Abstract
Mothers who are concerned about their young child's weight are more likely to use restrictive feeding, which has been associated with increased food seeking behaviors, emotional eating, and overeating in young children across multiple prospective studies. In the present study, we examined whether mothers' intuitive eating behaviors would moderate the association between their concern about their child's weight and their use of restrictive feeding. In a sample of 180 mothers of young children, two maternal intuitive eating behaviors (i.e., eating for physical reasons, trust in hunger and satiety cues) moderated this association after controlling for maternal age, body mass index, years of education, race/ethnicity, awareness of hunger and satiety cues and perceptions of child weight. More specifically, concern about child weight was unrelated to restrictive feeding for mothers with higher levels of eating for physical reasons and trust in hunger and satiety cues. However, concern about child weight was positively related to restrictive feeding among mothers with lower or average levels of eating for physical reasons and trust in hunger and satiety cues. These findings indicate that it may be important address maternal intuitive eating within interventions designed to improve self-regulated eating in children, as mothers who attend these interventions tend to be highly concerned about their child's weight and, if also low in intuitive eating, may be at risk for using restrictive feeding behaviors that interfere with children's self-regulated eating.
Keywords: restrictive feeding, intuitive eating, child overweight concern, maternal eating behavior, young children
Many efforts have been directed towards increasing public awareness of the prevalence and health correlates of child overweight and obesity. The manner in which child weight-related issues are framed and communicated to the public, however, can be detrimental (Barry, Jarlenski, Grob, Schlesinger, & Gollust, 2011). Saguy and Almeling (2008) conducted a content analysis of scientific articles on weight and health, and corresponding press releases and news reports, to determine how news media filter and translate scientific information to the public. They found that news media frequently (a) dramatize and exaggerate weight-related health risks, (b) blame parents for their child's weight, and (c) emphasize individual behavior change as the solution. Given that the majority of adults obtain health information via the news media (Kaiser Family Foundation, 2001; Pew Research Center, 2014), many parents may be exposed to these alarmist media messages and express concern about their child being or becoming overweight (Barry et al., 2011; Saguy & Almeling, 2008).
Indeed, data show that parents perceive health risks associated with childhood overweight and obesity, are concerned about their child being or becoming overweight, see themselves as responsible for their child's weight, and are motivated to alter their feeding practices to prevent or alleviate their child's weight gain (Etelson, Brand, Patrick, & Shirali, 2003). Because mothers are often expected to assume feeding responsibilities within the family, they especially may be held accountable (and hold themselves accountable) for their child's weight (Saguy & Almeling, 2008). When concerned about their child being overweight, then, some mothers may use restrictive feeding, or limiting a child's intake of sweets, high fat foods, and favorite foods and using these foods as rewards for good behavior (Birch et al., 2001). This process may be understood through the lens of an affect regulation framework (Webb, Butler-Ajibade, & Robinson, 2014). Specifically, being concerned about their child's weight could constitute negative affect for mothers (e.g., worry, anxiety, shame, guilt), and mothers can obtain relief from this negative affect by engaging in “proactive” efforts to lower their child's weight (or slow weight gain) by restricting their child's food intake (Webb et al., 2014). Indeed, many researchers have reported an association between mothers' concern about their child's weight and their restrictive feeding practices—a correlation which is significant, positive in direction, and typically moderate in strength (e.g., Birch, Fisher, & Davison, 2003; Birch et al., 2001; Francis, Hofer, & Birch, 2001; May et al., 2007; Tylka, Eneli, Kroon Van Diest, & Lumeng, 2013; Webber, Hill, Cook, Carnell, & Wardle, 2010).
While restricting children's access to palatable foods may appeal to mothers as a straightforward means of controlling weight (Fisher & Birch, 1999), several longitudinal and experimental studies have found restrictive feeding to be largely counterproductive. Mothers' restrictive feeding predicted their young (age 2 years) child's increased likelihood of overeating and emotional eating a year later (Rodgers et al., 2013). Parents' reports of restrictive feeding when their child was age 5 years predicted their child's increased eating in the absence of hunger at ages 7 and 9, with this link being stronger for overweight children (Birch et al., 2003; Fisher & Birch, 2002). When parents restricted their child's access to palatable foods in experimental tasks, the child responded with focused attention on the restricted food and displayed an increased desire to obtain and consume those foods (Fisher & Birch, 1999; Ogden, Cordey, Cutler, & Thomas, 2013; Rollins, Loken, Savage, & Birch, 2014). Rollins et al. further found that the association of restrictive feeding with increased food intake was stronger among children with lower self-regulation and higher appetitive drive. Conversely, when preschool children were taught to identify and eat in response to their internal hunger and satiety cues, they improved their ability to self-regulate their energy intake (Birch, McPhee, Shoba, Steinberg, & Krehbiel, 1987; Johnson, 2000). Although restrictive feeding has not been linked to future child weight gain or overeating in all studies (see Campbell et al., 2013), the collective body of research raises significant concerns about using restrictive feeding to control child weight.
Many mothers who are concerned about their child's weight may not choose to use restrictive feeding to prevent or alleviate weight gain in their child. Indeed, the correlation between maternal concern about child weight and restrictive feeding, while significant, is not extremely strong (see Birch et al., 2001, 2003; Francis et al., 2001; May et al., 2007; Tylka et al., 2013; Webber et al., 2010), suggesting that third variables may influence the strength of this relationship. Indeed, an affect regulation framework proposes that moderators, which represent individual variability, help determine the strength between situation-specific negative affect and coping strategies (Webb et al., 2014).
Perhaps mothers' own eating behaviors moderate the association between their concern about their child's weight and their restrictive feeding. Indeed, mothers' own eating behaviors have been found to be associated with how they feed their children. In a longitudinal study, Francis and Birch (2005) found that mothers who were preoccupied with their own weight and food intake reported increased levels of restricting their daughters' food intake. Similarly, mothers who restricted their own food intake and ate in the absence of hunger were more likely to restrict their young child's food intake (Birch & Fisher, 2000; Brown & Lee, 2011). However, to our knowledge, no study has examined whether mothers' eating behaviors moderate the association between concern about child weight and restrictive feeding.
