Abstract
Objective
The aim of this study was to evaluate the prognostic value of squamous cell carcinoma antigen (SCC-Ag) and the optimal cut-off value for predicting recurrence in cervical squamous cell carcinoma patients with complete remission after primary treatment.
Methods
We reviewed the records of 783 cervical squamous cell cancer patients who underwent primary therapy and showed complete remission at our institution between January 2000 and April 2014. A receiver operating characteristic curve was used to determine the optimal SCC-Ag threshold to predict recurrence. Cox regression model for disease free survival was used to assess differences in outcome.
Results
The median follow-up period was 41.2 months, and 154 patients (19.7%) had recurrent disease. The median pretreatment and posttreatment SCC-Ag level was 2.6 ng/mL (range, 0.1 to 532.0 ng/mL) and 0.7 ng/mL (range, 0.0 to 46.8 ng/mL), respectively. Both pretreatment and posttreatment SCC-Ag levels were higher in the recurrence group (P=0.017 and P=0.039). Optimal cut-off value of pretreatment and posttreatment SCC-Ag for predicting recurrence was 1.86 ng/mL (area under the curve, 0.663; P=0.000), and 0.9 ng/mL (area under the curve, 0.581; P=0.002), respectively. In the multivariate Cox regression model, pretreatment SCC-Ag >1.86 ng/mL (odds ratio, 2.11; 95% confidence interval, 1.38 to 3.22; P=0.001) and posttreatment SCC-Ag >0.9 ng/mL (odds ratio, 1.64; 95% confidence interval, 1.18 to 2.28; P=0.003) were significantly associated with poor disease free survival.
Conclusion
Patients with pretreatment SCC-Ag >1.86 ng/mL or posttreatment SCC-Ag >0.9 ng/mL should be considered at high risk for cancer recurrence after complete remission, and therefore, closer surveillance is needed.
Keywords: Cervical squamous cell cancer, Cut-off value, Disease-free survival, Squamous cell carcinoma-related antigen
Introduction
Carcinoma of the uterine cervix is the second most common cancer among women in developing countries and the fourth most common cancer in women worldwide [1]. The incidence and mortality of cervical cancer have been greatly reduced due to screening programs and vaccination [1]. However, cervical cancer is still one of the major causes of cancer deaths in women worldwide. Among different histological subtypes of cervical cancer, squamous cell carcinoma is the most common, accounting for about 80% of cervical cancer cases.
Squamous cell carcinoma antigen (SCC-Ag) is the most commonly used serum tumor marker for squamous cell cervical cancer [2,3]. Most studies reported that elevated pretreatment SCC-Ag levels correlate with extent of disease such as tumor diameter, depth of cervical stromal invasion, lymphovascular space invasion, parametrial involvement, and lymph node metastasis [4,5,6,7,8,9,10]. Monitoring of SCC-Ag during radiotherapy and/or chemotherapy reflects both the tumor response to the treatment and the clinical outcome of patients [11,12,13]. SCC-Ag has also been recognized as a sensitive indicator of recurrence [14,15].
The clinical relevance of pretreatment SCC-Ag level is still debated [16]. Some studies reported that it has no prognostic value [2,17,18], and some other studies reported that it is associated with disease free survival or overall survival [4,5,6,7,10,19]. Several studies reported variable cut off values of pretreatment SCC-Ag level for predicting cervical cancer recurrence, but most of the studies included limited patient groups considering the cancer stage or primary treatment modalities. The purpose of this study is to investigate the prognostic value and the optimal cut off value of pretreatment and posttreatment SCC-Ag level for predicting cancer recurrence in cervical squamous cell carcinoma patients who have achieved complete remission after primary treatment, regardless of the cancer stage and primary treatment modality.
Materials and methods
We retrospectively reviewed the records of total 783 patients with squamous cell carcinoma of the uterine cervix who had achieved complete remission after primary treatment at the Department of Obstetrics and Gynecology of Chonnam National University Hospital between January 2000 and April 2014. Patients were considered eligible for the study if they fulfilled the following criteria: histologically confirmed squamous cell carcinoma by punch biopsy, loop electrosurgical excision procedure, or hysterectomy specimen; patients in whom SCC-Ag levels were checked before and after primary treatment; and patients who had achieved complete response after primary treatment. Patients with underlying disease that can influence the SCC-Ag level, such as chronic liver disease or renal disease, benign lesions of the lung, or skin disease were excluded.
