Abstract
The Children’s Eating Behaviour Questionnaire (CEBQ; Wardle, Guthrie, Sanderson, & Rapoport, 2001) is a widely used measure of child eating behaviors. Yet, only one study has examined the factor structure of the CEBQ among low-income children. In the current study, we examined the internal consistency, factor structure, and validity of the CEBQ among 1002 low-income preschool-age children recruited from Head Start locations in the United States. Confirmatory Factor Analysis indicated the CEBQ evidenced a reasonable fit to the data. Results also indicate that CEBQ subscales demonstrate good internal reliability (α’s ≥ .70) and validity, with 7 of the 8 subscales associated with children’s BMI z-scores in the expected directions. Equivalent factor loadings and indicator means across White and Black non-Hispanic participants were found, supporting measurement invariance between these two groups. In sum, our study supports the factor structure of the CEBQ among low-income preschool-aged children in the United States.
Keywords: Low-income preschoolers, Child eating behavior, Measurement, Confirmatory Factor Analysis
Introduction
The Children’s Eating Behaviour Questionnaire (CEBQ; Wardle et al., 2001) is one of the most widely used measures of eating behaviors in children. The CEBQ, which has been used in children age 2 years and older, originally yielded 8 subscales: Food Responsiveness, Enjoyment of Food, Emotional Overeating, Desire to Drink, Satiety Responsiveness, Slowness in Eating, Emotional Undereating, and Food Fussiness (Wardle et al., 2001). As described by Wardle and others (Carnell & Wardle, 2007; Wardle et al., 2001), the Food Responsiveness subscale consists of items assessing appetite and an inclination towards appealing external food cues (i.e., external eating). The Enjoyment of Food subscale also reflects a child’s appetite and interest in eating. The Emotional Eating subscales tap into over- and under- eating in response to negative emotions (e.g., anger, sadness, anxiety, and boredom). A need for frequent beverage or drink consumption is assessed by Desire to Drink items. The Satiety Responsiveness subscale consists of items indicating that a child attends to internal cues of fullness and stops eating based on such perceived fullness. The Slowness in Eating (sometimes combined with the Satiety Responsiveness subscale) consists of items that assess a child’s speed of eating (e.g., taking a longer time to finish food or consume food). Finally, the Food Fussiness subscale consists of items reflecting a child being selective about foods eaten (e.g., picky eating or difficulty in pleasing a child with foods).
The CEBQ was originally developed and validated in the United Kingdom among White primarily middle-income samples (Ashcroft, Semmler, Carnell, van Jaarsveld, & Wardle, 2007; Carnell & Wardle, 2007; Wardle, et al., 2001; Webber, Hill, Saxton, Van Jaarsveld, & Wardle, 2009). In translated versions of the CEBQ in middle-income and/or well-educated samples in other Western and non-Western countries, the internal reliability and validity of the CEBQ subscales has also generally been supported (Mallan et al., 2013; Sleddens, Kremers, & Thijs, 2008; Svensson et al., 2011; Viana, Sinde, & Saxton, 2008). In three ethnically diverse samples in Australia (e.g., first-time mothers; immigrant Indian mothers; and immigrant Chinese mothers), Mallan and colleagues also found support for the factor structure and construct validity of the CEBQ. Yet, despite the prevalence of obesity in low-income children in the United States (US), only one study has examined the factor structure of the CEBQ in this population.
Sparks and Radnitz (2012) evaluated the factor structure of the CEBQ in a sample of 229 primary caregivers of children who were recruited from Head Start preschools. Sparks and Radnitz’s sample was unique in that most caregivers were Hispanic and Black. These authors conducted a Confirmatory Factor Analysis (CFA) on this sample and found that the original CEBQ factor structure did not replicate. The subscales of the CEBQ also did not significantly correlate with BMI, suggesting poor validity. Using exploratory factor analysis (EFA), these authors proposed an alternate 3-factor structure for the CEBQ to capture eating behaviors of racially/ethnically diverse samples of low-income children. This 3-factor structure consisted of 15 items contributing to the factors Disinhibition, Food Interest, and Undereating.
