Abstract
Newborns with hypoplastic left heart syndrome (HLHS) and other single right ventricular variants require substantial healthcare resources. Weekend acute care has been associated with worse outcomes and increased resource use in other populations, but has not been studied in single ventricle patients. Single Ventricle Reconstruction trial subjects were classified by whether or not they had a weekend admission and by day of the week of Norwood procedure. The primary outcome was hospital length of stay (LOS); secondary outcomes included transplant-free survival, intensive care unit (ICU) LOS and days of mechanical ventilation. Student’s t-test with log transformation and the Wilcoxon rank sum test were used to analyze associations. Admission day was categorized for 533/549 subjects (13% weekend). The day of the Norwood was Thursday/Friday in 39%. There was no difference in median hospital LOS, transplant-free survival, ICU LOS or days ventilated for weekend vs. non-weekend admissions. Day of Norwood procedure was not associated with a difference in hospital LOS, transplant-free survival, ICU LOS or days ventilated. Prenatally diagnosed infants born on the weekend had lower mean birth weight, younger gestational age, and were more likely to be intubated but did not have a difference in measured outcomes. In conclusion, in this cohort of single right ventricle patients, neither weekend admission, nor end-of-the-week Norwood procedure was associated with increased use of hospital resources or poorer outcomes. We speculate that the complex postoperative course following the Norwood procedure outweighs any impact that day of admission or operation may have on these outcomes.
Keywords: Hypoplastic Left Heart Syndrome, Norwood procedure, Outcomes
Introduction
Infants with hypoplastic left heart syndrome (HLHS) and other single right ventricle (RV) anomalies typically undergo the Norwood procedure within the first several days of life. Though highly resource intensive (1), the factors that impact resource utilization after the Norwood procedure the most remain unknown. The day of the week when the highest acuity of care is provided may have a significant impact on resource utilization. The “weekend effect” has been associated with increased resource utilization in children < 18 years undergoing cardiac surgery (2) and poorer clinical outcomes in adults admitted on the weekend for several clinical indications (3–7). The weekend effect may be modifiable, and previously has been improved with high-intensity staffing. (8) (9) Determining whether weekend admission or day of surgery impacts clinical outcomes or resource utilization may be valuable for planning perinatal management, surgical timing and modifying health care delivery systems. Using the cohort enrolled in the Single Ventricle Reconstruction (SVR) trial, we sought to determine if weekend admission and/or day of surgery in neonates undergoing the Norwood procedure was associated with measures of increased postoperative resource utilization or worse clinical outcomes.
Methods
We performed a secondary analysis of SVR trial data, the details of which have previously been published. (10,11) Briefly, patients with a diagnosis of HLHS or other single RV anomalies and a planned Norwood procedure were randomized to receive a modified Blalock Taussig Shunt (MBTS) or right ventricular-to-pulmonary artery shunt (RVPAS) to compare the incidence of death or transplant. Age at admission to the surgical center and presence of a prenatal diagnosis were recorded. The main outcomes from the SVR trial that were utilized for this analysis were in-hospital mortality, heart transplant status, hospital length of stay (LOS), ICU LOS, days to surgery, and days of mechanical ventilation.
A primary exposure status of “weekend admission” (Saturday or Sunday) or “weekday admission” (Monday through Friday) to the surgical center was assigned for each subject. Date of admission was unavailable in the SVR trial database. Therefore, for the prenatally diagnosed subjects, date of birth was used for classification of date of admission. For subjects who were postnatally diagnosed, the date of diagnosis at the surgical center was considered the date of admission. This was determined from age at diagnosis, which was rounded to the nearest full day to determine group assignment. For those <12 hours of age at diagnosis, we assumed that the day of diagnosis was the day of birth. Subjects whose weekend versus weekday designation was unclear based on the above algorithm were excluded from the analysis.
The day of week of the Norwood procedure was also analyzed as an exposure. Subjects were divided into those who underwent the Norwood procedure on Thursday or Friday (end of the week) vs. those who underwent the Norwood procedure on Monday through Wednesday. This classification was chosen since the highest acuity care, primarily the first few days postoperatively, would have occurred largely on the weekend in the “end of the week” Norwood group. Only one Norwood procedure occurred on the weekend, and that subject was excluded from this portion of the analysis.
Surrogates for resource utilization previously described in the literature (12–15), were selected as outcomes. The primary outcome for this analysis was hospital LOS for the Norwood hospitalization. Secondary outcomes included ICU LOS, number of hospital days prior to surgery after diagnosis, number of days mechanically ventilated during hospitalization, and a composite outcome of death or heart transplant prior to discharge from the Norwood hospitalization. Due to the variable effect of death or transplant on length of stay, those who died or were transplanted prior to discharge were excluded from the LOS analyses.
