Abstract
Respiratory protection provided by a particulate respirator is a function of particle penetration through filter media and through faceseal leakage. Faceseal leakage largely contributes to the penetration of particles through a respirator and compromises protection. When faceseal leaks arise, filter penetration is assumed to be negligible. The contribution of filter penetration and faceseal leakage to total inward leakage (TIL) of submicron-size bioaerosols is not well studied. To address this issue, TIL values for two N95 filtering facepiece respirator (FFR) models and two surgical mask (SM) models sealed to a manikin were measured at 8 L and 40 L breathing minute volumes with different artificial leak sizes. TIL values for different size (20–800 nm, electrical mobility diameter) NaCl particles representing submicron-size bioaerosols were measured using a scanning mobility particle sizer. Efficiency of filtering devices was assessed by measuring the penetration against NaCl aerosol similar to the method used for NIOSH particulate filter certification. Results showed that the most penetrating particle size (MPPS) was ∼45 nm for both N95 FFR models and one of the two SM models, and ∼350 nm for the other SM model at sealed condition with no leaks as well as with different leak sizes. TIL values increased with increasing leak sizes and breathing minute volumes. Relatively, higher efficiency N95 and SM models showed lower TIL values. Filter efficiency of FFRs and SMs influenced the TIL at different flow rates and leak sizes. Overall, the data indicate that good fitting higher-efficiency FFRs may offer higher protection against submicron-size bioaerosols.
Keywords: faceseal leakage, filter penetration, N95 filtering facepiece respirator, NaCl aerosol, surgical mask, total inward leakage
INTRODUCTION
Influenza and other pandemic infectious diseases cause illness and death worldwide. The mode of transmission of infection appears to be through large droplets, aerosols, fomites, or person-to-person contact.() Infected subjects are known to release a wide size range of particles during breathing, coughing, sneezing, and talking. The droplets travel some distance and evaporate to form smaller-size particles. Normal human subjects and infected individuals release considerable numbers of submicron diameter particles in the exhaled breath.(–) In one study, exhaled breath of seven subjects infected with influenza was collected on Teflon filters and exhaled particle concentrations measured using an optical particle counter.() Filters were tested for influenza virus by quantitative polymerase chain reaction (qPCR). Results for four subjects showed influenza virus particles in exhaled breath and over 87% of particles were under 1 μm in diameter. Recently, appreciable numbers of influenza particles were found in the ambient air in different locations.() Submicron aerosols can remain airborne for prolonged periods because of their low settling velocity. Infectious aerosol, when inhaled by susceptible persons, is likely to cause disease.
Respiratory protection is known to reduce the inhalation of infectious aerosols. The Centers for Disease Control and Prevention (CDC) has developed recommendations on the use of the National Institute for Occupational Safety and Health (NIOSH)-approved N95 filtering facepiece respirators (FFRs) and facemasks for protection against pandemic influenza virus transmission for home, community, and occupational settings.() SMs are used as barriers to limit the dissemination of secretions or large droplets from patient to others. The Food and Drug Administration (FDA) clears the SMs for sale, based on the test report provided by the manufacturers. SMs are confused with respirators because both look similar and are worn on the face. In general, the filter efficiency of N95 FFRs is superior to SMs.(,) Filter efficiency is enhanced by electrostatic charge on filter media of N95 FFRs. The most penetrating particle size (MPPS) for N95 FFRs is ∼50 nm (electrical mobility diameter).() In the case of SMs, both electrostatic as well as mechanical (MPPS >100 nm) types are available.() FFRs are fit-tested before use in workplaces whereas SMs are not. SMs were used for respiratory protection in health care facilities when there was a shortage of respirators during pandemic seasons.() Therefore, knowing the effectiveness of SMs against infectious bioaerosols is of public health importance.