There are certain aspects of Sparks and Radnitz’s study that could account for the poor fit of the original CEBQ to the data. First, the CEBQ was administered to participants in both Spanish and English, although the article did not specify the number of participants given the CEBQ in each language. Second, the CFA was conducted on only 34 of the 35 original items. Finally, the study had a small sample size of participants with complete data (n= 179). Addressing these limitations and evaluating the alternate 3-factor model in a new sample is needed to determine the factor structure of the original (or modified) CEBQ in low-income United States preschool-age populations.
The current study examines the factor structure and validity of the original 8-factor, as well as the 3-factor, CEBQ in a large sample of 1002 low-income preschool-age children in the United States. We hypothesized that the original factor structure will replicate in this sample given prior robust support for the CEBQ across diverse samples (e.g., Mallan et al., 2013). Finally, we explored measurement invariance of the CEBQ in White and Black non-Hispanic participants (i.e., the two racial/ethnic groups largely represented in the sample).
Materials and method
Participants
Primary caregivers and children were recruited from Head Start locations in South Central Michigan for participation in two large studies. Head Start is a free, federally-funded preschool program for low-income children. The first study examined stress and eating in low-income preschoolers (“Appetite, Behavior, and Cortisol [ABC]” Cohort; see Lumeng et al., 2014 for more details) and the second was an intervention study, with the CEBQ administered pre- and post-intervention (“Growing Healthy” cohort, see Miller et al., 2012 for a detailed description). The first administration of the CEBQ and corresponding BMI were used in the analyses for all participants.
Recruitment procedures and exclusion and inclusion criteria were nearly identical between the two studies. Families were told about the studies during Head Start classroom open houses and through flyers sent home in children’s backpacks. For the ABC cohort, potential participants were told that the study was focused on “stress and eating in preschoolers.” In order to participate in this study, children must have been aged 3 to 4 years at study enrollment and all caregivers were required to have less than a 4-year college degree. Exclusion criteria included that the child had developmental disabilities that would preclude participation, food allergies or significant medical problems that affected appetite or eating, or was in foster care; or that the caregiver was non-English speaking. For the Growing Healthy cohort, potential participants were told that the study was about “children’s development, behavior and growth.” This study had the same inclusion and exclusion criteria as the first study with two exceptions. First, no restriction was placed on educational attainment for the primary caregiver. Although this was not an exclusion criterion, few participants had a Bachelor’s degree or higher (n=16; see description of participants in Results section) in the Growing Healthy cohort. Second, presence of child food allergies was not an exclusion criterion in the Growing Healthy cohort. Both studies were approved by the University of Michigan Medical School Institutional Review Board; written informed consent was provided by the child’s legal guardian (most often, the biological mother). Participants received compensation for participation.
Procedures
Identical procedures were followed in the administration of the Child Eating Behaviour Questionnaire (CEBQ) and assessment of child body mass index (BMI) in both studies (see below). Questionnaires were administered orally by trained research assistants to the primary caregivers, to account for low literacy within the participating population. The oral administration of the CEBQ took place in participants’ homes or, if preferred by the participant, in private rooms in community locations (e.g., local Head Starts or community health agencies). The research assistants did not provide any additional clarification on the items. Research assistants were trained to repeat the item verbatim if the study participant requested clarification. During the measure administration, participants could view the CEBQ response options on a reference card. Caregiver height and weight measurements were taken in the home or in a community location (e.g., Head Start). For child BMI, research assistants obtained height and weight measurements in Head Start classrooms.
Measures
Demographic characteristics
Several demographic variables were assessed at the time of the CEBQ administration. For the child, demographic characteristics obtained were: sex, age, and race/ethnicity. Caregiver characteristics that were assessed included: relationship of caregiver to child, caregiver level of education, and race/ethnicity of primary caregiver.
