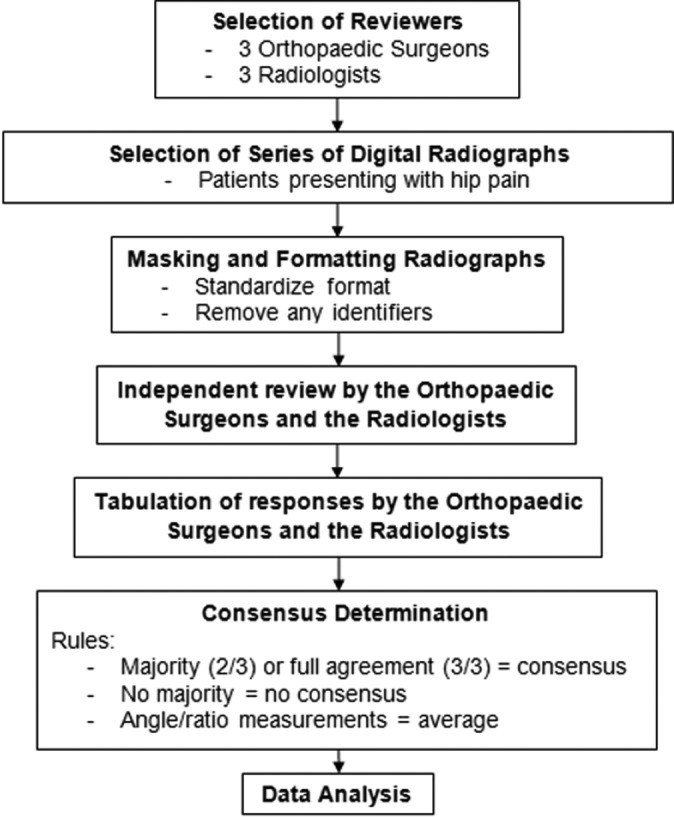
Summary of methods.
Reviewers
The panel of 6 reviewers included 3 fellowship-trained orthopaedic surgeons (1 in sports medicine and 2 in hip/knee arthroplasty) and 3 fellowship-trained musculoskeletal radiologists from our institution’s AGREE (Assessment Group for Radiographic Evaluation and Evidence) study group. All reviewers had at least 3 years of independent clinical practice and routinely evaluated plain radiographs of the hip (mean ± SD, 5.3 ± 1.9 years).
Selection of Cases
Patients were eligible for study inclusion if they presented to an adult outpatient orthopaedic clinic with a primary complaint of unilateral hip pain. Based on a review of clinical notes, these patients had a range of clinical presentations from mild to severe pain and dysfunction related to their hips. Fifty-one consecutive patients were selected for analysis and underwent an anteroposterior (AP) and frog-leg lateral hip radiographs. The number of radiographs was chosen based on a prestudy feasibility poll involving all reviewers. The AP radiographs were taken with the patient lying supine and both lower extremities internally rotated by 15°. Lateral views were obtained by flexing the patient’s knee to approximately 40° and abducting the hip to 45°.
Assessments
None of the reviewers were involved with the selection of the radiographs. All images were originally digital and uploaded for online display on a secure, password-protected adjudication platform (Global Adjudicator) in a random sequence. This Internet-based software program facilitates and streamlines the adjudication process for clinical studies. The reviewers completed their assessments of the radiographs in Global Adjudicator on 2 occasions or “batches,” at least 4 weeks apart, onto standardized data entry forms (Appendix). They were asked to determine the presence of FAI lesions based on the following radiographic features using uniform definitions: (1) pistol-grip deformity,13 (2) size of alpha angle,9 (3) femoral head-neck offset,9 (4) crossover sign abnormality,13 (5) posterior wall sign abnormality,13 (6) ischial spine sign abnormality,4 (7) coxa profunda abnormality,9 and (8) acetabular protrusion9 (Table 1). Reviewers also commented on the radiographic view that they found the most helpful.
TABLE 1.
