A prospective controlled trial conducted in two intensive care units found that an electronic hand hygiene reminder system that provides real-time feedback on overall unit-wide hand hygiene performance can increase hand hygiene activity.
Keywords: electronic monitoring, hand hygiene, intensive care unit, prospective controlled trial
Abstract
Background. The use of electronic hand hygiene reminder systems has been proposed as an approach to improve hand hygiene compliance among healthcare workers, although information on efficacy is limited. We prospectively assessed whether hand hygiene activities among healthcare workers could be increased using an electronic hand hygiene monitoring and reminder system.
Methods. A prospective controlled clinical trial was conducted in 2 medical intensive care units (ICUs) at an academic medical center with comparable patient populations, healthcare staff, and physical layout. Hand hygiene activity was monitored concurrently in both ICUs, and the reminder system was installed in the test ICU. The reminder system was tested during 3 administered phases including: room entry/exit chimes, display of real-time hand hygiene activity, and a combination of the 2.
Results. In the test ICU, the mean number of hand hygiene events increased from 1538 per day at baseline to 1911 per day (24% increase) with the use of a combination of room entry/exit chimes, real-time displays of hand hygiene activity, and manager reports (P < .001); in addition, the ratio of hand hygiene to room entry/exit events also increased from 26.1% to 36.6% (40% increase, P < .001). The performance returned to baseline (1473 hand hygiene events per day) during the follow-up phase. There was no significant change in hand hygiene activity in the control ICU during the course of the trial.
Conclusions. In an ICU setting, an electronic hand hygiene reminder system that provided real-time feedback on overall unit-wide hand hygiene performance significantly increased hand hygiene activity.
Hand hygiene is considered one of the most fundamental approaches for the prevention of both the transmission of multidrug-resistant pathogens and healthcare-acquired infections [1–3]. The past 15 years has seen increased attention to this prevention practice, and health organizations spearheading education efforts include the Centers for Disease Control, the World Health Organization, and The Joint Commission [2–4]. However, despite these efforts, hand hygiene compliance among healthcare workers remains below desired levels. A 2010 systematic review of studies on hand hygiene compliance in hospitals found an overall median compliance rate of 40% [5].
A number of electronic systems and tools have been developed to monitor and promote hand hygiene activity including video monitoring systems, individual healthcare worker electronic devices, and the use of alcohol sensor technology [6–20]. The efficacy of these systems to change healthcare behavior remains uncertain because they have been primarily evaluated in either before-and-after analyses or small uncontrolled trials; both have limited ability to fully assess the efficacy of the systems [6, 7, 15, 16, 18–21]. We have evaluated the utility of an electronic hand hygiene reminder system at an academic tertiary care medical center to promote hand hygiene activity in a prospective controlled trial conducted in 2 comparable intensive care units (ICUs). The hand hygiene reminder system was an electronic network of hand hygiene dispensers and room entry-exit monitors linked to an electronic database with active event processing capability to allow for real-time feedback of aggregate hand hygiene activity within an ICU unit.
METHODS
Study Design and Setting
The trial was conducted at an academic medical center within 2 medical ICUs with comparable patient populations, healthcare staff, and physical layouts (Supplementary Figure 1). The only difference between the 2 ICUs was the number of beds: the test ICU, which conducted the intervention, contained 16 beds and the control ICU contained 15 beds. Patients were placed in the 2 units on the basis of bed availability and not in relation to acuity. The University of Massachusetts Medical School Institutional Review Board approved the trial.
Technology
Electronic hand hygiene alcohol/soap dispensers were installed at all locations used by staff for hand hygiene within each ICU. Doorway entry/exit monitors were installed at the entrance of all patient rooms within the test ICU (n = 16) and programmed to provide a soft chime reminder on room entry/exit. Doorway entry/exit monitors were also installed at the entrance of 5 of 15 patient rooms within the control ICU without the programmed chime reminder to allow for the comparison of room entry/exit events in comparable room locations between the 2 ICUs. Every dispenser and doorway entry/exit monitor communicated through a wireless network to an electronic database, which collected the date and time of each dispense and room entry/exit event. In addition, the use of active complex event processing allowed for a continuous real-time display of the proportion of the total number of hand hygiene dispenser activations and room entry/exit events for the preceding 60 minutes. The system updated the display approximately 5 to 10 seconds after each event (dispenser activation or room entry/exit event), but it did not capture the identity of the individual responsible for each event. The continuous real-time rate of hand hygiene activity was displayed as a “screensaver” on 5 centrally located computers in the test ICU (Figure 1).
Figure 1.