Based on previously reported predictive models for these outcomes from the SVR trial (10), we compared subjects with respect to the variables identified as associated with the outcomes of interest to assess comparability of the groups. Baseline characteristics and risk factors are listed in Table 1 and 2. To deal with any potential interaction between prenatal versus postnatal diagnosis and day of admission, a subgroup analysis restricted to the prenatally diagnosed group was performed.
Table 1.
Baseline Characteristics of weekend vs. weekday groups and beginning of the week vs. end of the week Norwood
| Variable | Weekend admission (N=71) | Weekday admission (N=462) | p value | Mon–Wed Norwood (N=336) | Thu–Fri Norwood (N=212) | p value |
|---|---|---|---|---|---|---|
| Male | 46 (65%) | 285 (62%) | 0.7 | 211 (63%) | 128 (60%) | 0.6 |
| Prenatally diagnosed | 46 (65%) | 374 (81%) | 0.003 | 254 (76%) | 165 (78%) | 0.6 |
| Gestational age, weeks, mean ±SD | 37.9±2.0 | 38.2±1.5 | 0.2 | 38.2±1.6 | 38.1±1.6 | 0.3 |
| Birth weight, kg, mean±SD | 3.00±0.59 | 3.12±0.53 | 0.07 | 3.1±0.54 | 3.12±0.55 | 0.7 |
| Birth weight <2.5 kg | 15 (21%) | 59 (13%) | 0.07 | 46 (14%) | 30 (14%) | 0.9 |
| APGAR at 1 minute, median (IQR) | 8 (8,9) | 8 (8,9) | 0.9 | 8 (7,9) | 8 (8,9) | 0.5 |
| APGAR at 5 minutes, median (IQR) | 9 (8,9) | 9 (8,9) | 0.8 | 9 (8,9) | 9 (8,9) | 0.2 |
| Hypoplastic Left Heart Syndrome | 59 (83%) | 400 (87%) | 0.5 | 288 (86%) | 185 (87%) | 0.7 |
| Genetic syndrome | 4 (6%) | 19 (4%) | 0.04 | 15 (5%) | 11 (5%) | 0.9 |
| Unknown/no genetic evaluation | 31 (44%) | 140 (30%) | 107 (32%) | 69 (33%) | ||
| Non-syndromic abnormality | 9 (13%) | 92 (20%) | 65 (19%) | 40 (19%) | ||
| Unknown/no evaluation | 31 (44%) | 139 (30%) | 0.06 | 106 (32%) | 69 (33%) | >0.9 |
| Age at Norwood, days, median (IQR) | 5 (4,6) | 5 (3,7) | 5 (4,6) | 5 (3,7) | ||
| Center volume, per yr, median (IQR) | 21.5 (17.1,32.2) | 27.5 (17.1,32.2) | 27.5 (17.1,32.2) | 21.5 (17.1,32.2) | ||
| Center volume | 0.7 | 0.009 | ||||
| ≤15/yr | 11 (16%) | 82 (18%) | 0.4 | 61 (18%) | 32 (15%) | 0.9 |
| 16–20/yr | 19 (27%) | 86 (19%) | 0.4 | 61 (18%) | 48 (23%) | 0.6 |
| 21–30/yr | 23 (32%) | 144 (31%) | 108 (32%) | 38 (32%) | ||
| >30/yr | 18 (25%) | 150 (33%) | 106 (32%) | 34 (30%) | ||
| Surgeon Norwood volume, per yr median (IQR) | 12 (7.9,14.8) | 12.3 (6.9,13.6) | 12.0 (6.9, 13.3) | 12.6 (7.3,14.8) | ||
| Surgeon Norwood volume | ||||||
| ≤5/yr | 14 (20%) | 93 (20%) | 0.5 | 69 (21%) | 39 (18%) | 0.2 |
| 6–10/yr | 14 (20%) | 96 (21%) | >0.9 | 68 (20%) | 45 (21%) | 0.2 |
| 11–15/yr | 31 (44%) | 201 (44%) | 154 (46%) | 85 (40%) | ||
| >15/yr | 12 (17%) | 72 (16%) | 45 (13%) | 43 (20%) | ||
APGAR – Appearance, Pulse, Grimace, Activity, Respiration, IQR – interquartile range, kg – kilograms, yr - year
Table 2.