Primary treatment was selected considering the clinical stage of disease, age, and underlying disease in the patient. In patients with early stage cervical cancer (IA to IIA), surgery-based treatment was performed. Patients with locally advanced cervical cancer (IIB to IV) underwent radiotherapy (RT) only or concurrent chemotherapy with radiation therapy (CCRT). Adjuvant radiotherapy or CCRT after surgery was performed in patients who had one or more intermediate-risk factors (large tumor size, deep cervical stromal invasion, and lymph-vascular space involvement) or high-risk factors (positive lymph node involvement, microscopic parametrial invasion, and positive resection margins with the tumor). Cisplatin-based chemotherapy was administered in all cases that received CCRT.
Serum SCC-Ag level was checked at the time of diagnosis of cervical cnacer (pretreatment SCC-Ag level) and at the first visit after the completion of treatment (posttreatment SCC-Ag level). Clinical stage was determined according to the guidelines of the International Federation of Gynecology and Obstetrics (FIGO). Tumor size determined as the largest diameter of the primary tumor was evaluated by computed tomography (CT), magnetic resonance imaging (MRI), or hysterectomy specimen. Status of lymph node involvement was confirmed by either pathological verification of the surgical specimen or it was defined as nodal size >1 cm on CT or MRI [20,21]. Biochemical response was defined as the change in SCC-Ag levels before and after primary treatment. Positive biochemical response was defined when the SCC-Ag level was reduced, and biochemical failure was defined when there were two consecutive increases in the SCC-Ag level above 1 ng/mL than immediately before or elevation above 1.5 ng/mL. The rest of the responses were defined as negative biochemical responses.
Follow-up after primary treatment was performed approximately every 3 months for the first 2 years, every 6 months for the next 3 years, and every year thereafter. During the routine follow-up, imaging studies including CT or MRI were performed each year. Imaging and biopsy were performed when tumor recurrence was suspected based on the clinical finding or imaging study. Local recurrence was diagnosed by biopsy, and distant metastasis was diagnosed by imaging studies. Disease free survival (DFS) was defined as the time elapsed between the initiation of primary treatment and first detection of cancer recurrence or the date of the last visit for patients with no evidence of disease. The study protocol was evaluated and approved by the institutional review board at Chonnam National University Hospital.
Statistical analysis was performed using IBM SPSS ver. 21.0 (IBM Corp., Armonk, NY, USA). Statistical comparison was carried out using Student's t-test or Pearson chi-square test. To determine the sensitivity, specificity, and the optimal cut-off values of the parameters, receiver operating characteristic (ROC) curve analysis was performed. Variables showing a significant association with DFS were included in the multivariate analysis based on the Cox proportional-hazard model. Distant DFS curves were plotted using the Kaplan-Meier method. All reported P-values are two-sided, and P-values <0.05 were considered statistically significant.
Results
Seven hundred and eighty-three patients with squamous cell carcinoma of the uterine cervix who had achieved complete response after primary treatment were included. The median age of the patients was 58 years (range, 27 to 98 years) and the median follow-up period was 41.2 months (range, 1.0 to 165.9 months). The median pretreatment and posttreatment SCC-Ag level was 2.6 ng/mL (range, 0.1 to 532 ng/mL) and 0.7 ng/mL (range, 0 to 46.8 ng/mL), respectively. Five-year disease free survival and 5-year survival rate were 76.1% and 98.5%, respectively.
During the follow-up period, 154 patients (19.7%) experienced cervical cancer recurrence. Median SCC-Ag level at recurrence was 2.0 ng/mL (range, 0.2 to 117.0 ng/mL). The patient characteristics according to the presence of recurrent disease are shown in Table 1. Both pretreatment and posttreatment SCC-Ag levels were higher in the recurrence group (P=0.017 and P=0.039 respectively). The percentages of advanced FIGO stage, tumor >4 cm in diameter, and positive lymph node involvement were also significantly higher in the recurrence group. Negative biochemical response or failure was more frequently observed in the recurrence group. The distribution of treatment modalities was different among the two groups. The rate of primary surgery was significantly lower, and on the contrary, the rate of CCRT utilization was significantly higher in the recurrence group.
Table 1. Patient characteristics according to cancer recurrence.
