Abstract
Background:
Mouthwashes are an adjunct to, not a substitute for, regular brushing and flossing. Chlorohexidine is cationic bis-biguanide broad spectrum antiseptic with both anti-plaque and antibacterial properties. It has side-effects like brownish discoloration of teeth and dorsum of the tongue, taste perturbation, oral mucosal ulceration, etc. To compare the antiplaque efficacy of herbal and chlorohexidine gluconate mouthwash.
Materials and Methods:
A double-blinded parallel, randomized controlled clinical trial was conducted in the Department of Periodontics, MNR Dental College. Totally 100 preclinical dental students were randomized into three groups (0.2% chlorohexidine, Saline and herbal mouthwash). All the groups were made to refrain from their regular mechanical oral hygiene measures and were asked to rinse with given respective mouthwashes for 4 days. The gingival and plaque scores are evaluated on 1st day, and 5th day, and differences were compared statistically.
Results:
There was no significant difference in the gingival index (GI) and plaque index (PI) scores of the pre-rinsing scores of three groups and mean age of subjects in the three age groups, suggesting selected population for the three groups was homogenous. Mean GI and PI scores at the post rinsing stage were least for the Group A, followed by B and C. The difference of post rinsing PI and GI scores between Group A and Group B were statistically non-significant, which means anti-gingivitis and plaque inhibiting properties are similar for both.
Conclusion:
Within the limitations of this study chlorhexidine gluconate and herbal mouthwash (Hiora) showed similar anti plaque activity with latter showing no side effects.
Keywords: Chlorhexidine gluconate, disclosing agent, herbal mouth wash
Introduction
Dental plaque is host associated matrix enclosed biofilm with different bacterial populations, which adhere to tooth surfaces or other surfaces. Their end products bring about initiation of tissue destruction and alveolar bone loss. Effective plaque control measures will bring about change in quantity and composition of plaque biofilm.1 Personal oral hygiene has been maintained since ancient times as evident with the Chinese literature in 1600 BC using chewing sticks and Hippocrates2 reported the same around 460 BC. The mechanical plaque control involves tooth brushing either using a manual brush,3 motorized tooth brush or with the help of pressurized water pump system involving the use of water under pressure pumped through fine blunt needle or nozzle (irrigation both sub gingival and supragingival irrigation).
The chemical control of plaque includes organic or inorganic chemicals, which inhibit the accumulation, growth and survival of microbiota and debris. The main advantage of chemicals and their action depends on increased concentration in gingival crevicular fluid and saliva, which improves gingival health.4 A variety of products are available chemical plaque control, which are divided into first generation (e.g., phenols, quaternary ammonium compounds), second generation (e.g., bisbiguanides-chlorhexidine gluconate [CHXG]), third generation (e.g. delmopinol).5 CHXG is widely used with concentration of as mouth rinse. The antiplaque effect of CHXG and substantivity property has proven the gold standard efficacy of CHXG6 has adjunct to scaling when compared with other antiseptics it is cationic broad-spectrum antimicrobial agent, which mainly acts by preventing pellicle formation, and involves in destabilization of the outer bacterial membrane thereby preventing bacterial cell wall adsorption and binding of mature plaque.
This causes greater damage of membrane and the large molecular weight compounds are lost, coagulation and precipitation of cytoplasm occurs. The free CHXG molecules enter the cell and coagulate the proteins that cause decrease in activity of vital cell resulting in cell death. Until date, chlorhexidine is considered as the best plaque control agent. It has been shown that 0.2% CHXG mouth rinses prevents development of experimental gingivitis, in view of adverse effects of chlorhexidine7, alternate the study was conducted to find out efficacy of herbal mouthwash-Hiora (experimental group named as B) as compared with chlorhexidine mouthwash (positive control designated as A) with Saline (negative control designated as C). This study was designed to compare “de novo” plaque formation between the 3 groups A, B, C after 5 days refrainment from tooth brushing.
