Abstract
Objective
To determine the relationship between preoperative hypoalbuminemia and the development of complications after gynecological cancer surgery, as well as postoperative bowel function and hospital stay.
Methods
The medical records of 533 patients with gynecological cancer surgery at Konkuk University Hospital between 2005 and 2013 were reviewed. Serum albumin level <3.5 g/dL was defined as hypoalbuminemia. All perioperative complications within 30-days after surgery, time to resumption of normal diet and length of postoperative hospital stay, were analyzed. Regression models were used to assess predictors of postoperative morbidity.
Results
The median age was 49 years (range, 13 to 85 years). Eighty patients (15%) had hypoalbuminemia. Hypoalbuminemic patients had significantly higher consumption of alcohol >2 standard drinks per day, lower American Society of Anesthesiologist score, higher frequency of ascites, and more advanced stage compared with non-hypoalbuminemic patients. Overall complication rate within 30-days after surgery was 20.3% (108 out of 533). Hypoalbuminemic patients were more likely to develop postoperative complications compared to non-hypoalbuminemic patients (34.3% vs. 17.8%, P=0.022), and had significantly longer median time to resumption of normal diet (3.3 [1-6] vs. 2.8 [0-15] days, P=0.005) and length of postoperative hospital stay (0 [7-50] vs. 9 [1-97] days, P=0.014). In multivariate analysis, age >50 (odds ratio [OR], 2.478; 95% confidence interval [CI], 1.310 to 4.686; P=0.005), operation time (OR, 1.006; 95% CI, 1.002 to 1.009; P=0.006), and hypoalbuminemia (OR, 2.367; 95% CI, 1.021 to 5.487; P=0.044) were the significant risk factor for postoperative complications.
Conclusion
Preoperative hypoalbuminemia in patients with elective surgery for gynecologic malignancy is an independent predictor of 30-days postoperative complications. Identification of this subset and preoperative optimization of nutritional status may improve surgical outcomes.
Keywords: Genital neoplasms, female; Hypoalbuminemia; Nutritional status; Postoperative complications
Introduction
The potential risk of postsurgical complications is especially important for gynecologic cancer patients. Any delay in installation of adjunctive chemotherapy or radiotherapy in a timely fashion affects outcomes negatively [1,2]. There is evidence in colorectal cancer [2] and recently in ovarian cancer patients [3] that indicates a potentially negative effect of delay in adjuvant chemotherapy after surgery. In addition, post-operative complications add substantially to the cost of management in the post-operative setting [4]. Therefore, preoperative risk evaluation to recognize patients at a higher risk of postoperative morbidity and mortality are critical.