Analysis of risk factors for morbidity and mortality by exposure status.
| Variable | Weekend admission (N=71) | Weekday admission (N=462) | p value | Mon–Wed Norwood (N=336) | Thu–Fri Norwood (N=212) | p value |
|---|---|---|---|---|---|---|
| Preoperative highest lactate (mmol/L), median (IQR) | 3.2 (2.4,5.1) | 3.1 (2.5,4.2) | 0.1 | 3.1 (2.5,4.6) | 3.1 (2.4,4.3) | 0.2 |
| Preoperative intubation | 44 (62%) | 209 (45%) | 0.01 | 163 (49%) | 100 (47%) | 0.7 |
| Intubation due to apnea or transport | 13 (18%) | 84 (18%) | >0.9 | 63 (19%) | 38 (18%) | 0.8 |
| Intubation due to shock, respiratory failure, or metabolic acidosis | 26 (37%) | 86 (19%) | 0.001 | 72 (22%) | 45 (21%) | >0.9 |
| Preoperative intervention for atrial septum | 2 (3%) | 19 (4%) | >0.9 | 10 (3%) | 11 (5%) | 0.3 |
| Composite indicator for preoperative shock/arrest | 9 (13%) | 27 (6%) | 0.04 | 22 (7%) | 16 (8%) | 0.7 |
| Preoperative TR ≥2.5 mm | 10 (15%) | 52 (12%) | 0.5 | 40(12%) | 21 (10%) | 0.6 |
| ECMO used in OR | 3 (4%) | 32 (7%) | 0.6 | 18 (5%) | 17 (8%) | 0.2 |
| ECMO during Norwood hospitalization | 12 (17%) | 73 (16%) | 0.9 | 46 (14%) | 42 (20%) | 0.07 |
| Delayed sternal closure | 58 (84%) | 357 (78%) | 0.3 | 259 (78%) | 166 (79%) | 0.7 |
| Delayed sternal closure | 0.4 | 0.9 | ||||
| Yes, non-elective | 31 (45%) | 207 (45%) | 149 (45%) | 95 (46%) | ||
| Yes, elective | 27 (39%) | 150 (33%) | 110 (33%) | 71 (34%) | ||
| No, primary closure | 11 (16%) | 102 (22%) | 75 (23%) | 43 (21%) | ||
| Norwood perfusion type | 0.5 | 0.8 | ||||
| DHCA only | 34 (49%) | 255 (56%) | 184 (55%) | 111 (53%) | ||
| RCP and DHCA ≤10 min | 20 (29%) | 106 (23%) | 78 (24%) | 52 (25%) | ||
| RCP and DHCA ≥10 min | 15 (22%) | 98 (21%) | 70 (21%) | 48 (23%) | ||
| Total support time (min), mean±SD | 144±50 | 144±55 | >0.9 | 144±50 | 145±60 | 0.8 |
| Total DHCA time (min), mean±SD | 28±22 | 32±23 | 0.1 | 31±21 | 32±27 | 0.5 |
| DHCA time ≤45 min | 54 (76%) | 345 (75%) | 0.9 | 248 (74%) | 163 (77%) | 0.5 |
| Total RCP time (min), mean±SD | 27±29 | 23±29 | 0.3 | 23±30 | 24±28 | 0.8 |
| Infection prior to discharge | 30 (43%) | 193 (42%) | 0.9 | 147 (44%) | 89 (42%) | 0.7 |
| Number of other surgical procedures during Norwood hospitalization, median (IQR) | 1 (1,2) | 1 (1,2) | 0.6 | 1 (1,2) | 1 (1,3) | 0.3 |
DHCA – deep hypothermic cardiac arrest, ECMO – extracorporeal membrane oxygenation, IQR – interquartile range, min – minutes, OR – operating room, RCP – regional cerebral perfusion, SD – standard deviation, TR – tricuspid regurgitation,
The distributions of patient characteristics by day of week and day of Norwood groups were compared using a Fisher exact test for categorical variables, the Wilcoxon rank sum test for continuous skewed variables, and Student’s t-test for other continuous variables. The association between day of week and day of Norwood group and death/transplant prior to Norwood discharge was examined with a Fisher exact test. The associations between day of week and day of Norwood group and length of stay, number of days prior to surgery, and total number of days ventilated were analyzed using Student’s t-test of the log-transformed measure or a Wilcoxon rank sum test. Multivariable linear and logistic regression was also used to evaluate the weekend vs. weekday effect controlling for other known risk factors for post-Norwood outcomes such as birth weight, presence of a genetic syndrome, number of pre-Norwood surgeries, pre-Norwood intubation for shock, pre-Norwood tricuspid regurgitation, and center single ventricle patient volume (10). A two-sided p-value of 0.05 was considered significant. Analyses were conducted using SAS version 9.3 (Statistical Analysis System Corp., Cary, NC).
