Abstract
Background:
Many studies have compared the diagnostic capabilities of low-field magnetic resonance imaging (MRI) scanners to high-field MRI scanners; however, few have evaluated the low-field MRI diagnoses compared with intraoperative findings.
Purpose:
To determine the accuracy and sensitivity of low-field MRI scanners in diagnosing lesions of the rotator cuff and glenoid labrum.
Study Design:
Cohort study (diagnosis); Level of evidence, 3.
Methods:
Over a 2-year period, MRI examinations without intra-articular contrast were performed on 79 patients for shoulder pathologies using an in-office 0.2-T extremity scanner. The MRI examinations were read by board-certified, musculoskeletal fellowship–trained radiologists. All patients underwent shoulder arthroscopy performed by a single sports fellowship–trained orthopaedic surgeon within a mean time of 56 days (range, 8-188 days) after the MRI examination. The mean patient age was 54 years (range, 18-81 years). Operative notes from the shoulder arthroscopies were then retrospectively reviewed by a single blinded observer, and the intraoperative findings were compared with the MRI reports.
Results:
For partial-thickness rotator cuff tears, the sensitivity, specificity, positive predictive value, and negative predictive value were 85%, 89%, 79%, and 92%, respectively. For full-thickness rotator cuff tears, the respective values were 97%, 100%, 100%, and 98%. For anterior labral lesions, the values were 86%, 99%, 86%, and 99%, and for superior labral anterior-posterior (SLAP) lesions, the values were 20%, 100%, 100%, and 79%, respectively.
Conclusion:
Low-field MRI is an accurate tool for evaluation of partial- and full-thickness rotator cuff tears; however, it is not effective in diagnosing SLAP lesions. More information is needed to properly assess its ability to diagnose anterior and posterior labral lesions.
Keywords: low-field MRI, rotator cuff, glenoid labrum
Shoulder injuries are a common source of pain and disability. In 2010, more than 11 million physician visits were made for primary shoulder problems in the United States.21 Pain in the shoulder is often the result of injury to the rotator cuff or glenoid labrum, and, if the damage is significant enough, surgical intervention may be required.4,9 While radiographs and physical examinations are useful tools in diagnosing shoulder injuries, magnetic resonance imaging (MRI) scans continue to be the most effective diagnostic tool to evaluate the extent of soft tissue shoulder pathology.9
Improvements in MRI technology have allowed for a wider range of scanners, each with their own advantages and disadvantages. This has sparked debates regarding which scanners are the most accurate and cost efficient. There is particular interest in the effectiveness of low-field extremity scanners in comparison with their high-field counterparts. Extremity scanners allow for lower costs, less space, and easier installation in an office setting. The open nature of extremity scanners also provides better accommodation for claustrophobic patients.1,6,13 On the other hand, low-field scanners have lower signal-to-noise ratio, lower contrast, and lower resolution, which make it difficult to match the image quality of a high-field MRI.6,13,33 Increasing scan duration can sufficiently improve image quality, although doing so also increases the likelihood of motion artifacts.3,6,13,33
Previous studies have shown mixed results when comparing low- and high-field MRI images of the shoulder. A number of studies have shown no significant difference in interpretation between low- and high-field images; however, the evidence was not conclusive.1,18,24,25 A study by Tung et al28 showed decreased accuracy when attempting to identify superior labrum anterior and posterior (SLAP) lesions on low-field MRIs. Magee et al15 concluded that high-field MRI allowed more accurate predictions for both rotator cuff tears and labral tears.
When compared with surgical findings, the use of low-field extremity MRI scanners for identifying rotator cuff pathology has been promising (sensitivity, 89%-90%; specificity, 93%-100%); however, it has been found to be less reliable for identifying pathology of the glenoid labrum (sensitivity, 55%-89%; specificity, 95%-100%).24,35 These studies are not without limitations. Both studies evaluated data from both open and arthroscopic surgical procedures, which does not control for differences between the diagnostic capabilities of these 2 techniques. In particular, some tears of the labrum may only be visible using arthroscopy.20 The studies also compared multiple surgeons, which produces potential issues regarding interobserver reliability, and did not compare differences between partial- and full-thickness rotator cuff tears or between anterior, posterior, and superior labral lesions.