In the cancer patients, malnutrition may appear simultaneously with the disease and it may also adversely affect surgical outcomes [5,6]. Serum albumin is a good and a simple variable correlated with patients' nutritional status [7]. It has been demonstrated that hypoalbuminemia was associated with adverse surgical outcomes in patients who are undergoing cardiac [8] and major gastrointestinal surgeries [9,10,11]. However, the effect of hypoalbuminemia on postoperative complications incidence after gynecological cancer surgery has not been fully quantified. Hence, this study is aimed to determine the relationship between pre-operative hypoalbuminemia and the occurrence of 30-day morbidity after gynecologic cancer surgery, as well as postoperative bowel function and hospital stay.
Materials and methods
1. Patients
The patients in this study were obtained from a computerized database of gynecologic cancer patients who were diagnosed and treated in Konkuk University Hospital between May 2005 and December 2013. All patients who had had their elective surgery in our institution were considered eligible to be included. Those referred to a re-staging procedure after initial surgery at an outside hospital were also included. Only patients with a confirmed final diagnosis of malignancy based on the International Classification of Diseases 10th revision, and final diagnosis codes were included in the analysis. The patients who did not check preoperative albumin levels, who did not receive follow-up cares in our institution, and/or who had operations for recurrent tumors were excluded. The study was validated by the institutional review board of the center (KUH1040040).
2. Variables
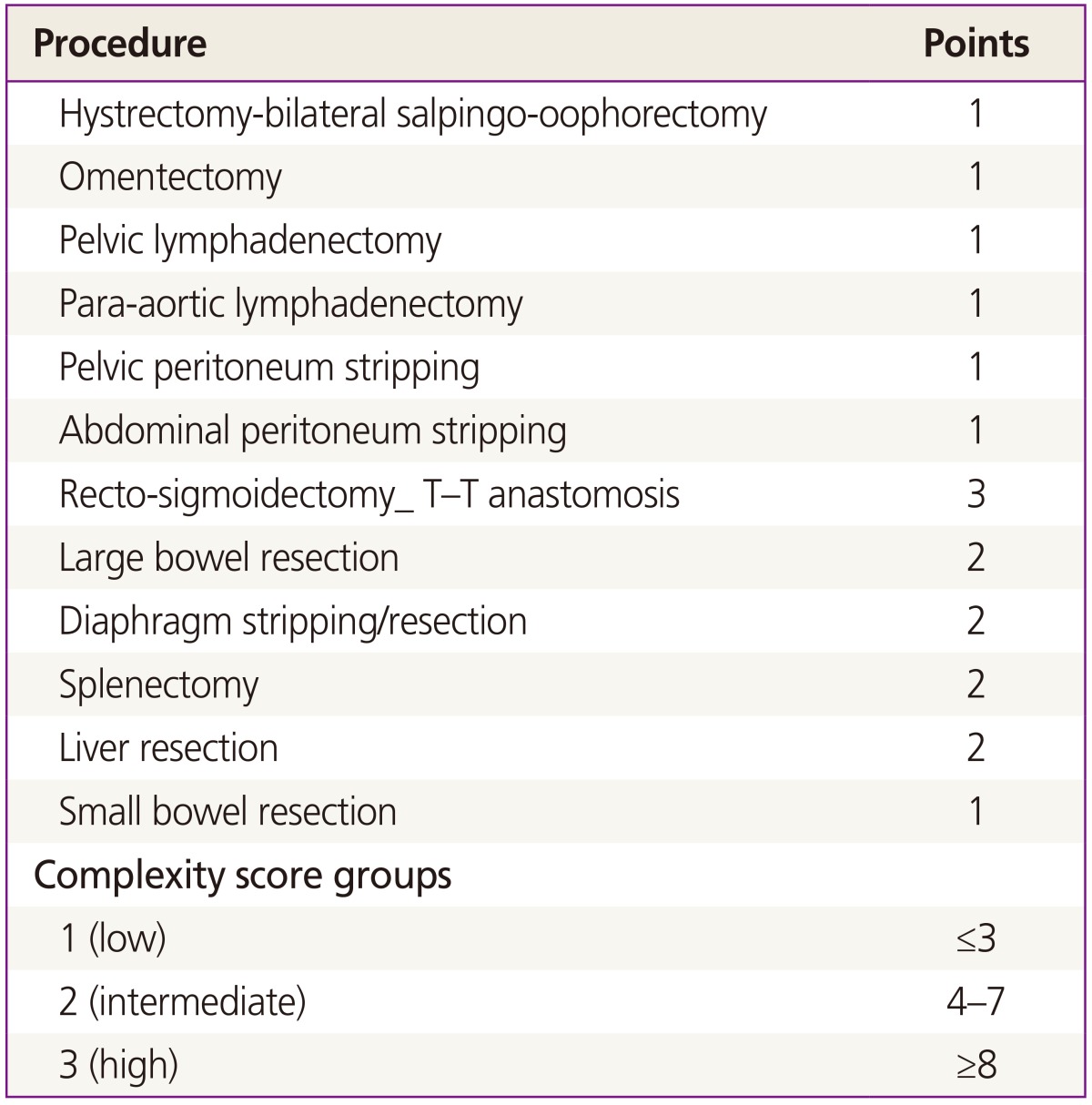
The clinicopathological and follow-up data were collected from the medical records. Preoperative variables for analysis were patients' age, parity, body mass index (BMI), consumption of alcohol >2 standard drinks per day, current smoking status, physical status according to the American Society of Anesthesiologist (ASA) classification system, comorbidity status, history of chemotherapy or radiotherapy prior to surgery, presence of ascites prior to surgery, preoperative lab findings including serum glutamic oxaloacetic transaminase, serum glutamic pyruvic transaminase, hematocrit, platelet count, prothrombin time, and activated partial thromboplastin time. Ascites were defined as the presence of ascites on two-thirds of the abdominopelvic computed tomography scan cuts (i.e., ascites on most cuts) [12]. Comorbidity was scored and categorised using a modification of the Charlson comorbidity index (Table 1) [13]. Postoperative variables for analysis were extent of surgical procedures, type of surgical