Results
Of the 549 subjects in the SVR trial who underwent Norwood, admission day could be categorized in 533 (97%). Weekend admission occurred in 71 (13%) and weekday admission in 462 (87%). There was a higher proportion of prenatally diagnosed patients admitted on weekdays (Table 1). Subjects admitted on the weekend were more likely to be intubated preoperatively, and more likely to be intubated for shock, respiratory failure or metabolic acidosis as opposed to electively prior to transport and to have had pre-operative shock or cardiac arrest (Table 2). In the prenatally diagnosed group, those admitted on the weekend were more likely to have a birth weight <2.5 kg and be of an earlier gestational age (Table 3). Similar to the overall cohort, they were more likely to be intubated due to shock, respiratory failure, or metabolic acidosis (Table 3).
Table 3.
Baseline characteristics and risk factors of those who were prenatally diagnosed (N=420).
| Weekend admission (N=46) | Weekday admission (N=374) | p value | |
|---|---|---|---|
| Male | 33 (72%) | 226 (60%) | 0.2 |
| Gestational age, (weeks), mean ±SD | 37.5±2.1 | 38.1±1.5 | 0.04 |
| Birth weight, (kg), mean±SD | 2.91±0.65 | 3.11±0.53 | <0.05 |
| Birth weight <2.5 kg | 13 (28%) | 52 (14%) | 0.02 |
| APGAR at 1 minute, median (IQR) | 8 (7,8) | 8(8,9) | 0.4 |
| APGAR at 5 minutes, median (IQR) | 9 (8,9) | 9(8,9) | 0.3 |
| Hypoplastic Left Heart Syndrome | 41 (89%) | 326 (87%) | 0.8 |
| Genetic syndrome present | 2 (4%) | 15 (4%) | 0.2 |
| Unknown/no genetic evaluation | 20 (44%) | 115 (31%) | |
| Non-syndromic abnormality present | 5 (11%) | 79 (21%) | 0.1 |
| Unknown/no evaluation | 20 (44%) | 114 (31%) | |
| Age at Norwood, (days), median (IQR) | 4 (3,5) | 5 (3,6) | 0.7 |
| Center volume, per year, median (IQR) | 27.5 (18.9, 49.6) | 27.5 (17.1, 32.2) | 0.6 |
| Center volume | 0.2 | ||
| ≤15/yr | 4 (9%) | 60 (16%) | |
| 16–20/yr | 13 (28%) | 66 (18%) | |
| 21–30/yr | 12 (26%) | 122 (32.6%) | |
| >30/yr | 17 (37%) | 126 (34%) | |
| Surgeon volume, per year, median, IQR | 12.3 (8.2,13.6) | 12.6 (7.1,13.6) | 0.6 |
| Surgeon Norwood volume | 0.5 | ||
| ≤5/yr | 5 (11%) | 68 (18%) | |
| 6–10/yr | 13 (28%) | 78 (21%) | |
| 11–15/yr | 22 (48%) | 167 (45%) | |
| >15/yr | 6 (13%) | 61 (16%) | |
| Risk factors | |||
| Preoperative highest lactate, (mmol/L), median (IQR) | 3.1 (2.3,4.4) | 3.1 (2.4,4.0) | 0.7 |
| Preoperative intubation | 25 (54%) | 147 (39%) | 0.06 |
| Intubation due to apnea or transport | 8 (17%) | 64 (17%) | >0.9 |
| Intubation due to shock, respiratory failure, or metabolic acidosis | 13 (28%) | 55 (15%) | 0.03 |
| Preoperative intervention for atrial septum | 1 (2%) | 15 (4%) | >0.9 |
| Composite indicator for preoperative shock/arrest | 1 (2%) | 15 (4%) | 0.5 |
| Preoperative TR ≥2.5 mm | 4 (9%) | 35 (10%) | >0.9 |
| ECMO used in OR | 1 (2%) | 26 (7%) | 0.3 |
| ECMO during Norwood hospitalization | 7 (15%) | 62 (17%) | >0.9 |
| Delayed sternal closure | 34 (76%) | 290 (78%) | 0.7 |
| Delayed sternal closure | 0.6 | ||
| Yes, non-elective | 16 (36%) | 161 (43%) | |
| No, primary closure | 11 (24%) | 82 (22%) | |
| Norwood perfusion type | 0.9 | ||
| DHCA only | 24 (53%) | 207 (56%) | |
| RCP and DHCA≤10 min | 11 (24%) | 83 (23%) | |
| RCP and DHCA≥10min | 10 (22%) | 80 (21%) | |
| Total support time, (min), mean±SD | 135±40 | 143±53 | 0.2 |
| Total DHCA time, (min), mean±SD | 28±19 | 32±23 | 0.2 |
| DHCA time ≤ 45 min | 35 (76%) | 277 (74%) | 0.9 |
| Total RCP time, (min), mean±SD | 25±29 | 23±29 | 0.7 |
| Infection prior to discharge | 16 (35%) | 150 (40%) | 0.5 |
