Abstract
Background:
Joint range of motion might affected by some factors like laxity and increase joint mobility. Generalized joint hypermobility and temporomandibular joint hypermobility (TMJH) are reported as risk factors for temporomandibular disorders. The aim of this study was to survey the etiological factors of TMJH and its relations to habitual status.
Materials and Methods:
In this cross-sectional descriptive study, 69 patients with TMJH were involved. After profiling personal information and medical history, the patients were divided into three groups based on their maximum mouth opening (MMO) as follow:
(Light) MMO of 50-55 mm, (moderate): MMO between 55 and 65 mm, (severe) MMO >65 mm. For subjective observations, patients were asked to fill the prepared questionnaire. The objective evaluations conducted by a specialist. Finally, all the data subjected Chi-Square test by using SPSS software version 22 at a significant level of 0.05.
Results:
TMJH was more common in women (74.2%). The light group had significant differences with other groups in the discomfort of TMJ and TMJ sound (P < 0.05). Furthermore, sever group manifested highest percentage of masticatory pains, significantly (P < 0.05).
Conclusion:
It can be concluded that pain in TMJ would have a correlation with MMO.
Keywords: Generalized joint hypermobility, Temporomandibular joint, Temporomandibular joint disorder
Introduction
Temporomandibular disorders (TMD) are called to a group of painful conditions with a prevalence rate of 3-15%, in which temporomandibular joints (TMJs) and/or masticatory muscles are typically involved.1-3 Patients with TMD frequently complain about multiple bodily pains outside of the orofacial regions.4,5 TMDs are often described based on some signs and symptoms like: TMJ sounds, impaired mandibular movement, limitation in mouth opening, preauricular pain, facial pain, headaches, and jaw tenderness on function.6
In cases of persistent and recurrent pains, TMD may demonstrate a chronic course. TMD is not a life-threatening disease, but the quality of life may be reduced.7
Generalized joint hypermobility is a hereditary problem defined by the increase in range of motion in multiple joints, which might affect TMJ in some cases that is named TMJ hypermobility (TMJH).3,8
Joint range of motion might be affected by numerous factors including: Biochemical changes in the structure of collagen and elastin, loss of resistance to traction, laxity, and increase joint mobility.3 Winocur et al. conducted a study about the prevalence of general joint laxity and TMJH among adolescent girls. They concluded that the prevalence of generalized joint laxity was 43% and TMJH was recognized in 27.3%.8
In another survey, Adair and Hecht discovered that participants with generalized joint hypermobility may be more likely to demonstrate some signs and symptoms of TMD than ones with normal joint mobility.9
In another view, correlations between dental occlusion and (TMD) have been proved, also mandibular resting position can be affected by different factors such as: Occlusal interferences, TMD, the position of the head and body of mandible, and emotional tensions, which may lead to bodily adaptations and realignments of tooth and TMJ.1,10,11
Due to the fact that generalized joint hypermobility and TMJH are reported as risk factors for TMD,12 the aim of this study was to clarify the etiological factors of TMJH and its relations to habitual modalities.
Materials and Methods
Ethics: Present article is based on thesis with ID number of UDK:616.724-08.089.23; the survey was executed in medical and surgical department of Poltava Dental Clinic and Maxillofacial Department of POKB, Ukraine; also a medical consent was filled by each contributors and all procedures were required for treatment plans.
This observational/case-control clinical study was conducted on 69 individuals between the ages of 22 and 42 who had the manifestation of TMJH.
Any severe systemic disease (like rheumatoid arteritis) and un-cooperation were assumed as criteria.
After profiling personal information and medical history, the patients were divided into three groups based on their maximum mouth opening (MMO), which was measured by a disposable ruler between upper and lower incisors:9
Light: 25 patients with MMO of 50-55 mm.
Moderate: 18 patients with MMO between 55 and 65 mm.
Severe: 26 patients with MMO > 65 mm.
For subjective observations, patients were asked to fill the prepared questionnaire, with the help of examiner if it was necessary, to reveal following information:
Discomfort of TMJ during MMO
Pain in TMJ during MMO
Pain in masticators
TMJ clicking or other sounds
Irradiation of pain in the ear(s), temple or neck
Usual side of chewing
Usual side of TMJ which was lied on during asleep
The first symptoms of TMJH if they were recalled.
