Abstract
Background:
An improvement in clinical parameters along with regeneration is the desired outcome of periodontal therapy. The aim of this study was to analyze and contrast the efficaciousness of combined open flap debridement (OFD) and subepithelial connective tissue graft (SECTG) to OFD in the management of periodontal supracrestal defects.
Materials and Methods:
Totally, 20 paired sites exhibiting supracrestal defects were subjected to surgical treatment adopting the split mouth design. The defects were divided randomly for treatment with OFD and SECTG (test) or OFD alone (control). The clinical effectiveness of the two arms of treatment was evaluated at 6 months and 12 months post-operatively by assessing clinical and radiographic parameters. The measurements carried out included probing pocket depth (PPD), relative attachment level (RAL), gingival marginal level, radiographic bone level (BL).
Results:
The mean reduction in PPD at 0-12 months was 3.20 ± 0.82 mm and RAL gain of 3.10 ± 1.51 mm was observed, the OFD and SECTG (test) group; corresponding observations for OFD (control) were 2.10 ± 0.63 mm and 1.90 ± 0.57 mm. However, BL changes did not follow the pattern of clinical improvement on the radiographic assessment of either treatment group. Post-operative evaluation was made. Improvement in different clinical parameters was statistically significant (P < 0.01).
Conclusion:
Treatment of supracrestal defects with a combination of OFD and SECTG led to significantly better clinical results compared to OFD alone.
Keywords: Gingival margin level, horizontal defects, periodontitis, regeneration, supracrestal defects, surgical flaps
Introduction
Periodontal pockets if left unaddressed inadvertently lead to further loss of the periodontal architecture. Though elimination of pockets has been a common goal of periodontal therapy, regeneration is a favored modality, where there is a reconstruction of lost or injured tissues in such a way that both the original structure and their function are completely restored.1
Supracrestal defects illustrated as horizontal bone loss radiographically, represents the least predictable periodontal defect type in the regenerative approaches and remain an unsolved dilemma for clinicians. Currently, used regenerative procedures are not routinely applicable to this type of lesion.2
Furthermore, open flap debridement (OFD) the accepted treatment modality for treatment of deep suprabony pockets results in significant gingival recession,3 it has also been reported that post-surgical recession is greater in sites with deeper periodontal pockets.4 Thus, implying that post-surgical recession is directly related to initial probing depth. The varied explanations, for post-surgical recession include inadequate bone support, thin gingival tissue, limited blood supply, and post-operative shrinkage of the flap. With sequelae like poor aesthetics and hypersensitivity, its prevention should be considered as a desirable end goal of periodontal therapy.
Subepithelial connective tissue grafts (SECTGs) have been used to treat labial and buccal gingival recession for attaining root coverage5,6 and clinical attachment gain.7,8 Furthermore, histological evidence of new attachment in previously exposed root surfaces has been widely published.6,9-11 Clinical gain of attachment has also been reported to be similar while comparing guided tissue regeneration (GTR) membrane and SECTG12,13 however, lesser post-operative recession has been observed with SECTG.13,14
It is possible to hypothesize that the use of SECTG in conjunction with OFD in treatment of supracrestal/horizontal osseous defects could lead to better clinical results; i.e. greater clinical attachment level gain, reduced probing pocket depth (PPD), and decreased post-surgical gingival recession.
Most of the reported studies which have examined the efficacy of SECTG along with OFD for treatment of horizontal bony defects have examined it in anterior segment,8,15,16 and in posterior segments as a treatment modality for furcation involvement.17 Thus, an attempt was made to assess the efficacy of SECTG along with OFD in the management of supracrestal defects of the posterior segments.
Materials and Methods
The study was designed as a randomized, split-mouth clinical trial, comparing the clinical treatment outcomes of the use of SECTG in conjunction with OFD to OFD in the treatment of horizontal osseous defects of posterior teeth. The study recruited 20 patients (10 males and 10 females, aged 18-56 years, with a mean age of 37.79 ± 10.58 years), with no dropout. All patients treated were medically stable, non-smokers with no contraindications to periodontal surgery, had not been subjected to any periodontal therapy for at least 6 months prior, and had no history of antibiotics use within 6 months prior to treatment.