approach, operative time, estimated blood loss (EBL), primary pathology, International Federation of Gynecology and Obstetrics (FIGO) stage, time to resumption of normal diet, and length of hospital stay. We assessed the extent of each surgery using surgical complexity score (SCS) [14]. Based on the number and complexity of the surgical procedures, patients were allotted to three groups: low, intermediate, or high (Table 2). Total operative time was recorded as the time from the first skin incision to the last skin closure. The EBL was recorded as the amount of blood in gauze and the amount of difference between suction bottled solution and saline irrigation used in surgery. The operative time and EBL were referred to anesthesia record drawn up by an anesthesiologist.
Table 1. Characteristics of non-hypoalbuminemic and hypoalbuminemic patients.
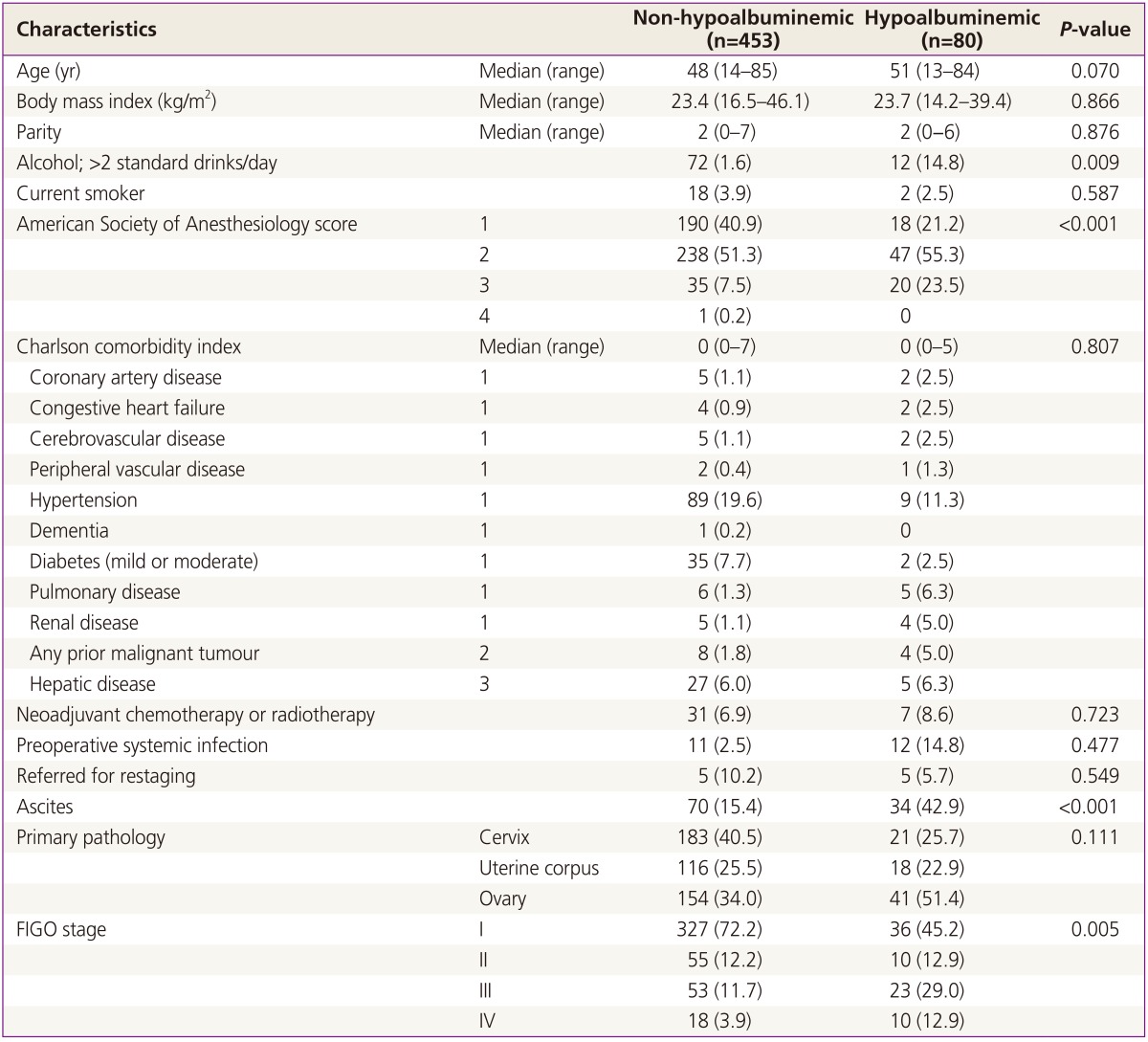
Values are presented as median (range) or number (%).
FIGO, International Federation of Gynecology and Obstetrics.
Table 2. Surgical complexity scoring system based upon complexity and number of surgical procedures performed.
3. Statistical analysis
The patients were categorized into two groups (non-hypoalbuminemia vs. hypoalbuminemia) according to the level of pre-operative serum albumin. Serum albumin less than 3.5 g/dL was defined as hypoalbuminemia. Our primary outcome was the development of 30-days postoperative complications. All intraoperative and postoperative complications within 30 days of operation were registered and categorized according to the previous reports (Table 3) [15,16]. Univariate and multivariate analyses of potential predictors for postoperative morbidity were performed by using binary logistic regression. To identify independent predictors of postoperative morbidity, statistically significant variables identified by univariate analysis were analyzed further by multivariate logistic regression analysis. Point estimates are expressed as odds ratios (ORs), and 95% confidence intervals (95% CI) are provided. Continuous variables that were normally distributed were presented as mean±standard deviation. Variables that were not normally distributed were presented as median (range) or median (interquatile range). Mean values between groups were compared using the Student t-test for normally distributed data or the Mann-Whitney U-test for data not normally distributed. Frequency distributions were compared using the chi-squared test or the Fisher exact test. A P-value <0.05 according to 2-sided tests indicated significant difference. All analyses were performed using IBM SPSS ver. 19.0 (IBM Corp., Armonk, NY, USA).
Table 3. Surgical procedures and related factors.
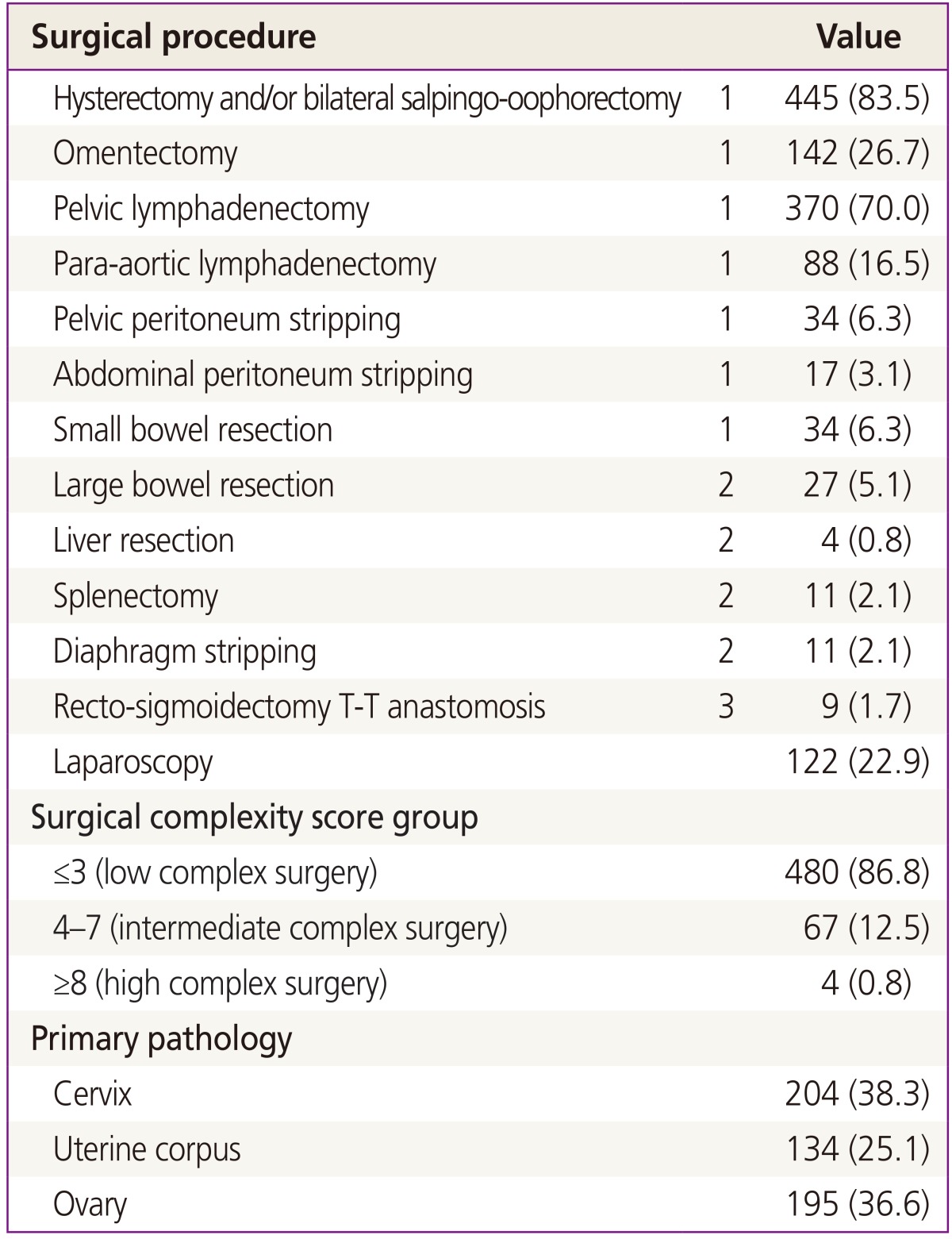
Values are presented as number (%).