In the present study, we examined whether maternal intuitive eating behaviors moderate the association between maternal concern about their child's weight and maternal use of restrictive feeding with their child. Intuitive eating is a flexible eating style characterized by trusting in and mainly following physiological hunger and satiety cues to determine when, what, and how much to eat (Tribole & Resch, 2012; Tylka, 2006). Intuitive eating, as described by Tylka (2006) is characterized by (a) eating for physical rather than emotional reasons, (b) unconditional permission to eat, and (c) reliance on internal hunger and satiety cues. Eating for physical rather than emotional reasons represents a pattern of eating when physically hungry rather than to cope with emotional distress, such as loneliness, anxiety, and boredom. Unconditional permission to eat reflects a willingness to eat when hungry rather than trying to stave off hunger and being inclusive with food choice (i.e., refusing to label certain foods as forbidden); unconditional permission to eat is not the same as disinhibited eating, which entails overeating in response to external cues such as daily circumstances, stress, or social settings (Stunkard & Messick, 1985). Reliance on internal hunger and satiety cues encompasses a general awareness of hunger and satiety cues and trust in these internal cues to direct when, what, and how much to eat, with subsequent research supporting a clear distinction between awareness and trust in internal cues among early adolescents (Dockendorff, Petrie, Greenleaf, & Martin, 2012). Among women, intuitive eating has been found to be associated adaptively with physical health (e.g., lower triglyceride levels, higher high density lipoprotein cholesterol), and psychological well-being (e.g., lower disordered and disinhibited eating as well as higher life satisfaction, body appreciation, and interoceptive sensitivity; Augustus-Horvath & Tylka, 2011; Denny, Loth, Eisenberg, Neumark-Sztainer, 2013; Hawks, Madanat, Hawks, & Harris, 2005; Herbert, Blechert, Hautzinger, Matthias, & Herbert, 2013; Madden, Leong, Gray, & Horwath, 2012; Smith & Hawks, 2006; Tylka & Wilcox, 2006; Van Dyke & Drinkwater, 2013).
It is plausible that maternal intuitive eating could buffer the association between mothers' concern about their child's weight and their use of restrictive feeding. Mothers who trust their own internal hunger and satiety cues may be likely to trust their child's ability follow his or her internal cues. When concerned about their child's weight, restrictive feeding may feel disingenuous for mothers high in intuitive eating, given that restrictive feeding practices are antithetical to trusting a child's internal cues to determine what, when, and how much to eat. Thus, mothers high in intuitive eating may refrain from using restrictive feeding. Conversely, by definition, mothers low in intuitive eating mistrust their internal hunger and satiety cues to regulate their eating and weight. When mothers low in intuitive eating are unconcerned about their child's weight, they may feel that there is no need to restrict their child's intake of high fat, high sugar, and favorite foods. Yet, when mothers low in intuitive eating are concerned about their child's weight, they may assume that their child's internal cues also cannot be trusted and feel it necessary to restrict their child's food intake.
Therefore, we hypothesized that intuitive eating would weaken the relationship between mothers' concern about their child's weight and restrictive feeding. That is, for mothers low in intuitive eating, concern about child weight would be strongly related to restrictive feeding; however, for mothers high in intuitive eating, concern about child weight would be unrelated to restrictive feeding. We examined three components of intuitive eating separately (i.e., eating for physical rather than emotional reasons, unconditional permission to eat, and trust in internal hunger and satiety cues), as research has upheld their distinction (Dockendorff et al., 2012; Tylka, 2006). We controlled for maternal variables that have been shown to be associated with mothers' feeding practices and/or concern about their child's weight, such as age (Hurley, Black, Papas, & Caufield, 2008), years of education (Crawford, Timperio, Telford, & Salmon, 2005), race/ethnicity (Cardel et al., 2012; Loth, MacLehose, Fulkerson, Crow, & Neumark-Sztainer (2013), body mass index (BMI; Webber et al., 2010), and perceptions of child weight (Francis et al., 2001). We also controlled for mothers' awareness of their hunger and satiety cues; theoretically, mothers who are not as aware of their internal hunger and satiety cues may worry that their child will also struggle with sensing these cues and attempt to help the child by placing restrictions on his or her eating. If our hypothesis is supported, the present study could serve as the foundation for more rigorous evaluations of whether maternal intuitive eating is a protective factor against restrictive feeding. Pursuing such investigations may yield clinical benefits, given that intuitive eating skills can be effectively taught (Bacon et al., 2002; Bacon, Stern, Van Loan, & Keim, 2005; Bush, Rossy, Mintz, & Schopp, 2014; Schaefer & Magnuson, 2014).
Method
Participants
Data from 180 mothers of young children were analyzed. Mothers' average age was 34.31 years (SD = 6.05), and the child's average age was 3.40 years (SD = 0.98, range = 2 to 5 years old). Mothers identified as Caucasian (70.6%), African American (16.7%), Asian (8.3%), Latina (2.2%), or Native American (1.7%). Mothers' average BMI, calculated from self-reported height and weight, was 26.41 (SD = 6.51): 46.7% were classified as normal weight, 20.6% as overweight, 21.1% as obese, and 11.7% as underweight (see CDC, 2010). In terms of mothers' highest level of education, 31.7% completed graduate school, 4.6% received some graduate education, 27.8% graduated college, 21.2% received some college education, 12.8% completed high school, and 2.2% received at least three years of high school education. On average, they reported 18 years of education. Mothers were married (63.3%), single (21.1%), divorced (5.6%), living with their significant other but not married (6.1%), separated (2.8%), or widowed (0.6%).
Measures
If mothers had multiple children, they were instructed to choose one child between the ages of 2 and 5 years old and report on their concern about this child's weight, their restrictive feeding with this child, and their perception of this child's weight.
Concern about child's weight
The Concern about Child Weight subscale of the Child Feeding Questionnaire (CFQ; Birch et al., 2001) assesses the degree to which parents are concerned about their child being overweight and eating too much food. This subscale contains three items (e.g., “How concerned are you about your child becoming overweight”) that are rated along a 5-point scale ranging from Unconcerned (scored as 1) to Concerned (scored as 5). Item responses are averaged. Estimates have upheld the internal consistency reliability (Cronbach's α = .75) and construct validity (via its positive relationship with child's weight status) of its scores in a sample of U.S. parents (Birch et al., 2001). Cronbach's alpha was .79 in the present study.
Restrictive feeding
The Restriction subscale of the CFQ (Birch et al., 2001) measures the degree to which parents limit the child's intake of sweets and fats. It contains eight items (e.g., “I have to be sure my child does not eat too many high fat foods”) that are rated along a 5-point scale ranging from Disagree (scored as 1) to Agree (scored as 5). Estimates have supported the internal consistency reliability (Cronbach's α = .73) and construct validity (via its relationships with other controlling feeding practices) of its scores among a sample of parents from the U.S. Cronbach's alpha was .73 in the present study.