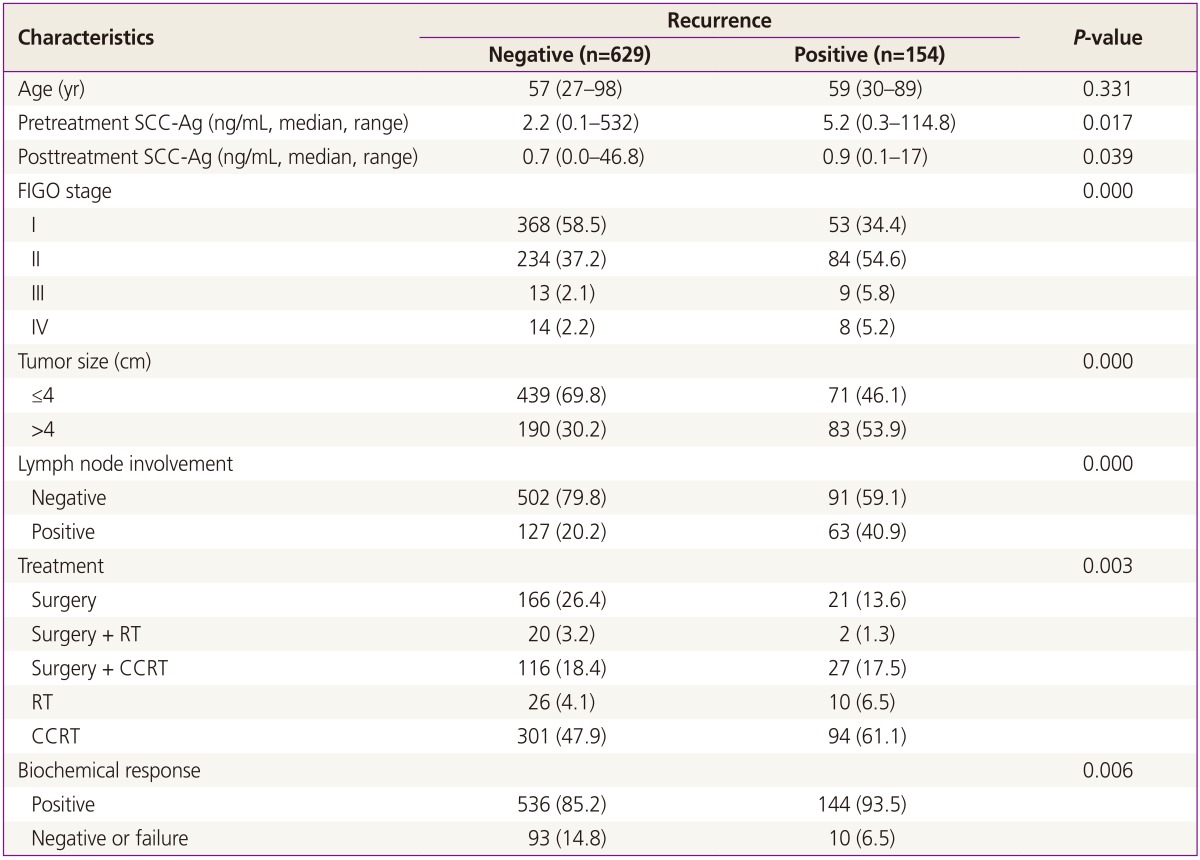
Values are presented as median (range) or number (%).
SCC-Ag, squamous cell carcinoma antigen; FIGO, International Federation of Gynecology and Obstetrics; RT, radiotherapy; CCRT, concurrent chemotherapy and radiotherapy.
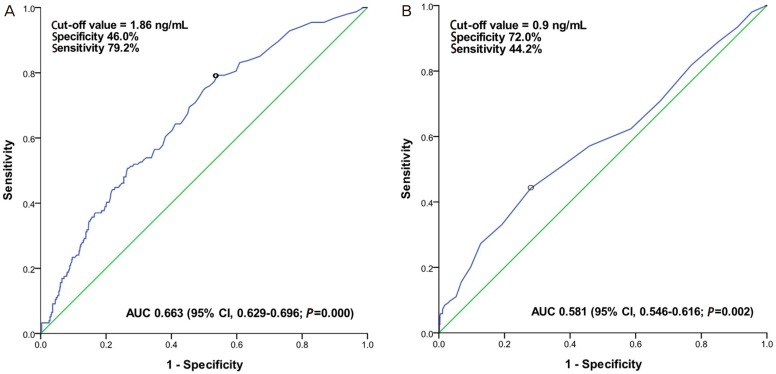
ROC curve analysis was used to obtain the optimal cut-off point values for pretreatment and posttreatment SCC-Ag levels for predicting cancer recurrence (Fig. 1). In this analysis, both pretreatment and posttreatment SCC-Ag levels had a statistically significant influence on predicting cancer recurrence (area under the curve=0.663 and 0.581 respectively, P=0.000 and 0.002 respectively). After studying the ROC analysis results and considering the best sensitivity and specificity, the optimal cut-off value of pretreatment and posttreatment SCC-Ag level was 1.86 ng/mL (sensitivity 79.2%, specificity 46.0%) and 0.9 ng/mL (sensitivity 44.2%, specificity 72.0%), respectively.