Intersurgeon Agreementa
| Adjudication Questions | Time 1 | Time 2 | ||||
|---|---|---|---|---|---|---|
| ICC | 95% CI | ICC | 95% CI | |||
| Lower | Upper | Lower | Upper | |||
| Findings consistent with FAI? | 0.72 | 0.52 | 0.84 | 0.70 | 0.52 | 0.82 |
| Cam lesion? | 0.74 | 0.57 | 0.84 | 0.62 | 0.39 | 0.77 |
| Pistol-grip abnormality? | 0.78 | 0.63 | 0.87 | 0.81 | 0.70 | 0.89 |
| Alpha angle >50.5? | 0.77 | 0.58 | 0.88 | 0.81 | 0.69 | 0.89 |
| Size of alpha angle? | 0.66 | 0.44 | 0.80 | 0.69 | 0.51 | 0.82 |
| Offset ratio of <0.17? | 0.64 | 0.40 | 0.79 | 0.80 | 0.67 | 0.88 |
| Size of offset ratio? | 0.69 | 0.50 | 0.82 | 0.50 | 0.21 | 0.70 |
| Pincer lesion? | 0.42 | 0.11 | 0.64 | 0.28 | −0.15 | 0.56 |
| Crossover sign abnormality? | 0.55 | 0.29 | 0.72 | 0.48 | 0.17 | 0.69 |
| Posterior wall sign abnormality? | 0.49 | 0.21 | 0.69 | 0.14 | −0.37 | 0.48 |
| Ischial spine sign abnormality? | 0.75 | 0.60 | 0.85 | 0.73 | 0.56 | 0.83 |
| Coxa profunda abnormality? | 0.68 | 0.48 | 0.81 | 0.69 | 0.51 | 0.82 |
| Acetabular protrusio abnormality? | 0.26 | −0.14 | 0.54 | 0.26 | −0.18 | 0.55 |
| Mixed FAI? | 0.62 | 0.38 | 0.77 | 0.35 | −0.04 | 0.61 |
| Radiographic view most helpful? | −0.10 | −0.072 | 0.33 | 0.00 | −0.59 | 0.40 |
aBoldfaced values indicate an intraclass correlation coefficient (ICC) ≥0.61, suggesting at least good agreement. FAI, femoroacetabular impingement.
All responses were tabulated by an independent research assistant. We considered a “consensus” to have been reached for each question when 2 of the 3 reviewers within a specialty recorded the same answer. Where applicable, the consensus decision was recorded as “unsure” when the reviewers’ answers were within 1 grade of each other, such as “definitely not,” “possibly not,” and “unsure.” Finally, the decision was recorded as “no consensus” when the reviewers’ answers varied by more than 1 grade of each other.
Data Analysis
Agreement was determined using the intraclass correlation coefficient (ICC) presented with 95% CIs. A 2-way mixed and consistency model was used in SPSS (IBM, Inc) for all these calculations. Interobserver agreement was determined using the individual responses from each reviewer within the same specialty. The consensus answers were used to compare the degree of agreement between surgeons and radiologists and to determine the intrarater agreement within each specialty (ie, after 4 weeks). We applied the following guidelines to interpret the ICC8: a value of <0.4 represents poor agreement, fair for 0.4 to 0.59, good for 0.60 to 0.74, and excellent for values from 0.75 to 1.0.
Results
Overall Impression of Radiographic FAI Diagnosis
Overall, there was good within-group reliability among the orthopaedic surgeons and radiologists when establishing a radiographic diagnosis of FAI at all time points, except 1 for the radiologists (Tables 2 and 3). The radiologists had the greatest degree of agreement during the second testing (ICC = 0.74; 95% CI, 0.59-0.84) (Table 3). However, when comparing the consensus answers between groups, there was poor agreement for a FAI diagnosis (ICC batch 1 = 0.33 [95% CI, –0.17 to 0.62]; ICC batch 2 = 0.15 [95% CI, –0.50 to 0.51]) (Table 4). Within each specialty, the raters also demonstrated only poor to fair intraobserver reliability for FAI diagnosis after repeat testing of the same question over the 4-week interval (surgeons: ICC = 0.41 [95% CI, –0.03 to 0.67]; radiologists: ICC = 0.25 [95% CI, –0.32 to 0.57]) (Table 4).
TABLE 2.