Intuitive eating
The 21-item Intuitive Eating Scale (IES; Tylka, 2006) measured mothers' tendency to trust in and eat in response to their own internal hunger and satiety cues. While Tylka (2006) divided the IES into three subscales (Tylka, 2006): Eating for Physical Rather than Emotional Reasons (EPR), Unconditional Permission to Eat (UPE), and Reliance on Internal Cues (RIC), other researchers have noted heterogeneity within the RIC subscale among adolescents, and suggested that it can be further divided into two subscales: Awareness of Internal Cues (AIC) and Trust in Internal Cues (TIC; Dockendorff et al., 2012). For the purposes of our study, we calculated four subscale scores: EPR (six items, e.g., “I use food to help me soothe my negative emotions”—reverse scored), UPE (nine items, e.g., “If I am craving a certain food, I allow myself to have it), AIC (three items, e.g., “When I'm eating, I can tell when I am getting full”), and TIC (three items, e.g., “I trust my body to tell me when to eat”). We used EPR, UPE, and TIC as moderators, and AIC to estimate mothers' awareness of their hunger and satiety cues, which we included as a covariate. All IES items are rated along a 5-point scale ranging from strongly disagree (scored as 1) to strongly agree (scored as 5) and averaged. Tylka (2006) reported evidence for the subscale scores' internal consistency reliability (Cronbach's αs ranged from .72 - .89) and construct validity via their inverse associations with eating disorder symptoms and poor interoceptive awareness among U.S. college women. In the present study, Cronbach's alphas were .88 for EPR, .76 for UPE, .79 for TIC, and .75 for AIC.
Perceived child weight
The CFQ Perceived Child Weight subscale (Birch et al., 2001) was used to gauge maternal perceptions of their child's weight status, which was treated as a covariate. This subscale asks participants, “Please indicate how you would classify your child's weight” at three life stages: as a toddler, preschooler, and kindergartener. Anchors for these items were Markedly or Very Underweight (scored as 1), Underweight (scored as 2), Average Weight (scored as 3), Overweight (scored as 4), and Markedly or Very Overweight (scored as 5). The child's age guided which of the three subscale items was interpreted. We chose to assess maternal perceptions of their child's weight status using these verbal descriptors in lieu of their child's BMI percentile for three reasons: (a) reporting child's weight and height during times of rapid growth may promote numerical inaccuracies and/or missing data, (b) maternal perceptions of child weight are likely to be more influential in determining how child weight may shape their feeding practices than an objective measure (i.e., BMI percentile), and (c) this subscale was found to be strongly related in a positive direction to child BMI percentile, lending support for its convergent validity (Webber et al., 2010).
Demographic data
Participants were asked to report their age, race/ethnicity, highest level of education, height, weight, relationship status, and child's age, as well as whether their child had any food allergies or conditions that would alter their feeding practices.
Procedure
After Institutional Review Board approval was granted from a large Midwestern U.S. Children's Hospital, mothers of young children were recruited from four childcare centers and a primary care clinic in an urban area. At childcare centers, staff distributed the survey to all mothers of children in the toddler and preschool classrooms. Centers were selected to increase participant diversity: one center was located on a large university campus, the second center was in an urban setting, the third center was situated in a low income area and offered subsidized childcare, and the fourth center was located in a semirural area. At the primary care clinic, eligible mothers with a young child were approached in the waiting room and invited to complete the survey. Mothers completed the survey at their convenience and mailed it back to the experimenters in the provided stamped, addressed envelope. They each received a $10 grocery card in exchange for completing the survey.
From 297 survey packets distributed, 188 were returned, yielding a response rate of 63%. We excluded eight participants who did not complete the survey. Although we planned to exclude participants with children who have congenital or metabolic abnormalities or serious food allergies because these conditions likely affect feeding practices, no mother indicated that her child had any of these conditions. Thus, data from 180 mothers were analyzed.
Data Analyses
First, we computed Pearson r correlations between the major study variables and the covariates. Next, we performed four hierarchical regression analyses with restrictive feeding as the criterion. For each, we entered maternal age, BMI, years of education, ethnicity1, awareness of internal cues, and perception of child's weight as covariates at Step 1. At Step 2, we entered maternal concern about child weight and a component of intuitive eating; these variables were centered to reduce multicollinearity between the main effect and interaction terms. At Step 3, we entered an interaction term created by multiplying the centered maternal concern about child weight and intuitive eating component variables. Moderation is evident when the interaction is a significant increment in R2 (i.e., ΔR2) at Step 3. However, because significant interactions are notoriously difficult to detect in nonexperimental research (McClelland & Judd, 1993), we also considered the effect size of the interaction. Given that interactions typically only account for between 1-3% of additional variance, we considered ΔR2 values at or above .01 to make unique and meaningful contributions to the criterion. For significant interactions, we conducted a simple slopes analysis (Aiken & West, 1991), which reveals the strength of the association between maternal concern about child weight and restrictive feeding at low (1 SD below the mean), average (at the mean), and high (1 SD above the mean) levels of the moderator (i.e., intuitive eating component). The strengths of these associations were considered strong at βs ≥ .35, moderate at βs ≤ .34 and > .02, and weak at βs ≤ .02 (Cohen, 1992). Last, we plotted the regression slopes of significant interactions.
Results
Preliminary Analyses
Across all measures, the count for individual missing data points across all items was low, ranging from 0 to 2.0% (M = 0.82%). Thus, we used mean substitution to estimate the few missing item values. All measures were normally distributed, and skewness and kurtosis values did not violate the assumptions of our planned analyses (Kline, 2010). No outliers were detected. Means, standard deviations, and correlations for the main study variables and covariates are presented in Table 1. Mothers' concern about their child's weight was positively related to their restrictive feeding practices and inversely related to their intuitive eating behaviors. Mothers' unconditional permission to eat was inversely related to their restrictive feeding.
Table 1. Means, Standard Deviations, and Correlations among Study Variables.
| Variable | M | SD | Range | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. IES: Eating for physical reasons | 3.28 | 0.99 | 1-5 | |||||||||
| 2. IES: Unconditional permission to eat | 3.18 | 0.73 | 1-5 | .46*** | ||||||||
| 3. IES: Awareness of hunger and satiety | 3.96 | 0.71 | 1-5 | .34*** | .06 | |||||||
| 4. IES: Trust in internal cues | 3.40 | 0.95 | 1-5 | .41*** | .31*** | .34*** | ||||||
| 5. CFQ: Restrictive feeding | 2.95 | 0.62 | 1-5 | -.09 | -.19** | .07 | .09 | |||||
| 6. CFQ: Concern about child weight | 2.01 | 1.15 | 1-5 | -.23** | -.25*** | -.15* | -.28*** | .24*** | ||||
| 7. Maternal age | 34.31 | 6.05 | 20-48 | .00 | -.01 | -.01 | -.02 | -.07 | .08 | |||
| 8. Maternal body mass index | 26.41 | 6.51 | 19-47 | -.31*** | -.17* | -.26*** | -.34*** | .06 | .34*** | -.11 | ||
| 9. Maternal education | 18.19 | 4.71 | 11-25 | -.05 | -.11 | .05 | .06 | -.04 | -.19** | .42*** | -.27*** | |
| 10. Perceived Child Weight | 2.95 | 0.46 | 1-5 | -.11 | -.02 | -.08 | .02 | .13 | .31*** | .07 | .12* | -.09 |
Note. N = 180. IES = Intuitive Eating Scale. CFQ = Child Feeding Questionnaire.
p < .05.
p < .01.
p < .001.