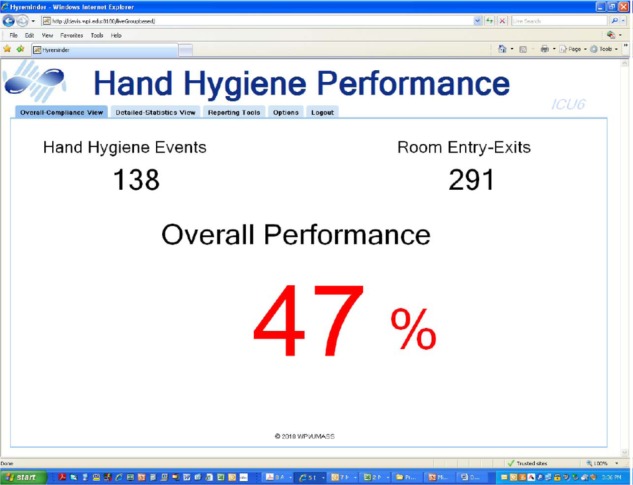
Real-time hand hygiene activity screensaver that was installed on 5 computer terminals within the test intensive care unit (ICU), which would be visible to the staff when computer terminals were not in use.
In addition, the active complex event-processing software concurrently monitored the performance of each device for potential data anomalies that could have arisen from device failure (such as equipment or individuals blocking the entry/exit monitors for sustained time periods that interfered with their function, devices losing battery power, or interruptions in network transmissions).
Intervention
The total number of hand hygiene events and total number of room entry/exits were collected in the test and control ICUs simultaneously. For the trial, several different reminder system phases were initiated sequentially in the test ICU that consisted of baseline (no reminder system) [6 weeks], doorway entry/exit chimes [5 weeks], both doorway entry/exit chimes and continuous real-time display of most recent hand hygiene compliance [5 weeks], continuous real-time display of most recent hand hygiene compliance [5 weeks], and a washout period (no reminder system) [4 weeks]. In addition, interim reports on hand hygiene compliance were provided to the test ICU staff detailing hand hygiene activity on an hourly, daily, weekly, and monthly basis. There were no interventions made at all in the control ICU except to notify the staff that a study was being done, and that necessitated the use of different hand hygiene dispensers as well as five door entry/exit monitors. The duration of the phases was based on general estimates of both the number of daily hand hygiene events in the test ICU as well as the amount of time necessary to observe a change in behavior potentially linked to alarm fatigue.
Outcomes
The primary study endpoints were as follows: (1) a comparison of the absolute number of hand hygiene events per day in the test ICU at baseline versus the audible room entry/exit chime, the use of the electronic performance display, and the combination of both reminders; (2) a comparison of the relative change in the number of hand hygiene events per day in the test ICU compared to the control ICU during each phase of the study; (3) a comparison of the ratio of hand hygiene events to room entry/exit events (HHEE ratio) in the test ICU at baseline versus each of the other phases of the study.
Secondary endpoints included the following: (1) a comparison of the absolute number of hand hygiene events per day in test ICU versus control ICU incorporating corrections for anomalous data (substituting average data for 10-minute time periods exceeding 6 standard deviations); (2) a comparison of both the absolute number of hand hygiene events per day and the HHEE ratio in the test ICU by shift (7:00 am–7:00 pm vs 7:00 pm–7:00 am).
Statistical Analysis
We used (1) both comparisons of the mean number of hand hygiene events per day and the mean HHEE ratio per day as well as (2) an interrupted time series analysis to estimate changes in hand hygiene compliance throughout the study period. The unit of time for this analysis was days. Linear regression models were parameterized with coefficients for phase, a continuous elapsed time from beginning of each phase, and dichotomous indicators of before versus after phase change. The Dickey-Fuller test allowed us to reject the unit-root null hypothesis and accept the alternative hypothesis that the response was generated by a stationary process (P < .001). The Breush-Godfrey and Durbin-Watson tests were used to test for autocorrelation. Statistical significance was defined as P < .05. SAS version 9.3 (SAS Institute, Inc., Cary, NC) was used for all analyses.
