Abstract
Background:
Invasive and continuous blood pressure (BP) monitoring is crucial after cardiac surgery. Accuracy of BP measurement mostly depends on patency of arterial catheter and acceptable waveform. Heparinized saline flush usually used for this purpose may be accompanied by potential heparin adverse effects.
Objectives:
The aim of this study was to compare heparinized and non-heparinized saline flush to maintain acceptable arterial waveform after cardiac surgery.
Materials and Methods:
In a double blind randomized trial study, 100 patients undergoing elective cardiac surgery were randomized to using heparinized (n = 50) or non-heparinized (normal) saline flush (n = 50) to maintain patency of arterial catheter after operation. Indwelling arterial catheters were checked daily for acceptable arterial waveform for three days as primary outcome measures.
Results:
Frequency of acceptable arterial waveform ranged from 66% to 80%, in first, second and third postoperative days. There were no statistically significant differences between heparinized and non-heparinized saline groups regarding acceptable arterial waveforms in all the three postoperative days (all P values > 0.05).
Conclusions:
Using non-heparinized normal saline is suitable to maintain acceptable arterial waveform for short-term (three days) after adult cardiac surgery considering potential adverse effects of heparin.
Keywords: Heparin, Saline Solution, Cardiac Surgery
1. Background
Cardiac surgery is increasingly performed for high-risk patients referred for operation; much attempts have been performed to reduce the operative mortality (1). Hemodynamic monitoring is necessary in cardiac intensive care unit. Since invasive hemodynamic monitoring provides continuously monitoring such as showing the curves continuously with more accuracy, it would be preferable to noninvasive methods (2, 3). Invasive hemodynamic monitoring is more costly, has more complications and requires more skill to perform and maintain a monitoring than non-invasive monitoring, also is acceptable as a standard method for monitoring critical patients (4). Arterial catheters are used for continuous monitoring of critical patients in intensive care units (5).
Arterial catheterization complications include inappropriate arterial waveform, bleeding, local hematoma and temporary occlusion of the arteries, sustained ischemic injury, pseudo-aneurysm and infection (6). Arterial thrombosis is the main complication of arterial catheterization (7). To obtain the correct data, transducer should be at the level of fourth intercostal space (8). In addition, zero the system is to neutralize the effect of hydrostatic pressure, transducer pressure, amplifier and oscilloscope (9).
Normal arterial waveform contains the following components: Ascending slope of systolic arterial pressure, peak systolic arterial pressure, descending slope of systolic arterial pressure, dicrotic notch, continue of blood flow through the artery to the vein based on the pressure gradient and end-diastolic pressure (5). Heparinized saline solution is widely used to prevent occlusion of arterial catheters in intensive care units (10). Heparin has effects at multiple sites of the intrinsic and extrinsic coagulation pathways. The most common complication of heparin is bleeding (11). Unfractionated heparin is used as a standard anticoagulant in patients undergoing cardiac surgeries (12). Evidence shows that chronic use of heparin, even at low dose, may cause thrombocytopenia and bleeding (13, 14). Recent evidence suggests that normal saline solution can maintain patency of arterial catheter, increase accuracy of coagulation tests and prevent patient from exposure to complications of heparin (10).
2. Objectives
The aim of this study was to compare heparinized and non-heparinized normal saline flush to maintain acceptable arterial waveform in indwelling arterial catheters after adult cardiac surgery including coronary bypass and valve operations.