Hierarchical Regression Analyses
Eating for physical reasons
Eating for physical rather than emotional reasons buffered the relationship between maternal concern about child weight and restrictive feeding (see Table 2). The interaction term accounted for 2.7% of additional variance in restrictive feeding. The simple slopes analysis showed that maternal concern about child weight was not related to restrictive feeding for women high (1 SD above the mean) on eating for physical reasons, β = .089, t(179) = 0.83, p = .408. However, maternal concern about child weight was positively related to restrictive feeding at a strong degree for women low (1 SD below the mean) on eating for physical reasons, β = .366, t(179) = 3.85, p < .001, and at a moderate degree for women with average levels of eating for physical reasons, β = .227, t(179) = 3.04, p = .003.
Table 2. Three Hierarchical Multiple Regression Analyses Exploring Intuitive Eating as a Buffer of the Relationship between Maternal Concern about Child Weight and Restrictive Feeding.
| Variables (at Step 3 of each regression) | Total R2 | ΔR2 | B | SE | β | t(179) | p |
|---|---|---|---|---|---|---|---|
| Maternal age | -0.009 | 0.008 | -.086 | -1.092 | .277 | ||
| Maternal body mass index | -0.001 | 0.008 | -.006 | -0.079 | .937 | ||
| Maternal years of education | 0.004 | 0.011 | .028 | 0.331 | .741 | ||
| Maternal ethnicity | -0.502 | 0.143 | -.262 | -3.511 | .001 | ||
| Maternal perception of child weight | 0.043 | 0.009 | .033 | 0.431 | .667 | ||
| Maternal awareness hunger and satiety | 0.122 | 0.067 | .140 | 1.822 | .070 | ||
| Maternal concern about child weight | 0.148 | 0.043 | .278 | 3.446 | .001 | ||
| Maternal eating for physical reasons | -0.066 | 0.052 | -.104 | -1.273 | .205 | ||
| Concern × eating for physical reasons | .202 | .027 | -0.087 | 0.037 | -.171 | -2.344 | .020 |
|
| |||||||
| Maternal age | -0.007 | 0.008 | -.067 | -0.835 | .405 | ||
| Maternal body mass index | 0.001 | 0.008 | .015 | 0.187 | .852 | ||
| Maternal years of education | -0.002 | 0.011 | -.015 | -0.170 | .865 | ||
| Maternal ethnicity | -0.476 | 0.142 | -.248 | -3.338 | .001 | ||
| Maternal perception of child weight | 0.097 | 0.099 | .074 | 0.977 | .330 | ||
| Maternal awareness hunger and satiety | 0.104 | 0.066 | .120 | 1.586 | .115 | ||
| Maternal concern about child weight | 0.131 | 0.045 | .247 | 2.909 | .004 | ||
| Maternal unconditional permission to eat | -0.120 | 0.067 | -.139 | -1.805 | .073 | ||
| Concern × unconditional permission | .184 | .006 | -0.054 | 0.052 | -.077 | -1.053 | .294 |
|
| |||||||
| Maternal age | -0.011 | 0.008 | -.106 | -1.319 | .189 | ||
| Maternal body mass index | 0.004 | 0.008 | .040 | 0.496 | .621 | ||
| Maternal years of education | 0.004 | 0.011 | .028 | 0.346 | .730 | ||
| Maternal ethnicity | -0.431 | 0.141 | -.225 | -3.046 | .003 | ||
| Maternal perception of child weight | 0.059 | 0.099 | .045 | 0.593 | .554 | ||
| Maternal awareness hunger and satiety | 0.078 | 0.068 | .090 | 1.150 | .252 | ||
| Maternal concern about child weight | 0.159 | 0.044 | .298 | 3.597 | <.001 | ||
| Maternal trust in internal cues | 0.078 | 0.052 | .120 | 1.487 | .139 | ||
| Concern × trust in internal cues | .196 | .022 | -0.087 | 0.041 | -.155 | -2.110 | .036 |
N = 180.
The regression slopes of this interaction are plotted in Figure 1. When mothers had low levels of concern about their child's weight, they were relatively similar in their levels of restrictive feeding, regardless of their level of eating for physical reasons. However, when mothers were concerned about their child's weight, mothers with high levels of eating for physical rather than emotional reasons were much less likely to use restrictive feeding than mothers with average or low levels of eating for physical rather than emotional reasons.
Figure 1.
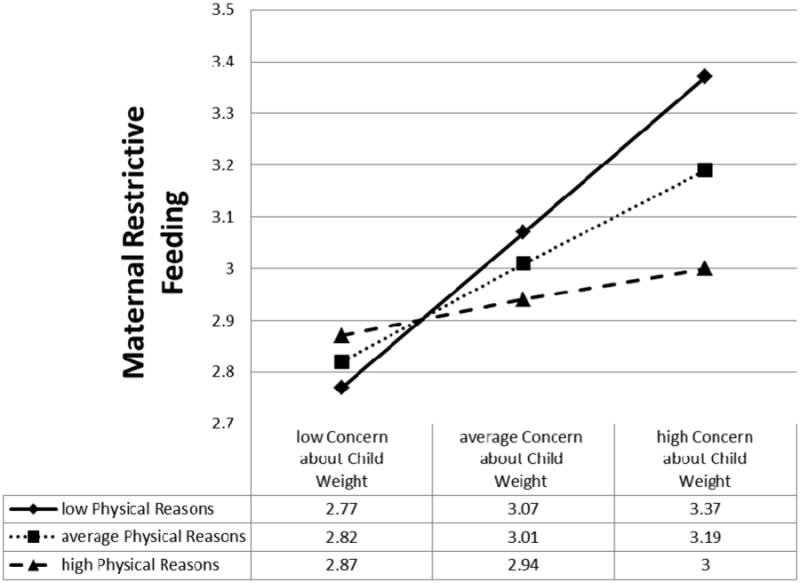
Regression lines showing the relationships between maternal concern about child weight and restrictive feeding by low (-1 SD), average (mean), and high (1 SD) levels of maternal eating for physical rather than emotional reasons. The full data set (N = 180) was used to calculate the regression lines.
Unconditional permission to eat
Contrary to hypotheses, unconditional permission to eat did not moderate the relationship between maternal concern about child weight and restrictive feeding. This analysis is presented in Table 2.
Trust in internal cues
Mothers' trust in internal hunger and satiety cues buffered the relationship between their concern about their child's weight and restrictive feeding (see Table 2). The interaction term accounted for 2.2% of additional variance in restrictive feeding. The simple slopes analysis demonstrated that maternal concern about child weight was not related to restrictive feeding for women with high (1 SD above the mean) trust in internal cues, β = .123, t(179) = 1.07, p = .286. In contrast, maternal concern about child weight was positively related to restrictive feeding to a strong degree for women with low (1 SD below the mean) trust in internal cues, β = .426, t(179) = 4.52, p < .001, and to a moderate degree for women with average trust in internal cues, β = .274, t(179) = 3.61, p < .001.