RESULTS
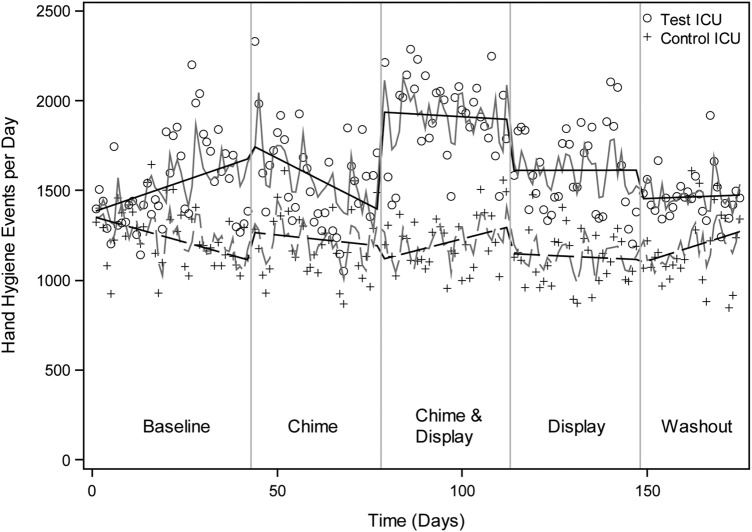
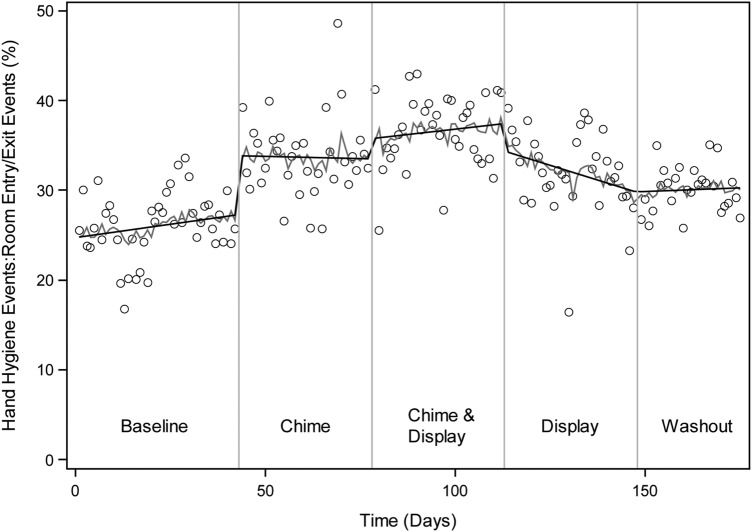
The mean bed occupancy rate during each phase of the trial remained over 92% in both ICUs, and there was no overall statistical difference in mean bed occupancy between the units during the trial, with an average occupancy rate of 94% in the test ICU and 95% in the control ICU (P = .642) (Supplementary Table 1). During the trial, there were 277 434 hand hygiene events in the test ICU and 205 202 events in the control ICU. The mean number of hand hygiene events per day and the mean HHEE ratio per day in each phase of the trial are shown in Table 1. The interrupted time series analysis showed that during the first intervention phase (the door entry/exit chime) in the test ICU, there was an initial increase in the number of hand hygiene events per day, but there was a statistically significant decay in hand hygiene activity during this phase (P = .014), and there was no overall improvement in the number of hand hygiene events (Figure 2). In contrast, the use of entry/exit chimes and real-time computer monitor feedback resulted in a 24% increase in the mean number of hand hygiene events per day compared to baseline (P < .001), and the time series analysis showed little decay in hand hygiene activity over the duration of this phase (P = .149). At the start of the third intervention phase, the number of events decreased with use of the real-time computer monitor feedback alone compared to the end of the dual reminder phase (P = .131); there was little decay in hand hygiene activity during the phase (P = .899). The number of hand hygiene events per day returned to baseline during the washout phase. In addition to the hand hygiene events per day analysis, the HHEE ratio analysis showed a significant increase during all 3 intervention phases compared to baseline in the test ICU (Figure 3). The use of entry/exit chimes and real-time computer monitor feedback resulted in a 40% increase in the mean HHEE ratio compared to baseline. A comparison of the mean number of hand hygiene events per day and the HHEE ratio between intervention phases was also conducted (Supplementary Table 2). Consistent with the baseline comparisons, both the mean number of hand hygiene events and the HHEE ratio were significantly greater with the use of both the entry/exit chimes and computer monitor feedback compared to all other intervention phases.
Table 1.
The Mean Number of Hand Hygiene Dispenser Events per Day in the Test and Control ICUs, and the HHEE Ratio in the Test ICU Over the Course of the Trial
| Phase | Number of Hand Hygiene Dispenser Events per Day (Mean [SD]) |
HHEE Ratio (Mean [SD]) |
||||
|---|---|---|---|---|---|---|
| Test ICU | P Value vs Baseline | Control ICU | P Value vs Baseline | Test ICU | P Value vs Baseline | |
| Baseline | 1538 (248) | – | 1246 (165) | – | 26.1% (3.7%) | – |
| Chime | 1569 (270) | .598 | 1205 (186) | .467 | 33.7% (4.5%) | <.0001 |
| Chime/Display | 1911 (237) | <.001 | 1218 (152) | .617 | 36.6% (4.1%) | <.0001 |
| Display | 1611 (238) | .196 | 1129 (149) | .542 | 32.0% (4.6%) | <.0001 |
| Washout | 1473 (131) | .214 | 1188 (208) | .188 | 30.1% (2.6%) | <.0001 |
Abbreviations: HHEE ratio, ratio of hand hygiene to room entry/exit events; ICU, intensive care unit; SD, standard deviation.