Children’s Eating Behaviour Questionnaire
As described in the Introduction, the CEBQ is a 35-item, caregiver-report questionnaire, consisting of the following subscales (with sample items): Food Responsiveness (“Given the choice, my child would eat most of the time”), Enjoyment of Food (“My child loves food”), Emotional Overeating (“My child eats more when worried”), Desire to Drink (“My child is always asking for a drink”), Satiety Responsiveness (“My child gets full before his/her meal is finished”), Slowness in Eating (“My child takes more than 30 minutes to finish a meal”), Emotional Undereating (“My child eats less when s/he is upset”), and Food Fussiness (“My child refuses new foods at first”). Participants rated child eating behaviors on a 5-point Likert scale ranging from never (1) to always (5), with higher ratings indicating greater endorsement of the given eating behavior. Subscales are calculated as means of the contributing items, with indicated items reverse-scored (see Figure 1 and Appendix for items). Items were identical to the original scale (Wardle et al., 2001) with the exceptions of (1) changing “favourite” to the American spelling “favorite” in item 28 and (2) changing “full up” to “full” in items 26 and 28.
Figure 1.
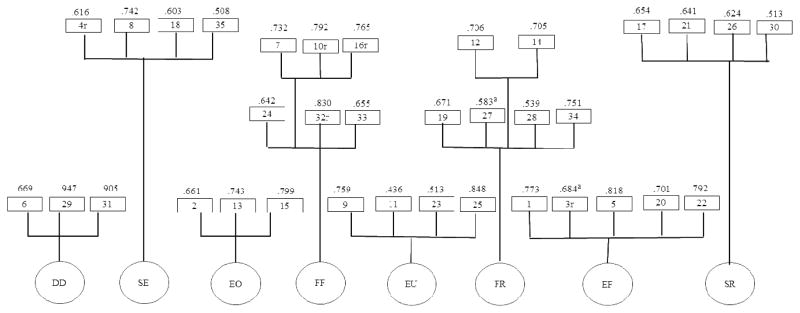
Confirmatory Factor Analysis of the CEBQ.
Note: Values within the boxes indicate CEBQ item number (reverse scored items are denoted with an “r”, see Appendix for items) and values above the boxes indicate standardized estimates. DD= Desire to Drink, SE= Slowness in Eating, EO= Emotional Overeating, FF=Food Fussiness, EU=Emotional Undereating, FR=Food Responsiveness, EF= Enjoyment of Food, and SR= Satiety Responsiveness. All loadings depicted are significant at p < .01. For clarity of the Figure, inter-correlations among factors are shown in Table 3. Model fit: RMSEA= .057, SRMR= .069
aIndicates modification from original CEBQ factor structure.
Anthropometry
Trained research assistants measured height and weight of children and caregivers. Participants were weighed using a Detecto Portable Scale Model # DR550 and height was measured using a Seca 217 portable stadiometer. Weight was measured twice. If the two measurements differed by more than 0.1 kg, the participant was weighed two more times. For the height measurement, the participant’s position and posture were checked, and height was measured twice. If measurements differed by more than 0.5 cm, two more measurements were taken. BMI was calculated and the child’s BMI z-score was derived using the age- and sex-specific US Centers for Disease Control and Prevention growth charts (Kuczmarski et al., 2000). Caregiver’s BMI’s were also calculated from measured heights and weights.
Statistical Analyses
First, descriptive statistics were conducted to ascertain the demographic characteristics of the sample and to calculate the means (SD) and range of scores of the original 8-factor CEBQ subscales. Second, confirmatory factor analyses (CFAs) were performed on the original 8-factor model and the recently proposed 3-factor model (Sparks & Radnitz, 2012) using maximum likelihood estimation via Mplus (Muthén & Muthén, 2012). We chose this estimation given that the frequency of missing data in our sample was small (e.g., the frequencies of missing data ranged from n=39 for “Eats less when angry” to n=53 for “Eats more when annoyed”). For each CFA, we set factor variance to 1 and allowed intercorrelations between each of the factors. We also kept the errors uncorrelated in these analyses and did not allow cross-factor loadings. Model fit was assessed using the root mean square error of approximation (RMSEA) and standardized root mean square residual (SRMR), as recommended by Hu and Bentler (1999). Cut-off values used to evaluate model fit included RMSEA less than or equal to 0.06 and SRMR less than or equal to 0.08 (Hu & Bentler, 1999). In addition to these fit indices, factor loadings, squared mean residuals, and modification indices were examined to establish model fit.