| Number of other surgical procedures during Norwood hospitalization, median (IQR) | 1 (1,2) | 1 (1,2) | 0.9 |
APGAR – Appearance, Pulse, Grimace, Activity, Respiration, DHCA – deep hypothermic cardiac arrest, ECMO – extracorporeal membrane oxygenation, IQR – interquartile range, kg – kilograms, min – minutes, OR – operating room, RCP – regional cerebral perfusion, SD – standard deviation, Yr – year
In transplant-free survivors, hospital LOS was similar between the weekend and weekday groups (Figure 1). Likewise, there was no difference in ICU LOS, days ventilated, or number of days prior to surgery (Table 4). There were 93 (17%) deaths and transplants prior to Norwood discharge with no difference in the incidence of death or transplant between the weekend and weekday groups. There were 4 (25%) deaths or transplants occurring in the group (n=16) that could not be assigned a day of admission. There was a small group of patients who died prior to Norwood procedure with no difference between weekend or weekday groups (3% vs. 3%, p>0.9). When prenatally and postnatally diagnosed subgroups were analyzed separately, the results remained similar, with the exception that postnatally diagnosed infants admitted on the weekend had fewer days in the hospital prior to surgery than those admitted on the weekday. (Table 4). When controlling for other known risk factors, there remained no significant difference according to weekend vs. weekday admission for our study outcomes (covariate adjusted p=0.07–0.47).
Figure 1.
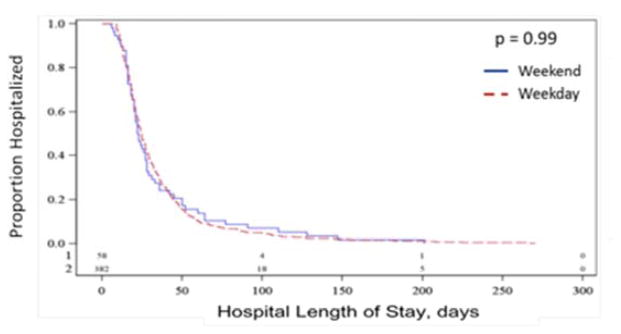
Distribution of Time to Discharge by Day of the week Diagnosis group using Kaplan-Meier Analysis.
Table 4.
Primary and secondary outcomes by exposure status and status of prenatal diagnosis
| Weekend admission (N=71) | Weekday admission (N=462) | p value | Mon–Wed Norwood (N=336) | Thu–Fri Norwood (N=212) | p value | |
|---|---|---|---|---|---|---|
| Hospital LOS, days, median (IQR)* | 23 (16,36) | 24 (17,40) | 0.7 | 25 (17,42) | 24 (18,36) | 0.7 |
| ICU LOS, days, median (IQR)* | 14 (8,21) | 14 (10,26) | 0.5 | 14 (9,26) | 14 (10,23) | 0.7 |
| Days ventilated, median (IQR)* | 7 (5,11) | 6 (5,11) | 0.3 | 6 (5,11) | 7 (5,11) | 0.8 |
| Days prior to surgery, median (IQR) | 4 (3,5) | 5 (3,7) | 0.3 | 5 (4,7) | 3 (3,6) | <0.001 |
| Death/transplant prior to discharge | 13 (18%) | 80 (17%) | 0.9 | 54 (16%) | 43 (20%) | 0.2 |
| Prenatally diagnosed | n=46 | n=374 | n=254 | n=165 | ||
| Hospital LOS, days, median (IQR)* | 21 (16,33) | 24 (16,40) | 0.3 | 25 (16,43) | 22 (16,36) | 0.2 |
| ICU LOS, days, median (IQR)* | 14 (8,21) | 14 (10,25) | 0.5 | 14 (9,27) | 14 (10,21) | 0.8 |
| Days ventilated, median (IQR)* | 7 (4,11) | 7 (5,11) | >0.9 | 7 (5,11) | 7 (5,11) | 0.6 |
| Days prior to surgery, median (IQR) | 4 (3,5) | 5 (3,6) | 0.7 | 5(4,7) | 3 (2,5) | <0.001 |
| Death/transplant prior to discharge | 7 (15%) | 66 (18%) | 0.8 | 39 (15%) | 34 (20%) | 0.2 |
| Postnatally diagnosed | n=25 | n=88 | n=82 | n=47 | ||
| Hospital LOS, days, median (IQR)* | 27 (20,50) | 27 (18,41) | 0.6 | 24 (17,42) | 29 (23,50) | 0.06 |
| ICU LOS, days, median (IQR)* | 14 (8,28) | 14 (9,27) | >0.9 | 15 (9,24) | 17 (10,29) | 0.2 |
| Days ventilated, median (IQR)* | 9 (5,23) | 6 (4,10) | 0.08 | 6 (4,10) | 7 (5,15) | 0.1 |
| Days prior to surgery, median (IQR) | 5 (4,5) | 6 (4,7) | 0.03 | 5(4,7) | 5 (4,8) | 0.4 |
| Death/transplant prior to discharge | 6 (24%) | 14 (16%) | 0.4 | 15 (18%) | 9 (19%) | >0.9 |
ICU – intensive care unit, IQR – interquartile range, LOS – length of stay
patients who died or were transplanted were excluded from length of stay and days ventilated analyses