Results
1. Patient characteristics
During the study period, 739 patients were newly diagnosed with gynecologic cancer and treated in our institution. Out of these 739 patients, 558 of them had elective surgery. In total, 533 patients satisfied all of the inclusion criteria. The characteristics of the enrolled patients are summarized in Table 1. The median age was 49 years (range, 13 to 85 years). Four hundred fifty-three patients (85.0%) were noted to have a normal albumin level, whereas 80 (15.0%) showed hypoalbuminemia. The mean albumin value of the hypoalbuminemic group was 3.05 g/dL, and the mean value for the normal albumin group was 4.06 g/dL. The demographic parameters of the entire cohort are presented in Table 1. There were no significant differences between the age, BMI, parity, proportion of patients smoking, history of neoadjuvant chemotherapy or radiotherapy, referral for restaging, primary pathology, and Charlson comorbidity index in two groups. However, the hypoalbuminemic group had a significantly higher proportion of alcohol intake, lower ASA score, higher frequency of ascites, and more advanced FIGO stage.
2. Surgical procedures
Details of the surgical procedures and related factors are shown in Table 3. The hysterectomy and/or salpingo-oophorectomy followed by pelvic/para-aortic/groin lymph node dissection were the most common procedures. One hundred twenty two (22.9%) patients had a laparoscopic procedure and 480 (86.8%) underwent surgery with low SCS. Two hundred four had cervical cancer, 134 had uterine corpus cancer, and 195 had ovarian cancer.
3. Surgical outcomes of non-hypoalbuminemic and hypoalbuminemic patients
Thirty days postoperative complication was detected in 108 patients (20.3%). Postoperative morbidity was 0.6% (n=3). Further details regarding the overall complications are depicted in Table 4. Infectious complications were diagnosed in 48 patients (9%); 31 surgical site infections, 6 sepsis, 5 anastomotic leakage, and 6 pneumonia. Hypoalbuminemic patients had a significantly higher rate of postoperative complication (34.3% vs. 17.8%, P=0.022).
Table 4. Clinical outcomes of non-hypoalbuminemic and hypoalbuminemic patients after gynecologic surgery.
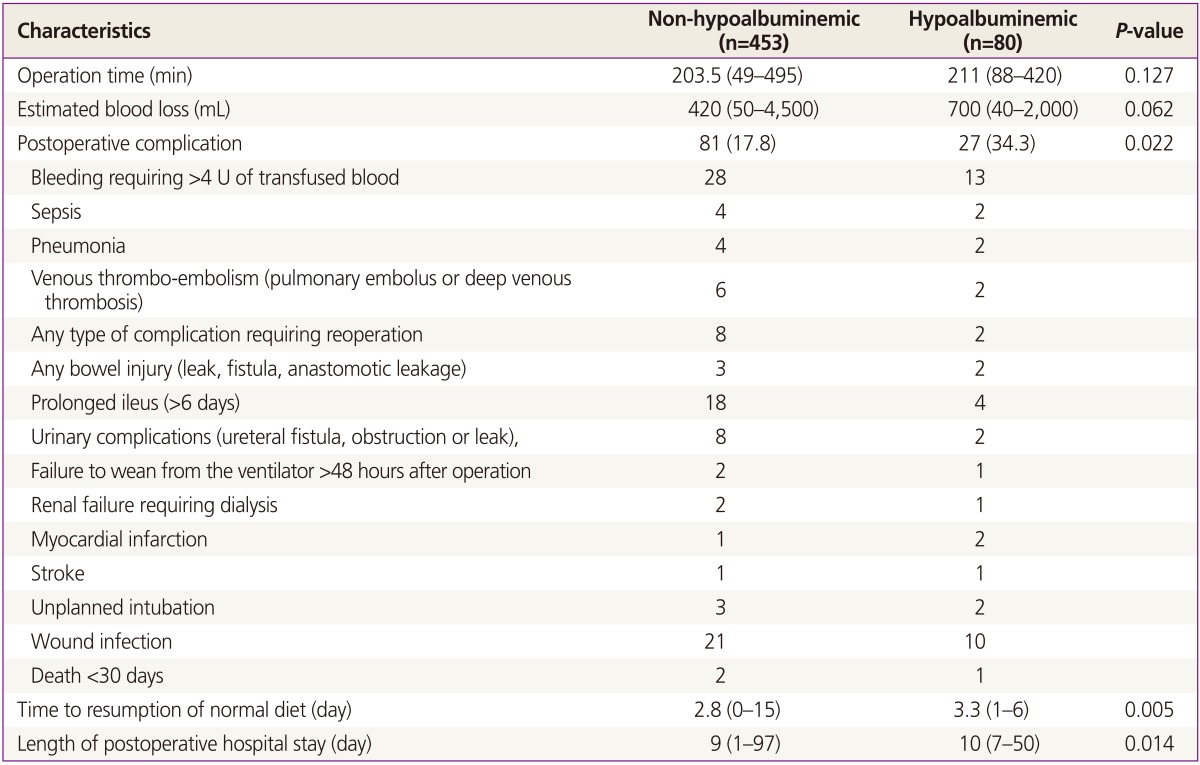
Values are presented as median (range), number (%), or number.