To be included in the study, patients had to have radiographic evidence of at least two identical bilateral suprabony pockets with horizontal bone loss pattern, patients having an adequate band of keratinized tissue for ease in surgical manipulation and suturing. Following the initial therapy, the selected sites displayed probing pockets depth of ≥4 mm and clinical attachment loss of ≥4 mm and horizontal bone loss detected by radiographic examination (alveolar crest level [ACL] - cementoenamel junction [CEJ] distance ≥4 mm) at three adjacent posterior teeth. Based on inclusion criteria, an informed consent was obtained from patients selected for study. Initial therapy included scaling and root planning followed by oral hygiene instructions. Post 6 weeks of Phase 1 periodontal therapy, re-evaluation of patients was done. Based on inclusion criteria, before periodontal flap surgery, baseline parameters were recorded. All the surgeries were carried out and the measurements recorded by the same operator.
Clinical measures
All the selected patients underwent Phase 1 therapy. At study baseline, 6 months and 12 months after treatment, the following ancillary parameters were evaluated: Plaque index (PI),18 papillary bleeding index (PBI).19 Alginate impressions were recorded and study casts for each patient were prepared. Furthermore, customized acrylic occlusal stent with a groove (guide plane) was fabricated on all these study casts. The groove acted as a guide for the clinical measurements, which were done by using a straight periodontal probe (University of North Carolina, UNC - 15) (Figure 1). The PPD was measured using the gingival margin as a reference to the base of the periodontal pocket. The relative attachment level (RAL) as the distance from the apical end of stent to the base of the periodontal pocket. Gingival marginal level (GML) was measured from the apical most end of the stent to the crest of the gingival margin, with the help of periodontal probe.20 All the acrylic stents were secured on the prepared study casts for the entire duration of the study to minimize distortion.
Figure 1.
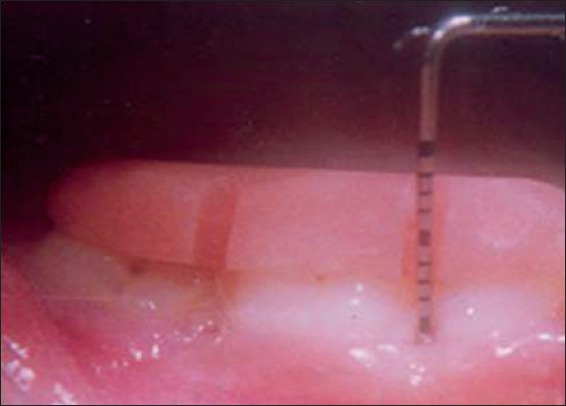
Customized acrylic occlusal stent with a groove (guide plane) and clinical measurements by using a straight periodontal probe (University of North Carolina, UNC -15).
Radiographic assessment
Routine diagnostic periapical radiographs were taken with the long cone paralleling technique. Baseline and 12 months follow-up radiographs were recorded. When measuring radiographic bone level (BL), the location of both ACL, and CEJ was determined.21 The CEJ position was identified according to Schei et al.22 The positions of ACL and CEJ were marked by a pencil on the radiographs and the distance ACL - CEJ (BL) was measured by a millimeter grid (Figure 2). Linear distances between the most coronal interproximal BL and the CEJ were obtained by counting the grids.23
Figure 2.