Figure 2 contains the regression slopes of this interaction. At low levels of concern about their child's weight, mothers who reported low trust in their internal hunger and satiety cues reported lower restrictive feeding compared to mothers who reported high trust in their internal cues. However, mothers who reported low trust in their internal cues had a steep incline in their restrictive feeding practices as they reported higher concern with their child's weight. Conversely, mothers who reported high trust in their internal cues did not have a significant incline in restrictive feeding as they reported higher concern with their child's weight.
Figure 2.
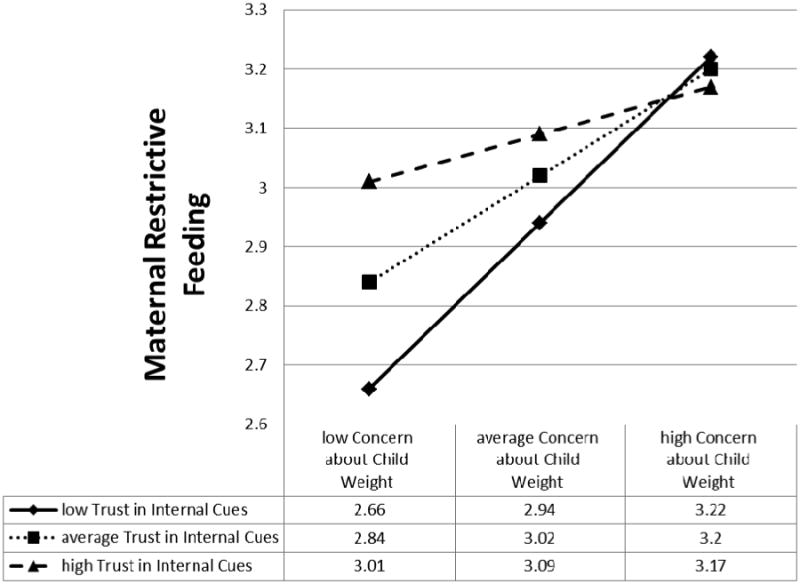
Regression lines showing the relationships between maternal concern about child weight and restrictive feeding by low (-1 SD), average (mean), and high (1 SD) levels of maternal trust in internal hunger and satiety cues. The full data set (N = 180) was used to calculate the regression lines.
Discussion
Many mothers who are concerned about their child's weight use restrictive feeding with a goal of controlling their child's weight and preventing excessive weight gain (Birch et al., 2001, 2003; Francis et al., 2001; May et al., 2007; Tylka et al., 2013; Webber et al., 2010). Restrictive feeding, however, has been reported to contribute to subsequent maladaptive outcomes for children, including increased overeating, emotional eating, eating in the absence of hunger, and preoccupation with the restricted foods (Birch et al., 2003; Fisher & Birch, 1999, 2002; Ogden et al., 2014; Rodgers et al., 2013; Rollins et al., 2014). Thus, identifying maternal variables that are associated with a weaker relationship between maternal concern about child weight and restrictive feeding may be informative for the prevention and treatment of maladaptive child eating behaviors linked to restrictive feeding. After controlling for several maternal variables including age, years of education, ethnicity, BMI, awareness of hunger and satiety cues, and perception of their child's weight, two maternal intuitive eating behaviors buffered this relationship: (a) eating for physical rather than emotional reasons and (b) trust in internal hunger and satiety cues. Mothers' unconditional permission to eat, however, did not buffer this relationship.
More specifically, mothers who reported high levels of eating in response to their physical hunger cues rather than emotions did not restrict their child's food intake and choices when concerned about their child's weight. Yet, for mothers who scored low on this intuitive eating component, their concern about their child's weight was strongly associated with higher restrictive feeding. A similar pattern emerged for mothers' trust in their internal hunger and satiety cues to guide their eating. When mothers reported high trust in their hunger and satiety cues, their concern about their child's weight was unrelated to their restrictive feeding. However, when mothers reported low trust in their hunger and satiety cues, their concern about their child's weight was strongly related to restrictive feeding in a positive direction.
While maternal eating for physical reasons and trust in internal hunger and satiety cues similarly moderated the relationship between maternal concern about child weight and restrictive feeding, the point at which their regression slopes interacted differed (see Figures 1 and 2). Maternal eating for physical reasons differentiated mothers' restrictive feeding more so at high levels of maternal concern about child weight compared to low levels of maternal concern about child weight—this pattern was expected. Conversely, maternal trust in internal hunger and satiety cues differentiated mothers' restrictive feeding more so at low levels of maternal concern about child weight compared to high levels of maternal concern about child weight. While it appears that mothers who distrust their internal hunger and satiety cues could promote low restrictive feeding when unconcerned about their child's weight, this pattern shifts to high restrictive feeding when mothers who distrust their internal cues are concerned about their child's weight. Given the prevalence of news media messages touting the hazards of childhood overweight and obesity that are often dramatized and misrepresentative of the scientific literature (Barry et al., 2011; Saguy & Almeling, 2008), mothers' lack of concern about child's weight may be precarious and increase with events such as exposure to news media on health and weight, witnessing their child gaining weight, and/or considering the child's genetic propensity to overweight or obesity (Etelson et al., 2003; Webber et al., 2010). Regardless of the point of interaction, both sets of regression slopes indicate that mothers high in these particular intuitive eating behaviors are less likely to respond to their concern about their child's weight with heightened restrictive feeding. Thus, according to an affect regulation framework (Webb et al., 2014), individual differences in mothers' intuitive eating help determine the strength between situation-specific negative affect (concern about child weight) and counterproductive behavioral efforts to reduce their negative affect by restrictive feeding.
Consequently, the present study's findings provide preliminary support for the assertion that maternal eating for physical rather than emotional reasons and trust in internal hunger and satiety cues may be protective against restrictive feeding. For mothers high in these two intuitive eating components, restrictive feeding may feel disingenuous, given that restrictive feeding would be antithetical to their beliefs that the body's internal hunger and satiety cues are reliable and can be trusted to determine what, when, and how much to eat. Yet, mothers low in these intuitive eating components may feel the need to restrict their child's feeding because, in the mothers' experience, internal hunger and satiety cues cannot be trusted and/or reliably followed (e.g., beliefs that if they eat when hungry, they will gain too much weight).