Figure 2.
Interrupted time series analysis of the daily number of hand hygiene events in the test intensive care unit (ICU) compared with the control ICU during baseline, chime, chime/display, display, and washout trial phases. o, the number of hand hygiene events on individual days in the test ICU; +, the number of hand hygiene events on individual days in the control ICU.
Figure 3.
Interrupted time series analysis of the hand hygiene event to room entry/exit event (HHEE) ratio in the test intensive care unit (ICU) during baseline, chime, chime/display, display and washout trial phases. o, the ratio of hand hygiene events to room entry/exit events on individual days.
A comparison of the total number of room entry/exit events for the 5 matching rooms with entry/exit monitors in the 2 ICUs showed variations in the total number of events between intervention phases; overall, there were slightly more entry/exit events in the matched rooms in the control ICU than the test ICU (Supplementary Table 3). In contrast, a comparison of hand hygiene events per day between the 2 ICUs showed that there was a consistent increase in hand hygiene activity in the test ICU during the 3 intervention phases, whereas the control ICU remained constant over time (Table 1 and Figure 2).
In a secondary analysis, we observed a small number of presumed anomalous events related to technological factors, which impacted less than 1% of the observations. To take these into account, we adjusted our hand hygiene activity for technological glitches; however, anomalous events did not influence the observed effects of the hand hygiene reminder system.
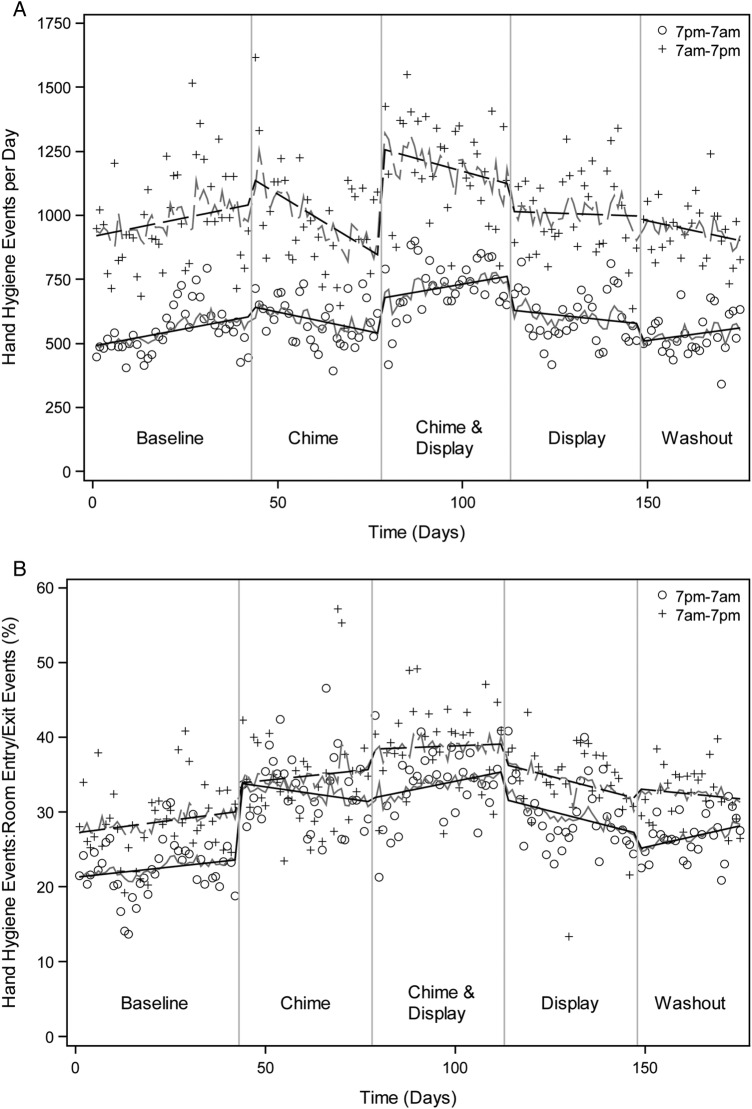
Analysis of the mean number of hand hygiene events by shift showed that in all phases of the trial, the number of events was statistically higher in the day shift (baseline <0.0001; chime <0.0001; chime/display <0.0001; display <0.0001; washout <0.0001) (Figure 4A). In addition, the HHEE ratio was higher in the day shift during most phases of the trial (baseline <0.0001; chime <0.157; chime/display <0.0001; display = 0.0002; washout <0.0001) (Figure 4B). The use of the door entry/exit chime and computer monitor feedback resulted in the greatest increase of activity compared to baseline during both shifts.