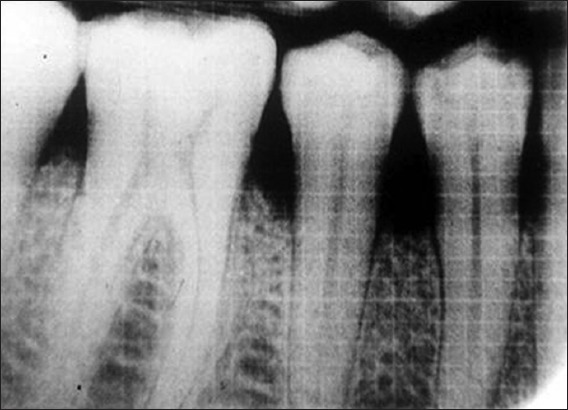
Measuring radiographic bone level, alveolar crest level and cementoenamel junction using millimeter grid.
Surgical protocol
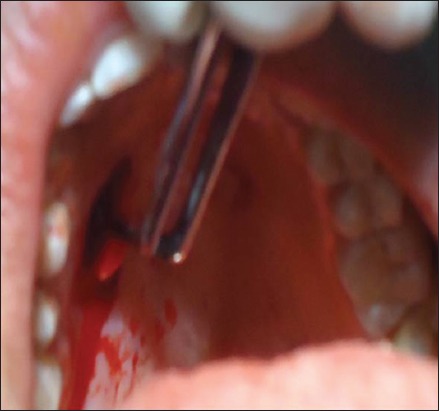
Patients were administered 2% lignocaine solution for obtaining anesthesia at the surgical site. Intracrevicular incisions were carried out at buccal and lingual aspects followed by full thickness mucoperiosteal flaps elevation (Figure 3). After the reflection of the flap, a sub-gingival calculus, plaque, pocket epithelium, and diseased granulation tissue were severed and surgical area was completely debrided. The SECTG was harvested from the palate (Figure 4).24 The dimension of the graft was adequate to cover the root surfaces up to the CEJ; the donor site was then secured with horizontal suturing technique. The harvested SECTG was trimmed to remove all visible epithelium, shaped, and placed under coronal part of buccal flap up to CEJ (Figure 5).
Figure 3.

Full thickness mucoperiosteal flaps elevated for thorough surgical debridement.
Figure 4.
Subepithelial connective tissue graft harvested from palate.
Figure 5.
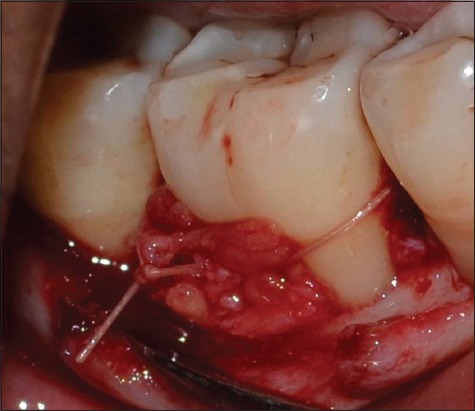
Harvested subepithelial connective tissue graft placed under coronal part of buccal flap up-to cementoenamel junction.
Surgical flaps were repositioned and primary closure was attained by the direct loop suturing technique using 3-0 silk suture (Mersilk-Ethicon, Division of Johnson and Johnson Ltd.) (Figure 6). The surgical and donor site were protected by placing a non-eugenol periodontal dressing (Coe-pack-GC America INC. ALSIP, IL, USA). Patients were given post-operative instructions.
Figure 6.

Surgical flaps repositioned to the pre-surgical level and sutured with 3-0 silk suture.
A similar surgical protocol was followed in control sites where only OFD was done without the use of SECTG.
Post-operative follow-up
Clinical examination of patients were done at 1-week post-surgery at the time of suture removal, all patients exhibited uneventful healing. Ancillary clinical parameters were recorded at 3 months, 6 months, and 12 months post-surgery, recording of clinical parameters and radiographic reassessment was done at 6 months and 12 months post-surgery. All along the patients received regular supportive periodontal therapy.
Statistical analysis
The means and standard deviations (mean ± standard deviation) values were calculated for all clinical and radiographic parameters.25 Student’s paired t-test was used to compare data from baseline with those at 6 months and 12 months in test sites and control sites.
