Abstract
Purpose
Patient-reported outcomes (PROs) is an umbrella term covering a range of outcomes, including symptoms, functioning, health-related quality-of-life, and supportive care needs. Research regarding the appropriate PRO questionnaires to use is informative. A previously published latent class analysis (LCA) examined patterns of function, symptoms, and supportive care needs in a sample of U.S. cancer patients. The current analysis investigated whether the findings from the original study were replicated in new samples from different countries and whether a larger sample combining all the data would affect the classes identified.
Methods
This secondary analysis of data from 408 Japanese and 189 Canadian cancer patients replicated the methods used in the original LCA using data from 117 U.S. cancer patients. In all samples, subjects completed the EORTC-QLQ-C30 and Supportive Care Needs Survey-Short Form-34 (SCNS-SF34). We first dichotomized individual function, symptom, and need domain scores. We then performed LCA to investigate the patterns of domains for each of the outcomes, both in the individual country samples and then combining the data from all three samples.
Results
Across all analyses, class assignment was made by level of function, symptoms, or needs. In individual samples, only two-class models (“high” vs. “low”) were generally identifiable while in the combined sample, three-class models (“high” vs. “moderate” vs. “low”) best fit the data for all outcomes.
Conclusions
In this analysis, the level of burden experienced by patients was the key factor in defining classes.
Keywords: Patient-reported outcomes, quality of life, cancer, supportive care needs, latent class analysis
Introduction
Patient-reported outcomes (PROs) is an umbrella term for various information collected directly from patients about a health condition or its treatment [1; 2]. Different types of PROs include symptoms, functioning, health-related quality-of-life (HRQOL), and supportive care needs. Research regarding the appropriate PRO questionnaires to use [3; 4] is informative.
A prior study by members of our research team used latent class analysis (LCA) to examine the relationship among symptoms, function, and supportive care needs in individual patients [5]. The LCA results categorized 117 cancer patients in the U.S. as either being high or low need, high or low function, and high or low symptom. Further, the results indicated that different domains contributed differentially to class assignment, supporting the need for an approach such as latent class analysis rather than simply summing domains.
This previous study also evaluated whether symptoms, function, and supportive care needs are redundant by examining the concordance of patients' class assignment for each of the three outcomes. That is, we examined the extent to which patients fell in concordant categories (high function/low symptom/low need or low function/high symptom/high need). While a majority of patients (66/117; 56%) were in concordant categories, among patients with a deficit in at least one area (n=68), concordance in classifications was much lower; 75% had some discordance in their classifications. These findings suggest that using scores in one outcome (e.g., symptoms) to predict scores in another (e.g., function) may not be appropriate.
While informative, the previous study was limited by a relatively small sample size and subjects recruited from a single academic institution in the U.S. Because of the small sample size, it is not clear whether the two-class models were found because they best represent the clinical phenomena under study or because the sample size did not allow for the identification of larger (e.g., three-class) models. For example, an alternative classification with more than two classes could have categorized patients based on clusters of symptoms rather than levels of symptom burden (e.g., patients with gastrointestinal symptoms, patients with fatigue, patients without symptoms). Further, because the sample was recruited from a single institution, the generalizability of the findings was unclear.
The primary objective of the current study was to examine whether the findings from the original LCA in the U.S. would be replicated in samples of cancer patients from Canada and Japan. Specifically, we used LCA to investigate a) whether classification of function, symptoms, and needs in the Japanese and Canadian samples followed similar patterns as the original analysis; and b) whether analysis using a larger data set combining all three samples enabled LCA solutions with greater than two classes. We expected that there would be general consistency across samples in the types of classes found but that larger data sets might allow models with more than two classes to emerge. Because our primary research question was concerned with examining the replication of the original findings, we employed the same methodological approach for the current study as was used in the original study.
Methods
Study Population
This secondary analysis compared data collected in prior studies in Japan and Canada to a previously published latent class analysis of data from the U.S.[5] In all three studies, subjects completed the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire Core 30 (QLQ-C30) and the Supportive Care Needs Survey-Short Form-34 (SCNS-SF34). All studies were approved by their respective institutional review boards and conducted in accordance with the 1964 Declaration of Helsinki principles. This secondary data analysis used de-identified data and was considered exempt. Each of the study samples is described briefly below.