The effectiveness of N95 FFRs and SMs in health care settings has been reviewed.(,) One study evaluated the health risk of nurses using respiratory protection during the severe acute respiratory syndrome (SARS) epidemic in Canada() and showed that N95 respirators were more protective than the SMs. Similarly, N95 respirators and hand washing were found to be effective in protecting health care workers against SARS transmission.() Another study reported a dramatic decrease of SARS infection from 52 to 8 among health care staff after implementation of the use of N95 masks, gloves, and gowns.()
Recently, the efficacy of N95 FFRs or SMs against influenza transmission was evaluated with human subjects exposed to live attenuated influenza vaccine particles.() Analysis for influenza virus in the nasal washes of test subjects by reverse transcription-polymerase chain reaction technique showed that wearing N95 respirators offered a higher level of protection than SMs. Another study measured the protection factor for SMs and FFRs on test subjects in a controlled environmental test chamber and showed that SMs may not be as protective as FFRs.()
Some studies have reported that SMs are as effective as N95 FFRs for respiratory protection from viral respiratory pathogens.(–) Protection performance was tested using a fluorescein-KCl aerosol spray onto the faces of subjects wearing N95 FFRs or SMs and performing intermittent exercises on a treadmill in a chamber.() Test aerosol size was assumed to be about 0.1–0.3 μm based on the comparison of the filtration efficiency obtained for N95 FFRs in their study with the efficiency reported by a different group.() After the experiment, fluorescent stain on the faces and KCl concentrations in different layers of FFRs and SMs were analyzed to calculate the filter efficiency. Results showed that both N95 FFRs and SMs gave 95% or greater filtration efficiency, and N95 FFRs had about 2% filtration efficiency higher than the SMs indicating that SMs and N95 FFRs can provide protection in a relatively low viral aerosol loading environment. A case-control study in Hong Kong hospitals showed that both SMs and N95 FFRs were significantly effective in reducing the risk of SARS infection among staff.() In another study, influenza virus collected during coughing of patients wearing N95 FFRs or SMs was analyzed by quantitative real time RT-PCR.() The efficacy of SMs and N95 FFRs was found to be similar in preventing the spread of influenza virus from patients. Similarly, the use of SMs compared with N95 FFRs showed a non-inferior rate of laboratory-confirmed influenza.()
Comprehensive information on the relative efficacy of FFRs and SMs for submicron-size bioaerosols is lacking. To address this issue, the Institute of Medicine (IOM) recommended further research in key areas including the effectiveness of facemasks and respirators against infectious particles and faceseal leakage contributing to the overall total inward leakage (TIL).() TIL is defined as an inverse function of a protection level offered by a respirator when the contributions of aerosol penetration through filter media, faceseal leakage, and leakage through other components are considered. It is known that FFRs are designed to provide good fitting on the human face unlike the SMs. Because of the difference in face-fitting characteristics, SMs will have a larger faceseal leakage than FFRs when used by workers. One way to compare the performance of FFRs with SMs is to measure the TIL under controlled leak sizes.
In this study, TIL for two N95 FFR models and two SM models sealed to a manikin was measured as a ratio of particle concentration inside the breathing zone (space covered around the face by the filtering device) (Cin) to outside (ambient) concentration (Cout) at different size artificial leak holes introduced on the filtering devices at two different breathing flow rates. Submicron diameter size NaCl aerosol was used to measure the TIL. This size range of particles is similar to the size of bioaerosols released by subjects under breathing conditions as reported previously.(–) Moreover, TIL, a measure of filter penetration and faceseal leakage for submicron-size particles would also be applicable to larger-size bioaerosols. TIL values for the two N95 FFR models and the two SM models were compared. The significance of filter penetration and faceseal leakage contributing to the TIL, and the efficacy of N95 FFRs and SMs against submicron-size bioaerosols are discussed.
MATERIALS AND METHODS
Filtering Facepiece Respirators (FFRs) and Surgical Masks (SMs)
Two NIOSH-approved N95 FFR models and two FDA-cleared SM models were tested in the study. These models were selected based on their performance in previous studies in our laboratory.(,) The manufacturers and models (in parentheses) of the N95 FFRs were: Willson (model 1105N,) and San Huei United Company (model 1895N,) labeled as N1 and N2, respectively, and the SM models were: Primed (model PG4-1073,) and 3M (model 1800) labeled as SM1 and SM2, respectively. None of the N95 models tested in the study had exhalation valves.
Filter Efficiency Test
Instantaneous filter penetration of FFRs and SMs was measured to assess their filter efficiency. Penetration of FFRs and SMs was measured using NaCl aerosol (count median diameter (CMD) 75±20 nm) generated by an Automated Filter Tester (AFT) TSI 8130 (TSI Inc., Shorewood, Minn.).() The AFT measures penetration based on the light scattering of particles that pass through the filter. A Plexiglas test box (L 20 cm × W 20 cm × H 10 cm) with a top and bottom plate containing a hole (2.5 cm diameter) in the center was used for measuring aerosol penetration.() A FFR or SM with its concave side facing down was sealed to a Plexiglas plate (L 20 cm × W 20 cm × H 0.5 cm) using melted wax. A silicone sealant was used to seal the top and bottom plates to make the Plexiglas box airtight. The Plexiglas box containing the FFR or SM was placed between the two filter chucks of the AFT and aligned to keep the top and bottom plate holes facing the upstream and downstream filter chucks, respectively. Penetration was measured for 1 min at 85 L/min constant flow under airtight conditions by closing the filter chucks.