Figure 4.
(A) Comparison of the number of hand hygiene events in the test intensive care unit (ICU) during the day and night shifts during baseline, chime, chime/display, display, and washout trial phases. +, the number of hand hygiene events on individual days on the day shift; o, the number of hand hygiene events on individual days on the night shift. (B) A comparison of the hand hygiene event to room entry exit event (HHEE) ratio in the test ICU for the day and night shifts during baseline, chime, chime/display, display and washout trial phases. +, the ratio of events on individual days on the day shift; o, the ratio of events on individual days on the night shift.
DISCUSSION
Despite intensive ongoing international efforts to improve hand hygiene compliance, few systems have been developed and objectively shown to improve healthcare worker hand hygiene activities. A number of studies have reported that hand hygiene activity amongst healthcare workers improved with the use of human auditors; however, there are concerns with observer and selection biases as well as with the Hawthorne effect [22]. More recently, improvement to hand hygiene compliance has been shown with the use of video monitoring systems, alcohol sensor systems, and individual healthcare worker wireless devices; although the use of these systems seems to be limited by high installation and/or maintenance costs [7–9, 11, 12].
Results from this prospective controlled trial found that an electronic hand hygiene monitoring system can increase both the absolute number of hand hygiene events and the ratio of hand hygiene events to room entry/exit events in an ICU setting. The use of a simple reminder chime on room entry/exit was able to initially increase hand hygiene activity, but it was associated with an apparent decay in the effectiveness of this audible alarm on room entry/exit over the 5-week phase. The decay is most likely related to the well defined problem of monitor alarm fatigue [23]. In contrast, the concurrent use of the audible room entry/exit chime and real-time feedback on hand hygiene activity to healthcare workers led to a sustained significant increase in hand hygiene activity without an observed decay in efficacy. Hand hygiene activity decreased when the real-time feedback was used alone without the concurrent audible chime, suggesting that the immediate reminder provided by the audible chime remained important; although it is also possible that the observed decrease was linked to a more delayed onset of alarm fatigue.
It should be noted that the calculated HHEE ratio is a different metric than hand hygiene compliance as measured by direct observation. First, with the exception of hand hygiene events that occur within patient rooms, it does not associate individual hand hygiene events with individual room entry/exit events to confirm individual provider compliance. Second, it does not recognize single hand hygiene events that are considered compliant for 2 patient encounters, for example, when a healthcare worker begins hand hygiene activity while exiting one patient room and immediately enters a second patient room; therefore we identified a lower ratio than through direct observation. Third, it does not identify occurrences when a healthcare worker might enter the doorway of a patient room and have a conversation with the patient or family or check on the status of a sleeping patient without becoming involved in patient care. Depending on the situation, such interactions may or may not be considered compliant by direct observation. However, the purpose of calculating and providing the HHEE ratio in the real-time display was to provide a relative index of hand hygiene performance that could be used to encourage unit staff to increase hand hygiene activity. In addition, both the absolute number of hand hygiene events and the HHEE ratio are objective, reproducible metrics that can be used to track hand hygiene activity over time for individual units as demonstrated in this and prior studies, and these could be potentially used to compare hand hygiene performance between units or institutions [24, 25].
Although subject to the limitations in defining hand hygiene compliance as noted above, the hand hygiene activity observed during the course of this trial was lower than hand hygiene compliance reported in studies done with human observers [4, 5]. However, the baseline hand hygiene activity appears comparable to that in multiple other studies of electronic hand hygiene monitoring systems [15, 16, 18, 26, 27]. Of note, a recent large study reported on hand hygiene activity between 2010 and 2013 in 35 hospitals that had installed electronic badge-based hand hygiene monitoring systems. The study encompassed over 4100 monitored healthcare workers and over 13.7 million hand hygiene opportunities; overall, hand hygiene compliance was only 42.6% during the first hour of a healthcare worker's shift and declined progressively during the time on duty to 34.8% at the end of a shift [27]. These differences in measured hand hygiene activity from electronic monitoring systems and human observations likely relate to technical factors as detailed above for the HHEE ratio, but also to limitations in human observation due to the small fraction of healthcare worker patient interactions that can be monitored, to measurement errors by human observers, and to very pronounced Hawthorne effects [16, 28–30]. The findings from this and other studies of electronic monitoring systems indicate that further efforts are needed to promote optimal hand hygiene by healthcare workers.