The purpose of this study was to investigate the effectiveness of low-field MRI for detecting lesions of the posterosuperior rotator cuff and the labrum compared with arthroscopic findings.
Materials and Methods
This retrospective study was conducted for patients who had a standard low-field shoulder MRI performed between December 3, 2008, and December 10, 2010. MRIs were ordered after history, physical examination, and radiographs primarily concerning rotator cuff pathology, acromioclavicular joint separation, and calcific tendinitis. Patients were also indicated for MRI if they failed a period of conservative management and the history and physical and radiographic examinations were inconclusive regarding a diagnosis. When there was clear indication for isolated labral pathology, given a history of traumatic dislocation with 2+ instability on load and shift examination as well as apprehension with a positive Jobe test, patients were referred to outside facilities for MR arthrograms and were excluded from the study. If a patient’s insurance provider did not authorize a low-field MRI, they were referred to an outside facility with a high-field scanner and were excluded from the study. Patients with a previous history of surgery on the affected shoulder were also excluded. Additionally, 1 patient was excluded because the time between his/her MRI and surgery was 230 days. This was done to decrease the likelihood that a new injury was sustained to a shoulder following MRI examination.
The resulting population consisted of 79 patients. There were 52 males (66%) and 27 females (34%), with a mean age of 54 years (range, 18-81 years) at the time of the MRI. A total of 47 patients (59%) had the right shoulder affected, and 32 patients (41%) had the left shoulder affected. All patients had arthroscopic shoulder surgery within a mean of 56 days (range, 8-188 days) after the MRI, and the MRI readings were available during the operations. Arthroscopic surgeries were performed by a single, board-certified orthopaedic surgeon fellowship trained in sports medicine with more than 17 years of experience in sports medicine.
Magnetic Resonance Imaging
An MRI of the shoulder was performed on a 0.2-T extremity scanner utilizing a dedicated shoulder coil (E-scan Opera; Esaote). The gradient magnetic fields for the system operated at 20 mT/m and have a slew rate of 25 mT/m/ms. The MRI scanner was owned and operated by our institution and was authorized by all insurance providers except for Medicare at the time of the study.
Each patient signed an informed consent form and was screened by the MRI technician for safety. The MRI technician placed each patient’s arm in the supine position, with the shoulder at neutral (Figure 1). The following 2-dimensional acquisitions were obtained: proton density (PD)–weighted oblique coronal and oblique sagittal planes, T2-weighted fast spin echo (FSE) oblique coronal and oblique axial planes, gradient echo (GRE) oblique axial plane, and short tau inversion recovery (STIR) oblique coronal plane. No 3-dimensional sequences were utilized. The average imaging time was approximately 45 minutes, and the imaging parameters are displayed in Table 1.
Figure 1.
Patient positioned in the E-Scan Opera Esaote 0.2-T scanner with left arm in the supine position and the shoulder at neutral.
TABLE 1.
MRI Parameters at 0.2 Ta
| Type of MR Image | TE, ms | Thickness, mm | Intersection Gap, mm | FOV, cm | Matrix | Voxel Size, mm3 | NEX |
|---|---|---|---|---|---|---|---|
| PD-weighted oblique coronal | 26 | 3.5 | 1 | 20 | 512 × 512 | 53.4 | 1 |
| PD-weighted oblique sagittal | 26 | 4 | 1 | 20 | 512 × 512 | 61.0 | 1 |
| T2-weighted FSE oblique coronal | 90 | 3.5 | 1 | 20 | 256 × 256 | 213.6 | 1 |
| T2-weighted FSE axial | 90 | 4 | 1 | 20 | 256 × 256 | 244.1 | 1 |
| GRE axial | 16 | 4 | 1 | 18 | 512 × 512 | 53.4 | 1 |
| STIR oblique coronalb | 25 | 3.5 | 1 | 20 | 256 × 256 | 213.6 | 3 |
aRepetition time (TR) varied by patient. FOV, field of view; FSE, fast spin echo; GRE, gradient echo; MRI, magnetic resonance imaging; NEX, number of excitations; PD, proton density; STIR, short tau inversion recovery; TE, echo time.
bInversion time (TI) = 75 ms.