U.S. Sample
The original latent class analysis included data from 117 breast, prostate and lung cancer patients currently undergoing treatment and age 18 years or older recruited from the Johns Hopkins Sidney Kimmel Comprehensive Cancer Center between January and May 2006. Detailed information on the study sample has been reported elsewhere [5; 6]. Briefly, the mean age of the 117 patients was 61 years, 49% were female, 77% were white, and 95% had an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1, reflecting good function. Most patients had breast (43%) or prostate (41%) cancer, with fewer lung cancer participants (16%).
Canadian Sample
The Canadian data were drawn from a prospective, multi-site, clustered randomized controlled trial and included newly diagnosed breast or colorectal cancer patients undergoing surgery in greater Toronto. This analysis used the baseline data (i.e., within seven days of discharge from the hospital following surgery) from 189 subjects with a mean age of 60 years, 21% of whom were male. The majority had breast cancer (63%) and the remainder colorectal cancer (37%). Data were collected between December 2005 and February 2009.
Japanese Sample
The Japanese data were originally collected as part of the validation study of the Japanese version of the SCNS-SF34 [7]. The patient sample consisted of 408 ambulatory patients diagnosed with breast cancer with a mean age of 56 and attending the outpatient Oncology, Immunology and Surgery Clinic of Nagoya City University Hospital. These women were in various stages of the cancer trajectory, ranging from 11 to 17,915 days from diagnosis (median 701). Data were collected between February 2006 and April 2007.
Measures
Supportive Care Needs Survey- Short Form-34
The SCNS-SF34 is a self-reported patient measure assessing the perceived needs of cancer patients [8; 9]. Respondents indicate their level of need for help over the last month across five domains of need: Psychological, Health System and Information, Physical and Daily Living, Patient Care and Support, and Sexuality. The following five response options are used: 1=Not applicable (no need); 2=Satisfied; 3=Low need; 4=Moderate need; 5=High need. Domain scores were calculated by averaging the scores of items within each domain.
EORTC-QLQ-C30
The EORTC-QLQ-C30 is a 30-item measure that has been used to assess quality of life in cancer patients in over 3,000 studies worldwide [10]. This measure includes five function subscales (physical, role, emotional, social, and cognitive), eight symptoms (fatigue, pain, nausea & vomiting, dyspnea, insomnia, appetite loss, constipation, and diarrhea), and measures of financial impact and global health/quality of life. All domains are transformed to a 0–100 score, with higher scores on the function domains representing better function and higher scores on the symptom domains representing greater symptom burden.
Statistical Analysis
We used latent class analysis to identify patterns in function, symptoms, and supportive care needs within patients. Latent class analysis models the relationship between discrete observed variables (in this case cancer-related function, symptoms, and supportive care needs) and a categorical latent variable that is not directly measurable [11]. To perform the latent class analysis using the Canadian and Japanese samples, we used the same latent class analysis methods as we used in the original U.S. study [5]. First, we dichotomized the individual domain scores for each of the outcomes to reduce the potential number of possible response patterns and improve the ability to identify classes. We used identical criteria for dichotomization as were used in the initial study. For the five function and eight symptom domain scores from the QLQ-C30, we used as the cut-off mean scores from 1,965 Norwegians sampled at random from the general population and published in the EORTC reference manual [12]. Because of the way the SCNS-SF34 is scored, average scores ≤2.0 represent no unmet need, and scores >2.0 represent some level of unmet need. We used 2.0 as the cut-off, thus differentiating between patients with and without unmet needs. Latent class models were then fit to each of the three sets of outcomes (i.e., function, symptoms, needs). The results of the latent class analyses were then used to categorize patients into classes based on reported patterns of function, symptoms, and needs.
Latent class analysis uses information about the patterns in the data to assign individuals to classes and allows each domain to have a different relationship with class assignment. Unlike simply summing domains to create a scale, which assumes each domain has equal weight, latent class analysis utilizes prevalence information for each domain to help distinguish between classes and allows certain domains to be more or less informative of class assignment.
For each set of outcomes, two and three class models were estimated. Model identifiability was evaluated by comparing point estimates between models and examining the width of posterior intervals of model parameters. Generally, due to limitations in sample size, we fit only two-class models. However, for outcomes where both two and three class models were identifiable, the appropriate number of classes was determined by calculating the Bayesian information criteria (BIC) for each model and selecting the model with the lowest BIC. A Bayesian estimation procedure was chosen because it provides posterior probabilities of class membership. Specifically, from the model results, posterior probabilities were estimated for each subject, defined as the probability of class membership for each class. The posterior probabilities were then used to categorize patients into different classes based on observed patterns of function, symptoms, and needs. Specifically, each patient was placed into one class for each of the three outcomes using the highest posterior probability for that subject. After conducting latent class analyses for each country separately, we then combined the data from the three datasets to determine whether the increased sample size would allow for identification of models with more classes.