Results
Clinical parameters
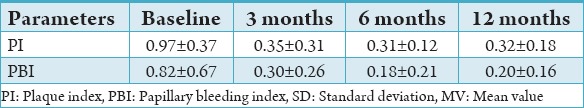
The full mouth mean PI and PBI scores decreased from baseline to 12 months follow-up. PI baseline 0.97 ± 0.37 to 12 months 0.32 ± 0.18 and PBI scores baseline 0.82 ± 0.67 to 12 months score 0.20 ± 0.16, When the scores were compared statistically using paired t-test and the difference was statistically significant (P > 0.05) in both the PI and PBI scores as shown in Table 1.
Table 1.
Ancillary clinical parameters: Mean plaque PI and PBI scores at baseline, at 3 months, at 6 months and at 12 months (MV±SD).
Comparison of baseline values
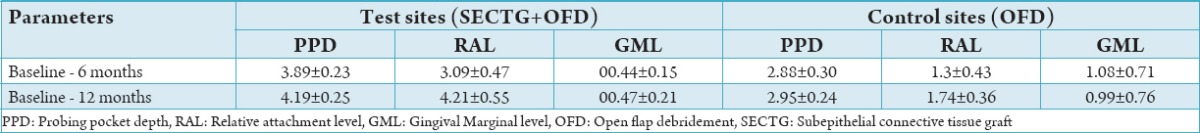
At baseline mean, PPD was 7.37 ± 0.23 mm in the test group and 6.94 ± 0.18. Mean RAL at baseline in the test group was 15.91 ± 0.45 and in control sites were 15.37 ± 0.39. The mean GML at baseline in the test group was 8.47 ± 0.13 and control sites was 8.04 ± 0.75 as shown in Table 2.
Table 2.
Clinical parameters: PPD, RAL and GML at baseline, at 6 months and at 12 months of both test sites (SECTG+OFD) and control sites (OFD) (MV±SD in mm).
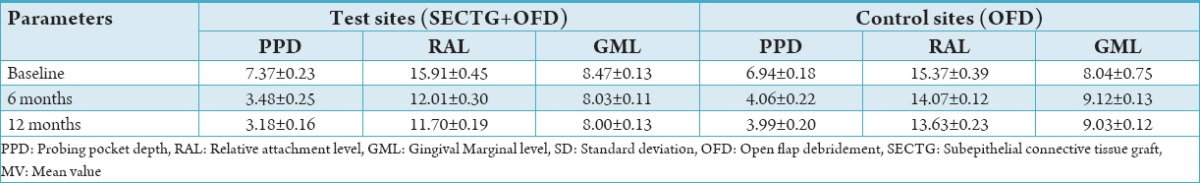
In the test group, the mean PPD from baseline to 6 months was 3.89 ± 0.23 and baseline to 12 months was 4.19 ± 0.25 both values were statistically significant. In the test group, the mean RAL from baseline to 6 months was 3.09 ± 0.47 which was not significant but baseline to 12 months was 4.21 ± 0.55 values were statistically significant. In the test group, the mean GML from baseline to 6 months was 0.44 ± 0.15 and baseline to 12 months was 0.47 ± 0.21 both values were statistically not significant. In control sites, PPD values were statistically significant in baseline to 6 and 12 months. RAL and GML does not show any significant change from baseline to 12 months at test site whereas in control site GML showed negative values both at 6 and 12 months compared to baseline thus implying presence of post-operative recession as shown in Table 3.
Table 3.
Comparative parameters from baseline to 6 months and baseline to 12 months.