We identified a consistent significantly higher level of hand hygiene activity during the overnight shift compared to the day shift. This difference persisted even though this information was conveyed to the unit staff during the course of the trial. It is likely that the night shift hand hygiene activity predominantly represents unit staff activity because other staff and visitors are less likely to be present. There are only limited other data on differences in hand hygiene activity in the hospital setting during the course of the day. Two studies that electronically tracked hand hygiene dispenser event found that the number of hand hygiene events was greater during the day shift than evening shift, although the studies could not assess the relationship between hand hygiene events and patient care activities [20, 31]. An additional study that measured alcohol rub dispenser use and room entry/exit monitors in a hematopoietic stem cell transplant/hematology unit similarly found that hand hygiene compliance was significantly higher during the day shift (8:00 am to 7:59 pm) than on the night shift [19]. However, a fourth study by Cheng et al [16] found no difference in hand hygiene activity between shifts in a small open 6-bed neurosurgical unit.
Why there is a difference in hand hygiene activity between shifts is not clear. Although variation in patient care practices between shifts certainly contributes to the observed differences, recent work on peer effects on hand hygiene compliance is likely also relevant to this issue [26, 32, 33]. In particular, Monsalve et al [26] assessed the relationship between hand hygiene compliance and the presence of other healthcare workers, and they found that when other healthcare workers were present—and within close proximity—hand hygiene compliance increased. Given that fewer healthcare workers are normally present during night shifts, the lack of peer effects could contribute to lower observed hand hygiene activity. It is notable that the one trial that did not observe differences in hand hygiene activity between shifts was performed in an open ward, all beds and healthcare worker activity was visible to others [16]. Future different teaching approaches are likely necessary for institutions to promote hand hygiene activity for personnel working at night [26].
The fact that hand hygiene activity varies by shift also raises concerns regarding how institutions monitor hand hygiene activity. The use of anonymous observers has been advocated for measuring hand hygiene compliance to avoid observer bias noted with unit-based hand hygiene observers that in general leads to an overestimation of healthcare worker hand hygiene activity [4, 34]. However, the use of anonymous observers is functionally implausible on night shifts in most hospital settings because nonunit-based observers will be immediately recognized by healthcare staff.
This trial has several significant strengths. First, the physical structure, staffing, and patient population characteristics of the 2 units allowed us to perform a prospective controlled trial of the monitoring and reminding technology. Second, the duration of the trial and the large number of observed events allowed us to assess differences in hand hygiene events during different time periods, and these factors also allowed for analysis of decays in the effectiveness of the reminder system linked to monitor fatigue.
The trial was subject to several limitations. First, overall hand hygiene activity across the entire unit was monitored, and individual healthcare worker activity was not collected. Therefore, it was impossible to define whether observed hand hygiene activity was linked to that of healthcare workers or to other individuals in the ICU, including housekeepers, radiology technicians, non-ICU healthcare workers, and/or visitors. In addition, other staff and visitors were not as aware of the reminder system, and thus they may have been less responsive to the audible reminders and real-time feedback displays. This could have led to an underestimation of the impact of the reminder system on the healthcare worker hand hygiene activity in the unit. Second, the system could not assess the 5 moments of hand hygiene advocated by the World Health Organization [3]. Third, it remains possible that there could have been intercurrent events that impacted overall healthcare worker awareness of the need to perform hand hygiene; although, in this regard, there was no apparent change in the number of hand hygiene events recorded in the control ICU during the course of the trial. Fourth, each reminder system phase was approximately 5 weeks, and it is possible that the study duration was not adequate to fully exclude the possibility of monitor fatigue. Finally, our study was conducted at a tertiary care academic medical center within 2 medical ICUs and may not be generalizable to other clinical settings.
CONCLUSIONS
In summary, an electronic hand hygiene monitoring and reminder system was found to be able to increase hand hygiene performance in an ICU setting. In particular, hand hygiene activity increased with the use of audible room entry/exit reminders as well as real-time computer monitor and manager reports feedback. The system was able to monitor hand hygiene activity for 24 hours a day, unlike direct observer monitoring, and it could do so at times when direct observations could not be objectively performed. Although the system did not provide the detail of information provided by electronic systems that identify individual healthcare worker behavior, this group monitoring system has the potential to be a less expensive approach to increasing hand hygiene behavior in the healthcare setting and to do so in a less intrusive manner. This anonymous approach may be more acceptable to those healthcare workers who have privacy concerns regarding hand hygiene monitoring [21]. Beyond this, by providing objective and detailed information on hand hygiene activity among healthcare workers, it can provide direct feedback to hospital staff as to their relative level of hand activity in comparison with different shifts in the same unit, in the same unit over time, or between different units using such a system. In addition, such systems could allow for a more definitive determination of the impact of hand hygiene on the rate of hospital-acquired infections as well as its effectiveness in limiting the transmission of multidrug-resistant bacteria [35, 36].