Of the 548 undergoing the Norwood procedure on a Monday through Friday, the procedure occurred at the beginning of the week in 61%, and the end of the week in 39%. The baseline characteristics and risk factors for postoperative morbidity and mortality were similar for the beginning of the week and end of the week Norwood groups (Table 1, Table 2). There was no difference in hospital LOS, ICU LOS, or days ventilated by day of the week of the Norwood procedure (Table 4). However, patients who had their Norwood procedure on Thursday and Friday had waited fewer days prior to surgery. There was no difference in the death/transplant rate between the beginning of the week or the end of the week Norwood groups (16% vs. 20%, p=0.2). In subgroup analyses, the results were similar to the overall cohort for subjects with prenatal and postnatal diagnosis with respect to day of Norwood procedure (Table 4).
Discussion
In this study, contrary to our hypotheses, we found that day of admission or day of surgery for neonates undergoing the Norwood procedure was not associated with clinical outcomes or surrogate markers of resource utilization in these infants. These findings are notable considering that a greater proportion of infants admitted on weekends had preoperative risk factors for postoperative morbidity such as lower birth weight and younger gestational age, and were more frequently intubated preoperatively for shock, respiratory failure or metabolic acidosis, but this did not translate into differences in the postoperative outcomes we examined.
In contrast to previous studies in pediatric heart surgery and adult admissions for stroke and myocardial infarction (2–8), weekend admission did not appear to have an impact on the outcomes or resource use. Previous studies demonstrating a mortality difference in weekend vs. weekday admissions in adults primarily evaluated patients with acute medical concerns such as stroke, myocardial infarction and conditions requiring surgical ICU admission. (3,4,6) While our population did have an increased incidence of morbidity when admitted on the weekend, the overall percentage of our population with preoperative instability was relatively low. It may be that neonates with HLHS and other related single right ventricle lesions, particularly those who are prenatally diagnosed, are clinically stable at the time of birth and remain so prior to surgery, despite the significant complexity of their disease. Connor et al reported that weekend admission was an independent predictor of increased resource utilization, as measured by charge data, in children admitted for congenital heart surgery. Their population, however, was significantly more heterogeneous than the cohort in our study, and included a wide range of diagnoses and ages. Additionally, while they adjusted for several risk factors, including emergent admission, they were not able to determine prenatal diagnosis status in the administrative data used. The percentage of patients prenatally diagnosed in the SVR cohort was high. This may have led to a relative stability of our patients preoperatively that was not present in the population described by Connor et al.(2) There are other diagnoses where preoperative instability may be more likely, including infants born with transposition of the great arteries and a restrictive foramen ovale, or those with congenital heart disease and intrauterine hydrops.(16) It is possible that patients presenting with demonstrated hemodynamic instability or other organ dysfunction may have different outcomes depending on when they are admitted to a pediatric cardiac center.