Hypoalbuminemic group had significantly longer median time to resumption of normal diet (3.3 [1-6] vs. 2.8 [0-15] days, P=0.005) and length of postoperative hospital stay (0 [7-50] vs. 9 [1-97] days, P=0.014). Median EBL tends to differ between normal and hypoalbuminemic groups with 420 (50-4,500) vs. 700 (40-2,000) mL, although they are not statistically significant (P=0.062).
4. Univariate and multivariate analyses of postoperative complications
Univariate analysis revealed age, ASA score, type of surgical approach, SCS, operation time, EBL, and hypoalbuminemia as risk factors for the development of postoperative complications (Table 5). In multivariate analysis, age >50 years (OR, 2.478; 95% CI, 1.310 to 4.686; P=0.005), operation time (OR, 1.006; 95% CI, 1.002 to 1.009; P=0.006), and hypoalbuminemia (OR, 2.367; 95% CI, 1.021 to 5.487; P=0.044) were the significant risk factor for postoperative complications.
Table 5. The relationship between the clinical characteristics of the patients and the development of postoperative complications analyzed using a multivariate model.
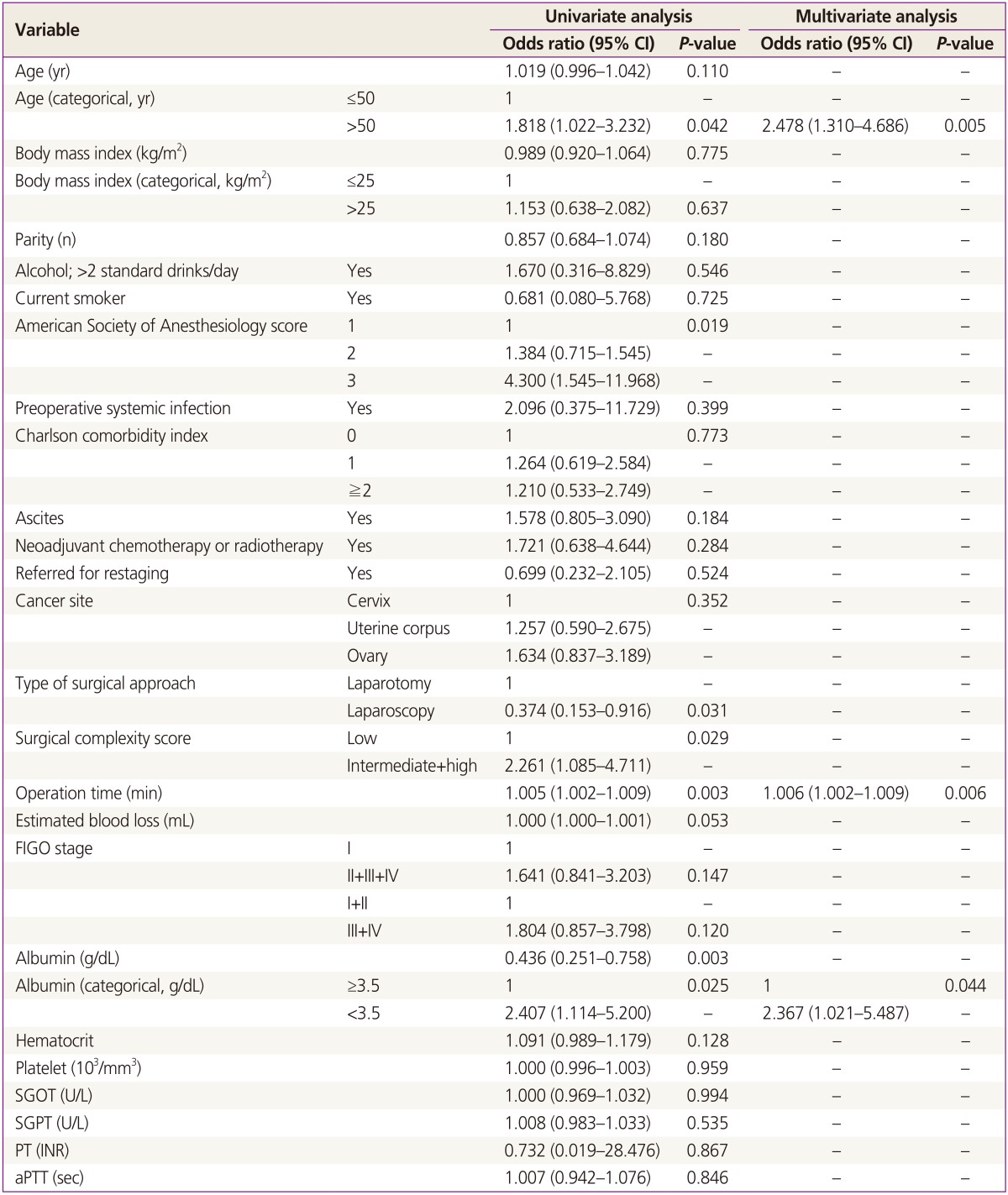
CI, confidence interval; FIGO, International Federation of Gynecology and Obstetrics; SGOT, serum glutamic oxaloacetic transaminase; SGPT, serum glutamic pyruvic transaminase; PT, prothrombin time; aPTT, activated partial thromboplastin time.