Materials and Methods
A randomized controlled clinical study was conducted in the Department of Periodontics, MNR Dental College, Sangareddy. It was an examiner blind, parallel designed clinical trial conducted on students of the college with each group having 50 students. Institutional Ethical Committee clearance and informed consent was taken was taken from all the participants before commencement of the study.
Based on the analysis of plaque re-growth studies, gingival index (GI) and plaque index (PI) index score differences were analyzed in three samples for which 150 students were included to provide sufficient sample size for detection. Materials used were chlorhexidine mouthwash (Rexidine, Warren Group, India), herbal mouthwash (Hiora, Himalaya, India), Saline, dispensing bottles, measuring cups and disclosing agent (Alphaplacr, DPI, India), scalars and polishing cups. Indices recorded were GI8 on all teeth except third molars with four sites per tooth-mesial, distal, facial/buccal and palatal/lingual and PI.9 Systematically healthy subjects with GI<1, at the time of examination, presence of 20 teeth with minimum of 5 teeth were enrolled in the study. Subjects with severe mal-aligned teeth, orthodontic appliances, fixed partial denture, removable partial denture, tobacco chewers, smokers and those individuals medically compromised were excluded. Study design: At the beginning of the study the GI and PI scores were recorded in order to assess the oral hygiene status of the subjects. All the recordings were done by the same examiner, the baseline scores were brought down near to 0 by supragingival scaling and polishing and it was confirmed with the of disclosing agent (Figures 1 and 2). Intra oral photographs were taken. Subjects were randomly allocated via simple random sampling technique (lottery method) to the three groups and were asked to refrain from mechanical plaque control (tooth brushing and flossing) but to rinse with mouthwashes as per prescribed therapeutic dose for 5 days. 10 ml of 0.2% chlorhexidine, 5 ml of Hiora and Saline were assigned to Group A, Group B, Group C respectively for rinsing twice daily for 1 min for 5 days. GI and PI scores were recorded by same examiner who was unaware of the mouthwashes, on the 6th day. Statistical comparison of GI and PI scores was done post rinsing for all the three groups by ANOVA and Student’s t-test using disclosing agent for PI. Side effects were evaluated from all the subjects by means of a questionnaire and clinical examination. Questionnaire included yes/no for pain, burning sensation, pruritus, dryness of mouth, taste disturbance, discoloration of teeth, feeling of bitter taste in mouth. The subjects were asked to evaluate the severity of side effects by rating them as mild, moderate or severe. With respect to taste disturbance, subjects were asked to specify which taste (salt, sour, bitter, sweet) had altered in perception.10 In clinical evaluation, the severity of soft tissue irritation, rated as none, change in color, desquamation or presence of aphthae. Discolorations were recorded as absent/present and if present, further classified as mild, moderate or severe (Figure 3). Photographs were taken of those who showed staining of teeth at the end of the study and thorough scaling and polishing was done for them. Subjects were then asked to return their normal oral hygiene measures after the completion of study period.
Figure 1.

Pre rinse clinical picture.
Figure 2.

Pre rinse with disclosing agent.
Figure 3.

Post rinse with disclosing agent.
Results
At baseline, there was no significant difference in GI and PI scores among the groups (P =0.969 and 0.427) respectively (Table 1).
Table 1.
Inter-group comparisons pre and post of GI and PI scores.
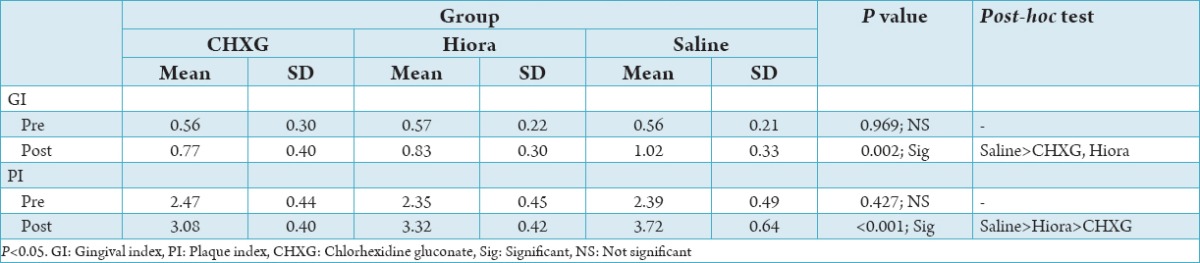
At follow-up or post, there was significant difference in the mean GI and PI scores (P =0.002) respectively. Post-hoc test showed that the mean GI was significantly higher for Saline group than CHXG and Hiora groups. No significant difference was seen between CHXG and Hiora groups. Similarly, post-hoc test showed that the mean PI was significantly higher for Saline followed by Hiora with least being CHXG group.