Cronbach alphas were calculated to examine the internal reliability of the 8-factor CEBQ subscales. Finally, bivariate correlations between each of the 8 CEBQ subscales and child BMI z-score were computed to establish validity.
Results
Sample Characteristics
A total of 1002 primary caregivers of pre-school children (M age= 4.05 years, SD= 0.53) participated. The vast majority of the primary caregivers (91.3%) were the biological mothers of the child participants (see Table 1 for demographic characteristics). Most of the caregivers reported low educational attainment (i.e., less than a Bachelor’s degree). Most primary caregivers were White (61.7%), with 24.6% identifying as Black and 7.7% as Hispanic. Sex distribution of the child participants was approximately equal (50.7% girls). Most children were either White (51.3%) or Black (24.5%); 11.5% of the children were of Hispanic ethnicity. Most children (62.1%) had a BMI z-score within the normal range (5th percentile < BMI < 85th percentile), with 18.6% and 17.0% falling within the overweight (85th percentile ≤ BMI < 95th percentile) and obese (BMI ≥ 95th percentile) weight status categories, respectively.
Table 1.
Demographic Characteristics of Participants (N=1002)
| Demographic variable | Mean (SD) or % (n) |
|---|---|
| Child age (years) | 4.05 (0.53) |
| Child BMI z-score | 0.67 (1.13) |
| Caregiver BMI | 31.83 (8.74) |
| Child sex (female) | 50.7% (507) |
|
| |
| Child race/ethnicity | |
| White, non-Hispanic | 51.3% (512) |
| Black, non-Hispanic | 24.5% (245) |
| Hispanic, any race | 11.5% (115) |
| Other, non-Hispanic | 12.6% (126) |
|
| |
| Caregiver race/ethnicity | |
| White, non-Hispanic | 61.7% (617) |
| Black, non-Hispanic | 24.6% (246) |
| Hispanic, any race | 7.7% (77) |
| Other, non-Hispanic | 6.0% (60) |
|
| |
| Caregiver education level | |
| Less than high school | 15.8% (156) |
| High school diploma or GED only | 71.5% (715) |
| 2-year college degree or higher | 12.9% (129) |
|
| |
| Relationship of caregiver to child | |
| Biological mother | 91.3% (915) |
| Not biological mother | 8.7% (87) |
|
| |
| Child weight status | |
| Underweight | 2.2% (22) |
| Normal | 62.1% (613) |
| Overweight | 18.6% (184) |
| Obese | 17.0% (168) |
Confirmatory factor analyses
A confirmatory factor analysis was conducted on the 8 factors of the original CEBQ: Food Responsiveness, Enjoyment of Food, Emotional Overeating, Desire to Drink, Satiety Responsiveness, Slowness in Eating, Emotional Undereating, and Food Fussiness. The 8 factor-model was found to have reasonable fit to the data (RMSEA= .062, SRMR= .076). The 35 items loaded on the respective 8 factors (above .40, p < .001; see Figure 1) and squared mean residuals were all above .1.
A review of the modification indices indicated that there were significant cross-loadings, potentially contributing to the less than ideal RMSEA. Item 27, “My child eats more when s/he has nothing else to do,” an Emotional Overeating subscale item, had a significant cross-loading on the Food Responsiveness factor. After allowing item 27 to load on to Food Responsiveness, its loading on Emotional Overeating was reduced to less than .30. As such, this item was specified to load only on Food Responsiveness. Theoretically, the fact that this item loads onto Food Responsiveness is consistent with the fact that this item reflects external eating, a type of eating behavior underlying food responsiveness (Wardle et al., 2001). The other cross-loading identified in the modification indices was item number 3 (reverse-scored), “My child has a big appetite,” which, in addition to its significant loading on the Satiety Responsiveness, also cross-loaded on the Enjoyment of Food factor (in an opposite direction). After allowing item 3 to load on to Enjoyment of Food, its loading on Satiety Responsiveness was reduced to less than .30. As such, this item was specified to load only on Enjoyment of Food. The rationale for making this modification is that a child with a “big appetite” may appear to enjoy food more. After making these modifications, model fit improved (RMSEA= .057, SRMR= .069), within recommended levels (Hu & Bentler, 1999).