Discussion
In the present study, hypoalbuminemia is revealed as an independent risk factor for 30 days postoperative complications following gynecologic cancer surgery after adjusting for age, ASA score, type of surgical approach, SCS, operation time, and EBL. Cancer patients are prone to malnutritional due to cancer-induced increased metabolic rate, decreased nutritional intake, and cancer cachexia [17]. There may also be an increased whole protein turnover and subsequent body nitrogen loss [16]. Tumor necrosis factor-alpha is considered to be the main mediator of cancer cachexia as it is responsible for altered metabolic rates and it leads to decreased hepatic protein synthesis [15]. Albumin has a long half-life of 20 days, so the metabolic effects on its concentration reflect prolonged malnourishment, as in cancer patients. Although serum albumin concentration may also be influenced by other factors such as trauma and surgical stress, it is generally accepted to be a good marker for malnutrition in previous national cancer studies [18,19].
Hypoalbuminemia has been reported to be associated with greater risk of negative surgical outcome in non-gynecologic surgery [11,18,20,21]. However, there is sparse literature addressing the effect of hypoalbuminemia on the risk of postoperative morbidity in patients who are undergoing gynecologic cancer surgery [16]. The National Veterans Affairs Surgical Risk Study, from 54,215 major general surgery cases examining 30-day morbidity and mortality, found that serum albumin level was the strongest predictor of morbidity and mortality [18]. Similarly, hypoalbuminemia was found to be the predictor of poor surgical outcomes of colon cancer and it was the poor indicator of long-term survival after curative resection in 2,529 patients [22]. In the retrospective study of 187 bladder cancer patients undergoing radical cystectomy by Lambert et al., they reported that patients with low preoperative albumin levels had an increased overall mortality and cancer-specific mortality risk than those with normal albumin levels [21]. Our finding is consistent with the recent study using national surgical quality improvement program (NSQIP), the large national database in the United States [16]. Uppal et al. [16] reported that preoperative albumin levels <3 g/dL identify a population of patients at a very high-risk of experiencing perioperative morbidity after gynecologic cancer surgery.
It is remarkable that BMI was not significantly different between non-hypoalbuminemic and hypoalbuminemic patients. Serum albumin level is a better indicator to detect protein-energy malnutrition than anthropomorphic markers of nutritional status [23]. Protein-energy malnutrition is not necessarily accompanied by lower body weight and it may not be clinically knowable, but it is related to adverse surgical outcomes [24]. Hypoalbuminemia is related to poor tissue healing, impaired collagen synthesis in the surgical wounds or at the anastomotic sites [25,26], and compromised immune responses [27,28]. These factors together could explain the higher risk of surgical site infections and anastomotic leakage, and remote infections such as pneumonia in hypoalbuminemic patients. In the present study, an inclination towards delayed recovery of postoperative bowel function has also been found in hypoalbuminemic patients. This may be because such patients develop more postoperative complications, and because hypoalbuminemia causes swelling and edema of the bowel [29], resulting in paralytic ileus [30]. Prolonged postoperative hospitalization in hypoalbuminemic patients may result from higher rates of postoperative complication and delayed recovery of bowel function.
Apropose of the treatment of preoperative hypoalbuminemia, no published studies have been able to show any benefit of intravenous albumin infusion on postoperative morbidity [31]. This may be due to the insufficient albumin replacement or increased leakage of synthetic albumin into the extravascular spaces [11]. Moreover, infused albumin will degrade rapidly and the underlying causes of adverse surgical outcomes were not corrected by infusion itself [32]. However, a recent randomized trial reported the perioperative supplement of diet was helpful to the outcomes in malnourished patients with gastrointestinal cancer [33]. This supports the growing consensus that enteral nutrition support may be the preferred approach [34]. Similarly, the American Society for Parenteral and Enteral Nutrition guidelines [35] and the European guidelines [36] recommend the enteral perioperative nutritional support in violently malnourished patients for 7 to 14 days preoperatively. Patients at a severe nutritional risk are defined as having at least one of the followings: weight loss more than 10% to 15% within 6 months, BMI less than 18.5 kg/m2, Subjective Global Assessment Grade C [37], or serum albumin below 3 g/dL.
Given the high incidence of postoperative complications in hypoalbuminemic patients, these patients should either be nutritionally supported or be considered with alternative treatment strategies that delay a potentially complicated surgery. In ovarian cancer patients with large volume of carcinomatosis, which generally induces a high catabolic state and decreased oral intake secondary to nausea and bloating, enteral feeding difficulty is common. Primary debulking surgery in this population may lead to a high postoperative complication rate and a subsequent delay in installation of adjuvant chemotherapy, which affects the overall survival negatively [3]. Recent randomized trial has demonstrated the non-inferiority of neoadjuvant chemotherapy followed by interval debulking compared with primary debulking surgery [30], and this approach is plausible in this high-risk population.