Interpretation of the MR Images
Each image was read in an independent prospective manner by 1 of 3 board-certified radiologists with MR musculoskeletal fellowship training. One radiologist had more than 22 years of experience reading musculoskeletal MR images and the other 2 had more than 8 years of experience. The radiologists were provided with basic demographic information, including the patient’s date of birth, sex, name, concerning pathology, and relevant symptoms presented in the initial history and examination.
Surgical Technique
For all shoulders, the glenohumeral and subacromial spaces were entered and evaluated through a posterior viewing portal with the patients in the lateral decubitus position with the operative extremity in 10 pounds of balanced suspension. Full examination of the proximal biceps tendon, humeral head, glenoid, anterior labrum, superior labrum, posterior labrum, supraspinatus tendon, subscapularis tendon, anterior superior triangle, posterior inferior axillary recess, and middle and inferior glenohumeral ligaments were performed and dictated in the operative report. The surgeon classified rotator cuff tears and labral lesions according to guidelines set forth by Snyder26 and Snyder et al.27
Data Collection
The MRI readings and operative reports were retrospectively evaluated, and data were compiled by a single blinded observer who had no involvement in the preoperative, intraoperative, or postoperative patient encounters. The MRI readings were compared with the intraoperative arthroscopy findings as dictated in the operative reports, and statistical analyses were performed. The terms tendinosis, tendinopathy, fraying, fibrillation, degeneration, attenuation, fringe, and scuffing were not categorized as tears in this study.
Statistical Analysis
Magnetic resonance imaging readings were compared with surgical findings to identify true positive, true negative, false positive, and false negative pathologies. True positive was defined as a tear identified on MRI and confirmed by surgical findings. True negative was defined as a nontear identified on MRI and confirmed by surgical findings. False positive was defined as a tear identified on MRI that was not confirmed by surgical findings. False negative was defined as a nontear identified on MRI that was not confirmed by surgical findings. Sensitivity, specificity, positive predictive value, and negative predictive value were calculated according to Table 2.
TABLE 2.
Relationships Among Statistical Terms
| Sensitivity = ∑ True positive/(∑ True positive + ∑ False negative) |
| Specificity = ∑ True negative/(∑ True negative + ∑ False positive) |
| Positive predictive value = ∑ True positive/(∑ True positive + ∑ False positive) |
| Negative predictive value = ∑ True negative/(∑ True negative + ∑ False negative) |
Results
Based on the gold standard of arthroscopic evaluation of shoulders, we found a total of 26 partial-thickness rotator cuff tears, 32 full-thickness rotator cuff tears, 7 anterior labral lesions, no posterior labral lesions, and 20 SLAP lesions. There were 10 patients (13%) without a rotator cuff tear or labral lesion and 26 patients (33%) with both. Table 3 summarizes the sensitivity, specificity, positive predictive value, and negative predictive value for the low-field MRI readings of the rotator cuff and glenoid labrum.
TABLE 3.
MRI Findings Compared With Arthroscopic Findings (N = 79 patients)a
| True Positive | True Negative | False Positive | False Negative | Sensitivity, % | Specificity, % | Positive Predictive Value, % | Negative Predictive Value, % | |
|---|---|---|---|---|---|---|---|---|
| Partial-thickness rotator cuff tear | 22 | 47 | 6 | 4 | 85 | 89 | 79 | 92 |
| Full-thickness rotator cuff tear | 31 | 47 | 0 | 1 | 97 | 100 | 100 | 98 |
| Anterior labral lesion | 6 | 71 | 1 | 1 | 86 | 99 | 86 | 99 |
| Posterior labral lesion | 0 | 78 | 1 | 0 | N/Ab | 99 | 0b | 100 |
| SLAP lesion | 4 | 59 | 0 | 16 | 20 | 100 | 100 | 79 |
aMRI, magnetic resonance imaging; N/A, not applicable; SLAP, superior labral anterior-posterior.
bNo posterior labral lesions were identified during arthroscopy.