In contrast to the 8-factor model, the 3-factor model demonstrated poor fit (RMSEA= .103, SRMR= 0.10). A review of the standardized regression weights indicated that 2 items had lower than ideal loadings on their respective factors (i.e., below .40). Attempts to improve model fit (e.g., removing items with less than ideal loadings, allowing cross-loadings) were unsuccessful.
Although the number of participants within each racial/ethnic groups was not large enough to examine measurement invariance across all racial/ethnic groups, we were able to explore the measurement invariance for two of the larger groups represented in the study: White non-Hispanic participants (n=617) and Black non-Hispanic participants (n=246). We conducted a multiple-group analysis using Mplus to test for measurement invariance between these two groups. Given the large sample size, we chose to examine change in CFI and RMSEA values to determine equivalence (Cheung and Rensvold, 2002; Timmons, 2010). These analyses showed support for equivalent factor loadings and indicator means across White and Black non-Hispanic participants, supporting measurement invariance between these two groups.
To examine the internal reliability and validity of the original 8 subscales, Cronbach alpha coefficients and zero-order correlations between the subscales and child BMI z-score were calculated (see Tables 2 and 3). Cronbach alphas for the subscales ranged from .70 to .87, indicating good internal reliability. Positive associations were found between child BMI z-score and Food Responsiveness, Enjoyment of Food, and Emotional Overeating subscales. The following subscales were negatively associated with child BMI z-score: Satiety Responsiveness, Slowness in Eating, Emotional Under-eating, and Food Fussiness. The Desire to Drink subscale was not associated with child BMI z-score (p = .58).
Table 2.
Descriptive statistics, internal reliability, and validity of CEBQ subscales
| Subscale | Mean (SD) | Cronbach alpha (# of items) | Correlation with Child BMI z-score |
|---|---|---|---|
| Food Responsiveness | 2.65 (0.94) | .80 (5) | .10** |
| Enjoyment of Food | 3.91 (0.80) | .86 (4) | .18** |
| Emotional Overeating | 1.80 (0.69) | .73 (4) | .08* |
| Desire to Drink | 3.85 (1.08) | .87 (3) | .02 |
| Satiety Responsiveness | 2.91 (0.70) | .72 (5) | −.18** |
| Slowness in Eating | 2.98 (0.77) | .70 (4) | −.16** |
| Emotional Undereating | 2.91 (0.91) | .73 (4) | −.08* |
| Food Fussiness | 2.78 (0.92) | .88 (6) | −.07* |
Note. Scales range from 1 (never) to 5 (always). N=1002.
p <.05,
p <.01
Table 3.
CEBQ Factor Intercorrelations
| Subscale | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Food Responsiveness | 1 | |||||||
| 2. Enjoyment of Food | .51** | 1 | ||||||
| 3. Emotional Overeating | .48** | .17** | 1 | |||||
| 4. Desire to Drink | .36** | .13** | .23** | 1 | ||||
| 5. Satiety Responsiveness | −.21** | −.54** | .01 | .10** | 1 | |||
| 6. Slowness in Eating | −.07* | −.32** | −.01 | .09** | .51** | 1 | ||
| 7. Emotional Undereating | .15** | −.06 | .30** | .13** | .26** | .28** | 1 | |
| 8. Food Fussiness | −.08* | −.47** | −.01 | .07* | .41** | .31** | .17** | 1 |
p <.01. N=1002.