We also evaluated timing of Norwood procedure, to determine if infants who were operated on at the end of the week and received more of their early acute postoperative care on the weekend had greater resource use or perioperative morbidity compared with those operated on earlier in the week. Our analysis did not show a difference in outcome by procedure day. It is possible that those hospitals that perform Norwood procedures and participated in the SVR trial have higher volume units and are more likely to have experienced staff even on the weekends, particularly during the early postoperative period for unstable infants; care may be as good when provided on the weekend as it is during the weekdays at these institutions. In addition, the prolonged and complicated hospital course that is typical after a Norwood procedure may dilute any impact of day of admission or day of Norwood procedure. It is possible that in other cohorts of patients with congenital heart disease with shorter, less complicated hospital stays, the effect of day of admission and day of procedure on outcome and resource utilization would be significant. While there was no impact of day of surgery on the measured outcomes in this analysis, it is possible that other outcome metrics reflecting the quality of early acute perioperative care such as long-term neurodevelopmental outcome may be associated with day of surgery.
We found that patients with a weekend admission had a higher prevalence of preoperative risk factors for postoperative morbidity including preoperative intubation and shock. While these risk factors did not translate into differences in our measured outcomes, including hospital LOS or mortality/transplant in these infants, they may have a long-term impact on other patient outcomes not measured in this study. The difference in gestational age between the weekend and weekday admission groups was slight. However, as lower gestational age has been found to be an independent risk factor for poorer neurodevelopmental outcome in neonates undergoing congenital heart surgery, this finding may represent increased clinical risk in this group. (10)
In the prenatal diagnosis group, weekend admissions were more likely to have a birth weight <2.5 kg, which is a known risk factor for morbidity and mortality during Norwood hospitalization (10), but again this did not translate into a difference in measured outcomes. Birth weight is also an independent risk factor for lower Psychomotor Development Index scores at 1 year of age. (17) The lower birth weight may possibly reflect a more urgent or emergent delivery, which resulted in a weekend admission in this subgroup. Additionally, while both birth weight and gestational age may pose long-term risk, these may or may not be modifiable depending on the circumstances surrounding the decisions to deliver these infants on the weekend.
The SVR trial was limited to 15 participating centers, performing ≥5 Norwood procedures annually, and therefore, these conclusions may not be generalizable to centers with smaller case volumes. Admission day was assumed for 20 patients, which may have resulted in some misclassification. Three percent of the study sample (16 patients) could not be assigned a day of admission, but this was unlikely to bias our results as this was a small percentage of the overall sample and should not be systematically related to the outcomes measured. Limited access to obstetric records limits our analysis of the decision-making surrounding the timing of delivery for these high-risk infants. In addition, we were unable to determine the presence of weekend provider availability, as this information was not known for each center.
In this cohort of single right ventricle patients, neither weekend admission, nor end-of-the-week Norwood procedure was associated with increased use of hospital resources or poorer outcomes. We speculate that the complex postoperative course following the Norwood procedure outweighs any impact that day of admission or operation may have on these outcomes.
Acknowledgments
Supported by U01 grants from the National Heart, Lung, and Blood Institute (HL068269, HL068270, HL068279, HL068281, HL068285, HL068292, HL068290, HL068288, HL085057, HL109781, and HL109737). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NHLBI or NIH.
Footnotes
We have no relevant relationships with industry to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.MMWR Morbidity and Mortality Weekly Reports. Centers for Disease Control and Prevention; 2007. Hospital stays, hospital charges, and in-hospital deaths among infants with selected birth defects: United States, 2003. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5602a1.htm. [PubMed] [Google Scholar]