Latent class models assume conditional independence, i.e., that there should be no association between function, symptom, or need domains within classes. Thus, we examined all of the possible two-by-two tables of function, symptom, and need domains within classes to test for associations using Fisher's exact test. Due to the number of comparisons (144 domain pairs), we considered p-values < 0.001 to be statistically significant. While this is a small p-value, it is more conservative than a Bonferroni corrected p-value of 0.0003, and would produce more combinations that could violate conditional independence. Latent class analyses were performed using WinBUGS and a Bayesian estimation procedure. Other statistical analyses were performed using R version 2.15.1.
Results
Latent class analysis of function, symptoms, and supportive care needs in individual samples
The results of the Canadian and Japanese latent class analyses largely replicated the findings from the original U.S. sample in that class assignment was made by level of function, symptoms, or needs (“high” vs. “low” in 2-class models; “high” vs. “moderate” vs. “low” in 3-class models). Also, as in the prior analyses, only two-class models (“high” vs. “low”) were identifiable with the exception of symptoms in the larger Japanese sample, in which a three-class model was identified (“high” vs. “moderate” vs. “low”).
In the U.S. and Japanese samples, the majority of patients were in the “high function” class (59% for both); in the Canadian sample, only 40% were categorized as “high function.” Similarly, 62% of the US sample fell in the “low symptom” class compared to 36% in the Canadian sample. The percentage of patients in the “low,” “moderate,” and “high symptom” classes in the Japanese sample were 48%, 35%, and 17% respectively. Finally, the U.S. sample was most likely to be classified as “low need” (70%) compared to 56% in the Canadian sample and 49% in the Japanese sample.
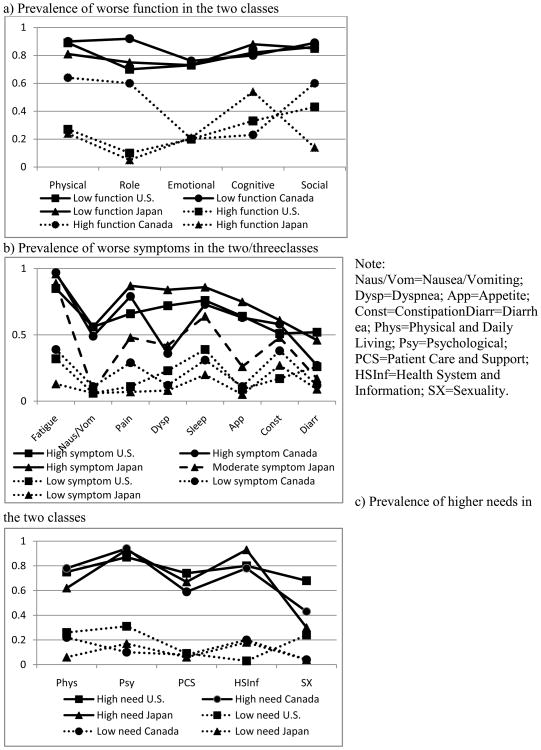
Figure 1 shows the prevalence of worse performance for the different function, symptoms, and supportive care needs classes across the three samples based on the model classes identified. As can be seen in Figure 1 (a), (b), and (c), there was generally good differentiation between or among the classes across all three samples, and differences in prevalence between or among classes ranged considerably (with wider differences revealing greater differentiation in class by that domain). For instance, in the function analyses, emotional function differentiated very well between the “high” and “low” classes in all three samples. Role and physical function did not differentiate well for the Canadian sample though they did for the other samples; social function generally did not differentiate well. In the symptom analyses, fatigue differentiated well between “high” and “low” symptom classes across the three samples while several symptoms (e.g., diarrhea, constipation) did not differentiate well. In the needs analyses, psychologic and health system and information needs differentiated well between “high” and “low” needs groups while sexuality needs differentiated well only for the U.S. sample; sexuality needs differentiated particularly poorly in the Japanese sample because these needs were very uncommon for both classes.
Fig. 1. Prevalence of worse performance in the two/three classes across the different samples.