There are some limitations given its retrospective nature of study design. However, the present study is the one of the largest study to evaluate the potential role of hypoabluminemia in patients undergoing gynecologic cancer surgery. The number of subjects was sufficiently large to analyze the correlation between serum albumin level and postoperative morbidity and to compare the surgical outcomes of hypoalbuminemic and non-hypoalbuminemic patients. In addition, our study is meaningful in terms of the first study to target the Korean people because there can be difference of outcomes between races. Prospective validation study to determine which markers of nutrition are valid as well as the possible benefit of various preoperative nutritional strategies are required for future study.
In conclusion, the present study suggested that preoperative serum albumin level helps identify a high-risk of surgical population. This report addresses the importance of preoperative albumin levels as they may relate to a patient's nutritional status and disease state. Identification of this subgroup and preoperative optimization of nutritional status or using alternative treatment strategies may improve surgical outcomes in this population potential for complications after gynecologic cancer surgery.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Donat SM, Shabsigh A, Savage C, Cronin AM, Bochner BH, Dalbagni G, et al. Potential impact of postoperative early complications on the timing of adjuvant chemotherapy in patients undergoing radical cystectomy: a high-volume tertiary cancer center experience. Eur Urol. 2009;55:177–185. doi: 10.1016/j.eururo.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 2.Biagi JJ, Raphael MJ, Mackillop WJ, Kong W, King WD, Booth CM. Association between time to initiation of adjuvant chemotherapy and survival in colorectal cancer: a systematic review and meta-analysis. JAMA. 2011;305:2335–2342. doi: 10.1001/jama.2011.749. [DOI] [PubMed] [Google Scholar]
- 3.Eskander R, Java J, Tewari K, Burger R, Monk B. Negative survival impact associated with >25 day interval from surgical cytoreduction to initiation of systemic therapy in advanced ovarian carcinoma: a Gynecologic Oncology Group ancillary data study. Gynecol Oncol. 2013;130:e22–e23. [Google Scholar]
- 4.Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell DA., Jr Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;199:531–537. doi: 10.1016/j.jamcollsurg.2004.05.276. [DOI] [PubMed] [Google Scholar]
- 5.Sungurtekin H, Sungurtekin U, Balci C, Zencir M, Erdem E. The influence of nutritional status on complications after major intraabdominal surgery. J Am Coll Nutr. 2004;23:227–232. doi: 10.1080/07315724.2004.10719365. [DOI] [PubMed] [Google Scholar]
- 6.Miner TJ, Brennan MF, Jaques DP. A prospective, symptom related, outcomes analysis of 1022 palliative procedures for advanced cancer. Ann Surg. 2004;240:719–726. doi: 10.1097/01.sla.0000141707.09312.dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fuhrman MP, Charney P, Mueller CM. Hepatic proteins and nutrition assessment. J Am Diet Assoc. 2004;104:1258–1264. doi: 10.1016/j.jada.2004.05.213. [DOI] [PubMed] [Google Scholar]
- 8.de la Cruz KI, Bakaeen FG, Wang XL, Huh J, LeMaire SA, Coselli JS, et al. Hypoalbuminemia and long-term survival after coronary artery bypass: a propensity score analysis. Ann Thorac Surg. 2011;91:671–675. doi: 10.1016/j.athoracsur.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 9.Nisar PJ, Appau KA, Remzi FH, Kiran RP. Preoperative hypoalbuminemia is associated with adverse outcomes after ileoanal pouch surgery. Inflamm Bowel Dis. 2012;18:1034–1041. doi: 10.1002/ibd.21842. [DOI] [PubMed] [Google Scholar]
- 10.Hennessey DB, Burke JP, Ni-Dhonochu T, Shields C, Winter DC, Mealy K. Preoperative hypoalbuminemia is an independent risk factor for the development of surgical site infection following gastrointestinal surgery: a multi-institutional study. Ann Surg. 2010;252:325–329. doi: 10.1097/SLA.0b013e3181e9819a. [DOI] [PubMed] [Google Scholar]
- 11.Lohsiriwat V, Lohsiriwat D, Boonnuch W, Chinswangwatanakul V, Akaraviputh T, Lert-Akayamanee N. Pre-operative hypoalbuminemia is a major risk factor for postoperative complications following rectal cancer surgery. World J Gastroenterol. 2008;14:1248–1251. doi: 10.3748/wjg.14.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Axtell AE, Lee MH, Bristow RE, Dowdy SC, Cliby WA, Raman S, et al. Multi-institutional reciprocal validation study of computed tomography predictors of suboptimal primary cytoreduction in patients with advanced ovarian cancer. J Clin Oncol. 2007;25:384–389. doi: 10.1200/JCO.2006.07.7800. [DOI] [PubMed] [Google Scholar]
- 13.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 14.Aletti GD, Santillan A, Eisenhauer EL, Hu J, Aletti G, Podratz KC, et al. A new frontier for quality of care in gynecologic oncology surgery: multi-institutional assessment of short-term outcomes for ovarian cancer using a risk-adjusted model. Gynecol Oncol. 2007;107:99–106. doi: 10.1016/j.ygyno.2007.05.032. [DOI] [PubMed] [Google Scholar]