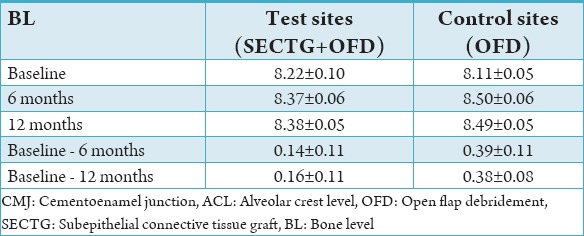
Radiographic parameters
The mean BL values at test sites baseline to 6 months is 0.14 ± 0.11 and baseline to 12 months is 0.16 ± 0.11 which were not statistically significant. Similarly at control sites, the baseline to 6 months is 0.39 ± 0.11 and baseline to 12 months is 0.38 ± 0.11 which were not statistically significant as shown in Table 4.
Table 4.
Radiographic assessment: BL=ACL−CEJ, ACL and CEJ in mm at baseline, at 6 months and at 12 months of both test sites (SECTG+OFD) and control sites (OFD) (MV±SD in mm).
Discussion
Specific surgical approaches have been reported to obtain primary flap closure and to preserve interdental and marginal gingival tissue loss. This study was a longitudinal 12 months test conducted with a prospective controlled, randomized design. The intent of the study was to clinically evaluate that, if the use of SECTG in conjunction with OFD versus the classically used approach of OFD in treatment of horizontal osseous defects, could lead to better clinical, and radiographic results; i.e. greater RAL gain, reduced PPD, decreased post-surgical gingival recession and supracrestal bone growth in the maxillary posterior, as well as the mandibular posterior region.
At the baseline examination, the various clinical variables did not show a statistical difference between the two groups. All participants of the present study showed good oral hygiene levels and healthy gingival conditions throughout the entire study period of 12 months as indicated by ancillary clinical parameters of PI and PBI scores. There were no significant differences in PI and sulcular bleeding index observed between control and experimental sites at any point during the study, suggesting that the different amounts clinical attachment gain between control and experimental sites were a result of the different treatment modalities tested and therefore unrelated to the amount of gingival inflammation present during healing.
Results revealed that both surgical treatments (OFD + SECTG and OFD alone) significantly improved the clinical parameters compared to the pre-surgical conditions; however, the addition of SECTG resulted in a significantly greater reduction in PPD and gain in RAL and a significantly lower gingival recession or apical displacement of GML both at 6 months and 12 months post-surgically.
The added benefit provided by SECTG is suggested by the greater RAL gain scores and the overall proportion of pockets undergoing complete closure (significantly greater).
SECTGs may have acted as a “natural” autogenous GTR membrane in this case, possibly allowing periodontal ligament cells, osteoblasts, and cementoblasts to repopulate the apical part of the wound.
The good results for RAL improvement obtained by using a connective tissue graft could be explained by the fact that in addition to providing a space for regenerating cells, the connective tissue graft may have better supported and protected the wound of the surgical site during the healing period.
A primary goal of periodontal therapy is to reduce PPD so as to limit the risk of local re-infection. Shallow pockets display a highly negative predictive value for future disease amelioration, whereas deep pockets in treated areas are a risk indicator for periodontal disease progression.26 In the present clinical study with an initial pocket range of 4-7 mm. At 6 months SECTG group showed (3.89 ± 0.23 mm) a greater mean PPD reduction compared with the (2.88 ± 0.30 mm) of OFD group. At 12 months period, the difference was not found to be significant. The mean PPD reductions observed in the present study for both groups are comparable to the results reported.8,27,28 Most of the improvements in clinical parameters were achieved during first 6 months post-surgery, and to a lesser extent at 12 months from baseline.
Horizontal bone loss represents 92% of the total bone loss in periodontal patients thus far exceeding the intrabony defects,29,30 which however have ironically received much surgical and regenerative therapeutic interventions, which in part can be attributed to the their favorable morphologic characteristic resulting in resolution associated with these treatment modalities.31
In clinical practice, OFD represents the non-resective surgical treatment of choice for horizontal bone defects, however, numerous attempts have been made32-36 for resolution of the defects.