Fig. 1. Receiver operating characteristic curve for pretreatment squamous cell carcinoma antigen (SCC-Ag) level (A), and posttreatment SCC-Ag level (B) for predicting recurrence. Optimal cut-off value of pretreatment and posttreatment SCC-Ag for predicting tumor recurrence was 1.86 and 0.9 ng/mL, respectively.
AUC, area under the curve; CI, confidence interval.
Univariate and multivariate analyses for DFS are shown in Table 2. In the multivariate Cox regression model, pretreatment SCC-Ag >1.86 ng/mL (odds ratio [OR], 2.11; 95% confidence interval [CI], 1.38 to 3.22; P=0.001) and posttreatment SCC-Ag >0.9 ng/mL (OR, 1.64; 95% CI, 1.18 to 2.28; P=0.003) were identified as independent risk factors associated with poor disease free survival. FIGO stage III to IV (OR, 1.74; 95% CI, 1.38 to 3.22; P=0.035), tumor size >4 cm (OR, 1.57; 95% CI, 1.09 to 2.26; P=0.015), and positive lymph node involvement (OR, 1.45; 95% CI, 1.01 to 2.07; P=0.043) were also associated with poor disease free survival.
Table 2. Univariate and multivariate analyses for disease free survival.
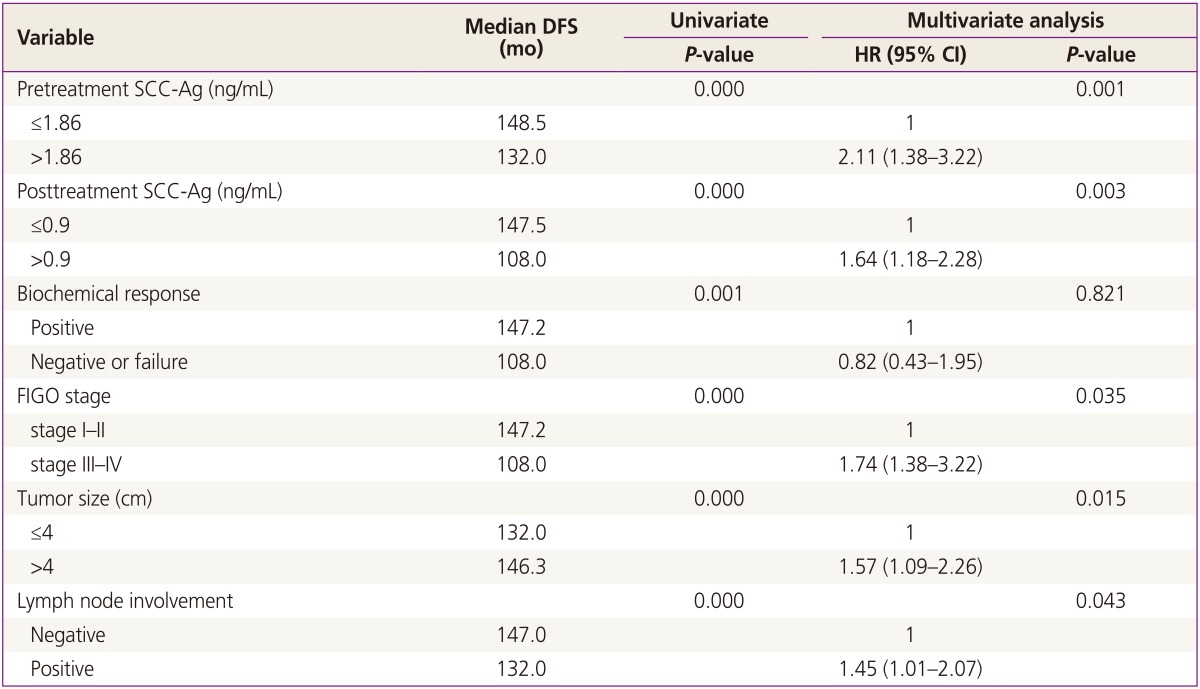
DFS, disease free survival; HR, hazard ratio; CI, confidence interval; SCC-Ag, squamous cell carcinoma antigen; FIGO, International Federation of Gynecology and Obstetrics.