Inter-radiologist Agreementa
| Adjudication Questions | Time 1 | Time 2 | ||||
|---|---|---|---|---|---|---|
| ICC | 95% CI | ICC | 95% CI | |||
| Lower | Upper | Lower | Upper | |||
| Findings consistent with FAI? | 0.59 | 0.35 | 0.76 | 0.74 | 0.59 | 0.84 |
| Cam lesion? | 0.54 | 0.27 | 0.73 | 0.69 | 0.50 | 0.81 |
| Pistol-grip abnormality? | 0.60 | 0.35 | 0.76 | 0.75 | 0.60 | 0.85 |
| Alpha angle >50.5? | 0.73 | 0.50 | 0.86 | 0.62 | 0.31 | 0.80 |
| Size of alpha angle? | 0.47 | 0.07 | 0.72 | 0.59 | 0.30 | 0.78 |
| Offset ratio of <0.17? | 0.69 | 0.49 | 0.82 | 0.69 | 0.46 | 0.83 |
| Size of offset ratio? | 0.31 | −0.22 | 0.63 | −0.04 | −0.74 | 0.41 |
| Pincer lesion? | 0.39 | 0.00 | 0.65 | 0.20 | −0.31 | 0.53 |
| Crossover sign abnormality? | 0.67 | 0.48 | 0.80 | 0.18 | −0.31 | 0.51 |
| Posterior wall sign abnormality? | 0.69 | 0.51 | 0.81 | 0.16 | −0.33 | 0.49 |
| Ischial spine sign abnormality? | 0.65 | 0.44 | 0.79 | 0.59 | 0.35 | 0.76 |
| Coxa profunda abnormality? | 0.39 | 0.02 | 0.63 | 0.26 | −0.18 | 0.55 |
| Acetabular protrusio abnormality? | 0.28 | −0.16 | 0.57 | 0.00 | −0.59 | 0.40 |
| Mixed FAI? | 0.62 | 0.39 | 0.77 | 0.34 | −0.06 | 0.60 |
| Radiographic view most helpful? | 0.33 | −0.07 | 0.60 | 0.57 | 0.31 | 0.74 |
aBoldfaced values indicate an intraclass correlation coefficient (ICC) ≥0.61, suggesting at least good agreement. FAI, femoroacetabular impingement.
TABLE 3.
Consensus Agreement Between Surgeons and Radiologistsa
| Adjudication Questions | Consensus in Time 1 | Consensus in Time 2 | ||||
|---|---|---|---|---|---|---|
| ICC | 95% CI | ICC | 95% CI | |||
| Lower | Upper | Lower | Upper | |||
| Findings consistent with FAI? | 0.33 | −0.17 | 0.62 | 0.15 | –0.50 | 0.51 |
| Cam lesion? | 0.78 | 0.61 | 0.87 | 0.74 | 0.54 | 0.85 |
| Pistol-grip abnormality? | 0.27 | −0.28 | 0.58 | 0.35 | −0.14 | 0.63 |
| Alpha angle >50.5? | 0.55 | 0.21 | 0.74 | 0.47 | 0.07 | 0.70 |
| Size of alpha angle? | 0.70 | 0.48 | 0.83 | 0.82 | 0.61 | 0.90 |
| Offset ratio of <0.17? | 0.31 | −0.22 | 0.60 | 0.45 | 0.04 | 0.69 |
| Size of offset ratio? | 0.51 | 0.14 | 0.72 | 0.70 | 0.47 | 0.83 |
| Pincer lesion? | 0.30 | −0.23 | 0.60 | −0.10 | −0.92 | 0.37 |
| Crossover sign abnormality? | 0.44 | 0.01 | 0.68 | 0.60 | 0.30 | 0.77 |
| Posterior wall sign abnormality? | 0.39 | −0.07 | 0.65 | 0.34 | −0.16 | 0.62 |
| Ischial spine sign abnormality? | 0.40 | −0.06 | 0.66 | 0.65 | 0.39 | 0.80 |
| Coxa profunda abnormality? | 0.63 | 0.35 | 0.79 | 0.27 | −0.28 | 0.59 |
| Acetabular protrusio abnormality? | 0.55 | 0.21 | 0.74 | −0.06 | −0.86 | 0.39 |
| Mixed FAI? | 0.67 | 0.42 | 0.81 | 0.57 | 0.25 | 0.76 |
| Radiographic view most helpful? | −0.29 | −1.26 | 0.27 | 0.00 | −0.75 | 0.43 |
aBoldfaced values indicate an intraclass correlation coefficient (ICC) ≥0.61, suggesting at least good agreement. FAI, femoroacetabular impingement.
TABLE 4.