Discussion
Low-field MRI scanners have many logistical benefits. They require less space, are convenient for patients in the office setting, and are less expensive to purchase. Their open nature has been shown to reduce the incidence of claustrophobia, and newer extremity coils and software have been designed to improve image quality. Yet, few studies exist to show whether their logistical benefits justify the lower resolution magnets associated with low-field MRI. In this study, we sought to assess low-field MRI reads to the gold standard of shoulder diagnosis—arthroscopy.
The low-field scanner used in this study was a good predictor of rotator cuff tears, with higher accuracy for full-thickness tears (sensitivity, 97%; specificity, 100%) than partial-thickness tears (sensitivity, 85%; specificity, 89%). This supports previous studies comparing low-field MRIs to surgical findings for rotator cuff tears (sensitivity, 89%-90%; specificity, 93%-100%).24,35 These results are also comparable with studies that used mid- and high-field MRIs to evaluate partial-thickness (sensitivity, 0%-92% ; specificity, 85%-99%) and full-thickness rotator cuff tears (sensitivity, 56%-100%; specificity, 73%-99%).2,9,22,23,32 It is worth noting that the lower sensitivities and specificities of these studies are likely due to limitations in the study protocols. In some cases, the MRIs were not read by musculoskeletal fellowship–trained radiologists, and some lower values are representative of individual observers and not indicative of larger trends. It is more useful to compare our findings with the upper limits of these ranges.
The results suggest that low-field MRIs are an excellent indicator of full-thickness rotator cuff tears (Figure 2), as there was only 1 false negative diagnosed as a partial-thickness tear. This is an important finding because distinguishing between partial- and full-thickness tears can affect the treatment plan of a patient. While identification of partial-thickness tears was less reliable, it was still sufficient enough to aid in the clinical management. Five of the 6 false positives were found to be normal at the time of surgery, and 3 of the 4 false negatives were read as either reactive changes due to calcific tendinitis or tendinosis and tendinopathy. Even using high-field MRIs, it is not uncommon to have difficulty distinguishing low-grade partial-thickness tears from tendinosis and tendinopathy and high-grade tears from full-thickness tears.2,32 All these patients trialed conservative management prior to surgical intervention.
Figure 2.
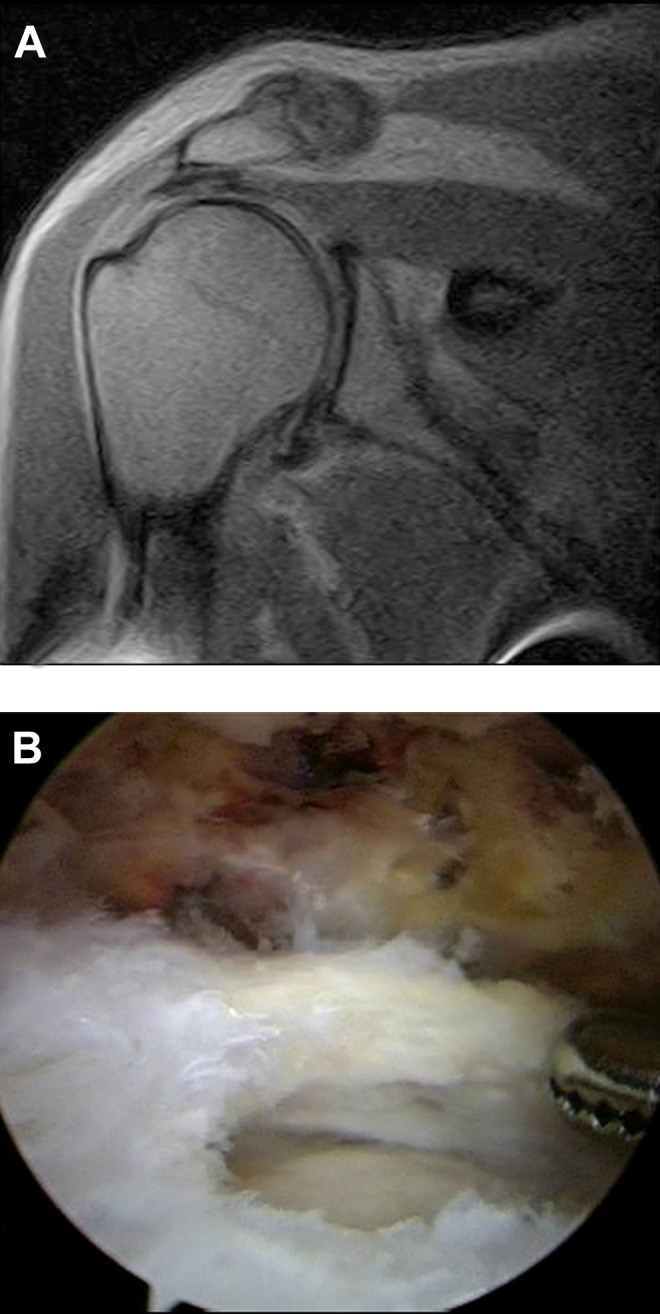
Magnetic resonance imaging and arthroscopic findings of a right shoulder full-thickness tear of the supraspinatus tendon with retraction. (A) Proton density–weighted oblique coronal view using an E-scan Opera Esaote 0.2-T scanner. (B) Standard posterior viewing portal with 30° arthroscope evaluating the rotator cuff following arthroscopic debridement.