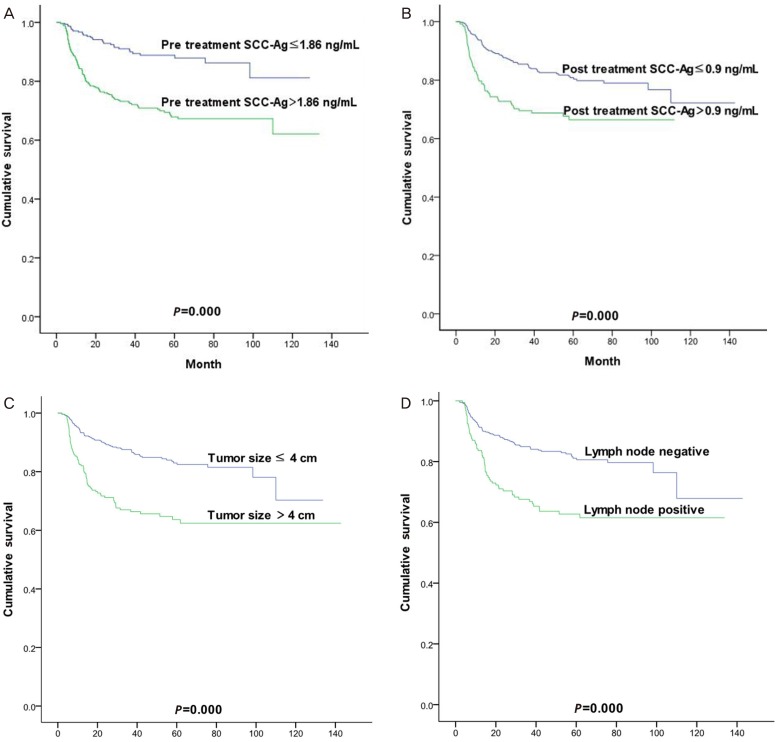
Distant DFS curves according to pretreatment and posttreatment SCC-Ag levels, tumor size, and lymph node involvement are shown in Fig. 2. Women with pretreatment SCC-Ag >1.86 ng/mL (P=0.000), posttreatment SCC-Ag >0.9 ng/mL (P=0.000), tumor size >4 cm in diameter (P=0.000), and positive lymph node involvement (P=0.000) had a significantly poor DFS (Fig. 2).
Fig. 2. Disease free survival depending on the pretreatment (A) and posttreatment (B) squamous cell carcinoma antigen (SCC-Ag) level, tumor size (C), lymph node involvement (D).
Discussion
The risk factors for recurrent disease in early stage cervical cancer include large tumor size, positive lymph node, parametrial involvement, and lymph-vascular space invasion [22]. Our finding that tumor size, lymph node involvement, and FIGO stage are associated with tumor recurrence in the multivariate analysis is in concurrence with this fact.
SCC-Ag is one of the major tumor markers, which is currently widely employed as a tumor marker in squamous cell carcinoma of the uterine cervix. Previous literature reported that the pretreatment level of SCC-Ag is associated with FIGO stage, tumor size, and parametrial involvement [4,5,6,7,8,9,10], and that continued or increasing levels of SCC-Ag reflect persistent or recurrent disease [23,24]. However, the clinical relevance of pretreatment SCC-Ag level is still debated [16]. In the study by Gaarenstroom et al. [10], SCC-Ag was significantly related to progression free survival and overall survival in the univariate analysis, but not in the multivariate analysis. Similarly, Yuan et al. [6] reported that elevated preoperative serum SCC-Ag level was a poor prognostic factor for survival in the univariate analysis but not in the multivariate analysis. In studies by Hong et al. [19] and Duk et al. [5], elevated pretreatment serum SCC-Ag level was an independent prognostic variable for survival. Elevated serum SCC-Ag level at the time of diagnosis was associated with a three times higher risk of recurrence [25]. Similarly, Strauss et al. [7] found that elevated pre-operative serum SCC-Ag level above 3 ng/mL was an independent poor prognostic factor for recurrence free survival and overall survival.
Our findings support the prognostic value of pretreatment SCC-Ag level in predicting recurrence. Pretreatment SCC-Ag >1.86 ng/mL was an independent risk factor of cancer recurrence in the multivariate analysis and disease progression in the survival analysis. However, the cut off values of elevated SCC-Ag level vary from study to study. Strauss et al. [7] reported a SCC-Ag cut off level of 3 ng/mL in patients with stages IA2 to IIB squamous cell carcinoma of the cervix who underwent radical hysterectomy. In another study of early stage squamous cell carcinoma of the cervix, a cut off value of 1.9 ng/mL was used to predict postoperative radiotherapy [9]. Davelaar et al. [26] reported that a cut off level of 1.1 ng/mL was associated with poor prognosis in early stage squamous cell carcinoma of the cervix. Gadducci et al. [27] reported that pretreatment serum SCC-Ag <7 ng/mL was associated with longer progression free survival and overall survival in the univariate analysis in patients with stage IB to IIIB disease who underwent neo-adjuvant chemotherapy followed by radical surgery. The differences in cut off values of pretreatment SCC-Ag may be contributable to differences in the cancer stages of patients included in each study. Since an increased pretreatment SCC-Ag level is known to correlate with advanced FIGO stage, the median level of pretreatment SCC-Ag in early stage of the disease would be lower than the median SCC-Ag level in advanced stage. Our study included patients with all stages of the disease, but the proportion of patients with stage III to IV disease was relatively low compared with that of patients with early stage of disease (5.6% vs. 94.4%). The relatively low cut-off value of 1.86 ng/mL in this study compared with 7 ng/mL in the study by Gadducci et al. [27] may be due to this reason.