It is important to acknowledge the present study's limitations, which carve avenues for future research. First, the present study is limited in terms of its design. Because our data are collected at one time point, our proposition that maternal intuitive eating may be protective against restrictive feeding is speculative. Nevertheless, our preliminary findings lay the groundwork and rationale for conducting future longitudinal and experimental explorations of maternal intuitive eating as a protective factor against restrictive feeding. We also used the original version of the IES in lieu of the IES-2 (Tylka & Kroon Van Diest, 2013), which was not published when data collection began for the present study. Along with its original subscales, the IES-2 assesses the tendency to make food choices that honor health by promoting energy, stamina, and body performance, while also tasting good. Researchers could explore whether this newly developed subscale moderates the relationship between maternal concern about child weight and restrictive feeding. In addition, we did not assess alternative feeding strategies mothers high in intuitive eating use when concerned about their child's weight. Researchers could investigate whether division of feeding responsibility (Eneli, Crum, & Tylka, 2008; Satter, 2005; Tylka et al., 2013) and covert monitoring (Brown, Ogden, Vögele, & Gibson, 2008) are alternative feeding strategies that mothers choose when high in both intuitive eating and concern about child weight. Moreover, our findings are based on self-report data, and thus it is possible that participants did not accurately report their responses due to social desirability, memory, and/or response style. Future studies could weigh and measure mothers and children in a laboratory setting to more confidently control for BMI and gather observational data via videotaped feeding sessions and hunger and satiety ratings across multiple time periods.
Second, our study is limited in that it did not consider other maternal and child variables that may impact the findings. We did not estimate biological underpinnings that could alter the relationships between maternal concern about child weight, intuitive eating, and feeding behaviors. Some individuals are not as responsive to satiety cues due to genetic factors, and relying on their satiety cues may thus prompt overeating and weight gain (den Hoed, Westerterp-Plantenga, Bouwman, Mariman, & Westerterp, 2009; English, Ghatei, Malik, Bloom, & Wilding, 2002). Mothers who cannot sense their satiety cues may be concerned that their child will not be able to sense his or her satiety cues, and mothers may then impose restrictions their young child's eating. Furthermore, mothers' negative attitudes towards fat (e.g., anti-fat bias, thin-ideal internalization) and their own bodies (e.g., high body shame, low body appreciation, low body compassion) may heighten their concern about their child's weight and desire to control their child's food consumption within a weight-focused culture. Thus, researchers could examine the extent mothers' weight bias and body image may (a) alter their concern about their child's weight and their use of restrictive feeding, as well as (b) moderate these variables. We also did not explore how child behavioral and emotional difficulties, both general (e.g., poor emotion regulation, impulsivity, oppositional-defiant behaviors) and food-related (e.g., eating in the absence of hunger, food neophobia, avoidant/restrictive food intake disorder) may be related to mothers' use of restrictive feeding, especially when concerned about child weight. Certain health conditions and diseases in children, such as food allergies and sensitivities, Type I diabetes, and reflux also would likely prompt maternal restrictive feeding, even if children are perceived as being underweight. Researchers could examine these behavioral and emotional difficulties and health conditions as predictors and covariates of restrictive feeding.
Third, the present study is limited in terms of its sample. Most mothers in our sample are Caucasian, well educated, married, and located within a large urban city in the U.S., making it possible that our findings may not generalize well to mothers who do not fit these categories. Future research should evaluate associations between maternal intuitive eating, concerns for child weight, and restrictive feeding behaviors within more diverse samples.
Despite these limitations, the present study's findings have important implications for the development of both children's and mothers' self-regulated eating (i.e., eating according to internal hunger and satiety cues) and well-being. Interventions designed to prevent and treat child eating problems (e.g., overweight, obesity, eating in the absence of hunger) by promoting child self-regulated eating and discouraging restrictive feeding, such as those proposed by Satter (2005), Miller et al. (2012), Boutelle et al. (2014), and Eneli et al. (in press), may want to incorporate an intuitive eating component for mothers early on in the intervention. Mothers who attend such interventions tend to be highly concerned about their child's weight (Eneli et al., in press). It is precisely these mothers who are more likely to engage in restrictive feeding if they score low on eating for physical reasons and trusting in their own internal hunger and satiety cues, as the present study has found. Rather, mothers who eat primarily for physical reasons and trust their internal hunger and satiety cues are more likely to allow their child to self-regulate his or her eating (Eneli, Tylka, Watowicz, & Lumeng, 2015).
Fortunately, intuitive eating appears to be teachable and facilitates mothers' trust in their physical hunger and satiety cues, eating in concert with these cues, and modeling these skills for their child (Schaefer & Magnuson, 2014; Tribole & Resch, 2012). Intuitive eating programs have revealed positive effects post-intervention, such as adult women's increased recognition, trust, and use of internal hunger and satiety cues to guide eating, as well as benefits to their physical and psychological well-being, such as lower levels of: total cholesterol, low-density lipoprotein cholesterol, triglycerides, systolic blood pressure, disinhibited eating, body dissatisfaction, drive for thinness, poor interceptive awareness, and depression (Bacon et al., 2002, 2005; Bush et al., 2014). Consequently, the present study's findings provide a rationale for examining whether the integration of an intuitive eating component into interventions focused on child self-regulation has an incremental benefit to mothers' intervention adherence, reduced restrictive feeding, and physical and psychological well-being, as well as improvement in the child's self-regulated eating.
Highlights.
Maternal concern about child weight was positively related to restrictive feeding.
Aspects of maternal intuitive eating moderated this relationship.
This relationship was nonsignificant for mothers high in eating for physical reasons.
This relationship was nonsignificant for mothers high in trust in hunger and satiety cues.
This relationship was strong for mothers low in these intuitive eating aspects.
Acknowledgments
Role of funding source: Funding for this study was supported by the National Institute of Diabetes, Digestive, and Kidney Disease (PAE-09-223) to Ihuoma U. Eneli (PI) and the National Center for Research Resources (UL1RR025755) to Ihuoma U. Eneli (PI). These sources did not have a role in the study design, collection, data analysis, interpretation of the findings, writing of the article, or the decision to submit the paper for publication.
Footnotes
Ethnicity was dummy coded 1 = Caucasian and African American, 0 = other, as there were differences in restrictive feeding between these classifications, t(178) = 3.05, p = .003. Mean restrictive feeding scores were 2.90 (SD = 0.62) for Caucasian and African American mothers and 3.34 (SD = 0.52) for other ethnicities (primarily Asian American mothers). Caucasian and African American mothers did not differ from one another in terms of their restrictive feeding scores, p = .850, thus they were combined.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Julie C. Lumeng, Email: jlumeng@umich.edu.