While in all cases classification was made based on the level of the outcome, there were differences across samples in the prevalence levels. For instance, as shown in Figure 1 (a), the prevalence for those in the “low function” classes was similar for all domains in all three samples, suggesting that the “low function” classification was relatively similar across the samples. By contrast, with the exception of emotional function, the prevalence ranged considerably for those in the “high function” classes across the samples, suggesting differences across samples in the definition of “high function.”
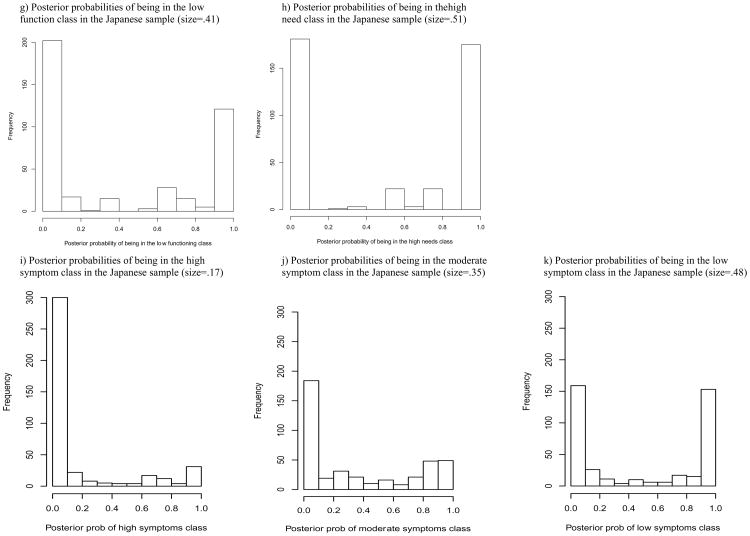
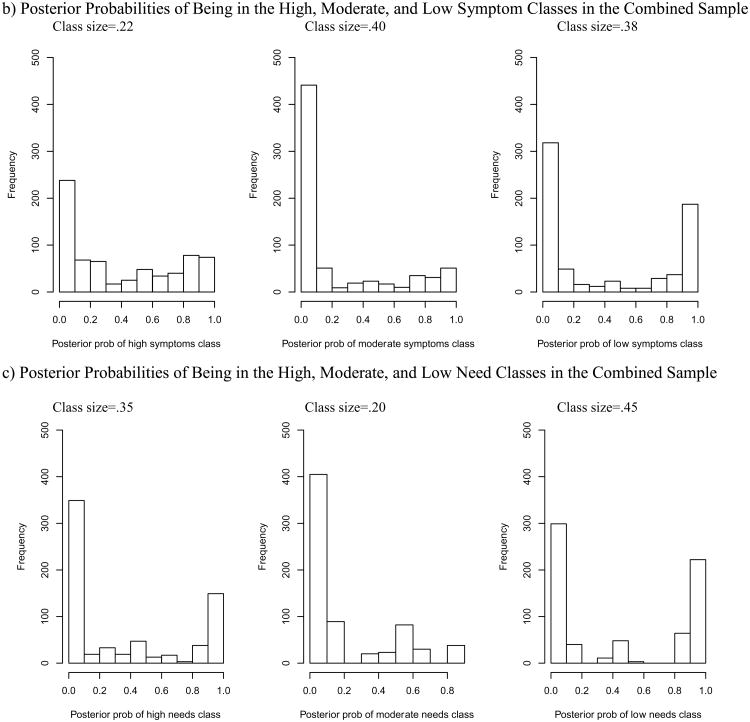
From the model results, posterior probabilities were estimated for each subject. An examination of the posterior probability (i.e., the probability of class membership obtained from model results) for each subject for function, symptoms, and supportive care needs within each sample showed similarities with the prior study. Figure 2 shows the posterior probability of being assigned to the poor performing class for each of the three outcomes in the U.S. [5], Canadian, and Japanese samples. Although some patients fall in the middle (e.g., Canadian “low function” class), most patients had either a very high (>0.90) or very low probability (<0.10) of being assigned to a particular class. This suggests good differentiation with most patients having a very high or low probability of being assigned to the poorly performing class (i.e., “low function”; “high symptom”; “high need”). Among 288 pairs within classes across all analyses in all three samples, only one pair within classes tested was significantly associated with each other at a threshold of p < 0.001, suggesting that the assumption of conditional independence holds.
Fig. 2.