While rotator cuff pathology was identified well using the extremity scanner, findings were mixed with regard to the glenoid labrum. Diagnosis of anterior labral lesions was accurate (sensitivity, 86%; specificity, 99%); however, with only 7 such lesions confirmed by surgical findings, the data are somewhat limited by sample size. The same can be said for posterior labral lesions, which were not reported in the surgical findings of any patient during this series. While only 1 false positive was found during the study (specificity, 99%), we are unable to determine the usefulness of low-field MRI in correctly identifying a posterior labral lesion. SLAP lesions were poorly identified using our low-field scanner (sensitivity, 20%; specificity 100%). While all SLAP lesions identified on the MRI reading were confirmed at the time of surgery, most were missed by the MRI altogether. This suggests that regular low-field MRI images are not sensitive enough to identify abnormal signal consistent with a SLAP lesion. Although previous studies comparing low-field MRIs to surgical findings also showed decreased reliability for identifying labral pathology, their sensitivities were still considerably higher than ours (sensitivity, 55%-89%; specificity, 95%-100%).24,35 It is unclear why this difference may exist, and since they evaluated labral lesions as a whole, we cannot compare our findings for the different types of lesions.
In comparison with the rotator cuff, decreased accuracy for identifying pathology of the glenoid labrum is not isolated to low-field MRIs. Mid- and high-field MRIs without arthrogram also showed varied results when evaluating labral lesions (sensitivity, 44%-95%; specificity, 63%-91%).1,5,19,25,28 Similar to our study, Gusmer et al7 also found that high-field MRIs are most sensitive to anterior labral lesions, followed by SLAP lesions, and then posterior labral lesions. To better evaluate the glenoid labrum, MR arthrography may be recommended. Arthrograms have been shown to improve identification of soft tissue shoulder pathology using low- and high-field MRI scanners, which is of particular value for evaluating the labrum.3,8,10–14,29,31,34 Given our results, we would also recommend MR arthrograms when labral pathology is of primary concern.
In an effort to reduce confounding factors, we used data from a single surgeon to eliminate potential interobserver variability in surgical findings; however, there still exists the possibility of variability between the 3 radiologists, as well as between the radiologists and the surgeon. While some variability may exist between radiologists, we would anticipate it to be limited as each radiologist is highly experienced in musculoskeletal radiology and works within the same radiology group. Loew et al13 found there to be good agreement between radiologists when reading both low- and high-field MRIs. Future studies could control for this by using a single radiologist, although including MRI readings from a group of radiologists more accurately mimics reality and strengthens the clinical relevance of the results. The radiologist’s interpretations were done at the time of the study, which may reduce bias. Additionally, variability may exist between the surgeon and radiologists, though again our study is representative of the process in a clinical setting.
Another limitation within any study of this nature is the difficulty of assessing false positive and false negative results for patients who never had surgery. Patients who did not pursue surgery despite showing a tear on the MRI were likely able to tolerate or resolve their symptoms through conservative management. While patients are often able to live with small tears of the rotator cuff or labrum, it would not be surprising if some of these patients may have been incorrectly diagnosed with tears on the MRI. The same issues arise when assessing false negative results, as patients with negative results would be less likely to pursue operative management, which is a difficult issue to control for without exposing patients to unnecessary surgery. With that said, patients with negative MRIs who subsequently failed conservative management would have been likely to receive a repeat MRI, an MR arthrogram, or diagnostic arthroscopy.