Ihuoma U. Eneli, Email: Ihuoma.Eneli@nationwidechildrens.org.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park: Sage; 1991. [Google Scholar]
- Augustus-Horvath CL, Tylka TL. The acceptance model of intuitive eating: A comparison of women in emerging adulthood, early adulthood, and middle adulthood. Journal of Counseling Psychology. 2011;58:110–125. doi: 10.1037/a0022129. [DOI] [PubMed] [Google Scholar]
- Bacon L, Keim NL, Van Loan MD, Derricote M, Gale B, Kazaks A, Stern JS. Evaluating a ‘non-diet’ wellness intervention for improvement of metabolic fitness, psychological well-being and eating and activity behaviors. International Journal of Obesity. 2002;26:854–865. doi: 10.1038/sj.ijo.0802012. [DOI] [PubMed] [Google Scholar]
- Bacon L, Stern JS, Van Loan MD, Keim NL. Size acceptance and intuitive eating improve health for obese, female chronic dieters. Journal of the American Dietetic Association. 2005;105:929–936. doi: 10.1016/j.jada.2005.03.011. [DOI] [PubMed] [Google Scholar]
- Barry CL, Jarlenski M, Grob R, Schlesinger M, Gollust SE. News media framing of childhood obesity in the United States from 2000 to 2009. Pediatrics. 2011;128:132–145. doi: 10.1542/peds.2010-3924. [DOI] [PubMed] [Google Scholar]
- Birch LL, Fisher JO. Mothers' child-feeding practices influence daughters' eating and weight. American Journal of Clinical Nutrition. 2000;71:1054–1061. doi: 10.1093/ajcn/71.5.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch LL, Fisher JO, Davison KK. Learning to overeat: Maternal use of restrictive feeding practices promotes girls' eating in the absence of hunger. American Journal of Clinical Nutrition. 2003;78:215–220. doi: 10.1093/ajcn/78.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: A measure of parental attitudes, beliefs, and practices about child feeding and obesity proneness. Appetite. 2001;36:201–210. doi: 10.1006/appe.2001.0398. [DOI] [PubMed] [Google Scholar]
- Birch LL, McPhee L, Shoba BC, Steinberg L, Krehbiel R. “Clean up your plate”: Effects of child feeding practices on the conditioning of meal size. Learning and Motivation. 1987;18:301–317. doi: 10.1016/0023-9690(87)90017-8. [DOI] [Google Scholar]
- Boutelle KN, Zucker N, Peterson CB, Rydell S, Carlson J, Harnack LJ. An intervention based on Schachter's externality theory for overweight children: The regulation of cues pilot. Journal of Pediatric Psychology. 2014;39:405–417. doi: 10.1093/jpepsy/jst142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown A, Lee M. Maternal child-feeding style during the weaning period: Association with infant weight and maternal eating style. Eating Behaviors. 2011;12:108–111. doi: 10.1016/j.eatbeh.2011.01.002. [DOI] [PubMed] [Google Scholar]
- Brown KA, Ogden J, Vögele C, Gibson EL. The role of parental control practices in explaining children's diet and BMI. Appetite. 2008;50:252–259. doi: 10.1016/j.appet.2007.07.010. [DOI] [PubMed] [Google Scholar]
- Bush HE, Rossy L, Mintz LB, Schopp L. Eat for life: A work site feasibility study of a novel mindfulness-based intuitive eating intervention. American Journal of Health Promotion. 2014;28:380–388. doi: 10.4278/ajhp.120404-QUAN-186. [DOI] [PubMed] [Google Scholar]
- Campbell K, Andrianopoulous N, Hesketh K, Ball K, Crawford D, Brennan L, et al. Timperio A. Parental use of restrictive feeding practices and child BMI z-score. A 3-year prospective cohort study. Appetite. 2010;55:84–88. doi: 10.1016/j.appet.2010.04.006. [DOI] [PubMed] [Google Scholar]
- Cardel M, Willig AL, Dulin-Keita A, Casazza K, Beasley M, Fernández JR. Parental feeding practices and socioeconomic status are associated with child adiposity in a multi-ethnic sample of children. Appetite. 2012;58:347–353. doi: 10.1016/j.appet.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Calculating BMI. 2010 Retrieved from http://collab.nlm.nih.gov/webcastsandvideos/drew/teachingresources/obesity/F3BMI.pdf.
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Crawford D, Timperio A, Telford A, Salmon J. Parental concerns about childhood obesity and the strategies employed to prevent unhealthy weight gain in children. Public Health Nutrition. 2005;9:889–895. doi: 10.1017/PHN2005917. [DOI] [PubMed] [Google Scholar]
- den Hoed M, Westerterp-Plantenga MS, Bouwman FG, Mariman ECM, Westerterp KR. Postprandial responses in hunger and satiety are associated with the rs9939609 single nucleotide polymorphism in FTO. American Journal of Clinical Nutrition. 2009;90:1426–1432. doi: 10.3945/ajcn.2009.28053. [DOI] [PubMed] [Google Scholar]
- Denny KN, Loth K, Eisenberg ME, Neumark-Sztainer D. Intuitive eating in young adults. Who is doing it, and how is it related to disordered eating behaviors? Appetite. 2013;60:13–19. doi: 10.1016/j.appet.2012.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dockendorff SA, Petrie TA, Greenleaf CA, Martin S. Intuitive Eating Scale: An examination among early adolescents. Journal of Counseling Psychology. 2012;59:604–611. doi: 10.1037/a0029962. [DOI] [PubMed] [Google Scholar]
- Eneli IU, Crum PA, Tylka TL. The trust model: A different feeding paradigm for managing childhood obesity. Obesity. 2008;16:2197–2204. doi: 10.1038/oby.2008.378. [DOI] [PubMed] [Google Scholar]
- Eneli IU, Tylka TL, Watowicz RP, Hummel J, Ritter J, Lumeng JC. Targeting feeding and eating behaviors: Development of the Feeding Dynamic Intervention (FDI) for caregivers of 2- to 5-year-old children. Journal of Obesity. doi: 10.1155/2015/964249. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eneli IU, Tylka TL, Watowicz RP, Lumeng JC. Maternal and child roles in the feeding relationship: What are mothers doing? Clinical Pediatrics. 2015;54:179–182. doi: 10.1177/0009922814529363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- English PJ, Ghatei MA, Malik IA, Bloom SR, Wilding JPH. Food fails to suppress ghrelin levels in obese humans. Journal of Clinical Endocrinology & Metabolism. 2002;87:2984–2987. doi: 10.1210/jcem.87.6.8738. [DOI] [PubMed] [Google Scholar]
- Etelson D, Brand DA, Patrick PA, Shirali A. Childhood obesity: Do parents recognize this health risk? Obesity Research. 2003;11:1362–1368. doi: 10.1038/oby.2003.184. [DOI] [PubMed] [Google Scholar]
- Fisher JO, Birch LL. Restricting access to palatable foods affects children's behavioral response, food selection, and intake. American Journal of Clinical Nutrition. 1999;69:1264–1272. doi: 10.1093/ajcn/69.6.1264. [DOI] [PubMed] [Google Scholar]
- Fisher JO, Birch LL. Eating in the absence of hunger and overweight in girls from 5 to 7 y of age. American Journal of Clinical Nutrition. 2002;76:226–231. doi: 10.1093/ajcn/76.1.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis LA, Birch LL. Maternal influences on daughters' restrained eating behavior. Health Psychology. 2005;24:548–554. doi: 10.1037/0278-6133.24.6.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis LA, Hofer SM, Birch LL. Predictors of maternal child-feeding style: Maternal and child characteristics. Appetite. 2001;37:231–243. doi: 10.1006/appe.2001.0427. [DOI] [PubMed] [Google Scholar]