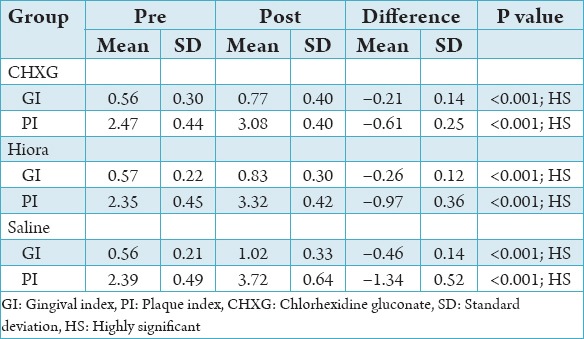
Tables 2 and 3 show, significant difference between CHXG versus Saline and Hiora versus Saline post rinse after 5th day in index and highly significant difference (P <0.001) was seen in PI in post rinse group after 5th day i.e., CHXG versus Saline and Hiora versus Saline signifies that CHXG and Hiora are effective in removal of plaque than the control. The intra group comparison shows the scores were significantly lower for the three groups at the baseline when compared with the post rinse scores. The results of this study signifies a greater increase in scores of both plaque and gingival indices and the intra group comparison shows there was a significant difference between the two groups and CHXG showed more significant decrease in plaque and gingival scores when compared with the other two. The baseline scores were lower for the GI and PI scores when compared with follow-up or post in all the groups (Graph 1).
Table 2.
Post-hoc test additional details.
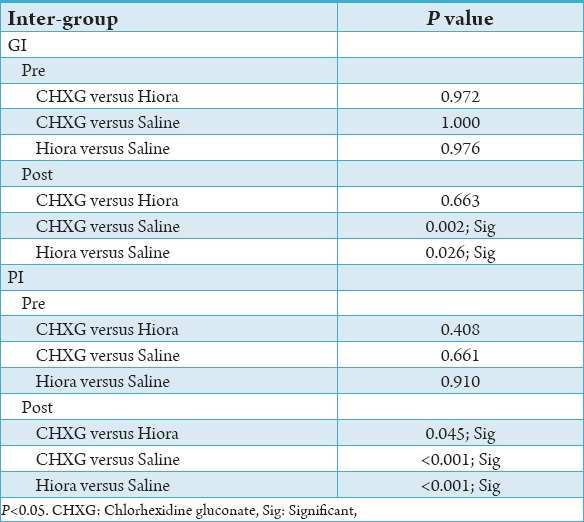
Table 3.
Intra-group (pre and post) comparison.
Graph 1.
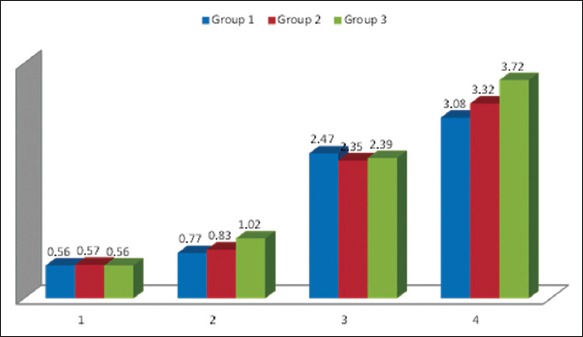
Means of all the three groups. (1) Pre gingival index, (2) Post gingival index, (3) Pre plaque index, (4) Post plaque index.