Histograms showing the distributions of model-based posterior probabilities of being assigned to the classes first for the U.S. sample (N=117; From Snyder, Garrett-Mayer, Blackford et al., 2009)[5], followed by the Canadian sample (N=189) and Japanese sample (N=407). Each value represents the probability that a particular individual is in that particular class, given his or her pattern of responses to the QLQ-C30 and SCNS items. Values close to 0 and 1 represent good classification, while values near 0.50 represent class assignment based on chance. Class size is presented as the proportion of the sample (out of 100).
Latent class analysis of function, symptoms, and supportive care needs in combined sample
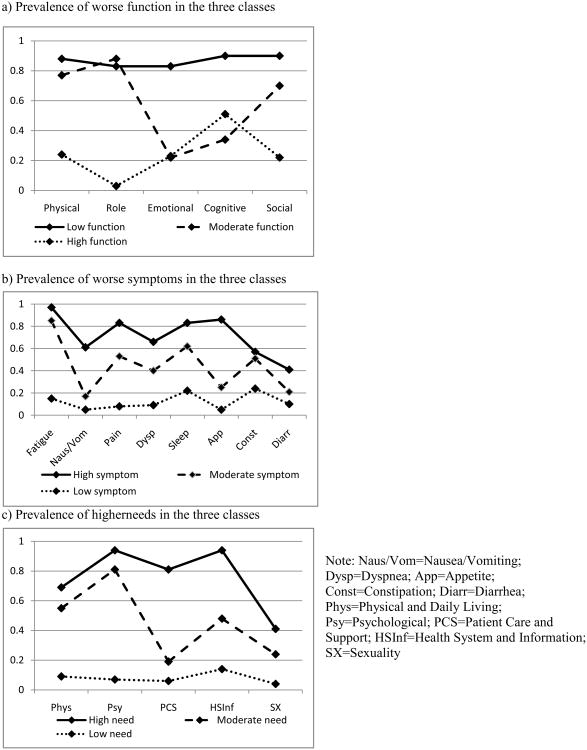
In analyses combining all three samples, a three-class model fit better than a two-class model for each outcome. Figure 3 displays the prevalence of worse performance in the combined sample for each of the three classes (“high,” “moderate”, and “low”). That a three-class model was found suggests that with a larger sample size, a greater number of classes was able to be identified. As in the individual samples, classes were generally assigned based on level rather than type of burden. Thus, the increased sample size allowed for a more granular classification of level of burden but did not lead to stark differences in the types of classes identified. However, there were some nuances; for instance, one different interpretation of the function analyses in the combined sample might be: “consistent low function,” “low physical/role function but moderate others,” and “high physical/role function but moderate others.”
Fig. 3. Prevalence of worse performance in the three classes in the combined sample (N=687).
The plurality of patients was categorized as “high function” (47%), “moderate symptom” (40%), and “low need” (45%). The percentage of patients in the classes with poorest performance (i.e., “low function,” “high symptom” and “high need”) were 37%, 22% and 35%, respectively. Finally, the percentages of patients in the remaining classes (“moderate function,” “low symptom”, and “moderate need”) were 16%, 38%, 20%. We examined the percentage of US, Canadian, and Japanese patients comprising the classes in the combined analyses. For needs, each sample contributed roughly the same percentage of patients to each level (e.g., 25%, 37% and 26% of Canadian, Japanese and U.S. patients were classified as “high need” respectively). However, for function and symptoms, more Canadian patients were assigned to poorly performing classes in the combined sample relative to the other samples. Specifically, more Canadian patients were classified as “low function” (57%) compared to the Japanese and U.S. samples (29% and 32%, respectively) and as “high symptom” (30%) compared to these other samples (16% and 23%, respectively). We also compared the classification of patients in the individual country and combined analyses and found that there was general consistency among the classifications (e.g., patients categorized in the worse class in the individual country analyses tended to be categorized in the worse class in the combined analyses).
As shown in Figure 3 (a), in the function analysis, the “low function” class had a similarly high prevalence of poor function across all domains, while the prevalence of poor function ranged considerably across domains for both the “moderate” and “high function” classes. By contrast, as shown in Figure 3 (b) and (c) representing the symptom and needs analyses, respectively, the “moderate symptom” class and “moderate need” classes had a prevalence for all domains that fell between the two extremes. Fatigue and sleep symptoms were highly prevalent (≥ .62) in both the “moderate” and “high symptom” classes in the symptoms analysis; similarly, psychologic needs were highly prevalent (≥ .81) in both the “moderate” and “high need” classes in the needs analysis. Sexual needs were the least common of all needs overall, but they were nearly twice as common in the “high need” class as in the “moderate need” class.