The lack of significant supracrestal bone growth observed in this study is in agreement with the data from Jentsch and Purschwitz37 and Yilmaz et al.38 This finding is anticipated if we take into consideration that, there is a paucity of available space under the gingival flap in supra-alveolar-type defects to allow new bone formation. The present results agree with those previously reported in literature which demonstrate the efficacy of both treatment approaches, though statistical differences have been found with respect to improvement of various parameters between both arms of the experimental groups, long-term studies need to be conducted to prove the added benefits using SECTG in conjunction with OFD.
Conclusion
Within the confines of the present study, results revealed that the use of SECTG along with OFD compared to OFD alone resulted in significantly higher RAL gain and significantly lower post-surgical gingival recession. However, both techniques failed to show significant supracrestal bone growth. Therefore use of SECTG along with OFD, followed with regular maintenance therapy, has clinically predictable results in the treatment of periodontal horizontal osseous defects. Long-term clinical trials are warranted to further substantiate the efficacy of this technique.
Footnotes
Conflicts of Interest: None
Source of Support: Nil
References
- 1.Ramseier CA, Rasperini G, Batia S, Giannobile WV. Advanced reconstructive technologies for periodontal tissue repair. Periodontol 2000. 2012;59(1):185–202. doi: 10.1111/j.1600-0757.2011.00432.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Di Tullio M, Femminella B, Pilloni A, Romano L, D’Arcangelo C, De Ninis P, et al. Treatment of supra-alveolar-type defects by a simplified papilla preservation technique for access flap surgery with or without enamel matrix proteins. J Periodontol. 2013;84(8):1100–10. doi: 10.1902/jop.2012.120075. [DOI] [PubMed] [Google Scholar]
- 3.Palcanis KG. Surgical pocket therapy. Ann Periodontol. 1996;1(1):589–617. doi: 10.1902/annals.1996.1.1.589. [DOI] [PubMed] [Google Scholar]
- 4.Becker W, Becker BE, Caffesse R, Kerry G, Ochsenbein C, Morrison E, et al. A longitudinal study comparing scaling, osseous surgery, and modified Widman procedures: Results after 5 years. J Periodontol. 2001;72(12):1675–84. doi: 10.1902/jop.2001.72.12.1675. [DOI] [PubMed] [Google Scholar]
- 5.Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985;56(12):715–20. doi: 10.1902/jop.1985.56.12.715. [DOI] [PubMed] [Google Scholar]
- 6.Harris RJ. The connective tissue and partial thickness double pedicle graft: A predictable method of obtaining root coverage. J Periodontol. 1992;63(5):477–86. doi: 10.1902/jop.1992.63.5.477. [DOI] [PubMed] [Google Scholar]
- 7.Miller PD., Jr Root coverage using a free soft tissue autograft following citric acid application. Part 1: Technique. Int J Periodontics Restorative Dent. 1982;2(1):65–70. [PubMed] [Google Scholar]
- 8.Hirsch A, Brayer L, Shapira L, Goldstein M. Prevention of gingival recession following flap debridement surgery by subepithelial connective tissue graft: Consecutive case series. J Periodontol. 2004;75(5):757–61. doi: 10.1902/jop.2004.75.5.757. [DOI] [PubMed] [Google Scholar]
- 9.Harris RJ. Human histologic evaluation of root coverage obtained with a connective tissue with partial thickness double pedicle graft. A case report. J Periodontol. 1999;70(7):813–21. doi: 10.1902/jop.1999.70.7.813. [DOI] [PubMed] [Google Scholar]