The clinical procedure continued with objective tests by an oral and maxillofacial specialist. Then extra oral observation followed as facial asymmetry, condition of the facial musculoskeletal system, functional and morphological changes in the teeth and jaw system and a detailed research of the nature of pathological changes in the TMJ, palpation of TMJ projection zone, manual assessment of muscle tone, movements of the mandible in the horizontal and vertical planes, malocclusion caused by teeth positions, analysis of dynamic occlusion in order to evaluate the performance of jaw movements, the amount of lateral movements of the mandible, passive movement of the mandible, passive compression by means of bilaminar zone adaptation, and dynamic compression for evaluation of ligamentous apparatus, the joint capsule and articular surfaces.
To assess masticatory system specially temporal and medial pterygoid muscles, the shape, size, density, vitality, and pain were tested. Auscultation was performed using stethoscope which was tightly applied to the joint, but without pressure. It was necessary to listen to the noise in the joint space or separate quadrants of the joints. At the end, consultations with orthopedic, dentists, rheumatologist, and neurologist were performed if necessary. All the data subjected to Chi-square test by using SPSS software version 22 at a significant level of 0.05.
Results
This study was conducted on 69 patients (54 women and 15 men), at the age from 22 to 42 years old. The largest number of patients with TMJH was at the age of 31-42 years old (70.99%), while 37.67% were at the age from 26 to 35 years old. Furthermore, the number of women was three times more (78.2%) than men.
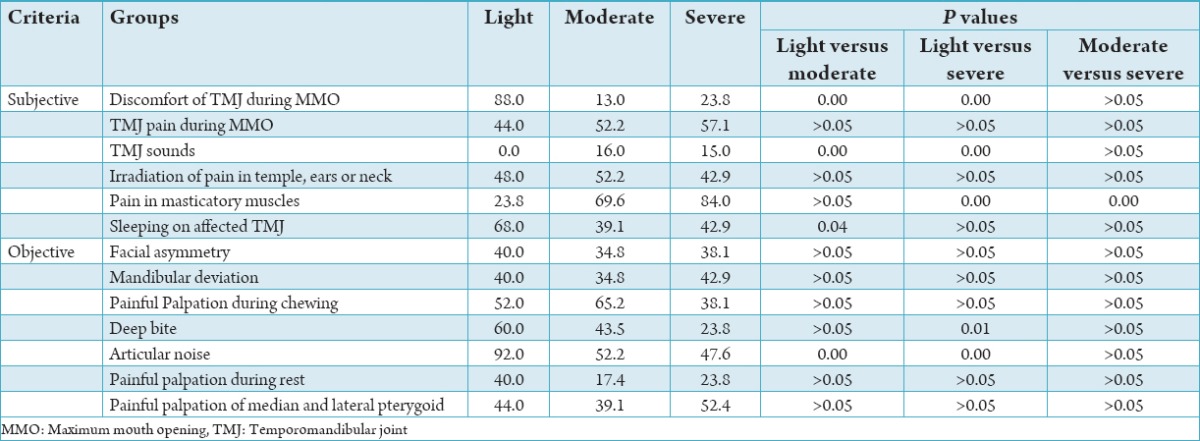
Table 1 represents all subjective and objective signs and symptoms of all the groups.
Table 1.
Distribution of subjective and objective criteria (%) of all the groups alongside with statistical comparisons (P value).
Medical history of patients revealed the presence of familial TMJ diseases in one case of a moderate group. The beginning of disease was gradual in all the periods of remission. Period of illness ranged from 2 to 5 years. Eight patients did not ask for medical treatments, 4 people referred to a dentist, 2 people to otorhinolaryngologist, and 2 others to a neurologist. The main treatment was to assign non-narcotic analgesics and physiotherapy, however, the effects were short-term in 11 people and without success for 5 patients.
Discussion
Based on the results of this study, TMJH was more common in women (74.2%), which is in agreement with other studies.13-15
Pain appears to have significant relationship with impairment of oral health related to the quality of life. Pain is induced when an imbalance occurs between the amount of stimuli and the efficacy of modulation mechanisms.7,16,17 As the result showed, the light group had significant differences with other groups in the discomfort of TMJ and TMJ sound.
In a study with the aim of classifying symptomatic patients diagnosed with TMD into homogenous groups based on their clinical presentation, Pimenta e Silva Machado et al. claimed that localized masticatory muscle pain is recognized as the most common complaint in TMD patients.18 Similar results were found in present study in which sever group manifested highest percentage of masticatory pains, significantly. In that study, pain in TMJ was not considered as an individual complaint.