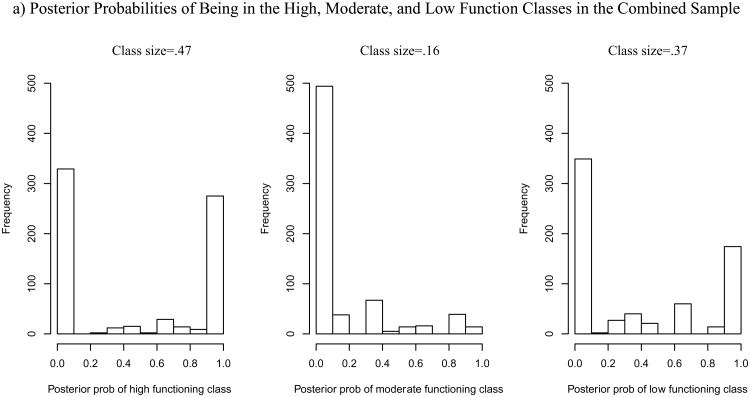
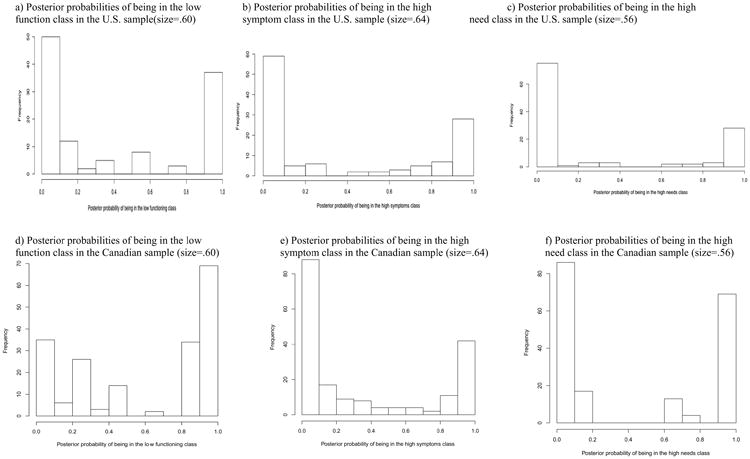
Figure 4 shows the posterior probability of being assigned to classes for function (a), symptoms (b), and supportive care needs (c) in the combined sample. For function, most patients have very high (>0.90) or very low (<0.10) probabilities of being assigned to the “high” or “low function” classes. A much smaller number of patients fell in the “moderate” class (16%) and most patients had a very low (< 0.10) probability of being in the moderate function class but this suggests that the patients assigned to this class are done so appropriately. The probability of being in the “low symptom” or “low need” classes was reasonably well differentiated (either < 0.10 or > 0.90). The difference between the moderate and high symptom classes was less distinguishable. For those assigned to the “moderate” or “high need” classes, the probability of being in the class was not as strong in that fewer patients had a probability > 0.80. There was a clear division between the strong probability of not being in the high or moderate needs class (<0.10) or suggestion of being in either (>0.10). Altogether, only 11 out of 144 pairs within classes tested were significantly associated with each other at a threshold of p < 0.001, so there was no evidence against conditional independence.
Fig. 4.
Histograms showing the distributions of model-based posterior probabilities of being assigned to each class in the combined sample (N=687). Each value represents the probability that a particular individual is in that particular class, given his or her pattern of responses to the QLQ-C30 and SCNS items. Values close to 0 and 1 represent good classification, while values near 0.50 represent class assignment based on chance. Class size is presented as the proportion of the combined sample (out of 100).
Discussion
The current study examined whether cancer patients' patterns of function, symptoms, and supportive care needs were consistent across cultures by comparing whether results of a latent class analysis conducted previously with data from cancer patients in the U.S. [5] would be replicated in samples of cancer patients from Canada and Japan. Indeed, the results of the Japanese and Canadian data analyses were generally consistent with the U.S. findings in that patients were classified based on their level of burden in each of the three outcomes. There were interesting differences in the prevalence of poor (and high) performance, suggesting some variation in the specific classes across the three samples. In other words, what it means to be classified as “high”, “low”, or “moderately” performing may differ in different patient groups. Further, the larger sample size in the analyses combining all three samples allowed three-class models to emerge, but these classifications were still generally based on the level of burden. That we found similarities in the classification of patients across cultures and clinically diverse samples, as well as in the separate and pooled analyses, supports the findings, even though the specific performance of groups across domains might differ in different samples.