Total Inward Leakage Measurements Using a Manikin Setup
Figure 1 shows a manikin setup employed to evaluate the effect of faceseal leakage on TIL as described previously.() TIL was measured in two general configurations: (1) sealed to the manikin face with no artificial leaks induced through needles; and (2) sealed to the manikin face with artificial leaks induced through needles. A FFR or SM was sealed to a manikin head form using a silicone sealant and placed inside a test chamber (48 × 48 × 48 cm3). The head form was connected to a breathing simulator (Breathing Simulator Series 1101, Hans Rudolph, Inc., Shawnee, Kans.) through an isolation chamber consisting of a rubber bladder inside an airtight glass container. A metal tube (2.5 cm diameter) from the back of the mouth was connected to an inflatable rubber bladder, which mimics a human lung, inside the glass container connected to a breathing simulator. The breathing simulator allows air to go back and forth into the glass container. In response, ambient air enters the bladder through the FFR sealed to the manikin head form during inhalation and exits during exhalation. Thus, the isolation chamber prevented particles created by the breathing simulator pump from getting inside the breathing zone of the respirator. The breathing simulator allowed for several parameters to be varied including tidal volume and breathing rate, which provided simulation of more realistic breathing conditions.
Figure 1. Flow diagram of the manikin experimental setup used for submicron-size particle leakage under simulated breathing conditions (The rubber bladder mimics a human lung and allows breathing air to enter and exit through the mouth. A typical FFR with a sample probe and one leak probe is shown in the inset. The differential mobility analyzer (DMA) of the SMPS separates particles based on their electrical mobility.) (color figure available online).
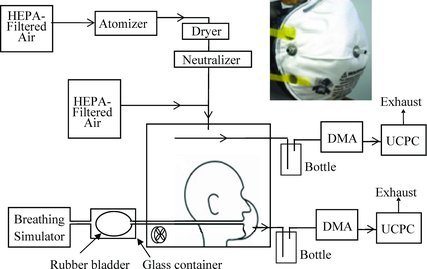
NaCl aerosol used for TIL measurement was different from the aerosol used for testing filter penetration. Size distribution of NaCl aerosol was obtained in a manner similar to that described previously.() Briefly, polydisperse NaCl aerosol was generated using a 1.5% NaCl solution with a constant output atomizer (TSI 3076) and passed through a dryer, a 85Kr charge neutralizer (TSI model 3077A), diluted with 50 L/min of dry air passed through a high efficiency particulate air filter (HEPA) and then into the test chamber (48 × 48 × 48 cm3; Figure 1). Excess aerosol exited through a hole (1.3 cm diameter) in the back of the test chamber. A small fan was installed at the bottom of the chamber to ensure an even distribution of particles throughout. Aerosol samples from the test chamber were analyzed for number concentration for different size monodisperse particles (20–800 nm, electrical mobility diameter) over 240 sec and repeated after a 30 sec interval, using a scanning mobility particle sizer (SMPS) (TSI model 3080) with a long differential mobility analyzer (DMA), and an ultra-fine condensation particle counter (UCPC, TSI 3776). The DMA separates particles based on their electrical mobility. The count median diameter (CMD) and mode size (peak size) of the test aerosols were obtained from the SMPS scans.
The test FFR was equipped with a sample probe to measure aerosol concentration inside the FFR and two leak probes to introduce artificial leakage (Figure 1, Inset).() The leak probes (∼3 mm diameter and ∼1 cm long) were filled with non-hardening putty and increasing leak sizes were obtained by carefully inserting hypodermic needles (16 and 13 gauge sizes with inner diameters of 1.18 and 1.80 mm, respectively) through the putty to provide consistent leak channels through the needles (∼2.56 cm long). Care was taken to ensure the needle was kept open after inserting it into the putty. The tip of the needle was positioned proximately close to the inner surface of the respirator. Because the above leak sizes did not produce a significant difference in the TIL for SMs, larger leak sizes were used.
For comparison, SMs as well as FFRs were fixed with larger leak probes (∼3 mm diameter and ∼1 cm long). Each leak size was created using two leak probes, one on each side. TIL was measured with three different leak sizes (two 3 mm, four 3 mm or six 3 mm). Samples from inside and outside the FFRs and SMs were withdrawn and analyzed by two SMPS systems simultaneously.() The two SMPS systems scanned the particles in the 20–800 nm size range three times each three min. Samples were withdrawn simultaneously during manikin breathing at 8 and 40 L minute volumes with tidal volumes of 0.5 and 1.5 L, respectively. These tidal volumes corresponded to 16 and 26.7 breaths per minute, respectively. TIL was calculated as the ratio of particle concentration inside (Cin) of the FFR or SM to the outside concentration (Cout) and multiplied by 100%.