Discussion
Ayurvedic drugs have been used to treat oral diseases including periodontal diseases. Oral rinses with herbal composition are used in periodontal therapy to control plaque and inflammation (Figure 4). According to Dalirsani et al.,11 Anupama et al.12 herbal mouth wash have advantages such as decreased side-effects and more economical when compared to chlorhexidine. (Nagavalli Piper betle) shows anti-inflammatory, anti-oxidant, anti-microbial properties. Pilu (Salvadora persica) shows anti-oxidant activity, it has peppermint that contains menthol, which activates cold sensitive TRPM8 receptors in mucosa and it is also used as primary agent in toothpastes and chewing gums, peppermint in Wikipedia). Here an attempt was made to use herbal mouth wash (Hiora) and study was conducted to evaluate the efficacy of herbal mouth wash containing pilu (S. persica), bibhitaka (Terminalia bellirica), Nagavalli, ela (cardamom), pipperment satva, bellenic myrobalan (vibhitaki compared to chlorhexidine digluconate). Chlorhexidine was developed in 1950, which is considered as gold standard6 till date and most anti plaque agent. However the long-term use of chlorhexidine is limited by altered taste perception and staining of tooth with prolonged usage, as reported by Fardal and Turnbull.13 To overcome the limitation of chlorhexidine usage, herbal mouthwash was advocated to the patients and the plaque gingival diseases are measured. The results of the present study showed there was no significant difference in pre rinsing scores of 3 groups there was no significant difference in mean age of subjects in all three groups indicating homogenous distribution. Mean GI and PI scores at the post rinsing stage were least for the group A, followed by Group B and Group C. In all the three groups’ reformation of plaque was evident in all individuals within 24 h after thorough oral prophylaxis by self-evaluation patient and same reported in the questionnaire given. Because of its effervescent property could have better access into the interproximal areas and embrasures where the plaque could be thin and incompletely organized. A major drawback of chlorhexidine was staining of tongue. The antiplaque efficacy of CHXG was attributed by the retention of the compound CHXG in the oral cavity and its slow release.14 Although the effect of the plaque re growth and gingival inflammation observed with CHXG was superior to herbal mouthwash, the latter did not exhibit any other side effects. The similar antiplaque activity was observed as the post rinsing PI and GI scores showed no significant difference statistically. In contrast to this study Almas et al.15 conducted a study antimicrobial activity of about eight mouthwashes and concluded that mouthwash containing CHXG were with maximum antibacterial activity and mouthwash with miswak extract containing CHXG were with maximum antibacterial activity and mouthwash with miswak extract (pilu) with low antibacterial activity. In accordance with our study Scherer et al.16 compared herbal mouthwash and water and concluded that herbal mouthwash has better efficacy when compared to normal distilled water. Within limitations of the study, such as insufficient period of time to evaluate the anti-gingivitis property of herbal mouthwash as the 4 day plaque model was considered and further are directed towards anti-plaque, and gingivitis efficacy of herbal mouthwash. The anti-plaque activity of herbal and CHXG mouthwashes can even further help in post rinsing of periodontal surgeries.
Figure 4.
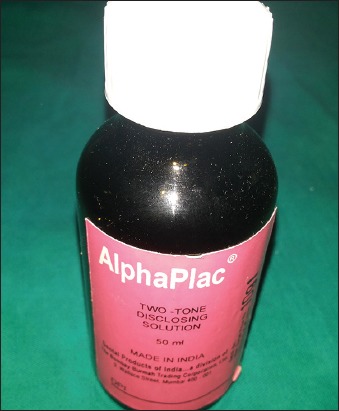
Disclosing agent.
Conclusion
As plaque control is essential for the prevention of inflammatory periodontal diseases, mouthwashes can prevent plaque formation and thus help in maintaining healthy periodontium. Within limitations of the study, CHXG and herbal mouthwash (Hiora) showed similar anti-plaque activity with latter showing no side-effects.