Intraobserver Consensus Agreementa
| Adjudication Questions | Surgeons | Radiologists | ||||
|---|---|---|---|---|---|---|
| ICC | 95% CI | ICC | 95% CI | |||
| Lower | Upper | Lower | Upper | |||
| Findings consistent with FAI? | 0.41 | −0.03 | 0.67 | 0.25 | −0.32 | 0.57 |
| Cam lesion? | 0.86 | 0.76 | 0.92 | 0.72 | 0.50 | 0.84 |
| Pistol-grip abnormality? | 0.01 | −0.73 | 0.44 | 0.68 | 0.44 | 0.82 |
| Alpha angle >50.5? | 0.19 | −0.43 | 0.54 | 0.42 | −0.01 | 0.67 |
| Size of alpha angle? | 0.84 | 0.72 | 0.91 | 0.91 | 0.84 | 0.95 |
| Offset ratio of <0.17? | 0.40 | −0.06 | 0.66 | 0.71 | 0.49 | 0.83 |
| Size of offset ratio? | 0.82 | 0.68 | 0.90 | −0.04 | −0.82 | 0.41 |
| Pincer lesion? | 0.70 | 0.48 | 0.83 | −0.13 | −0.98 | 0.36 |
| Crossover sign abnormality? | 0.29 | −0.25 | 0.59 | 0.26 | −0.30 | 0.58 |
| Posterior wall sign abnormality? | 0.20 | −0.40 | 0.54 | 0.48 | 0.08 | 0.70 |
| Ischial spine sign abnormality? | 0.55 | 0.20 | 0.74 | 0.80 | 0.65 | 0.89 |
| Coxa profunda abnormality? | 0.02 | −0.72 | 0.44 | 0.52 | 0.16 | 0.73 |
| Acetabular protrusio abnormality? | 0.10 | −0.57 | 0.49 | −0.03 | −0.81 | 0.41 |
| Mixed FAI? | 0.15 | −0.49 | 0.52 | 0.45 | 0.04 | 0.69 |
| Radiographic view most helpful? | 0.00 | −0.75 | 0.43 | 0.20 | −0.40 | 0.54 |
aBoldfaced values indicate an intraclass correlation coefficient (ICC) ≥0.61, suggesting at least good agreement. FAI, femoroacetabular impingement.
Reliability of Different FAI Parameters
Tables 2 to 4 summarize the reliabilities of the different radiographic parameters used in this study. Among the orthopaedic surgeons, reliability was highest for detecting pistol-grip deformities (ICC = 0.81; 95% CI, 0.70-0.89) and abnormal alpha angles (ICC = 0.81; 95% CI, 0.69-0.89) (Table 2). By comparison, the radiologists demonstrated the highest reliability for pistol-grip deformities (ICC = 0.75; 95% CI, 0.60-0.85).
Both the orthopaedic surgeons and radiologists demonstrated only poor to fair within-group reliability when establishing a diagnosis of pincer FAI lesions (Tables 2 and 3). They also demonstrated poor to no agreement between groups for pincer lesions (Table 4). This was in contrast to cam or mixed-type lesions, where each group demonstrated at least a good degree of agreement on 1 testing.
In addition, both within- and between-group agreements were consistently low when deciding on which radiographic view was the most helpful for diagnosis. This reliability remained low within each group over time (Table 4).
Discussion
The current investigation demonstrated a wide range of agreement within the 2 groups of physicians. However, it was particularly interesting that there was only a poor amount of agreement between the 2 specialties when establishing a diagnosis of FAI, which was in contrast to the higher interobserver reliability within each specialty. In general, these results may suggest that surgeons and radiologists agree among themselves, but an accurate diagnosis between specialties remains less reproducible.
The results of the present study appear to coincide with a study by Carlisle et al.7 They found that a group of physicians with varying clinical experience (1 orthopaedic fellow, 2 orthopaedic residents, and 2 attending musculoskeletal physiatrists)—none of whom had an exclusive practice focused on hips—could reliably perform radiographic hip measurements on an individual basis, but demonstrated limited agreement between raters. It is unclear why there was a general lack of agreement between the surgeons and radiologists. One possible explanation is that orthopaedic surgeons are becoming increasingly more cognizant of the clinical diagnosis of FAI and obtain more exposure and practice with the associated radiographic measurements. In a systematic review of FAI-related publications between 2005 and 2010, 66% of the 298 studies arose from the orthopaedic literature, compared with 15% from radiology.2 Another indication that experience may have affected our results was when the degree of agreement among the radiologists improved from fair (ICC = 0.59; 95% CI, 0.35-0.76) to good (ICC = 0.74; 95% CI, 0.59-0.84) after 2 tests (Table 2) when establishing an FAI diagnosis.