RESULTS
Filter Efficiency
NaCl aerosol penetrations for N95 FFR models were lower than the penetrations for the SM models at 85 L/min flow rate (Table I). In addition, penetrations for N1 and SM1 were relatively lower than the values obtained for N2 and SM2, respectively. Based on the penetration values, N1 and SM1 are described as higher-efficiency FFR and SM models, respectively, throughout the article.Table 2
Table 1. Filter Penetration for the N95 FFR Models and SM Models at 85 L/min Constant Flow (Average of three samples (n = 3), error represents one standard deviation.).
| Filter Penetration (%) |
||||
|---|---|---|---|---|
| Penetration Method | N1 | N2 | SM1 | SM2 |
| NaCl aerosol (CMD 75 ± 20 nm) (TSI 8130 – photometric, Constant flow - 85 L/min) | 0.17 ± 0.06 | 0.86 ± 0.22 | 1.58 ± 0.25 | 88.1 ± 0.81 |
Table 2. Comparison of Total Inward Leakage (TIL) at Two Different Breathing Minute Volumes and Three Leak Sizes (Average of 4 samples (n = 4), error represents one standard deviation.).
| TIL (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Particle Size (nm) |
|||||||||
| N1 | N2 | SM1 | SM2 | ||||||
| Leak Size | Breathing Minute | ______________________ | ______________________ | ______________________ | _____________________ | ||||
| (mm) | Volume (L/min) | 45 | 300 | 45 | 300 | 45 | 300 | 45 | 300 |
| No Leaks | 8 | 0.31±0.4 | 0.12±0.1 | 1.48±2.1 | 1.01±0.3 | 3.58±1.5 | 2.91±1.5 | 45.08±20 | 87.55±28 |
| 40 | 1.56±0.9 | 0.31±0.2 | 4.96±2.9 | 2.55±1.9 | 9.33±2.4 | 2.27±2.1 | 68.44±14 | 96.59±10 | |
| Two 3 mm | 8 | 10.67±4.6 | 9.94±3.1 | 11.52±7.7 | 10.14±1.6 | 14.76±5.1 | 9.70±10.3 | 67.01±7.0 | 100.03±95 |
| 40 | 8.56±3.1 | 8.45±2.4 | 11.75±4.6 | 9.14±1.6 | 14.02±3.8 | 9.25±3.95 | 71.57±6.1 | 99.78±5.2 | |
| Four 3 mm | 8 | 30.54±4.2 | 28.48±2.5 | 30.66±6.3 | 29.26±3.9 | 28.15±3.8 | 27.56±5.3 | 66.65±7.5 | 99.21±11 |
| 40 | 29.5±3.6 | 27.53±2.6 | 27.86±3.2 | 24.42±3.5 | 25.62±6.4 | 25.06±4.7 | 70.54±10 | 104.38±12 | |
| Six 3 mm | 8 | 38.72±5.7 | 39.87±4.8 | 36.22±7.3 | 37.18±3.7 | 35.67±6.3 | 33.53±7.2 | 52.92±16 | 95.52±16 |
| 40 | 31.45±3.4 | 32.58±4.9 | 36.96±4.0 | 35.83±3.4 | 37.37±4.6 | 36.40±3.6 | 72.12±9.5 | 93.47±7.5 | |
TIL Measurement Under Breathing Conditions
The size distribution of NaCl aerosol used for TIL measurement showed a CMD of ∼82 nm and a mode size (peak size) of ∼75 nm. Figure 2 shows the TIL measured at no leak condition and with two small leak sizes at 8 L (left panels) and at 40 L (right panels) breathing minute volumes for the two N95 models. TIL for different size particles increased with increasing breathing minute volumes from 8 to 40 L with no leaks. The most penetrating particle size (MPPS) was ∼45 nm for both FFR models which can be easily seen at 40 L breathing minute volume. With increasing leak sizes (2×1.18 mm and 2×1.80 mm), the TIL for different size particles increased for the two FFR models at both breathing rates. The MPPS remained at ∼45 nm with different leak sizes. The TIL for the MPPS was higher than the values for the other size particles. Among the two N95 models, N1 showed lower TIL values for different size particles than N2 at both breathing rates.
Figure 2. Typical TIL values for the two N95 FFR models N1 and N2 at 8 L/min (left column) and 40 L/min (right column) breathing minute volumes (The symbols indicate sealed with no leaks (•), two 1.18 mm leaks (○), and two 1.80 mm leaks (▾). The solid vertical line corresponds to the approximate MPPS (45 nm) of the two N95 FFR models. The dashed vertical line corresponds to the mode of the challenge aerosol (75 nm).).