Footnotes
Conflicts of Interest: None
Source of Support: Nil
References
- 1.Haffajee AD, Smith C, Torresyap G, Thompson M, Guerrero D, Socransky SS. Efficacy of manual and powered toothbrushes (II). Effect on microbiological parameters. J Clin Periodontol. 2001;28(10):947–54. doi: 10.1034/j.1600-051x.2001.028010947.x. [DOI] [PubMed] [Google Scholar]
- 2.Carranza F, Shklar G. History of Periodontology. London: Quintessence; 2003. Ancient India and China; pp. 9–13. [Google Scholar]
- 3.Kim JH. A review of mechanical dental plaque control 2012. [Last accessed on 2014 Sep 7]. http://www.surgicalrestorative.com/articles/2012/12/a-review-of-mechanical-dental-plaque-control.html .
- 4.Ciancio SG, Mather ML, McMullen JA. An evaluation of minocycline in patients with periodontal disease. J Periodontol. 1980;51(9):530–4. doi: 10.1902/jop.1980.51.9.530. [DOI] [PubMed] [Google Scholar]
- 5.Mhaske M, Samad BN, Jawade R, Bhansali A. Chemical agents in control of dental plaque in dentistry: An overview of current knowledge and future challenges. Adv Appl Sci Res. 2012;3(1):268–72. [Google Scholar]
- 6.Flötra L, Gjermo P, Rölla G, Waerhaug J. Side effects of chlorhexidine mouth washes. Scand J Dent Res. 1971;79(2):119–25. doi: 10.1111/j.1600-0722.1971.tb02001.x. [DOI] [PubMed] [Google Scholar]
- 7.Jones CG. Chlorhexidine: Is it still the gold standard? Periodontol 2000. 1997;15:55–62. doi: 10.1111/j.1600-0757.1997.tb00105.x. [DOI] [PubMed] [Google Scholar]
- 8.Löe H. The Gingival Index, the Plaque Index and the Retention Index Systems. J Periodontol. 1967;38(Suppl):610–6. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 9.Quigley GA, Hein JW. Comparative cleansing efficiency of manual and power brushing. J Am Dent Assoc. 1962;65:26–9. doi: 10.14219/jada.archive.1962.0184. [DOI] [PubMed] [Google Scholar]
- 10.Parwani SR, Parwani RN, Chitnis PJ, Dadlani HP, Prasad SV. Comparative evaluation of anti-plaque efficacy of herbal and 0.2% chlorhexidine gluconate mouthwash in a 4-day plaque re-growth study. J Indian Soc Periodontol. 2013;17(1):72–7. doi: 10.4103/0972-124X.107478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dalirsani Z, Aghazadeh M, Adibpour M, Amirrchagmaghi M, Pakfetrat A. In vitro comparison of the antibacterial activity of ten herbal extracts against Steptococcus mutans with chlorhexidine. J Appl Sci. 2011;11(5):878–82. [Google Scholar]
- 12.Anupama D, Anil M, Surangama D. A clinical trial to evaluate the effect of triphala as a mouthwash in comparison with chlorhexidine in chronic generalized periodontitis patient. Indian J Dent Adv. 2010;2:243–7. [Google Scholar]
- 13.Fardal O, Turnbull RS. A review of the literature on use of chlorhexidine in dentistry. J Am Dent Assoc. 1986;112(6):863–9. doi: 10.14219/jada.archive.1986.0118. [DOI] [PubMed] [Google Scholar]
- 14.Addy M. Chlorhexidine compared with other locally delivered antimicrobials. A short review. J Clin Periodontol. 1986;13(10):957–64. doi: 10.1111/j.1600-051x.1986.tb01434.x. [DOI] [PubMed] [Google Scholar]
- 15.Almas K, Skaug N, Ahmad I. An in vitro antimicrobial comparison of miswak extract with commercially available non-alcohol mouthrinses. Int J Dent Hyg. 2005;3(1):18–24. doi: 10.1111/j.1601-5037.2004.00111.x. [DOI] [PubMed] [Google Scholar]
- 16.Scherer W, Gultz J, Lee SS, Kaim J. The ability of an herbal mouthrinse to reduce gingival bleeding. J Clin Dent. 1998;9(4):97–100. [PubMed] [Google Scholar]