Supplementary Material
Acknowledgments
This work was presented in part in abstract form at IDweek in October 2013. We are grateful to the staff of the intensive care units that participated in the study, to the UMass Memorial Medical Center Critical Care Operations Committee for its support of the trial, and to Han Wang, Lei Cao, Charles Johnston, John Hennessy, John Kilburg, David Snodgrass, Lauren Brais, and Tonje Stolpestad for their assistance in this work.
Financial support. This work was supported by a University of Massachusetts Medical School – Worcester Polytechnic Institute pilot program; and by the National Center for Research Resources (NCRR) [grant number UL1RR031982]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NCRR or the National Institutes of Health. Ultraclenz, LLC, provided all hardware components and the basic software for the Electronic Hand Hygiene Reminder System.
Potential conflicts of interest. Richard Ellison, Di Wang, and Elke Rundensteiner have patent pending on software used for active complex event processing software system used for real-time data processing and the electronic reminder system. All other authors report no potential conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Larson E. A causal link between handwashing and risk of infection? Examination of the evidence. Infect Control Hosp Epidemiol 1988; 9:28–36. [DOI] [PubMed] [Google Scholar]
- 2.Boyce JM, Pittet D. Guideline for hand hygiene in health-care settings. Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Society for Healthcare Epidemiology of America/Association for Professionals in Infection Control/Infectious Diseases Society of America. MMWR Recomm Rep 2002; 51(RR-16):1–45. [PubMed] [Google Scholar]
- 3.Pittet D, Allegranzi B, Boyce J. The World Health Organization Guidelines on Hand Hygiene in Health Care and their consensus recommendations. Infect Control Hosp Epidemiol 2009; 30:611–22. [DOI] [PubMed] [Google Scholar]
- 4.The Joint Commission Measuring Hand Hygiene Adherence: Overcoming the Challenges. 1st ed Oakbrook Terrace, IL: The Joint Commission, 2009. [Google Scholar]
- 5.Erasmus V, Daha TJ, Brug H et al. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol 2010; 31:283–94. [DOI] [PubMed] [Google Scholar]
- 6.Boyce JM. Measuring healthcare worker hand hygiene activity: current practices and emerging technologies. Infect Control Hosp Epidemiol 2011; 32:1016–28. [DOI] [PubMed] [Google Scholar]
- 7.Ward MA, Schweizer ML, Polgreen PM et al. Automated and electronically assisted hand hygiene monitoring systems: A systematic review. Am J Infect Control 2014; 42:472–8. [DOI] [PubMed] [Google Scholar]
- 8.Armellino D, Hussain E, Schilling ME et al. Using high-technology to enforce low-technology safety measures: the use of third-party remote video auditing and real-time feedback in healthcare. Clin Infect Dis 2012; 54:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Armellino D, Trivedi M, Law I et al. Replicating changes in hand hygiene in a surgical intensive care unit with remote video auditing and feedback. Am J Infect Control 2013; 41:925–7. [DOI] [PubMed] [Google Scholar]
- 10.Levchenko AI, Boscart VM, Fernie GR. The feasibility of an automated monitoring system to improve nurses’ hand hygiene. Int J Med Inform 2011; 80:596–603. [DOI] [PubMed] [Google Scholar]
- 11.Marra AR, Sampaio Camargo TZ, Magnus TP et al. The use of real-time feedback via wireless technology to improve hand hygiene compliance. Am J Infect Control 2014; 42:608–11. [DOI] [PubMed] [Google Scholar]
- 12.Edmond MB, Goodell A, Zuelzer W et al. Successful use of alcohol sensor technology to monitor and report hand hygiene compliance. J Hosp Infect 2010; 76:364–5. [DOI] [PubMed] [Google Scholar]
- 13.Al Salman JM, Hani S, de Marcellis-Warin N, Fatima Isa S. Effectiveness of an electronic hand hygiene monitoring system on healthcare workers’ compliance to guidelines. J Infect Public Health 2015; 8:117–26. [DOI] [PubMed] [Google Scholar]
- 14.Storey SJ, FitzGerald G, Moore G et al. Effect of a contact monitoring system with immediate visual feedback on hand hygiene compliance. J Hosp Infect 2014; 88:84–8. [DOI] [PubMed] [Google Scholar]
- 15.Swoboda SM, Earsing K, Strauss K et al. Electronic monitoring and voice prompts improve hand hygiene and decrease nosocomial infections in an intermediate care unit. Crit Care Med 2004; 32:358–63. [DOI] [PubMed] [Google Scholar]