3. Materials and Methods
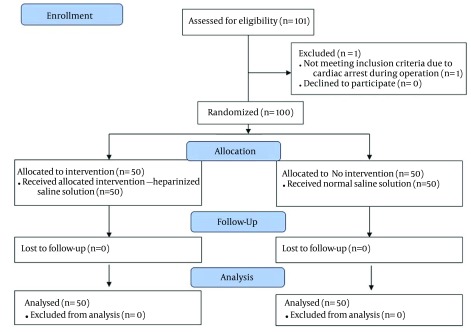
In a double blind randomized clinical trial study, 100 patients undergoing elective cardiac surgery entered the study. The study was approved in institutional ethic committee and all patients filled out informed consents. The patients were randomized to use heparinized (n = 50) or non-heparinized (normal) saline flush (n = 50) to maintain patency of arterial catheter after operation. The randomization method was simple and random allocation was performed using an online method (URL:http://www.graphpad.com/quickcalcs/randomize2/). The random allocation was concealed from researcher and kept confidential with third person until the end of study. The study flow diagram is shown in Figure 1. Inclusion criteria were patients who had arterial catheters, PT (prothrombin time) up to 13 seconds, activated partial prothrombin time (aPTT) up to 45 seconds, platelet count 140000 - 440000 mm3, filling out a consent form for the study and placement of catheters in intensive care unit. Exclusion criteria were known allergy to heparin, history of heparin-induced thrombocytopenia, coagulation disorder before using heparin, more than five times effort to put the catheter in place, thrombocytopenia with platelets less than 100000 mm3 and simultaneous participation in any other study.
Figure 1. The Study Flow Diagram.
For the survey of arterial waveform, monitoring devices were connected to the patient. Arterial catheters should positive response to the flush test. This means that with the serum flush in the arterial catheter, arterial wave disappeared and a direct line appeared in the monitoring device. Closing the catheter should also have a rapid decline to below the baseline. Flush test can determine damping situation in system. This means normal damped, over damped and under damped, in which in any situation with response to the flush test, pressure increases in the system, but reaction in the end of flush test is varied. In the normal damped system at end of flash test, there would be one to two oscillation. In the over damped system, at the end of flush test there is no oscillation and with under damped system, there would be several oscillation at the end of flush test on the oscilloscope.
Our data gathered daily and repeated for three days. In the heparinized saline group to remain patency of catheters, heparin with concentration of 10 u/mL was used. In the normal saline group, 5 mL of normal saline was used for each flush.
The collected data was analyzed using SPSS v.21.0 statistical software (SPSS Inc. Chicago, IL, USA). Categorical data analyzed using chi-square or Fisher’s exact test as appropriate. Mean values of continuous parameters compared between the two groups using independent samples t-test. P value ≤ 0.05 was considered statistically significant in this study.
4. Results
Of 100 studied patients, 69 were men and 31 women. All patients completed the study. Patients’ demographic and clinical data are summarized in Table 1. As Table 1 shows, mean of aPTT tests and platelet count were comparable in heparinized and non-heparinized normal saline flush groups. Most commonly used arterial catheter size was 20 gauges and most common catheterization site was radial artery.
Table 1. Demographic and Clinical Characteristics of Patients in the Two Study Groups a,b,c.
| Parameters | Heparinized Saline Group (n = 50) | Normal Saline Group (n = 50) | P Value |
|---|---|---|---|
| Age, y | 49.7 ± 11.2 | 53.5 ± 12.2 | 0.194 |
| Gender | |||
| Male | 30 (60) | 39 (78) | 0.052 |
| Female | 20 (40) | 11 (22) | |
| Height, cm | 162 ± 14 | 160 ± 15 | 0.492 |
| Weight, kg | 69.1 ± 11.1 | 67.4 ± 10.8 | 0.440 |
| Type of surgery | |||
| CABG | 33 (66) | 27 (54) | 0.710 |
| Valve | 22 (44) | 28 (56) | |
| aPTT, sec c | 33.7 ± 4.9 | 32.1 ± 4.2 | 0.083 |
| Platelet count, × 103 c | 226 ± 51 | 240 ± 57 | 0.199 |
| Arterial catheter size (gauge) | |||
| 20 | 46 (92) | 48 (96) | 0.678 |
| 18 | 4 (8) | 2 (4) | |
| Arterial catheter site | |||
| Radial | 42 (84) | 41 (82) | |
| Brachial | 5 (10) | 6 (12) | |
| Femoral | 2 (4) | 0 | 0.791 |
a Abbreviations: aPTT, Activated partial prothrombin time; and CABG, Coronary artery bypass grafting.
b Data are presented as No. (%) or Mean ± SD.
c In second postoperative day.