Recently the most popular theories about etiology of TMDs are based on the biopsychosocial pattern, which is a combination of biological, psychological, and social factors. Quality and pattern of sleeping and stress showed correlation with TMDs.7,19 Sleeping on affected TMJ was the highest in the light group. Perhaps, the higher level of pain in moderate and sever groups make some uncomfortable sensation during sleeping on the affected TMJ.
Winocur et al. found a positive correlation between TMJH and MMO.8 This result is in accordance with Pasinato et al. study about evaluating clinical and psychosocial aspects in TMD patients with or without generalized joint hypermobility, too.3 However, Westling and Helkimo did not found a significant relationship between MMO and peripheral joint mobility.20 Furthermore, Hirsch et al. concluded that patients with hypermobility had a lower risk of having limited MMO.21 Present result hypothesis the correlation between pain in masticatory muscles and higher MMO.
Facial asymmetry and mandibular deviation were not insignificant difference among groups. Inui et al. concluded that facial asymmetry due to mandibular lateral displacement is a relatively common problem in TMDs.22 However, Haghigaht et al. reported that condylar distance was higher in posterior and superior borders in TMJH.23 That might explain the differences.
Articular noise during palpation and auscultation was the highest in a severe group significantly. Ogütcen-Toller believed that clicking and crepitation may be considered as signs of abnormal joint disorder24 and the present result confirmed it too.
In the present study, a few of individuals sought for the TMJH treatments. Although hypermobility is relatively common in the general population, but reports about musculoskeletal complaints are infrequent. As most symptoms are mild and self-limiting, so patients may not search for medical attention.25
Conclusion
Regarding to the limitations of this study like: Low sample size, uneven sample size in groups, limitation of time and etc., it can be concluded that pain in TMJ would have a correlation with MMO.
Footnotes
Conflicts of Interest: None
Source of Support: Nil
References
- 1.El Hage Y, Politti F, de Sousa DF, Herpich CM, Gloria IP, Gomes CA, et al. Effect of mandibular mobilization on electromyographic signals in muscles of mastication and static balance in individuals with temporomandibular disorder: Study protocol for a randomized controlled trial. Trials. 2013;14:316. doi: 10.1186/1745-6215-14-316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alonso-Blanco C, Fernández-de-Las-Peñas C, de-la-Llave-Rincón AI, Zarco-Moreno P, Galán-Del-Río F, Svensson P. Characteristics of referred muscle pain to the head from active trigger points in women with myofascial temporomandibular pain and fibromyalgia syndrome. J Headache Pain. 2012;13(8):625–37. doi: 10.1007/s10194-012-0477-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pasinato F, Souza JA, Corrêa EC, Silva AM. Temporomandibular disorder and generalized joint hypermobility: Application of diagnostic criteria. Braz J Otorhinolaryngol. 2011;77(4):418–25. doi: 10.1590/S1808-86942011000400003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen H, Slade G, Lim PF, Miller V, Maixner W, Diatchenko L. Relationship between temporomandibular disorders, widespread palpation tenderness, and multiple pain conditions: A case-control study. J Pain. 2012;13(10):1016–27. doi: 10.1016/j.jpain.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Melo CE, Oliveira JL, Jesus AC, Maia ML, de Santana JC, Andrade LS, et al. Temporomandibular disorders dysfunction in headache patients. Med Oral Patol Oral Cir Bucal. 2012;17(6):e1042–6. doi: 10.4317/medoral.18007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barbosa Tde S, Miyakoda LS, Pocztaruk Rde L, Rocha CP, Gavião MB. Temporomandibular disorders and bruxism in childhood and adolescence: Review of the literature. Int J Pediatr Otorhinolaryngol. 2008;72(3):299–314. doi: 10.1016/j.ijporl.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 7.Conti PC, Pinto-Fiamengui LM, Cunha CO, Conti AC. Orofacial pain and temporomandibular disorders: The impact on oral health and quality of life. Braz Oral Res. 2012;26(Suppl 1):120–3. doi: 10.1590/s1806-83242012000700018. [DOI] [PubMed] [Google Scholar]