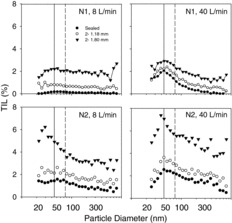
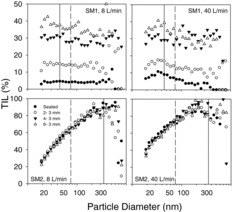
Figure 3 shows an increase in the TIL for different size particles with increasing leak sizes from 3 to 5 (2×3 mm, 4×3 mm, and 6×3 mm, respectively) for both FFR models, at 8 and 40 L/min. Larger leak holes (4×3 mm and 6×3 mm) tend to produce similar TIL values for different size particles. Similar trends in TIL results were obtained for SM1 at different leak sizes and flow rates (Figure 4, top panels). The MPPS was ∼45 nm with no leaks and with a smaller leak size (2×3 mm), which can be seen at 40 L/min. For SM2, however, TIL values for the various size particles at no leak condition and with different induced leak sizes showed very little change at both breathing flow rates (Figure 4, bottom panels). The MPPS for SM2 was ∼350 nm at all test conditions. Table II shows the TIL for the two FFR models and the two SM models at different leak sizes and flow rates. Models N1, N2 and SM1 showed higher TIL values for 45 nm particles than for 300 nm size particles at smaller leak sizes as reported previously.(24) For SM2, however, TIL values were smaller at 45 nm than at 300 nm at all test conditions.
Figure 3. Typical TIL values for the two N95 FFR models N1 and N2 at 8 L/min (left column) and 40 L/min (right column) breathing minute volumes (The symbols indicate: sealed with no leaks (•), two 3 mm leaks (○), four 3 mm leaks (▾), and six 3 mm leaks (Δ). The solid vertical line corresponds to the approximate MPPS (45 nm) of the two N95 FFR models. The dashed vertical line corresponds to the mode of the challenge aerosol [75 nm]).
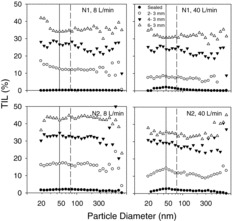
Figure 4. Typical TIL values for the two surgical models SM1 and SM2 at 8 L/min (left column) and 40 L/min (right column) breathing minute volume (The symbols indicate: sealed with no leaks (•), two 3 mm leaks (○), four 3 mm leaks (▾), and six 3 mm leaks (▵). The solid vertical line corresponds to the MPPS of ∼45 nm for SM1 and ∼350 nm for SM2 models. The dashed vertical line corresponds to the mode of the challenge aerosol [75 nm]).
DISCUSSION
TIL measured for 20–800 nm diameter size NaCl aerosols for the two N95 FFR models were lower than the values obtained for the two SM models at the two different breathing flow rates without induced leaks. TIL value without induced leaks represents penetration through filter media and agrees with the trend in penetration measured at NIOSH certification test condition. The inverse relationship between TIL and filter efficiency can also be seen among the FFR models, N1 (higher efficiency) and N2 (lower efficiency) as well as between the SM models, SM1 (higher efficiency) and SM2 (lower efficiency). With increasing leak sizes, TIL for 20–800 nm size particles increased with increasing breathing flow rates for both FFR models as well as for the SM1 model. TIL values for the two FFR models were lower than the values for the SM models at similar flow rates and leak sizes, indicating the influence of filter efficiency. TIL values for the FFR models and SM1 did not vary significantly at larger leak sizes where minimum protection can be expected. However, TIL values between FFRs and SM2 were markedly different. Similar difference in TIL can also be seen between SM1 and SM2. The results can be explained by the large difference in filter efficiency between the filtering devices (FFRs and SM1 vs. SM2), and the inverse relationship between efficiency and TIL.
Results obtained in the present study are consistent with the data for four different N95 FFR models tested previously.() In that study, two relatively higher-efficiency N95 FFR models showed lower TIL values than two lower-efficiency models with different leak sizes and flow rates. The inverse relationship between filter efficiency and TIL provides a better explanation for the higher levels of respiratory protection offered by the N95 FFRs than the SMs reported previously.(,,)
The MPPS was ∼45 nm for N1, N2, and SM1 models, and ∼350 nm for SM2 with no faceseal leakage. Similar results were obtained with smaller leak sizes at different breathing rates. Results from the study indicated that FFRs producing smaller TIL value at the MPPS may provide relatively higher protection against submicron virus aerosols. Among the two SM models tested, SM1 appears to be more effective than SM2 for submicron-size virus aerosols.