Although findings from the study generally supported a method of classification based on level of burden, there were some nuances in our findings that may suggest symptom clusters. Symptom clusters are defined as the presence of three or more concurrent symptoms that are related and may or may not have a similar etiology [13]. For instance, classification of patients from the combined sample function analysis might be interpreted as “consistent low function,” “low physical/role function but moderate others,” and “high physical/role function/moderate others” as opposed to “low”, “moderate,” and “high” function. Given that the identification of symptom clusters has been shown to differ across research samples due to differences in characteristics of the study population (e.g., cancer site, cancer stage, phase in treatment) [14], it is possible that the heterogeneity in the three cross-cultural samples in the current study may have limited our ability to find symptom clusters. In future studies, larger samples using relatively homogeneous groups allowing for a larger number of classes to be tested might be better able to determine whether patients' function, symptoms, and needs are best classified according to level of burden or symptom clusters.
The findings of this study should be interpreted in the context of its strengths and limitations. Important strengths include the inclusion of patients with varying diagnoses, stages of treatment, and countries of origin. While the study sample was quite large when combined, it may not have been large enough to find the presence of symptom clusters in a heterogeneous group. Another major limitation is that differences in demographic and clinical characteristics across the countries in the current study limited our ability to compare whether patients across cultures were similar in their classifications. That is, had this analysis included patient samples at similar points in the cancer trajectory, we could have compared whether patients across cultures experienced similar levels of function, symptoms, and needs. Because of the heterogeneity of our samples, it is unclear whether differences in class sizes across countries were due to clinical reasons alone or whether culture also played a role. For instance, class sizes of the more poorly performing classes were larger in the Canadian sample, and a greater percentage of this sample made up the poorly performing patient classes in the combined analysis, but this sample was recruited immediately after surgery and therefore could be expected to report higher symptom severity or higher supportive care needs. Additionally, taboos against reporting sexuality needs may have contributed to the low self-reported rate of sexuality needs found for the Japanese sample although this would need to be supported by future research. Finally, given that treatments can be a key driver of the patient perspective, future studies should gather complete treatment data – which we did not have – to allow for a detailed analysis of how treatment plays a role in patients' function, symptoms, and supportive care needs and their classification in these outcomes.
An additional limitation is that this analysis did not allow us to examine the concordance of patients' symptoms, function, and needs, as we did in the prior study [5]. As the sample size and therefore the number of classes in the models grew in the current study, it became increasingly difficult to define what classifications would be considered “concordant.” For instance, is moderate function concordant only with moderate symptoms and needs? Continued research examining the associations among cancer patients' function, symptoms, and supportive care needs using the finer gradations that emerged from this study could clarify our understanding of these relationships.
In summary, this analysis supported the findings of our original study that the levels of deficits patients experience in their symptoms, functioning, and supportive care needs are the key factors in classification. Findings support the use of latent class analysis as an informative method for understanding patterns in cancer patients' function, symptoms, and needs. Changes to the methodological or statistical approach employed, including using different cut-off scores to dichotomize performance or employing other statistical methods (e.g., latent profile analysis), could potentially lead to different classifications and should be investigated in future research. Further, future research using longitudinal designs and interventions will allow investigation of how patients' classifications change over time or whether they are amenable to change through interventions (e.g., symptom management, cognitive behavior therapy) [15; 16].
Supplementary Material
Acknowledgments
The authors wish to thank Elizabeth Garrett-Mayer, PhD, for her valuable review of a preliminary draft and for assistance with revising the manuscript. Dr. Snyder is supported by the American Cancer Society (MRSG-08-011-01-CPPB) and is a member of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins (P30CA006973). The original Japanese data collection was supported in part by Grants-in-Aid for Cancer Research and the Third Term Comprehensive 10-Year Strategy for Cancer Control from the Ministry of Health, Labour and Welfare, Japan. The original Canadian data collection was supported by Canadian Institutes of Health Research and Ontario Ministry of Health & Long-term Care.