- 15.Khuri SF, Daley J, Henderson W, Hur K, Demakis J, Aust JB, et al. The Department of Veterans Affairs' NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg. 1998;228:491–507. doi: 10.1097/00000658-199810000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Uppal S, Al-Niaimi A, Rice LW, Rose SL, Kushner DM, Spencer RJ, et al. Preoperative hypoalbuminemia is an independent predictor of poor perioperative outcomes in women undergoing open surgery for gynecologic malignancies. Gynecol Oncol. 2013;131:416–422. doi: 10.1016/j.ygyno.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 17.Di Saia PJ, Creasman WT. Clinical gynecologic oncology. Philadelphia (PA): Elsevier/Saunders; 2012. [Google Scholar]
- 18.Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri SF. Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the National VA Surgical Risk Study. Arch Surg. 1999;134:36–42. doi: 10.1001/archsurg.134.1.36. [DOI] [PubMed] [Google Scholar]
- 19.Goldwasser P, Feldman J. Association of serum albumin and mortality risk. J Clin Epidemiol. 1997;50:693–703. doi: 10.1016/s0895-4356(97)00015-2. [DOI] [PubMed] [Google Scholar]
- 20.Rady MY, Ryan T, Starr NJ. Clinical characteristics of preoperative hypoalbuminemia predict outcome of cardiovascular surgery. JPEN J Parenter Enteral Nutr. 1997;21:81–90. doi: 10.1177/014860719702100281. [DOI] [PubMed] [Google Scholar]
- 21.Lambert JW, Ingham M, Gibbs BB, Given RW, Lance RS, Riggs SB. Using preoperative albumin levels as a surrogate marker for outcomes after radical cystectomy for bladder cancer. Urology. 2013;81:587–592. doi: 10.1016/j.urology.2012.10.055. [DOI] [PubMed] [Google Scholar]
- 22.Lai CC, You JF, Yeh CY, Chen JS, Tang R, Wang JY, et al. Low preoperative serum albumin in colon cancer: a risk factor for poor outcome. Int J Colorectal Dis. 2011;26:473–481. doi: 10.1007/s00384-010-1113-4. [DOI] [PubMed] [Google Scholar]
- 23.Apelgren KN, Rombeau JL, Twomey PL, Miller RA. Comparison of nutritional indices and outcome in critically ill patients. Crit Care Med. 1982;10:305–307. doi: 10.1097/00003246-198205000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Blackburn GL, Harvey KB. Prognostic strength of nutritional assessment. Prog Clin Biol Res. 1981;77:689–697. [PubMed] [Google Scholar]
- 25.Ward MW, Danzi M, Lewin MR, Rennie MJ, Clark CG. The effects of subclinical malnutrition and refeeding on the healing of experimental colonic anastomoses. Br J Surg. 1982;69:308–310. doi: 10.1002/bjs.1800690604. [DOI] [PubMed] [Google Scholar]
- 26.Testini M, Margari A, Amoruso M, Lissidini G, Bonomo GM. The dehiscence of colorectal anastomoses: the risk factors. Ann Ital Chir. 2000;71:433–440. [PubMed] [Google Scholar]
- 27.Rivadeneira DE, Grobmyer SR, Naama HA, Mackrell PJ, Mestre JR, Stapleton PP, et al. Malnutrition-induced macrophage apoptosis. Surgery. 2001;129:617–625. doi: 10.1067/msy.2001.112963. [DOI] [PubMed] [Google Scholar]
- 28.Reynolds JV, Redmond HP, Ueno N, Steigman C, Ziegler MM, Daly JM, et al. Impairment of macrophage activation and granuloma formation by protein deprivation in mice. Cell Immunol. 1992;139:493–504. doi: 10.1016/0008-8749(92)90088-7. [DOI] [PubMed] [Google Scholar]
- 29.Margarson MP, Soni N. Serum albumin: touchstone or totem? Anaesthesia. 1998;53:789–803. doi: 10.1046/j.1365-2044.1998.00438.x. [DOI] [PubMed] [Google Scholar]
- 30.Mattei P, Rombeau JL. Review of the pathophysiology and management of postoperative ileus. World J Surg. 2006;30:1382–1391. doi: 10.1007/s00268-005-0613-9. [DOI] [PubMed] [Google Scholar]
- 31.Rubin H, Carlson S, DeMeo M, Ganger D, Craig RM. Randomized, double-blind study of intravenous human albumin in hypoalbuminemic patients receiving total parenteral nutrition. Crit Care Med. 1997;25:249–252. doi: 10.1097/00003246-199702000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Rothschild MA, Oratz M, Schreiber SS. Serum albumin. Hepatology. 1988;8:385–401. doi: 10.1002/hep.1840080234. [DOI] [PubMed] [Google Scholar]
- 33.Moskovitz DN, Kim YI. Does perioperative immunonutrition reduce postoperative complications in patients with gastrointestinal cancer undergoing operations? Nutr Rev. 2004;62:443–447. doi: 10.1111/j.1753-4887.2004.tb00016.x. [DOI] [PubMed] [Google Scholar]
- 34.Gramlich L, Kichian K, Pinilla J, Rodych NJ, Dhaliwal R, Heyland DK. Does enteral nutrition compared to parenteral nutrition result in better outcomes in critically ill adult patients? A systematic review of the literature. Nutrition. 2004;20:843–848. doi: 10.1016/j.nut.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 35.Huhmann MB, August DA. Nutrition support in surgical oncology. Nutr Clin Pract. 2009;24:520–526. doi: 10.1177/0884533609335375. [DOI] [PubMed] [Google Scholar]
- 36.Weimann A, Braga M, Harsanyi L, Laviano A, Ljungqvist O, Soeters P, et al. ESPEN Guidelines on Enteral Nutrition: Surgery including organ transplantation. Clin Nutr. 2006;25:224–244. doi: 10.1016/j.clnu.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 37.Jeejeebhoy KN, Detsky AS, Baker JP. Assessment of nutritional status. JPEN J Parenter Enteral Nutr. 1990;14(5 Suppl):193S–1936. doi: 10.1177/014860719001400509. [DOI] [PubMed] [Google Scholar]