- 16.Cheng VC, Tai JW, Ho SK et al. Introduction of an electronic monitoring system for monitoring compliance with Moments 1 and 4 of the WHO “My 5 Moments for Hand Hygiene” methodology. BMC Infect Dis. 2011; 11:151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Swoboda SM, Earsing K, Strauss K et al. Isolation status and voice prompts improve hand hygiene. Am J Infect Control 2007; 35:470–6. [DOI] [PubMed] [Google Scholar]
- 18.Fisher DA, Seetoh T, Oh May-Lin H et al. Automated measures of hand hygiene compliance among healthcare workers using ultrasound: validation and a randomized controlled trial. Infect Control Hosp Epidemiol 2013; 34:919–28. [DOI] [PubMed] [Google Scholar]
- 19.Venkatesh AK, Lankford MG, Rooney DM et al. Use of electronic alerts to enhance hand hygiene compliance and decrease transmission of vancomycin-resistant Enterococcus in a hematology unit. Am J Infect Control 2008; 36:199–205. [DOI] [PubMed] [Google Scholar]
- 20.Boyce JM, Cooper T, Dolan MJ. Evaluation of an electronic device for real‐time measurement of alcohol‐based hand rub use. Infect Control Hosp Epidemiol 2009; 30:1090–5. [DOI] [PubMed] [Google Scholar]
- 21.Srigley JA, Gardam M, Fernie G et al. Hand hygiene monitoring technology: a systematic review of efficacy. J Hosp Infect 2015; 89:51–60. [DOI] [PubMed] [Google Scholar]
- 22.Srigley JA, Furness CD, Baker GR, Gardam M. Quantification of the Hawthorne effect in hand hygiene compliance monitoring using an electronic monitoring system: a retrospective cohort study. BMJ Qual Saf 2014; 23:974–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cvach M. Monitor alarm fatigue: an integrative review. Biomed Instrum Technol 2012; 46:268–77. [DOI] [PubMed] [Google Scholar]
- 24.Marra AR, D'Arco C, Bravim Bde A et al. Controlled trial measuring the effect of a feedback intervention on hand hygiene compliance in a step-down unit. Infect Control Hosp Epidemiol 2008; 29:730–5. [DOI] [PubMed] [Google Scholar]
- 25.Morgan DJ, Pineles L, Shardell M et al. Automated hand hygiene count devices may better measure compliance than human observation. Am J Infect Control 2012; 40:955–9. [DOI] [PubMed] [Google Scholar]
- 26.Monsalve MN, Pemmaraju SV, Thomas GW et al. Do peer effects improve hand hygiene adherence among healthcare workers? Infect Control Hosp Epidemiol 2014; 35:1277–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dai H, Milkman KL, Hofmann DA, Staats BR. The impact of time at work and time off from work on rule compliance: the case of hand hygiene in health care. J Appl Psychol 2015; 100:846–62. [DOI] [PubMed] [Google Scholar]
- 28.Fries J, Segre AM, Thomas G et al. Monitoring hand hygiene via human observers: how should we be sampling? Infect Control Hosp Epidemiol 2012; 33:689–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sharma D, Thomas GW, Foster ED et al. The precision of human-generated hand-hygiene observations: a comparison of human observation with an automated monitoring system. Infect Control Hosp Epidemiol 2012; 33:1259–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hagel S, Reischke J, Kesselmeier M et al. Quantifying the Hawthorne effect in hand hygiene compliance through comparing direct observation with automated hand hygiene monitoring. Infect Control Hosp Epidemiol 2015; 36:957–62. [DOI] [PubMed] [Google Scholar]
- 31.Helder OK, van Goudoever JB, Hop WC et al. Hand disinfection in a neonatal intensive care unit: continuous electronic monitoring over a one-year period. BMC Infect Dis 2012; 12:248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lankford MG, Zembower TR, Trick WE et al. Influence of role models and hospital design on hand hygiene of healthcare workers. Emerg Infect Dis 2003; 9:217–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Haessler S, Bhagavan A, Kleppel R et al. Getting doctors to clean their hands: lead the followers. BMJ Qual Saf 2012; 21:499–502. [DOI] [PubMed] [Google Scholar]
- 34.Haas JP, Larson EL. Measurement of compliance with hand hygiene. J Hosp Infect 2007; 66:6–14. [DOI] [PubMed] [Google Scholar]
- 35.Pittet D, Hugonnet S, Harbarth S et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infect Control Programme Lancet 2000; 356:1307–12. [DOI] [PubMed] [Google Scholar]
- 36.Derde LP, Cooper BS, Goossens H et al. Interventions to reduce colonisation and transmission of antimicrobial-resistant bacteria in intensive care units: an interrupted time series study and cluster randomised trial. Lancet Infect Dis 2014; 14:31–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.