The MRI scanner utilized in the study is owned and operated by our practice, so bias and self-referral are valid topics of discussion. However, the radiologist who read the MRIs did not have ownership of the scanner, and no MRI or operative reports were reinterpreted at any time during the retrospective review of the data. MRIs were performed in our office out of convenience to the patient and to expedite diagnoses. Patients who either requested to have their MRIs performed at another facility or did not have insurance coverage for our scanner were provided with information regarding other locations in the area. Patients who indicated the need for an MR arthrogram were also referred elsewhere. Because of the variability of scanners at outside facilities, we did not include any of these patients in the study. Furthermore, the objective of the study was to compare low-field MRI with arthroscopy, not to compare low-field MRI directly with high-field MRI. We felt that evaluating a single scanner with a consistent imaging protocol was the best way to achieve this goal and decrease possible variables.
Low- and standard high-field MRIs are still the most commonly used imaging techniques for diagnosing soft tissue injuries to the shoulder, although they are not the only options. Recent advances in MRI technology have led to the availability of 3.0-T scanners. These super–high-field scanners offer superior imaging quality, but do so at increased cost. Studies have not shown that 3.0-tesla scanners are better able to identify partial-thickness (sensitivity, 75%-92%; specificity, 100%) or full-thickness (sensitivity, 92%-98%; specificity, 96%-100%) rotator cuff tears in comparison with other scanners.14,16 However, they have shown promise in better identifying lesions of the anterior (sensitivity, 83%-89%; specificity, 100%), posterior (sensitivity, 84%-86%; specificity, 100%), and superior labrum (sensitivity, 83%-90%; specificity, 99-100%).14,17 A faster and less expensive alternative to the MRI altogether is ultrasound. Ultrasound has been very effective in diagnosing full-thickness rotator cuff tears and, although results for partial-thickness tears have been more mixed, a recent study by Vylchou et al30 showed no significant difference between an ultrasound and high-field MRI. However, these authors still recommended the use of MRI for complex injuries that also involve structures around the rotator cuff, and they also mentioned that there is a significant learning curve for those not yet trained in the use of diagnostic ultrasound.30 In a time when cost control is at the forefront of health care reform, it is important to identify ways to lower costs without compromising patient care. Ultrasound and low-field MRI are 2 good options for achieving this goal when diagnosing rotator cuff tears, and the use of one method over the other will likely depend on the user’s familiarity with each method.
Conclusion
Magnetic resonance imaging is a useful tool for identifying the extent of soft tissue shoulder injuries, but it is not without limitations. Patient history, symptoms, and physical examination should be used to support MRI findings and be factored into the patient’s treatment plan. This study shows that low-field extremity MRI scanners are accurate in determining partial- and full-thickness rotator cuff tears when compared with surgical findings; however, they cannot accurately identify SLAP lesions. At this time, more information is needed regarding anterior and posterior labral lesions, and future prospective studies comparing low-field MR arthrograms to regular low-field MRIs for the same patient group would be of use.
Acknowledgment
The authors thank the following radiologists for reading the images in this study: Gregory R. Applegate, MD; Emily H. Lee, MD; and Robert K. Lee, MD.
Footnotes
One or more of the authors has reported the following potential conflict of interest or source of funding: W.B.S. and S.E.P. are partners in the practice (Stetson Powell Orthopaedics and Sports Medicine) that owns and operates the MRI machine used in this study.