As Table 2 demonstrates, frequency of acceptable arterial waveform ranged from 66% to 80%, in first, second and third postoperative days. There were no statistically significant differences between the heparinized and non-heparinized saline groups regarding acceptable arterial waveforms in all the three postoperative days (all P values > 0.05). Repeated measures ANOVA test showed statistically significant changes during consecutive three postoperative days in frequency of acceptable arterial waveform in each study group (P < 0.05).
Table 2. Frequency of Acceptable Arterial Waveform in First, Second and Third Postoperative Days a.
| Variable | Heparinized Saline Group (n = 50) | Normal Saline Group (n = 50) | P Value |
|---|---|---|---|
| Acceptable arterial waveform in 1st postop Day | 39 (78) | 36 (72) | 0.774 |
| Acceptable arterial waveform in 2nd postop Day | 40 (80) | 39 (78) | 0.793 |
| Acceptable arterial waveform in 3rd postop Day | 33 (66) | 32 (65.3) | 0.887 |
a Data are presented as No. (%).
There was one case of arterial occlusion in radial artery during three postoperative days in each study groups, needed to change the catheter place and indwelling arterial catheter in other radial side.
5. Discussion
Heparinized saline solution is known as a common solution in maintaining catheter patency and effectiveness (13). However, adverse effects of heparinized saline solution and effect of normal saline in maintaining patency of arterial catheter lead to controversy over the type of flush solutions to maintain catheter effectiveness (10, 15-17). In a recent systematic review, Kordzadeh et al. (15) concluded that heparinized saline solution may be better for long-term use of arterial line. Use of heparin, even in low dose, can be associated with potential complications such as heparin induced thrombocytopenia (13). In addition, use of heparin in flush solution can increase aPTT significantly (5). Therefore, our aim was to determine the effect of heparinized saline and normal saline solution to provide acceptable arterial waveform for short-term maintenance. Our study showed that acceptable arterial waveforms in heparinized saline and normal saline groups in the first, second and third days were not statistically different.
Normal saline provided acceptable arterial waveform and regarding heparin complications such as bleeding, thrombosis and thrombocytopenia, we suggest to use normal saline solution as an effective alternative solution for heparinized saline solution. In conclusion, normal saline solution can be used as a safe alternative for heparinized saline solution for short-term after adult cardiac surgery.
5.1. Limitations
One of the limitations in this study was patient population (adult cardiac surgery), so these results could not be generalizable to other patient population. This trial was performed on limited sample size (n = 100) and in a single center base; large scale multicenter studies could be more powerful. As our patients’ stay were limited to 3-4 days in ICU, we assessed the arterial waveform only for three days; for evaluation of efficacy of normal saline on long-term arterial waveform, more research must be performed in ICU with long-term patient stay.
Acknowledgments
We would like to thank all our colleagues in our center cardiac surgery intensive care unit for their support, especially nurses Mr. Najafikhah and Miss Barati, Hashemi and Shojaei.