There have been several studies about posttreatment SCC-Ag monitoring associated with treatment response or follow up of tumor recurrence [11,12,13,19,25]. However, these studies did not consider posttreatment SCC-Ag level as an independent risk factor for disease progression. In our study, posttreatment SCC-Ag >0.9 ng/mL was also associated with higher risk of recurrence in the multivariate analysis. This data from the current study suggest that serum SCC-Ag level not only before the primary treatment but also at the end of primary treatment can be used as a prognostic factor for disease progression.
Hong et al. [19] noted that persistently elevated serum SCC-Ag level after radiotherapy is a strong predictor for treatment failure. In this study, biochemical response was a poor prognostic factor for recurrence in the univariate analysis but not in the multivariate analysis. Since our study included only patients who had achieved complete remission after primary treatment and excluded the other patients with treatment failure, majority of the biochemical failure or negative patients would have been excluded, and the prognostic value of biochemical response would be limited.
There are several potential limitations of this study. First, the patient group included in our study was relatively heterogeneous compared with that in other studies. Our study included all FIGO stages and all types of treatment modalities. Among the 783 patients, 36 (4.6%) patients underwent radiotherapy alone instead of CCRT due to old age, underlying disease, or poor performance status. One hundred and sixty-five (21.1%) patients underwent adjuvant therapy due to one or more risk factors after surgery. Difference in treatment modalities might have influenced the response to treatment and consequently, the recurrence rate. Further studies involving a patient group with subdivided treatment modality and FIGO stage may be necessary to confirm the findings of this study.
Second, tumor size or lymph node involvement was determined by imaging studies in the patients who did not undergo surgery. Staging accuracy of MRI and CT imaging have been reported to be approximately 79% (range, 47% to 90%) and 62% (range, 32% to 80%), respectively [28]. Also, the accuracy of detecting lymph node involvement by CT or MRI varies from 75% to 86% and from 75% to 100%, respectively [28]. In our study, 55% of the subjects did not undergo surgery, and CT or MRI imaging was performed, hence the discrepancy in accuracy.
Lastly, an important risk factor such as human papillomavirus (HPV) genotyping was not incorporated in our study. HPV is a well established cause of cervical cancer [29,30], and its genotyping has been used for prognosis prediction in cervical cancer [31,32,33]. The effect of HPV genotype on disease progression was not assessed in our study.
In conclusion, elevated pretreatment and posttreatment SCC-Ag levels are associated with higher risk of tumor recucrence and poor disease free survival. Patients with pretreatment SCC-Ag >1.86 ng/mL or posttreatment SCC-Ag >0.9 ng/mL should be considered at high risk for cancer recurrence after complete remission have been achieved, and therefore, closer surveillance is needed.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.American Cancer Society. Global cancer facts & figures 3rd edition [Internet] Atlanta (GA): American Cancer Society; c2015. [cited 2015 Feb 20]. Available from: http://www.cancer.org/research/cancerfactsstatistics. [Google Scholar]
- 2.Bonfrer JM, Gaarenstroom KN, Korse CM, Van Bunningen BN, Kenemans P. Cyfra 21-1 in monitoring cervical cancer: a comparison with tissue polypeptide antigen and squamous cell carcinoma antigen. Anticancer Res. 1997;17:2329–2334. [PubMed] [Google Scholar]
- 3.Esajas MD, Duk JM, de Bruijn HW, Aalders JG, Willemse PH, Sluiter W, et al. Clinical value of routine serum squamous cell carcinoma antigen in follow-up of patients with early-stage cervical cancer. J Clin Oncol. 2001;19:3960–3966. doi: 10.1200/JCO.2001.19.19.3960. [DOI] [PubMed] [Google Scholar]