These findings are important because they indicate a need for improvement in radiographic hip measurements between orthopaedic surgeons and musculoskeletal radiologists, especially since plain radiographs remain one of the most important initial diagnostic imaging studies for hip impingement.13 Poor reliability can ultimately influence the care of patients with symptomatic FAI due to missed, delayed, or inappropriate diagnoses and treatments. Although the current study has demonstrated limitations with the use of plain radiographs, they stress the importance of combining a thorough history and physical examination with appropriate diagnostic imaging to arrive at the correct diagnosis. Uncertainty regarding the origin of a patient’s “hip pain” can be further investigated with intra-articular anesthetic injections6 and advanced imaging, such as CT or MRI.
The current investigation also demonstrated that there was only a poor to no amount of agreement between the surgeons and radiologists when identifying pincer FAI lesions. This may be a consequence of the poor validity of individual radiographic measurements. Anderson et al1 previously showed that coxa profunda was a nonspecific finding and did not relate to acetabular overcoverage (pincer lesion). Similar findings were observed by Nepple et al.15 In addition, Zaltz et al20 found that the crossover sign overestimated true acetabular retroversion. They concluded that acetabular retroversion remained difficult to diagnose.20 These results have implications not only for the diagnosis of FAI but also for the surgical management of pincer lesions. Unreliable radiographic evaluations may contribute to difficulties with determining the appropriate limits of acetabular rim trimmings. Further research and strategies to improve the accuracy and reliability of diagnosing pincer FAI lesions are needed with inputs from orthopaedic surgeons and radiologists. Additional radiographic measures, such as the center-edge angle,12,17 may be helpful, although this was not assessed in the current investigation.
A limitation of the study includes the variability in radiographic technique, which may have occurred despite attempts to standardize the images. This may have affected the results because the projected hip morphology depends on pelvic positioning during radiographic acquisition,18,19 which may be more relevant in pincer-type impingement.
Conclusion
There is a need to improve the degree of agreement between orthopaedic surgeons and musculoskeletal radiologists in the radiographic interpretation of FAI. The observed degree of low reliability may ultimately lead to missed, delayed, or inappropriate treatments for patients with symptomatic FAI. Additional efforts to enhance reliability may be obtained through education, clarifying the radiographic hip measurements, or integrating the radiographic criteria into current imaging software.7 Future research should re-evaluate inter- and intraobserver reliability after focused educational and training initiatives.
APPENDIX
Sample Data Entry Form
| Please indicate the patient label: ______________ | |||||
| Please answer the following questions for the cases presented. | |||||
| 1. Does this patient have radiographic findings consistent with femoroacetabular impingement? | |||||
| □ Definitely Not | □ Possibly Not | □ Unsure | □ Possibly Yes | □ Definitely Yes | |
| 2. Is a CAM lesion present? | |||||
| □ Yes | □ No | ||||
| a) Please indicate whether a pistol-grip abnormality is present? | |||||
| □ Definitely Not | □ Possibly Not | □ Unsure | □ Possibly Yes | □ Definitely Yes | |
| b) Please indicate whether an alpha angle >50.5° is present? | |||||
| □ Definitely Not | □ Possibly Not | □ Unsure | □ Possibly Yes | □ Definitely Yes | |
| Please indicate the alpha angle present: ___________ degrees | |||||
| c) Please indicate whether an offset ratio of < 0.17 is present? | |||||
| □ Definitely Not | □ Possibly Not | □ Unsure | □ Possibly Yes | □ Definitely Yes | |
| Please indicate the offset ratio present: __________ | |||||
| 3. Is a PINCER lesion present? | |||||
| □ Yes | □ No | ||||
| a) Please indicate whether a crossover sign abnormality is present? | |||||
| □ Definitely Not | □ Possibly Not | □ Unsure | □ Possibly Yes | □ Definitely Yes | |
| b) Please indicate whether a posterior wall sign abnormality is present? | |||||
| □ Definitely Not | □ Possibly Not | □ Unsure | □ Possibly Yes | □ Definitely Yes | |
| c) Please indicate whether an ischial spine sign abnormality is present? | |||||
| □ Definitely Not | □ Possibly Not | □ Unsure | □ Possibly Yes | □ Definitely Yes | |
| d) Please indicate whether a coxa profunda abnormality is present? | |||||
| □ Definitely Not | □ Possibly Not | □ Unsure | □ Possibly Yes | □ Definitely Yes | |
| e) Please indicate whether an acetabular protrusio abnormality is present? | |||||
| □ Definitely Not | □ Possibly Not | □ Unsure | □ Possibly Yes | □ Definitely Yes | |
| 4. Is this a case of mixed femoroacetabular impingement? | |||||
| □ Definitely Not | □ Possibly Not | □ Unsure | □ Possibly Yes | □ Definitely Yes | |
| 5. Which radiographic view was most helpful in making your decisions? | |||||
| □ Neither view | □ Anteroposterior (AP) | □ Frog lateral | □ Both views | ||
Footnotes
The authors have reported the following potential conflicts of interest or source of funding: M.B. is partially funded by a Canada Research Chair.