- 8.Winocur E, Gavish A, Halachmi M, Bloom A, Gazit E. Generalized joint laxity and its relation with oral habits and temporomandibular disorders in adolescent girls. J Oral Rehabil. 2000;27(7):614–22. doi: 10.1046/j.1365-2842.2000.00546.x. [DOI] [PubMed] [Google Scholar]
- 9.Adair SM, Hecht C. Association of generalized joint hypermobility with history, signs, and symptoms of temporomandibular joint dysfunction in children. Pediatr Dent. 1993;15(5):323–6. [PubMed] [Google Scholar]
- 10.Bracco P, Deregibus A, Piscetta R. Effects of different jaw relations on postural stability in human subjects. Neurosci Lett. 2004;356(3):228–30. doi: 10.1016/j.neulet.2003.11.055. [DOI] [PubMed] [Google Scholar]
- 11.Nobili A, Adversi R. Relationship between posture and occlusion: A clinical and experimental investigation. Cranio. 1996;14(4):274–85. doi: 10.1080/08869634.1996.11745978. [DOI] [PubMed] [Google Scholar]
- 12.Kavuncu V, Sahin S, Kamanli A, Karan A, Aksoy C. The role of systemic hypermobility and condylar hypermobility in temporomandibular joint dysfunction syndrome. Rheumatol Int. 2006;26(3):257–60. doi: 10.1007/s00296-005-0620-z. [DOI] [PubMed] [Google Scholar]
- 13.Michalak M, Paulo M, Bozyk A, Zadrozny L, Wysokinska-Miszczuk J, Michalak I, et al. Incidence of abnormalities in temporomandibular joints in a population of 1,100 urban and rural patients lacking teeth and other parafunctions in 2003-2008. An international problem. Ann Agric Environ Med. 2013;20(1):86–90. [PubMed] [Google Scholar]
- 14.Ozdemir-Karatas M, Peker K, Balik A, Uysal O, Tuncer EB. Identifying potential predictors of pain-related disability in Turkish patients with chronic temporomandibular disorder pain. J Headache Pain. 2013;14(1):17. doi: 10.1186/1129-2377-14-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davoudi A, Haghighat A, Rybalov O, Shadmehr E, Hatami A. Investigating activity of masticatory muscles in patients with hypermobile temporomandibular joints by using EMG. J Clin Exp Dent. 2015;7:e310–5. doi: 10.4317/jced.52125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dahlström L, Carlsson GE. Temporomandibular disorders and oral health-related quality of life. A systematic review. Acta Odontol Scand. 2010;68(2):80–5. doi: 10.3109/00016350903431118. [DOI] [PubMed] [Google Scholar]
- 17.John MT, Reissmann DR, Schierz O, Wassell RW. Oral health-related quality of life in patients with temporomandibular disorders. J Orofac Pain. 2007;21(1):46–54. [PubMed] [Google Scholar]
- 18.Pimenta e Silva Machado L, de Macedo Nery MB, de Góis Nery C, Leles CR. Profiling the clinical presentation of diagnostic characteristics of a sample of symptomatic TMD patients. BMC Oral Health. 2012;12:26. doi: 10.1186/1472-6831-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rai B, Kaur J. Association between stress, sleep quality and temporomandibular joint dysfunction: Simulated Mars mission. Oman Med J. 2013;28(3):216–9. doi: 10.5001/omj.2013.59. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 20.Westling L, Helkimo E. Maximum jaw opening capacity in adolescents in relation to general joint mobility. J Oral Rehabil. 1992;19(5):485–94. doi: 10.1111/j.1365-2842.1992.tb01112.x. [DOI] [PubMed] [Google Scholar]
- 21.Hirsch C, John MT, Stang A. Association between generalized joint hypermobility and signs and diagnoses of temporomandibular disorders. Eur J Oral Sci. 2008;116:525–30. doi: 10.1111/j.1600-0722.2008.00581.x. [DOI] [PubMed] [Google Scholar]
- 22.Inui M, Fushima K, Sato S. Facial asymmetry in temporomandibular joint disorders. J Oral Rehabil. 1999;26(5):402–6. doi: 10.1046/j.1365-2842.1999.00387.x. [DOI] [PubMed] [Google Scholar]
- 23.Haghigaht A, Davoudi A, Rybalov O, Hatami A. Condylar distances in hypermobile temporomandibular joints of patients with excessive mouth openings by using computed tomography. J Clin Exp Dent. 2014;6(5):e509–13. doi: 10.4317/jced.51562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ogütcen-Toller M. Sound analysis of temporomandibular joint internal derangements with phonographic recordings. J Prosthet Dent. 2003;89(3):311–8. doi: 10.1067/mpr.2003.18. [DOI] [PubMed] [Google Scholar]
- 25.Kirk JA, Ansell BM, Bywaters EG. The hypermobility syndrome. Musculoskeletal complaints associated with generalized joint hypermobility. Ann Rheum Dis. 1967;26(5):419–25. doi: 10.1136/ard.26.5.419. [DOI] [PMC free article] [PubMed] [Google Scholar]