- 4.Avall-Lundqvist EH, Sjovall K, Nilsson BR, Eneroth PH. Prognostic significance of pretreatment serum levels of squamous cell carcinoma antigen and CA 125 in cervical carcinoma. Eur J Cancer. 1992;28A:1695–1702. doi: 10.1016/0959-8049(92)90071-9. [DOI] [PubMed] [Google Scholar]
- 5.Duk JM, Groenier KH, de Bruijn HW, Hollema H, ten Hoor KA, van der Zee AG, et al. Pretreatment serum squamous cell carcinoma antigen: a newly identified prognostic factor in early-stage cervical carcinoma. J Clin Oncol. 1996;14:111–118. doi: 10.1200/JCO.1996.14.1.111. [DOI] [PubMed] [Google Scholar]
- 6.Yuan CC, Wang PH, Ng HT, Tsai LC, Juang CM, Chiu LM. Both TPA and SCC-Ag levels are prognostic even in highrisk stage Ib-IIa cervical carcinoma as determined by a stratification analysis. Eur J Gynaecol Oncol. 2002;23:17–20. [PubMed] [Google Scholar]
- 7.Strauss HG, Laban C, Lautenschlager C, Buchmann J, Schneider I, Koelbl H. SCC antigen in the serum as an independent prognostic factor in operable squamous cell carcinoma of the cervix. Eur J Cancer. 2002;38:1987–1991. doi: 10.1016/s0959-8049(02)00159-4. [DOI] [PubMed] [Google Scholar]
- 8.Molina R, Filella X, Lejarcegui JA, Pahisa J, Torne A, Rovirosa A, et al. Prospective evaluation of squamous cell carcinoma and carcinoembryonic antigen as prognostic factors in patients with cervical cancer. Tumour Biol. 2003;24:156–164. doi: 10.1159/000073846. [DOI] [PubMed] [Google Scholar]
- 9.Reesink-Peters N, van der Velden J, Ten Hoor KA, Boezen HM, de Vries EG, Schilthuis MS, et al. Preoperative serum squamous cell carcinoma antigen levels in clinical decision making for patients with early-stage cervical cancer. J Clin Oncol. 2005;23:1455–1462. doi: 10.1200/JCO.2005.02.123. [DOI] [PubMed] [Google Scholar]
- 10.Gaarenstroom KN, Kenter GG, Bonfrer JM, Korse CM, Van de Vijver MJ, Fleuren GJ, et al. Can initial serum cyfra 21-1, SCC antigen, and TPA levels in squamous cell cervical cancer predict lymph node metastases or prognosis. Gynecol Oncol. 2000;77:164–170. doi: 10.1006/gyno.2000.5732. [DOI] [PubMed] [Google Scholar]
- 11.Scambia G, Panici PB, Baiocchi G, Amoroso M, Foti E, Greggi S, et al. The value of squamous cell carcinoma antigen in patients with locally advanced cervical cancer undergoing neoadjuvant chemotherapy. Am J Obstet Gynecol. 1991;164:631–636. doi: 10.1016/s0002-9378(11)80037-2. [DOI] [PubMed] [Google Scholar]
- 12.Micke O, Prott FJ, Schafer U, Tangerding S, Potter R, Willich N. The impact of squamous cell carcinoma (SCC) antigen in the follow-up after radiotherapy in patients with cervical cancer. Anticancer Res. 2000;20:5113–5115. [PubMed] [Google Scholar]
- 13.Ohara K, Tanaka Y, Tsunoda H, Nishida M, Sugahara S, Itai Y. Assessment of cervical cancer radioresponse by serum squamous cell carcinoma antigen and magnetic resonance imaging. Obstet Gynecol. 2002;100:781–787. doi: 10.1016/s0029-7844(02)02204-4. [DOI] [PubMed] [Google Scholar]
- 14.Maiman M. The clinical application of serum squamous cell carcinoma antigen level monitoring in invasive cervical carcinoma. Gynecol Oncol. 2002;84:4–6. doi: 10.1006/gyno.2001.6532. [DOI] [PubMed] [Google Scholar]
- 15.Gadducci A, Tana R, Fanucchi A, Genazzani AR. Biochemical prognostic factors and risk of relapses in patients with cervical cancer. Gynecol Oncol. 2007;107(1 Suppl 1):S23–S26. doi: 10.1016/j.ygyno.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 16.Gadducci A, Tana R, Cosio S, Genazzani AR. The serum assay of tumour markers in the prognostic evaluation, treatment monitoring and follow-up of patients with cervical cancer: a review of the literature. Crit Rev Oncol Hematol. 2008;66:10–20. doi: 10.1016/j.critrevonc.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 17.Abe A, Nakano T, Morita S, Oka K. Clinical evaluation of serum and immunohistochemical expression of SCC and CA19-9 in radiation therapy for cervical cancer. Anticancer Res. 1999;19:829–836. [PubMed] [Google Scholar]