- 2.Connor JA, Gauvreau K, Jenkins KJ. Factors associated with increased resource utilization for congenital heart disease. Pediatrics. 2005;116:689–695. doi: 10.1542/peds.2004-2071. [DOI] [PubMed] [Google Scholar]
- 3.Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med. 2007;356:1099–1109. doi: 10.1056/NEJMoa063355. [DOI] [PubMed] [Google Scholar]
- 4.Saposnik G, Baibergenova A, Bayer N, Hachinski V. Weekends: a dangerous time for having a stroke? Stroke. 2007;38:1211–1215. doi: 10.1161/01.STR.0000259622.78616.ea. [DOI] [PubMed] [Google Scholar]
- 5.McKinney JS, Deng Y, Kasner SE, Kostis JB. Comprehensive stroke centers overcome the weekend versus weekday gap in stroke treatment and mortality. Stroke. 2011;42:2403–2409. doi: 10.1161/STROKEAHA.110.612317. [DOI] [PubMed] [Google Scholar]
- 6.Ensminger SA, Morales IJ, Peters SG, Keegan MT, Finkielman JD, Lymp JF, Afessa B. The Hospital Mortality of Patients Admitted to the ICU on Weekends. Chest. 2004;126:1292–1298. doi: 10.1378/chest.126.4.1292. [DOI] [PubMed] [Google Scholar]
- 7.Bell CM, Redelmeier DA. Mortality Among Patients Admitted to Hospitals on Weekends as Compared With Weekdays. N Engl J Med. 2001;1:663–668. doi: 10.1056/NEJMsa003376. [DOI] [PubMed] [Google Scholar]
- 8.Jauss M, Schutz HJ, Tanislav C, Misselwitz B, Rosenow F. Effect of daytime, weekday and year of admission on outcome in acute ischaemic stroke patients treated with thrombolytic therapy. Eur J Neurol. 2010;17:555–561. doi: 10.1111/j.1468-1331.2009.02845.x. [DOI] [PubMed] [Google Scholar]
- 9.Hixson ED, Davis S, Morris S, Harrison AM. Do weekends or evenings matter in a pediatric intensive care unit? Pediatr Crit Care Med. 2005;6:523–530. doi: 10.1097/01.pcc.0000165564.01639.cb. [DOI] [PubMed] [Google Scholar]
- 10.Tabbutt S, Ghanayem N, Ravishankar C, Sleeper LA, Cooper DS, Frank DU, Lu M, Pizarro C, Frommelt P, Goldberg CS, Graham EM, Krawczeski CD, Lai WW, Lewis A, Kirsh JA, Mahoney L, Ohye RG, Simsic J, Lodge AJ, Spurrier E, Stylianou M, Laussen P. Risk factors for hospital morbidity and mortality after the Norwood procedure: A report from the Pediatric Heart Network Single Ventricle Reconstruction trial. J Thorac Cardiovasc Surg. 2012;144:882–895. doi: 10.1016/j.jtcvs.2012.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ohye RG, Sleeper LA, Mahony L, Newburger JW, Pearson GD, Lu M, Goldberg CS, Tabbutt S, Frommelt PC, Ghanayem NS, Laussen PC, Rhodes JF, Lewis AB, Mital S, Ravishankar C, Williams IA, Dunbar-Masterson C, Atz AM, Colan S, Minich LL, Pizarro C, Kanter KR, Jaggers J, Jacobs JP, Krawczeski CD, Pike N, McCrindle BW, Virzi L, Gaynor JW. Comparison of shunt types in the Norwood procedure for single-ventricle lesions. N Engl J Med. 2010;362:1980–1992. doi: 10.1056/NEJMoa0912461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Amula V, Ellsworth GL, Bratton SL, Arrington CB, Witte MK. Heterotaxy syndrome: impact of ventricular morphology on resource utilization. Pediatr Cardiol. 2014;35:38–46. doi: 10.1007/s00246-013-0736-y. [DOI] [PubMed] [Google Scholar]
- 13.Knott EM, Gasior AC, Ostlie DJ, Holcomb GW, 3rd, St Peter SD. Decreased resource utilization since initiation of institutional clinical pathway for care of children with perforated appendicitis. J Pediatr Surg. 2013;48:1395–1398. doi: 10.1016/j.jpedsurg.2013.03.044. [DOI] [PubMed] [Google Scholar]
- 14.McNab A, Burns B, Bhullar I, Chesire D, Kerwin A. A prehospital shock index for trauma correlates with measures of hospital resource use and mortality. Surgery. 2012;152:473–476. doi: 10.1016/j.surg.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 15.Baker L, Emil S, Baird R. A comparison of techniques for laparoscopic gastrostomy placement in children. J Surg Res. 2013;184:392–396. doi: 10.1016/j.jss.2013.05.067. [DOI] [PubMed] [Google Scholar]
- 16.Donofrio MT, Levy RJ, Schuette JJ, Skurow-Todd K, Sten MB, Stallings C, Pike JI, Krishnan A, Ratnayaka K, Sinha P, duPlessis AJ, Downing DS, Fries MI, Berger JT. Specialized delivery room planning for fetuses with critical congenital heart disease. Am J Cardiol. 2013;111:737–747. doi: 10.1016/j.amjcard.2012.11.029. [DOI] [PubMed] [Google Scholar]
- 17.Newburger JW, Sleeper LA, Bellinger DC, Goldberg CS, Tabbutt S, Lu M, Mussatto KA, Williams IA, Gustafson KE, Mital S, Pike N, Sood E, Mahle WT, Cooper DS, Dunbar-Masterson C, Krawczeski CD, Lews A, Menon SC, Pemberton VL, Ravishankar C, Atz TW, Ohye RG, Gaynor JW. Early developmental outcome in children with hypoplastic left heart syndrome and related anomalies: the single ventricle reconstruction trial. Circulation. 2012;125:2081–2091. doi: 10.1161/CIRCULATIONAHA.111.064113. [DOI] [PMC free article] [PubMed] [Google Scholar]