- 10.Harris RJ. A comparison of 2 root coverage techniques: Guided tissue regeneration with a bioabsorbable matrix style membrane versus a connective tissue graft combined with a coronally positioned pedicle graft without vertical incisions. results of a series of consecutive cases. J Periodontol. 1998;69(12):1426–34. doi: 10.1902/jop.1998.69.12.1426. [DOI] [PubMed] [Google Scholar]
- 11.Pasquinelli KL. The histology of new attachment utilizing a thick autogenous soft tissue graft in an area of deep recession: A case report. Int J Periodontics Restorative Dent. 1995;15:248–57. [PubMed] [Google Scholar]
- 12.Ricci G, Silvestri M, Tinti C, Rasperini G. A clinical/statistical comparison between the subpedicle connective tissue graft method and the guided tissue regeneration technique in root coverage. Int J Periodontics Restorative Dent. 1996;16(6):538–45. [PubMed] [Google Scholar]
- 13.Tatakis DN, Trombelli L. Gingival recession treatment: Guided tissue regeneration with bioabsorbable membrane versus connective tissue graft. J Periodontol. 2000;71(2):299–307. doi: 10.1902/jop.2000.71.2.299. [DOI] [PubMed] [Google Scholar]
- 14.Trombelli L, Scabbia A, Tatakis DN, Checchi L, Calura G. Resorbable barrier and envelope flap surgery in the treatment of human gingival recession defects. Case reports. J Clin Periodontol. 1998;25(1):24–9. doi: 10.1111/j.1600-051x.1998.tb02359.x. [DOI] [PubMed] [Google Scholar]
- 15.Chavan RS, Tiwari IR, Bhongade ML, Jaiswal P, Deo VD. Open flap debridement in combination with subepithelial connective tissue graft for the prevention of post-operative recession: A report on a series of cases. Periodontal Pract Today. 2008;5(4):275–80. [Google Scholar]
- 16.Koudale SB, Charde PA, Bhongade ML. A comparative clinical evaluation of acellular dermal matrix allograft and sub-epithelial connective tissue graft for the treatment of multiple gingival recessions. J Indian Soc Periodontol. 2012;16(3):411–6. doi: 10.4103/0972-124X.100921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Belal MH, Al-Noamany FA, El-Tonsy MM, El-Guindy HM, Ishikawa I. Treatment of human class II furcation defects using connective tissue grafts, bioabsorbable membrane, and resorbable hydroxylapatite: A comparative study. J Int Acad Periodontol. 2005;7(4):114–28. [PubMed] [Google Scholar]
- 18.Turesky S, Gilmore ND, Glickman I. Reduced plaque formation by the chloromethyl analogue of victamine C. J Periodontol. 1970;41(1):41–3. doi: 10.1902/jop.1970.41.41.41. [DOI] [PubMed] [Google Scholar]
- 19.Mühlemann HR. Psychological and chemical mediators of gingival health. J Prev Dent. 1977;4:6–17. [PubMed] [Google Scholar]
- 20.Isidor F, Karring T, Attström R. Reproducibility of pocket depth and attachment level measurements when using a flexible splint. J Clin Periodontol. 1984;11(10):662–8. doi: 10.1111/j.1600-051x.1984.tb01314.x. [DOI] [PubMed] [Google Scholar]
- 21.Kiliç AR, Efeoglu E, Yilmaz S. Guided tissue regeneration in conjunction with hydroxyapatite-collagen grafts for intrabony defects. A clinical and radiological evaluation. J Clin Periodontol. 1997;24(6):372–83. doi: 10.1111/j.1600-051x.1997.tb00200.x. [DOI] [PubMed] [Google Scholar]
- 22.Schei O, Waerhaug J, Lovdal A, Arro A. Alveolar boneloss as related to oral hygiene and age. J Periodontol. 1959;30:7–16. [Google Scholar]
- 23.Nery EB, Olson JW, Henkin JM, Kalbfleisch JH. Film-holder device for radiographic assessment of periodontal tissues. J Periodontal Res. 1985;20(1):97–105. doi: 10.1111/j.1600-0765.1985.tb00416.x. [DOI] [PubMed] [Google Scholar]