References
- 1.LaPar DJ, Filardo G, Crosby IK, Speir AM, Rich JB, Kron IL, et al. The challenge of achieving 1% operative mortality for coronary artery bypass grafting: a multi-institution Society of Thoracic Surgeons Database analysis. J Thorac Cardiovasc Surg. 2014;148(6):2686–96. doi: 10.1016/j.jtcvs.2014.06.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Langwieser N, Prechtl L, Meidert AS, Hapfelmeier A, Bradaric C, Ibrahim T, et al. Radial artery applanation tonometry for continuous noninvasive arterial blood pressure monitoring in the cardiac intensive care unit. Clin Res Cardiol. 2015;104(6):518–24. doi: 10.1007/s00392-015-0816-5. [DOI] [PubMed] [Google Scholar]
- 3.Esper SA, Pinsky MR. Arterial waveform analysis. Best Pract Res Clin Anaesthesiol. 2014;28(4):363–80. doi: 10.1016/j.bpa.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 4.Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Young WL. Miller's anesthesia. 8th ed. Elsevier; 2015. [Google Scholar]
- 5.Del Cotillo M, Grane N, Llavore M, Quintana S. Heparinized solution vs. saline solution in the maintenance of arterial catheters: a double blind randomized clinical trial. Intensive Care Med. 2008;34(2):339–43. doi: 10.1007/s00134-007-0886-6. [DOI] [PubMed] [Google Scholar]
- 6.Handlogten KS, Wilson GA, Clifford L, Nuttall GA, Kor DJ. Brachial Artery Catheterization: An Assessment of Use Patterns and Associated Complications. Anaesth Analg. 2014;118(2):288–95. doi: 10.1213/ANE.0000000000000082. [DOI] [PubMed] [Google Scholar]
- 7.Brancati MF, Burzotta F, Coluccia V, Trani C. The occurrence of radial artery occlusion following catheterization. Expert Rev Cardiovasc Ther. 2012;10(10):1287–95. doi: 10.1586/erc.12.125. [DOI] [PubMed] [Google Scholar]
- 8.Jones HA. Arterial transducer placement and cerebral perfusion pressure monitoring: a discussion. Nurs Crit Care. 2009;14(6):303–10. doi: 10.1111/j.1478-5153.2009.00352.x. [DOI] [PubMed] [Google Scholar]
- 9.Hersh LT, Friedman B, Luczyk W, Sesing J. Evaluation of filtering methods for acquiring radial intra-artery blood pressure waveforms. J Clin Monit Comput. 2014 doi: 10.1007/s10877-014-9649-4. [DOI] [PubMed] [Google Scholar]
- 10.Robertson-Malt S, Malt GN, Farquhar V, Greer W. Heparin versus normal saline for patency of arterial lines. Cochrane Database Syst Rev. 2014;5:CD007364. doi: 10.1002/14651858.CD007364.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Besser MW, Ortmann E, Klein AA. Haemostatic management of cardiac surgical haemorrhage. Anaesthesia. 2015;70 Suppl 1:87–95. doi: 10.1111/anae.12898. e29-31. [DOI] [PubMed] [Google Scholar]
- 12.Murphy GS, Marymont JH. Alternative anticoagulation management strategies for the patient with heparin-induced thrombocytopenia undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2007;21(1):113–26. doi: 10.1053/j.jvca.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 13.Bertoglio S, Solari N, Meszaros P, Vassallo F, Bonvento M, Pastorino S, et al. Efficacy of normal saline versus heparinized saline solution for locking catheters of totally implantable long-term central vascular access devices in adult cancer patients. Cancer Nurs. 2012;35(4):E35–42. doi: 10.1097/NCC.0b013e31823312b1. [DOI] [PubMed] [Google Scholar]
- 14.Brzezinski M, Luisetti T, London MJ. Radial artery cannulation: a comprehensive review of recent anatomic and physiologic investigations. Anesth Analg. 2009;109(6):1763–81. doi: 10.1213/ANE.0b013e3181bbd416. [DOI] [PubMed] [Google Scholar]
- 15.Kordzadeh A, Austin T, Panayiotopoulos Y. Efficacy of normal saline in the maintenance of the arterial lines in comparison to heparin flush: a comprehensive review of the literature. J Vasc Access. 2014;15(2):123–7. doi: 10.5301/jva.5000183. [DOI] [PubMed] [Google Scholar]
- 16.Kannan A. Heparinised saline or normal saline? J Perioper Pract. 2008;18(10):440–1. doi: 10.1177/175045890801801003. [DOI] [PubMed] [Google Scholar]
- 17.Mortezaiyan H, Aarabi-Moghadam M, Asadpour N, Parchami-Ghazaee S, Khalili Y, Vahidshahi K. Treatment of femoral artery thrombosis with streptokinase and heparin after cardiac catheterization. Res Cardiovasc Med. 2014;3(1):e28086. doi: 10.5812/cardiovascmed.13552. [DOI] [PMC free article] [PubMed] [Google Scholar]