Discussion
Valid measurement of low-income children’s eating behaviors is necessary for the development of effective interventions to target potentially obesity-promoting eating behaviors and prevent childhood obesity. The CEBQ is a widely used caregiver-report measure of a range of eating behaviors that are potentially obesity-promoting, as well as behaviors associated with undereating. In a sample of 1002 low-income primary caregivers of preschool children attending Head Start, we found that the CEBQ evidenced a reasonable fit to the data based on the CFA results. Subscales of the CEBQ demonstrated good internal reliability (α’s ≥ .70) and validity, based on the significant correlations between 7 of the 8 subscales and children’s BMI z-scores, in the expected directions. The magnitude of these correlations was comparable to others (Mallan et al., 2013). In sum, our study supports the factor structure and validity of the CEBQ among low-income preschool-aged children in the United States.
It is important to discuss the aspects of the CEBQ factor structure that differed from the original 8-factor model. First, item 27, “My child eats more when s/he has nothing else to do,” had loadings on the Emotional Overeating and Food Responsiveness subscales. Although this item is typically considered an Emotional Overeating item, Wardle et al. (2001) also originally found that this item clustered with other Food Responsiveness items in the CEBQ development paper. Their rationale for placing this item with other Emotional Overeating items was that it allowed for better comparability with the Emotional Eating subscale on a frequently-used measure of adult eating behavior, the Dutch Eating Behaviour Questionnaire (Van Strien, Frijters, Bergers, & Defares, 1986; cited in Wardle et al., 2001). Recent research suggests, however, that eating when bored is considered to be different from emotional eating behaviors by low-income parents (Hayman, Lee, Miller, & Lumeng, 2014), and a behavior that is more commonly endorsed than other emotional eating behaviors (Hayman et al., 2014; Koball, Meers, Storfer-Isser, Domoff, & Musher-Eizenman, 2012). Indeed, the Emotional Overeating subscale had the lowest mean of the CEBQ subscales in the current study and in Wardle et al. (2001). Furthermore, this scale was missing the most data (though small, i.e., 5% or less) of the CEBQ scales, suggesting that mothers were not endorsing these items or were unable to determine if their children ate more or less when feeling certain emotions. Given the stigma associated with reporting emotional eating (e.g., Hayman et al., 2014), and given that eating when bored may reflect an eating behavior distinct from other types of emotional eating (e.g., Koball et al., 2012), this type of eating behavior warrants further investigation in children.
An unexpected finding was the lack of association between Desire to Drink and child BMI z-score. Greater consumption of soft drink or other sugar-sweetened beverages is associated with higher child BMI (Haycraft, Farrow, Meyer, Powell, & Blissett, 2011) and a positive association between mean scores on the Desire to Drink subscale and child BMI has been found previously (Webber et al., 2009). One possible explanation for the lack of association in the current study is that the sample mean for Desire to Drink was higher in the current study than sample means in the Webber et al. (2009) study and others (e.g., Mallan et al., 2013; Sleddens et al., 2008; Svensson et al., 2011; Wardle et al., 2001). Approximately 86% of our sample had mean scores at or above the mid-point of the scale, suggesting that children’s requests for and consumption of beverages are more frequently endorsed in our sample. This limited range of scores may account for the lack of association between Desire to Drink and child BMI z-score.
Our findings differ from those of Sparks and Radnitz (2012), the only other examination of the factor validity of the CEBQ in a low-income US sample. There are likely multiple reasons for why our findings diverge from those of this prior study. First, we excluded primary caregivers who were not English-speaking whereas Sparks and Radnitz offered measures in both English and Spanish. Another difference lies in the mode of administration. In our study, to account for lower educational attainment of participants, research assistants read the CEBQ items aloud to the primary caregivers. Additionally, our sample differed from their sample with regard to racial/ethnic diversity. Our sample consisted primarily of non-Hispanic White and Black primary caregivers whereas Sparks and Radnitz (2012)’s cohort was primarily Hispanic (57.2%). Although we found support for measurement invariance for White and Black non-Hispanic participants, the sample sizes of Hispanic and other racial/ethnic minority participants were too small to test measurement invariance for these groups. Thus, future research is recommended to investigate measurement invariance in low-income Hispanic populations.