- 24.Zucchelli G, Mele M, Stefanini M, Mazzotti C, Marzadori M, Montebugnoli L, et al. Patient morbidity and root coverage outcome after subepithelial connective tissue and de-epithelialized grafts: A comparative randomized-controlled clinical trial. J Clin Periodontol. 2010;7:728–38. doi: 10.1111/j.1600-051X.2010.01550.x. [DOI] [PubMed] [Google Scholar]
- 25.Mahajan BK. 5th ed. New Delhi: Jaypee Brothers; 1991. Book Method in Biostatistics. [Google Scholar]
- 26.Armitage GC. Periodontal diseases: Diagnosis. Ann Periodontol. 1996;1(1):37–215. doi: 10.1902/annals.1996.1.1.37. [DOI] [PubMed] [Google Scholar]
- 27.Nelson SW. Subperiosteal connective tissue grafts for pocket reduction and preservation of gingival esthetics: A case report. J Periodontol. 2001;72(8):1092–9. doi: 10.1902/jop.2001.72.8.1092. [DOI] [PubMed] [Google Scholar]
- 28.Castellani R, Wolffe GN, Renggli HH. Pocket elimination surgery with simultaneous connective tissue graft. A case report with 3-year follow-up. J Clin Periodontol. 2001;28(4):365–71. doi: 10.1034/j.1600-051x.2001.028004365.x. [DOI] [PubMed] [Google Scholar]
- 29.Jayakumar A, Rohini S, Naveen A, Haritha A, Reddy K. Horizontal alveolar bone loss: A periodontal orphan. J Indian Soc Periodontol. 2010;14(3):181–5. doi: 10.4103/0972-124X.75914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Persson RE, Hollender LG, Laurell L, Persson GR. Horizontal alveolar bone loss and vertical bone defects in an adult patient population. J Periodontol. 1998;69:348–56. doi: 10.1902/jop.1998.69.3.348. [DOI] [PubMed] [Google Scholar]
- 31.Garrett S, Bogle G. Periodontal regeneration: A review of flap management. Periodontol 2000. 1993;1:100–8. [PubMed] [Google Scholar]
- 32.Stahl SS, Froum SJ. Healing of human suprabony lesions treated with guided tissue regeneration and coronally anchored flaps. Case reports. J Clin Periodontol. 1991;18(1):69–74. doi: 10.1111/j.1600-051x.1991.tb01122.x. [DOI] [PubMed] [Google Scholar]
- 33.Kassolis JD, Bowers GM. Supracrestal bone regeneration: A pilot study. Int J Periodontics Restorative Dent. 1999;19(2):131–9. [PubMed] [Google Scholar]
- 34.Kotschy P, Laky M. Reconstruction of supracrestal alveolar bone lost as a result of severe chronic periodontitis. Five-year outcome: Case report. Int J Periodontics Restorative Dent. 2006;26(5):425–31. [PubMed] [Google Scholar]
- 35.Blumenthal NM. The effect of supracrestal tricalcium phosphate ceramic-microfibrillar collagen grafting on postsurgical soft tissue levels. J Periodontol. 1988;59(1):18–22. doi: 10.1902/jop.1988.59.1.18. [DOI] [PubMed] [Google Scholar]
- 36.Nemcovsky CE, Zahavi S, Moses O, Kebudi E, Artzi Z, Beny L, et al. Effect of enamel matrix protein derivative on healing of surgical supra-infrabony periodontal defects in the rat molar: A histomorphometric study. J Periodontol. 2006;77(6):996–1002. doi: 10.1902/jop.2006.050317. [DOI] [PubMed] [Google Scholar]
- 37.Jentsch H, Purschwitz R. A clinical study evaluating the treatment of supra-alveolar-type defects with access flap surgery with and without an enamel matrix protein derivative: A pilot study. J Clin Periodontol. 2008;35(8):713–8. doi: 10.1111/j.1600-051X.2008.01253.x. [DOI] [PubMed] [Google Scholar]
- 38.Yilmaz S, Kuru B, Altuna-Kiraç E. Enamel matrix proteins in the treatment of periodontal sites with horizontal type of bone loss. J Clin Periodontol. 2003;30(3):197–206. doi: 10.1034/j.1600-051x.2003.10190.x. [DOI] [PubMed] [Google Scholar]