References
- 1.Acquadro C, Berzon R, Dubois D, Leidy NK, Marquis P, Revicki D, Rothman M. Incorporating the patient's perspective into drug development and communication: an ad hoc task force report of the Patient-Reported Outcomes (PRO) Harmonization Group meeting at the Food and Drug Administration, February 16, 2001. Value Health. 2003;6(5):522–531. doi: 10.1046/j.1524-4733.2003.65309.x. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Food and Drug Administration. Guidance for Industry: Patient Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims. 2009 doi: 10.1186/1477-7525-4-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Snyder CF, Dy SM, Hendricks DE, Brahmer JR, Carducci MA, Wolff AC, Wu AW. Asking the right questions: investigating needs assessments and health-related quality-of-life questionnaires for use in oncology clinical practice. Support Care Cancer. 2007;15(9):1075–1085. doi: 10.1007/s00520-007-0223-1. [DOI] [PubMed] [Google Scholar]
- 4.Snyder CF, Jensen RE, Geller G, Carducci MA, Wu AW. Relevant content for a patient-reported outcomes questionnaire for use in oncology clinical practice: Putting doctors and patients on the same page. Qual Life Res. 2010;19(7):1045–1055. doi: 10.1007/s11136-010-9655-z. [DOI] [PubMed] [Google Scholar]
- 5.Snyder CF, Garrett-Mayer E, Blackford AL, Brahmer JR, Carducci MA, Pili R, Stearns V, Wolff AC, Dy SM, Wu AW. Concordance of cancer patients' function, symptoms, and supportive care needs. Qual Life Res. 2009;18(8):991–998. doi: 10.1007/s11136-009-9519-6. [DOI] [PubMed] [Google Scholar]
- 6.Snyder CF, Garrett-Mayer E, Brahmer JR, Carducci MA, Pili R, Stearns V, Wolff AC, Dy SM, Wu AW. Symptoms, supportive care needs, and function in cancer patients: how are they related? Qual Life Res. 2008;17(5):665–677. doi: 10.1007/s11136-008-9331-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Okuyama T, Akechi T, Yamashita H, Toyama T, Endo C, Sagawa R, Uchida M, Furukawa TA. Reliability and validity of the Japanese version of the Short-form Supportive Care Needs Survey questionnaire (SCNS-SF34-J) Psychooncology. 2009;18(9):1003–1010. doi: 10.1002/pon.1482. [DOI] [PubMed] [Google Scholar]
- 8.Bonevski B, Sanson-Fisher R, Girgis A, Burton L, Cook P, Boyes A. Evaluation of an instrument to assess the needs of patients with cancer. Supportive Care Review Group. Cancer. 2000;88(1):217–225. doi: 10.1002/(sici)1097-0142(20000101)88:1<217::aid-cncr29>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 9.Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P. The unmet supportive care needs of patients with cancer. Supportive Care Review Group. Cancer. 2000;88(1):226–237. doi: 10.1002/(sici)1097-0142(20000101)88:1<226::aid-cncr30>3.3.co;2-g. [DOI] [PubMed] [Google Scholar]
- 10.Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, Haes JCJMd, Kaasa S, Klee M, Osoba D, Razavi D, Rofe PB, Schraub S, Sneeuw K, Sullivan M, Takeda F. The European Organization for Research and Treatment of Cancer QLQ-C30: A Quality-of-Life Instrument for Use in International Clinical Trials in Oncology. Journal of the National Cancer Institute. 1993;85(5):365–376. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 11.Lanza ST, Bray BC, Collins LM. An Introduction to Latent Class and Latent Transition Analysis. In: Weiner IB, editor. Handbook of Psychology: Research Methods in Psychology. Second. Vol. 2. Hoboken, NJ: John Wiley & Sons, Inc; 2013. pp. 691–716. [Google Scholar]
- 12.Fayers PM, Weeden S, Curran D on behalf of the EORTC Quality of Life Study Group. EORTC Reference Values. Brussels: EORTC; 1998. [Google Scholar]
- 13.Dodd MJ, Miaskowski C, Paul SM. Symptom clusters and their effect on the functional status of patients with cancer. Oncol Nurs Forum. 2001;28(3):465–470. [PubMed] [Google Scholar]
- 14.Fan G, Filipczak L, Chow E. Symptom clusters in cancer patients: a review of the literature. Curr Oncol. 2007;14(5):173–179. doi: 10.3747/co.2007.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miaskowski C, Dodd M, Lee K. Symptom clusters: the new frontier in symptom management research. J Natl Cancer Inst Monogr. 2004;(32):17–21. doi: 10.1093/jncimonographs/lgh023. [DOI] [PubMed] [Google Scholar]
- 16.Gift AG, Stommel M, Jablonski A, Given W. A cluster of symptoms over time in patients with lung cancer. Nurs Res. 2003;52(6):393–400. doi: 10.1097/00006199-200311000-00007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.