References
- 1. Allmann KH, Walter O, Laubenberger J, et al. Magnetic resonance diagnosis of the anterior labrum and capsule. Effect of field strength on efficacy. Invest Radiol. 1998;33:415–420. [DOI] [PubMed] [Google Scholar]
- 2. Balich SM, Sheley RC, Brown TR, Sauser DD, Quinn SF. MR imaging of the rotator cuff tendon: interobserver agreement and analysis of interpretive errors. Radiology. 1997;204:191–194. [DOI] [PubMed] [Google Scholar]
- 3. Bencardino JT, Beltran J, Rosenberg ZS, et al. Superior labrum anterior-posterior lesions: diagnosis with MR arthrography of the shoulder. Radiology. 2000;214:267–271. [DOI] [PubMed] [Google Scholar]
- 4. Dinnes J, Loveman E, McIntyre L, Waugh N. The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review. Health Technol Assess. 2003;7:1–166. [DOI] [PubMed] [Google Scholar]
- 5. Garneau RA, Renfrew DL, Moore TE, el-Khoury GY, Nepola JV, Lemke JH. Glenoid labrum: evaluation with MR imaging. Radiology. 1991;179:519–522. [DOI] [PubMed] [Google Scholar]
- 6. Ghazinoor S, Crues JV 3rd, Crowley C. Low-field musculoskeletal MRI. J Magn Reson Imaging. 2007;25:234–244. [DOI] [PubMed] [Google Scholar]
- 7. Gusmer PB, Potter HG, Schatz JA, et al. Labral injuries: accuracy of detection with unenhanced MR imaging of the shoulder. Radiology. 1996;200:519–524. [DOI] [PubMed] [Google Scholar]
- 8. Holzapfel K, Waldt S, Bruegel M, et al. Inter- and intraobserver variability of MR arthrography in the detection and classification of superior labral anterior posterior (SLAP) lesions: evaluation in 78 cases with arthroscopic correlation. Eur Radiol. 2010;20:666–673. [DOI] [PubMed] [Google Scholar]
- 9. Iannotti JP, Zlatkin MB, Esterhai JL, Kressel HY, Dalinka MK, Spindler KP. Magnetic resonance imaging of the shoulder. Sensitivity, specificity, and predictive value. J Bone Joint Surg Am. 1991;73:17–29. [PubMed] [Google Scholar]
- 10. Iqbal HJ, Rani S, Mahmood A, Brownson P, Aniq H. Diagnostic value of MR arthrogram in SLAP lesions of the shoulder. Surgeon. 2010;8:303–309. [DOI] [PubMed] [Google Scholar]
- 11. Jonas SC, Walton MJ, Sarangi PP. Is MRA an unnecessary expense in the management of a clinically unstable shoulder? A comparison of MRA and arthroscopic findings in 90 patients. Acta Orthop. 2012;83:267–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kreitner KF, Loew R, Runkel M, Zollner J, Thelen M. Low-field MR arthrography of the shoulder joint: technique, indications, and clinical results. Eur Radiol. 2003;13:320–329. [DOI] [PubMed] [Google Scholar]
- 13. Loew R, Kreitner KF, Runkel M, Zoellner J, Thelen M. MR arthrography of the shoulder: comparison of low-field (0.2 T) vs high-field (1.5 T) imaging. Eur Radiol. 2000;10:989–996. [DOI] [PubMed] [Google Scholar]
- 14. Magee T. 3-T MRI of the shoulder: is MR arthrography necessary? AJR Am J Roentgenol. 2009;192:86–92. [DOI] [PubMed] [Google Scholar]
- 15. Magee T, Shapiro M, Williams D. Comparison of high-field-strength versus low-field-strength MRI of the shoulder. AJR Am J Roentgenol. 2003;181:1211–1215. [DOI] [PubMed] [Google Scholar]
- 16. Magee T, Williams D. 3.0-T MRI of the supraspinatus tendon. AJR Am J Roentgenol. 2006;187:881–886. [DOI] [PubMed] [Google Scholar]
- 17. Magee TH, Williams D. Sensitivity and specificity in detection of labral tears with 3.0-T MRI of the shoulder. AJR Am J Roentgenol. 2006;187:1448–1452. [DOI] [PubMed] [Google Scholar]
- 18. Merl T, Scholz M, Gerhardt P, et al. Results of a prospective multicenter study for evaluation of the diagnostic quality of an open whole-body low-field MRI unit. A comparison with high-field MRI measured by the applicable gold standard. Eur J Radiol. 1999;30:43–53. [DOI] [PubMed] [Google Scholar]