The relative impact of filter penetration is believed to be minimal or insignificant once leaks are introduced in the facemask. In this study, artificial leaks introduced in the N95 FFRs and SMs sealed to the manikin allowed the test aerosols (mode size ∼75 nm) to enter and exit the breathing zone (space covered around the face by the filtering device) during breathing flow conditions. Interestingly, the MPPS values for FFR and SM models with induced leak sizes were similar to the MPPS obtained with no leaks. The above phenomenon can be explained by the effect of filter penetration or filter media characteristic regulating the concentration of different size particles inside the FFR or SM sealed to the breathing manikin at different leak sizes. The results are consistent with our previous finding() that faceseal leakage acts as a gatekeeper and indiscriminately allows the test aerosols to flow through the leaks and increases the concentration of all size test aerosol inside the breathing zone, while filter penetration or filter media characteristic assigns the TIL values for different size particles. The results obtained in the study indicate that filter penetration potentially influences the TIL of different size particles. The data provide a better understanding on the contribution of faceseal leakage and filter penetration to the overall TIL.
The contributions of filter penetration and faceseal leakage to the TIL results obtained with the manikin raise the question of how well these processes are represented when a respirator is worn by a human subject. Faceseal leakage is known to be a major pathway that contributes to the TIL of particles.(–) The number of particles penetrating through the faceseal leakage pathway of the respirators and SMs tested on subjects has been shown to far exceed the number of particles passing through the filter medium.() The influence of filter penetration and faceseal leakage on the TIL measured for test subjects has been described.(,) In one study, the overall TIL values for Korean half-masks and three different class (top class, 1st class, and 2nd class) FFR models donned on test subjects were measured.() Among the FFRs, top class FFRs (≥99% efficiency) showed average TIL values of ∼5.0%. However, the TIL values for lower-efficiency FFRs (“1st class”, ≥94% and “2nd class”, ≥80%) were ∼2 times higher than the TIL values obtained for “top class” FFRs. Overall, the results indicated lower TIL values for the higher-efficiency FFRs. This finding is supported by the data obtained in our recent study on the inter-laboratory comparison of TIL measurement.() Five different N95 FFR models with different filter efficiencies were tested on 35 human subjects performing the Occupational Safety and Health Administration (OSHA) fit-testing exercises in two different test laboratories. A PortaCount Pro (TSI, Shorewood, Minn.) measured the Cout /Cin ratio which was then converted to TIL values based on the inverse relationship between the two parameters. Filter efficiency was obtained only for four of the five models. Results showed that the overall TIL values were lower for a relatively higher-efficiency N95 model, and higher for three lower efficiency models in both laboratories. Moreover, a good agreement between the two laboratories on the TIL values measured for different N95 models was obtained, indicating the measurement was reproducible. Filter efficiency dependence of TIL obtained for human subjects in the above studies may explain the higher protection offered by the N95 FFRs compared to the SMS in health care settings.(,,)
Filter efficiency of the N95 FFRs is generally higher than that of SMs because of the difference in the filter media used for construction. The N95 FFRs are developed to meet more challenging test conditions than are the SMs. Filter efficiency for N95 FFRs is >95% when tested using charge neutralized NaCl aerosols with a CMD of 75±20 nm at 85 L/min. The penetration level does not exceed 5%, up to 200 mg aerosol loading. However, the performance among SMs may vary widely because of the far less challenging test methods used for their clearance by the FDA.() Filtration efficiency of high and moderate barrier SMs is >98% and low barrier SMs is >95% based on the penetration measured against non-neutralized Staphylococcus aureus bacteria of 3000±300 nm at 28.3 L/min. Some types of SMs are also tested with 100 nm diameter non-neutralized polystyrene latex spheres (PSL) at 1 to 25 cm/sec face velocity which may produce wide differences in their efficiencies. Non-neutralization of test aerosol may overestimate the filter efficiency and partly contribute to the enormous difference in the filter performance among SMs.(,) TIL is dependent on efficiency of the filter device.(,) Because of the higher filter efficiency, N95 FFRs are expected to show lower TIL values than do SMs as described previously.(,)
Faceseal leakage is a major pathway for aerosol transport inside the filtering device.(,) The SMs are not designed to provide a good fitting on a human face that may allow more aerosol leakage. However, SMs were found to be as effective as N95 FFRs against aerosol particles similar to the size of infectious aerosols.(,,) In one study, the transmission of influenza during routine health care activities by hospital nurses using N95 FFRs and SMs was assessed.() These authors showed that SMs were equally effective in preventing influenza virus transmission among health care workers. A similar conclusion was obtained in other studies.(,) However, the performance of N95 FFRs may be higher where considerable aerosol generation can occur during procedures such as intubation or bronchoscopy.() Other factors, including training and consistency in the use of the device and concentration of aerosol exposure, can also influence the overall effectiveness of protective devices.