Another limitation of the study is that our results may also be specific to oral administration of the CEBQ. It is possible that reading the items aloud to the participants reduced error in participant response, or that participants were more or less likely to endorse certain behaviors due to social desirability bias. This may be why emotional eating items were rarely endorsed. Given the rates of low educational attainment and possible lower literacy rates in economically disadvantaged samples, however, modification of the CEBQ administration in this manner may be helpful when working with this population.
Conclusions
Our study supports the original 8-factor structure of the CEBQ in a sample of low-income primary caregivers describing behaviors of their preschool-aged children. Several subscales of the measure demonstrate validity as expected with children’s BMI z-score. Because this is the first study to demonstrate support for the original factor structure of the CEBQ in low-income children in the United States, replication of this study and further examination of low-income mothers’ conceptualization of child eating behaviors, particularly emotional eating and eating when bored, is warranted.
Highlights.
The Children’s Eating Behaviour Questionnaire (CEBQ) is a commonly used measure.
The CEBQ has not been validated in low-income populations in the US.
Using CFA, we found support for the 8-factor CEBQ in low-income US preschoolers.
CEBQ subscales demonstrated good internal reliability (α’s ≥ .70).
Expected associations were found between CEBQ subscales and child BMI z-scores.
Acknowledgments
This material is based upon work that is supported by the National Institute of Food and Agriculture, U.S. Department of Agriculture, under award number 2010-04785. The study was also supported by the NIDDK 1RC1DK086376. Dr. Domoff’s work on this study was supported by NIDDK R01DK098983 and NICHD R01HD061356.
Appendix
| Number | Item content (My child…) |
|---|---|
| 1 | Loves food |
| 2 | Eats more when worried |
| 3 | Has a big appetite |
| 4 | Finishes his/her meal quickly |
| 5 | Is interested in food |
| 6 | Is always asking for a drink |
| 7 | Refuses new foods at first |
| 8 | Eats slowly |
| 9 | Eats less when angry |
| 10 | Enjoys tasting new foods |
| 11 | Eats less when s/he is tired |
| 12 | Is always asking for food |
| 13 | Eats more when annoyed |
| 14 | If allowed to, would eat too much |
| 15 | Eats more when anxious |
| 16 | Enjoys a wide variety of foods |
| 17 | Leaves food on his/her plate at the end of a meal |
| 18 | Takes more than 30 minutes to finish a meal |
| 19 | Given the choice, would eat most of the time |
| 20 | Looks forward to mealtimes |
| 21 | Gets full before his/her meal is finished |
| 22 | Enjoys eating |
| 23 | Eats more when s/he is happy |
| 24 | Is difficult to please with meals |
| 25 | Eats less when upset |
| 26 | Gets full easily |
| 27 | Eats more when s/he has nothing else to do |
| 28 | Even if full s/he finds room to eat his/her favorite food |
| 29 | If given the chance, would drink continuously throughout the day |
| 30 | Cannot eat a meal if s/he has had a snack just before |
| 31 | If given the chance, would always be having a drink |
| 32 | Is interested in tasting food s/he hasn’t tasted before |
| 33 | Decides that s/he doesn’t like a food, even without tasting it |
| 34 | If given the chance, would always have food in his/her mouth |
| 35 | Eats more and more slowly during the course of a meal |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ashcroft J, Semmler C, Carnell S, van Jaarsveld CHM, Wardle J. Continuity and stability of eating behaviour traits in children. Eur J Clin Nutr. 2007;62:985–990. doi: 10.1038/sj.ejcn.1602855. [DOI] [PubMed] [Google Scholar]