References
- 1. Anderson LA, Kapron AL, Aoki SK, Peters CL. Coxa profunda: is the deep acetabulum overcovered? Clin Orthop Relat Res. 2012;470:3375–3382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ayeni OR, Chan K, Al-Asiri J, et al. Sources and quality of literature addressing femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2013;21:415–419. [DOI] [PubMed] [Google Scholar]
- 3. Beall DP, Sweet CF, Martin HD, et al. Imaging findings of femoroacetabular impingement syndrome. Skeletal Radiol. 2005;34:691–701. [DOI] [PubMed] [Google Scholar]
- 4. Beaulé PE, Allen DJ, Clohisy JC, Schoenecker P, Leunig M. The young adult with hip impingement: deciding on the optimal intervention. J Bone Joint Surg Am. 2009;91:210–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burnett RS, Della Rocca GJ, Prather H, Curry M, Maloney WJ, Clohisy JC. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006;88:1448–1457. [DOI] [PubMed] [Google Scholar]
- 6. Byrd JW, Jones KS. Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, and intra-articular injection in hip arthroscopy patients. Am J Sports Med. 2004;32:1668–1674. [DOI] [PubMed] [Google Scholar]
- 7. Carlisle JC, Zebala LP, Shia DS, et al. Reliability of various observers in determining common radiographic parameters of adult hip structural anatomy. Iowa Orthop J. 2011;31:52–58. [PMC free article] [PubMed] [Google Scholar]
- 8. Cicchetti D V. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6:284–290. [Google Scholar]
- 9. Clohisy JC, Carlisle JC, Beaulé PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90 (suppl 4):47–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Clohisy JC, Carlisle JC, Trousdale R, et al. Radiographic evaluation of the hip has limited reliability. Clin Orthop Relat Res. 2009;467:666–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112–120. [DOI] [PubMed] [Google Scholar]
- 12. Kutty S, Schneider P, Faris P, et al. Reliability and predictability of the centre-edge angle in the assessment of pincer femoroacetabular impingement. Int Orthop. 2012;36:505–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Maheshwari A V, Malik A, Dorr LD. Impingement of the native hip joint. J Bone Joint Surg Am. 2007;89:2508–2518. [DOI] [PubMed] [Google Scholar]
- 14. Mast NH, Impellizzeri F, Keller S, Leunig M. Reliability and agreement of measures used in radiographic evaluation of the adult hip. Clin Orthop Relat Res. 2011;469:188–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nepple JJ, Lehmann CL, Ross JR, Schoenecker PL, Clohisy JC. Coxa profunda is not a useful radiographic parameter for diagnosing pincer-type femoroacetabular impingement. J Bone Joint Surg Am. 2013;95:417–423. [DOI] [PubMed] [Google Scholar]
- 16. Parvizi J, Leunig M, Ganz R. Femoroacetabular impingement. J Am Acad Orthop Surg. 2007;15:561–570. [DOI] [PubMed] [Google Scholar]
- 17. Philippon MJ, Wolff AB, Briggs KK, Zehms CT, Kuppersmith DA. Acetabular rim reduction for the treatment of femoroacetabular impingement correlates with preoperative and postoperative center-edge angle. Arthroscopy. 2010;26:757–761. [DOI] [PubMed] [Google Scholar]
- 18. Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;(407):241–248. [DOI] [PubMed] [Google Scholar]
- 19. Tannast M, Zheng G, Anderegg C, et al. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190. [DOI] [PubMed] [Google Scholar]
- 20. Zaltz I, Kelly BT, Hetsroni I, Bedi A. The crossover sign overestimates acetabular retroversion. Clin Orthop Relat Res. 2013;471:2463–2470. [DOI] [PMC free article] [PubMed] [Google Scholar]