A shortage of respiratory protection devices during pandemic diseases is possible. To address the issue, the CDC has stockpiled large numbers of them. Respirators were stockpiled based on several factors, including their approval for use in health care facilities and availability in the market. Results obtained in the present study may be important for this stockpiling. For example, relatively higher efficiency N95 FFRs, as well as SMs, are expected to produce lower TIL values representing higher protection against infectious aerosols. This indicates that filter efficiency of respiratory protection devices should also be considered for stockpiling purposes.
Limitations and Recommendations for Future Studies
The limitations of the current study include the small number of N95 FFR and SM models tested for TIL measurement. Additional models, including those equipped with an exhalation valve, need to be tested to obtain conclusive information on filter efficiency dependence of TIL. Another limitation of the study is the TIL measurement for particles below 800 nm size range. TIL study for a wide size range of airborne particles using additional equipment may provide more realistic information. Nevertheless, the measurement for 20–800 nm size range provides the underlying mechanism of regulation of TIL by filter penetration and faceseal leakage processes. Further studies on TIL, using test subjects, are important to evaluate the performance of N95 FFRs against submicron-size bioaerosols.
CONCLUSION
Filtration efficiencies of the two N95 FFRs were higher than those of the two SMs tested in the study against NaCl aerosol. Efficiencies of N1and SM1 were relatively higher than those of N2 and SM2, respectively. TIL for NaCl aerosol (CMD ∼82 nm) using a manikin setup showed a MPPS of ∼45 nm for N95 FFR models N1 and N2 and SM1 models, and ∼350 nm for the SM2 model at different flow rates and leak sizes. Leakage of test aerosols through artificial holes increased the TIL for different size particles while the MPPS remained at the same sizes obtained at sealed condition with no artificial leaks, showing that filter penetration regulates TIL. In general, higher-efficiency N95 and SM models showed lower TIL values than the lower-efficiency models, indicating the potential influence of filter efficiency. TIL results obtained in the study indicate that faceseal leakage allows all the different diameter size test aerosols to enter and exit the filtering device while filter penetration assigns the TIL for different size particles. Overall, the data suggest that higher-efficiency N95 FFRs with good fitting characteristics would provide higher protection against submicron-size bioaerosols.
ACKNOWLEDGMENTS
The authors acknowledge NIOSH colleagues including Christopher Coffey, Ray Roberge, and Jay Parker for their useful suggestions and critical review of the manuscript. This research work was supported by NIOSH funding.
DISCLAIMER
Mention of a commercial product or trade name does not constitute endorsement by the National Institute for Occupational Safety and Health. The findings and conclusions of this report are those of the authors and do not necessarily represent the views of NIOSH. This article not subject to US copyright law.
REFERENCES
- Siegel J.D., Rhinehart E., Jackson M., and Chiarello L.: Healthcare Infection Control Practices Advisory Committee. “2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings.” Available at http://www.cdc.gov/ncidod/dhqp/pdf/isolation2007.pdf (accessed March 12, 2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabian P., McDevitt J.J., DeHaan W.H., et al. : Influenza virus in human exhaled breath: An observational study. PloS ONE:1–6 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsley W.G., Pearce T.A., Hudnall J.B., et al. : Quantity and size distribution of cough-generated aerosol particles produced by influenza patients during and after illness. J. Occup. Environ. Hyg. 9:443–449 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards D.A., Man J.C., Brand P., et al. : Inhaling to mitigate exhaled bioaerosols. Proc. Natl. Acad. Sci. 101:17383–17388 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang W., Elankumaran S. and Marr L.C.: Concentrations and size distributions of airborne influenza A viruses measured indoors at a health centre, a day-care centre and on airoplanes. J. R. Soc. Interface 8:1176–1184 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) : Interim Recommendations for Facemask and Respirator Use to Reduce Novel Influenza A (H1N1) Virus Transmission. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services, Public Health Service, Tuberculosis Control Division, Atlanta. . Available at http://www.cdc.gov/h1n1flu/masks.htm (accessed March 15, 2013).