- Carnell S, Wardle J. Measuring behavioural susceptibility to obesity: Validation of the child eating behaviour questionnaire. Appetite. 2007;48:104–113. doi: 10.1016/j.appet.2006.07.075. [DOI] [PubMed] [Google Scholar]
- Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct equ modeling. 2002;9:233–255. [Google Scholar]
- Haycraft E, Farrow C, Meyer C, Powell F, Blissett J. Relationships between temperament and eating behaviours in young children. Appetite. 2011;56:689–692. doi: 10.1016/j.appet.2011.02.005. [DOI] [PubMed] [Google Scholar]
- Hayman LW, Jr, Lee HJ, Miller AL, Lumeng JC. Low-income women’s conceptualizations of emotional- and stress-eating. Appetite. 2014;83:269–276. doi: 10.1016/j.appet.2014.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct equ modeling. 1999;6:1–55. [Google Scholar]
- Koball AM, Meers MR, Storfer-Isser A, Domoff SE, Musher-Eizenman DR. Eating when bored: Revision of the Emotional Eating Scale with a focus on boredom. Health Psychol. 2012;31:521. doi: 10.1037/a0025893. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Johnson CL. CDC growth charts: United States. Advance data. 2000;314:1–27. [PubMed] [Google Scholar]
- Lumeng JC, Miller A, Peterson KE, Kaciroti N, Sturza J, Rosenblum K, Vazquez DM. Diurnal cortisol pattern, eating behaviors and overweight in low-income preschool-aged children. Appetite. 2014;73:65–72. doi: 10.1016/j.appet.2013.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallan KM, Liu WH, Mehta RJ, Daniels LA, Magarey A, Battistutta D. Maternal report of young children’s eating styles. Validation of the Children’s Eating Behaviour Questionnaire in three ethnically diverse Australian samples. Appetite. 2013;64:48–55. doi: 10.1016/j.appet.2013.01.003. [DOI] [PubMed] [Google Scholar]
- Miller AL, Horodynski MA, Herb HEB, Peterson KE, Contreras D, Kaciroti N, Lumeng JC. Enhancing self-regulation as a strategy for obesity prevention in Head Start preschoolers: the growing healthy study. BMC public health. 2012;12:1040. doi: 10.1186/1471-2458-12-1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- Sleddens EFC, Kremers SPJ, Thijs C. The Children’s Eating Behaviour Questionnaire: Factorial validity and association with Body Mass Index in Dutch children aged 6–7. Int J Behav Nutr Phy. 2008;5:49. doi: 10.1186/1479-5868-5-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparks MA, Radnitz CL. Confirmatory factor analysis of the Children’s Eating Behaviour Questionnaire in a low-income sample. Eat Behav. 2012;13:267–270. doi: 10.1016/j.eatbeh.2012.03.002. [DOI] [PubMed] [Google Scholar]
- Svensson V, Lundborg L, Cao Y, Nowicka P, Marcus C, Sobko T. Obesity related eating behaviour patterns in Swedish preschool children and association with age, gender, relative weight and parental weight--factorial validation of the Children’s Eating Behaviour Questionnaire. Int J Behav Nutr Phy. 2011;8:134. doi: 10.1186/1479-5868-8-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timmons AC. Establishing Factorial Invariance for Multiple-Group Confirmatory Factor Analysis. KUant Guide. 2010;22 [Google Scholar]
- Van Strien T, Frijters JER, Bergers G, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disorder. 1986;5:295–315. [Google Scholar]
- Viana V, Sinde S, Saxton JC. Children’s Eating Behaviour Questionnaire: associations with BMI in Portuguese children. Brit J Nutr. 2008;100:445–450. doi: 10.1017/S0007114508894391. [DOI] [PubMed] [Google Scholar]
- Wardle Jane, Guthrie Carol Ann, Sanderson Saskia, Rapoport Lorna. Development of the Children’s Eating Behaviour Questionnaire. J Child Psychol Psyc. 2001;42:963–970. doi: 10.1111/1469-7610.00792. [DOI] [PubMed] [Google Scholar]
- Webber L, Hill C, Saxton J, Van Jaarsveld CHM, Wardle J. Eating behaviour and weight in children. Int J Obes. 2009;33:21–28. doi: 10.1038/ijo.2008.219. [DOI] [PMC free article] [PubMed] [Google Scholar]