- 18.Bolger BS, Dabbas M, Lopes A, Monaghan JM. Prognostic value of preoperative squamous cell carcinoma antigen level in patients surgically treated for cervical carcinoma. Gynecol Oncol. 1997;65:309–313. doi: 10.1006/gyno.1997.4619. [DOI] [PubMed] [Google Scholar]
- 19.Hong JH, Tsai CS, Chang JT, Wang CC, Lai CH, Lee SP, et al. The prognostic significance of pre- and posttreatment SCC levels in patients with squamous cell carcinoma of the cervix treated by radiotherapy. Int J Radiat Oncol Biol Phys. 19981;41:823–830. doi: 10.1016/s0360-3016(98)00147-3. [DOI] [PubMed] [Google Scholar]
- 20.Dorfman RE, Alpern MB, Gross BH, Sandler MA. Upper abdominal lymph nodes: criteria for normal size determined with CT. Radiology. 1991;180:319–322. doi: 10.1148/radiology.180.2.2068292. [DOI] [PubMed] [Google Scholar]
- 21.Nicolet V, Carignan L, Bourdon F, Prosmanne O. MR imaging of cervical carcinoma: a practical staging approach. Radiographics. 2000;20:1539–1549. doi: 10.1148/radiographics.20.6.g00nv111539. [DOI] [PubMed] [Google Scholar]
- 22.Miller C, Elkas JC. Cervical and vaginal cancer. In: Berek JS, editor. Berek & Novak's gynecology. 15th ed. Philadelphia (PA): Lippincott Williams & Wilkins; 2012. pp. 1304–1349. [Google Scholar]
- 23.Montag TW. Tumor markers in gynecologic oncology. Obstet Gynecol Surv. 1990;45:94–105. doi: 10.1097/00006254-199002000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Duk JM, de Bruijn HW, Groenier KH, Hollema H, ten Hoor KA, Krans M, et al. Cancer of the uterine cervix: sensitivity and specificity of serum squamous cell carcinoma antigen determinations. Gynecol Oncol. 1990;39:186–194. doi: 10.1016/0090-8258(90)90430-s. [DOI] [PubMed] [Google Scholar]
- 25.de Bruijn HW, Duk JM, van der Zee AG, Pras E, Willemse PH, Boonstra H, et al. The clinical value of squamous cell carcinoma antigen in cancer of the uterine cervix. Tumour Biol. 1998;19:505–516. doi: 10.1159/000030044. [DOI] [PubMed] [Google Scholar]
- 26.Davelaar EM, van de Lande J, von Mensdorff-Pouilly S, Blankenstein MA, Verheijen RH, Kenemans P. A combination of serum tumor markers identifies high-risk patients with early-stage squamous cervical cancer. Tumour Biol. 2008;29:9–17. doi: 10.1159/000132566. [DOI] [PubMed] [Google Scholar]
- 27.Gadducci A, Scambia G, Panici PB, Ferdeghini M, Battaglia F, Caenaro G, et al. The prognostic relevance of pretreatment serum immunosuppressive acidic protein (IAP) in patients with squamous cell carcinoma of the uterine cervix: a comparison with squamous cell carcinoma antigen (SCC) Cancer J. 1994;7:241–247. [Google Scholar]
- 28.Boss EA, Barentsz JO, Massuger LF, Boonstra H. The role of MR imaging in invasive cervical carcinoma. Eur Radiol. 2000;10:256–270. doi: 10.1007/s003300050042. [DOI] [PubMed] [Google Scholar]
- 29.Munoz N, Bosch FX, de Sanjose S, Herrero R, Castellsague X, Shah KV, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348:518–527. doi: 10.1056/NEJMoa021641. [DOI] [PubMed] [Google Scholar]
- 30.Snijders PJ, Steenbergen RD, Heideman DA, Meijer CJ. HPV-mediated cervical carcinogenesis: concepts and clinical implications. J Pathol. 2006;208:152–164. doi: 10.1002/path.1866. [DOI] [PubMed] [Google Scholar]
- 31.de Cremoux P, de la Rochefordiere A, Savignoni A, Kirova Y, Alran S, Fourchotte V, et al. Different outcome of invasive cervical cancer associated with high-risk versus intermediate-risk HPV genotype. Int J Cancer. 2009;124:778–782. doi: 10.1002/ijc.24075. [DOI] [PubMed] [Google Scholar]
- 32.Lai CH, Chang CJ, Huang HJ, Hsueh S, Chao A, Yang JE, et al. Role of human papillomavirus genotype in prognosis of early-stage cervical cancer undergoing primary surgery. J Clin Oncol. 2007;25:3628–3634. doi: 10.1200/JCO.2007.11.2995. [DOI] [PubMed] [Google Scholar]
- 33.Schwartz SM, Daling JR, Shera KA, Madeleine MM, McKnight B, Galloway DA, et al. Human papillomavirus and prognosis of invasive cervical cancer: a population-based study. J Clin Oncol. 2001;19:1906–1915. doi: 10.1200/JCO.2001.19.7.1906. [DOI] [PubMed] [Google Scholar]