- Oberg T., and Brosseau L.M.: Surgical mask filter and fit performance. Am. J. Infect. Control 36:276–282 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rengasamy S., Miller A. , Eimer B., and Shaffer R.E.: Filtration performance of FDA-cleared surgical masks. J. Int. Soc. Res. Prot. 26:54–70 (2009). [PMC free article] [PubMed] [Google Scholar]
- Srinivasan A., Jernign D.B., Liedtke L., and Strausbaugh L.: Hospital preparedness for severe acute respiratory syndrome in the United States: Views from a national survey of infectious diseases consultants. Clin. Infect. Dis. 39:272–274 (2004). [DOI] [PubMed] [Google Scholar]
- Cowling B.J., Zhou Y., Leung G.M., Aiello A.E.: Face masks to prevent transmission of influenza virus: A systematic review. Epidemiol. Infect. 138:449–456 (2010). [DOI] [PubMed] [Google Scholar]
- Gralton J., and McLaws M.-L.: Protecting healthcare workers from pandemic influenza: N95 or surgical masks? Crit. Care Med. 38:657–667 (2010). [DOI] [PubMed] [Google Scholar]
- Loeb M., McGeer A., Henry B., et al. : SARS among critical care nurses, Toronto. Emerg. Infect. Dis. 10:251–255 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teleman M.D., Boudville I.C., Heng B.H., Zhu D., Leo Y.S.: Factors associated with transmission of severe acute respiratory syndrome among health-care workers in Singapore. Epidemiol. Infect. 132:797–803 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M.I.C., Leo Y.-S., Ang B.S.P., Heng B.-H., and Choo P.: The outbreak of SARS at Tan Tock Seng Hospital - Relating epidemiology to control. Ann. Acad. Med. Singapore 35:317–325 (2006). [PubMed] [Google Scholar]
- Bischoff W.E., Reid T., Russell G.B., and Peters T.R.: Transocular entry of seasonal influenza-attenuated virus aerosols and the efficacy of N95 respirators, surgical masks, and eye protection in humans. J. Infect. Dis. 204:193–199 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.-A., Grinshpun S.A., and Reponen T.: Respiratory performance offered by N95 respirators and surgical masks: Human subject evaluation with NaCl aerosol representing bacterial and viral particle size range. Ann. Occup. Hyg. 52:177–185 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Wong T., Chung J., et al. : In vivo protective performance of N95 respirator and surgical facemask. Am. J. Ind. Med. 49:1056–1065 (2006). [DOI] [PubMed] [Google Scholar]
- Seto W.H., Yung R.W.H., Ching T.Y., et al. : Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). Lancet 361:1519–1520 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeb M., Dafoe R.N., Mahony J., et al. : Surgical mask vs. N95 respirator for preventing influenza among health care workers - A randomized trial. J. Am. Med. Assoc. 302:1865–1871 (2009). [DOI] [PubMed] [Google Scholar]
- Johnson D.F., Druce J.D., Birch C., and Grayson M.L.: A quantitative assessment of the efficacy of surgical and N95 masks to fitler influenza virus in patients with acute influenza infection. Clin. Infect. Dis. 49:275–277 (2009). [DOI] [PubMed] [Google Scholar]
- Qian Y., Willeke K., Grinshpun S., Donnely J., and Coffey C.C.: Performance of N95 respirators: Filtration efficiency for airborne microbial and inert particles. Am. Indus. Hyg. Assoc. J. 59:128–132 (1998). [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (IOM) : Certifying Personal Protective Technologies: Improving Worker Safety. Washington, D.C.: National Academies Press; . Available at http://www.nap.edu/catalog/12962.html (accessed March 15, 2013). [PubMed] [Google Scholar]
- Rengasamy S., Verbofsky R., King W.P, and Shaffer R.E.: Nanoparticle penetration through NIOSH-approved N95 filtering-facepiece respirators. J. Int. Soc. Res. Prot. 24:49–59 (2007). [Google Scholar]
- Rengasamy S., and Eimer B.: Nanoparticle penetration through filter media and leakage through faceseal interface of N95 filtering facepiece respirators. Ann. Occup. Hyg. 56:568–580 (2012). [DOI] [PubMed] [Google Scholar]
- Han D.H., and Lee J.: Evaluation of particulate filtering respirators using inward leakage (IL) or total inward leakage (TIL) testing—Korean experience. Ann. Occup. Hyg. 49:569–574 (2005). [DOI] [PubMed] [Google Scholar]
- Rengasamy S., Walbert G. F., Newcomb W. E., Rengasamy K. Faulkner, M.J.M., Szalajda J.J. Brannen, and J.: Total inward leakage measurement of particulates for N95 filtering facepiece respirators - A comparison study. Ann. Occup. Hyg. 58:206–216 (2014). [DOI] [PubMed] [Google Scholar]
- Grinshpun S., Haruta H., Eninger R.M., Reponen M., McKay R., and Lee S.-A.: Performance of an N95 filtering facepiece particulate respirator and a surgical mask during human breathing: Two pathways for particle penetration. J. Occup. Environ. Hyg. 6:593–603 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Food and Drug Administration (FDA) : “Guidance for Industry and FDA Staff. Surgical Masks - Premarket Notification [510(k)] Submissions: Guidance for Industry and FDA.” Washington, D.C.: U.S. Department of Health and Human Services, Food and Drug Administration, Center for Devices and Radiological Health. . Available at http://www.fda.gov/cdrh/ode/guidance/094.html (accessed March 15, 2013).