- 19. Monu JU, Pope TL, Jr, Chabon SJ, Vanarthos WJ. MR diagnosis of superior labral anterior posterior (SLAP) injuries of the glenoid labrum: value of routine imaging without intraarticular injection of contrast material. AJR Am J Roentgenol. 1994;163:1425–1429. [DOI] [PubMed] [Google Scholar]
- 20. Nam EK, Snyder SJ. The diagnosis and treatment of superior labrum, anterior and posterior (SLAP) lesions. Am J Sports Med. 2003;31:798–810. [DOI] [PubMed] [Google Scholar]
- 21. National Ambulatory Medical Care Survey. Hyattsville, MD: Public Health Service; 2010. [Google Scholar]
- 22. Quinn SF, Sheley RC, Demlow TA, Szumowski J. Rotator cuff tendon tears: evaluation with fat-suppressed MR imaging with arthroscopic correlation in 100 patients. Radiology. 1995;195:497–500. [DOI] [PubMed] [Google Scholar]
- 23. Robertson PL, Schweitzer ME, Mitchell DG, et al. Rotator cuff disorders: interobserver and intraobserver variation in diagnosis with MR imaging. Radiology. 1995;194:831–835. [DOI] [PubMed] [Google Scholar]
- 24. Shellock FG, Bert JM, Fritts HM, Gundry CR, Easton R, Crues JV. 3rd Evaluation of the rotator cuff and glenoid labrum using a 0.2-tesla extremity magnetic resonance (MR) system: MR results compared to surgical findings. J Magn Reson Imaging. 2001;14:763–770. [DOI] [PubMed] [Google Scholar]
- 25. Shih TT, Chen WG, Su CT, Huang KM, Ericson F, Chiu LC. MR patterns of rotator cuff and labral lesions: comparison between low-field and high-field images. J Formos Med Assoc. 1993;92:146–151. [PubMed] [Google Scholar]
- 26. Snyder SJ. Shoulder Arthroscopy. 2nd ed Philadelphia, PA: Lippincott Williams & Wilkins; 2003. [Google Scholar]
- 27. Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthroscopy. 1990;6:274–279. [DOI] [PubMed] [Google Scholar]
- 28. Tung GA, Entzian D, Green A, Brody JM. High-field and low-field MR imaging of superior glenoid labral tears and associated tendon injuries. AJR Am J Roentgenol. 2000;174:1107–1114. [DOI] [PubMed] [Google Scholar]
- 29. Tung GA, Hou DD. MR arthrography of the posterior labrocapsular complex: relationship with glenohumeral joint alignment and clinical posterior instability. AJR Am J Roentgenol. 2003;180:369–375. [DOI] [PubMed] [Google Scholar]
- 30. Vlychou M, Dailiana Z, Fotiadou A, Papanagiotou M, Fezoulidis IV, Malizos K. Symptomatic partial rotator cuff tears: diagnostic performance of ultrasound and magnetic resonance imaging with surgical correlation. Acta Radiol. 2009;50:101–105. [DOI] [PubMed] [Google Scholar]
- 31. Waldt S, Burkart A, Imhoff AB, Bruegel M, Rummeny EJ, Woertler K. Anterior shoulder instability: accuracy of MR arthrography in the classification of anteroinferior labroligamentous injuries. Radiology. 2005;237:578–583. [DOI] [PubMed] [Google Scholar]
- 32. Wnorowski DC, Levinsohn EM, Chamberlain BC, McAndrew DL. Magnetic resonance imaging assessment of the rotator cuff: is it really accurate? Arthroscopy. 1997;13:710–719. [DOI] [PubMed] [Google Scholar]
- 33. Woertler K, Strothmann M, Tombach B, Reimer P. Detection of articular cartilage lesions: experimental evaluation of low- and high-field-strength MR imaging at 0.18 and 1.0 T. J Magn Reson Imaging. 2000;11:678–685. [DOI] [PubMed] [Google Scholar]
- 34. Woertler K, Waldt S. MR imaging in sports-related glenohumeral instability. Eur Radiol. 2006;16:2622–2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zlatkin MB, Hoffman C, Shellock FG. Assessment of the rotator cuff and glenoid labrum using an extremity MR system: MR results compared to surgical findings from a multi-center study. J Magn Reson Imaging. 2004;19:623–631. [DOI] [PubMed] [Google Scholar]