- Hawks S, Madanat H, Hawks J, Harris A. The relationship between intuitive eating and health indicators among college women. American Journal of Health Education. 2005;36:331–336. doi: 10.1080/19325937.2005.10608206. [DOI] [Google Scholar]
- Herbert BM, Blechert J, Hautzinger M, Matthias E, Herbert C. Intuitive eating is associated with interoceptive sensitivity. Effects on body mass index. Appetite. 2013;70:22–30. doi: 10.1016/j.appet.2013.06.082. [DOI] [PubMed] [Google Scholar]
- Hurley KM, Black MM, Papas MA, Caulfield LE. Maternal symptoms of stress, depression, and anxiety are related to nonresponsive feeding styles in a statewide sample of WIC participants. Journal of Nutrition. 2008;138:799–805. doi: 10.1093/jn/138.4.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SL. Preschoolers' self-regulation of energy intake. Pediatrics. 2000;106:1429–1435. doi: 10.1542/peds.106.6.1429. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation/Harvard School of Public Health. September/October 2001 health news index. Menlo Park, CA: Kaiser Family Foundation; 2001. [Google Scholar]
- Kline RB. Principles and practices of structural equation modeling. 3rd. New York: Guilford Press; 2010. [Google Scholar]
- Loth KA, MacLehose RF, Fulkerson JA, Crow S, Neumark-Sztainer D. Eat this, not that! Parental demographic correlates of food-related parenting practices. Appetite. 2013;60:140–147. doi: 10.1016/j.appet.2012.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden CEL, Leong SL, Gray A, Horwath CC. Eating in response to hunger and satiety signals is related to BMI in a nationwide sample of 1601 mid-age New Zealand women. Public Health Nutrition. 2012;15:2272–2279. doi: 10.1017/S1368980012000882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May AL, Donohue M, Scanlon KS, Sherry B, Dalenius K, Faulkner P, Birch LL. Child-feeding strategies are associated with maternal concern about children becoming overweight, but not children's weight status. Journal of the American Dietetic Association. 2007;107:1167–1174. doi: 10.1016/j.jada.2007.04.009. [DOI] [PubMed] [Google Scholar]
- McClelland GH, Judd CM. Statistical difficulties of detecting interactions and moderator effects. Psychological Bulletin. 1993;114:376–390. doi: 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- Miller AL, Horodynski MA, Herb HEB, Peterson KE, Contreras D, Kaciroti N, et al. Lumeng JC. Enhancing self-regulation as a strategy for obesity prevention in Head Start preschoolers: The growing healthy study. BMC Public Health. 2012;121040 doi: 10.1186/1471-2458-12-1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden J, Cordey P, Cutler L, Thomas H. Parental restriction and children's diets. The chocolate coin and Easter egg experiments. Appetite. 2013;61:36–44. doi: 10.1016/j.appet.2012.10.021. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. The social life of health information. 2014 Retrieved from http://www.pewresearch.org/fact-tank/2014/01/15/the-social-life-of-health-information/
- Rodgers RF, Paxton SJ, Massey R, Campbell KJ, Wertheim EH, Skouteris H, Gibbons K. Maternal feeding practices predict weight gain and obesogenic eating behaviors in young children: A prospective study. International Journal of Behavioral Nutrition and Physical Activity. 2013;10 doi: 10.1186/1479-5868-10-24. Available at http://www.ijbnpa.org/content/10/1/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rollins BY, Loken E, Savage JS, Birch LL. Effects of restriction on children's intake differ by child temperament, food reinforcement, and parent's chronic use of restriction. Appetite. 2014;73:31–39. doi: 10.1016/j.appet.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saguy AC, Almeling R. Fat in the fire? Science, the news media, and the “obesity epidemic”. Sociological Forum. 2008;23:53–83. doi: 10.1111/j.1573-7861.2007.00046.x. [DOI] [Google Scholar]
- Satter E. Your child's weight: Helping without harming. Madison, WI: Kelcy Press; 2005. [Google Scholar]
- Schaefer JT, Magnuson AB. A review of interventions that promote eating by internal cues. Journal of the Academy of Nutrition and Dietetics. 2014;114:734–760. doi: 10.1016/j.jand.2013.12.024. [DOI] [PubMed] [Google Scholar]
- Smith T, Hawks SR. Intuitive eating, diet composition, and the meaning of food in healthy weight promotion. American Journal of Health Education. 2006;37:130–136. [Google Scholar]
- Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition, and hunger. Journal of Psychometric Research. 1985;29:71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- Tribole E, Resch E. Intuitive eating: A revolutionary program that works. 3rd. New York: St. Martin's Press; 2012. [Google Scholar]
- Tylka TL. Development and psychometric evaluation of a measure of intuitive eating. Journal of Counseling Psychology. 2006;53:226–240. doi: 10.1037/0022-0167.53.2.226. [DOI] [Google Scholar]
- Tylka TL, Eneli IU, Kroon Van Diest AM, Lumeng JC. Which adaptive maternal eating behaviors predict child feeding practices? An examination with mothers of 2- to 5-year-old children. Eating Behaviors. 2013;14:57–63. doi: 10.1016/j.eatbeh.2012.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tylka TL, Kroon Van Diest AM. The Intuitive Eating Scale-2: Item refinement and psychometric evaluation with college women and men. Journal of Counseling Psychology. 2013;60:137–153. doi: 10.1037/a0030893. [DOI] [PubMed] [Google Scholar]
- Tylka TL, Wilcox JA. Are intuitive eating and eating disorder symptomatology opposite poles of the same construct? Journal of Counseling Psychology. 2006;53:474–485. doi: 10.1037/0022-0167.53.4.474. [DOI] [Google Scholar]
- Van Dyke N, Drinkwater EJ. Relationships between intuitive eating and health indicators: Literature review. Public Health Nutrition. 2013;17:1757–1766. doi: 10.1017/S1368980013002139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb JB, Butler-Ajibade P, Robinson SA. Considering an affect regulation framework for examining the association between body dissatisfaction and positive body image in Black older adolescent females: Does body mass index matter? Body Image. 2014;11:426–437. doi: 10.1016/j.bodyim.2014.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webber L, Hill C, Cooke L, Carnell S, Wardle J. Associations between child weight and maternal feeding styles are mediated by maternal perceptions and concerns. European Journal of Clinical Nutrition. 2010;64:259–265. doi: 10.1038/ejcn.2009.146. [DOI] [PMC free article] [PubMed] [Google Scholar]


