Abstract
Corpus luteal rupture is a common gynecologic cause for hemoperitoneum. Recent sexual intercourse is usually a preceding factor. However, postcoital hemoperitoneum without evident vaginal injury or trauma is rarely reported. We present a 34-year-old female who presented to the emergency department with severe bilateral lower quadrant abdominal pain after sexual intercourse. CT of the abdomen and pelvis revealed an intra-abdominal hematoma with extravasation of contrast questionable to be from one of the branches of the left internal iliac artery, and no adnexal abnormalities. Left internal iliac artery angiogram was performed and revealed no active extravasation. Exploratory laparotomy was performed and revealed an actively bleeding left ovarian ruptured area that was repaired and biopsied. No evidence of cysts was observed. Histopathological examination revealed a hemorrhagic corpus luteal cyst. Suspicion for corpus luteal rupture as a cause of postcoital hemoperitoneum should be maintained despite nonevidence of cysts on CT or intraoperatively.
INTRODUCTION
Postcoital hemoperitoneum without evident vaginal injury is rarely reported [1, 2]. Ruptured hemorrhagic corpus luteum is one of the most common gynecologic causes of hemoperitoneum [3, 4]. We here report the case of a 34-year-old female who presented with postcoital hemoperitoneum without vaginal injury due to rupture of a corpus luteal cyst that was identified only after surgical biopsy and histopathological examination.
CASE REPORT
A 34-year-old female with no past medical history was transferred to our emergency department from an outside hospital due to concern for intra-abdominal bleeding. She initially presented with lower abdominal pain immediately following vaginal intercourse described as nonvigorous with the patient mostly ‘on top’, and no history of foreign body use or trauma. CT of the abdomen and pelvis with IV contrast performed at the outside hospital revealed an intra-abdominal hematoma with extravasation of contrast questionably from one of the branches of the left internal iliac artery (Figs 1 and 2). No adnexal lesions were identified on the CT. Upon arrival, the patient was complaining of constant, sharp, severe bilateral lower quadrant abdominal pain, nausea and fatigue. There was no history of loss of consciousness, vomiting, vaginal or rectal bleeding, or hematuria. A past surgical history consisted of appendectomy. Her last menstrual period was 19 days prior to presentation.
Figure 1:
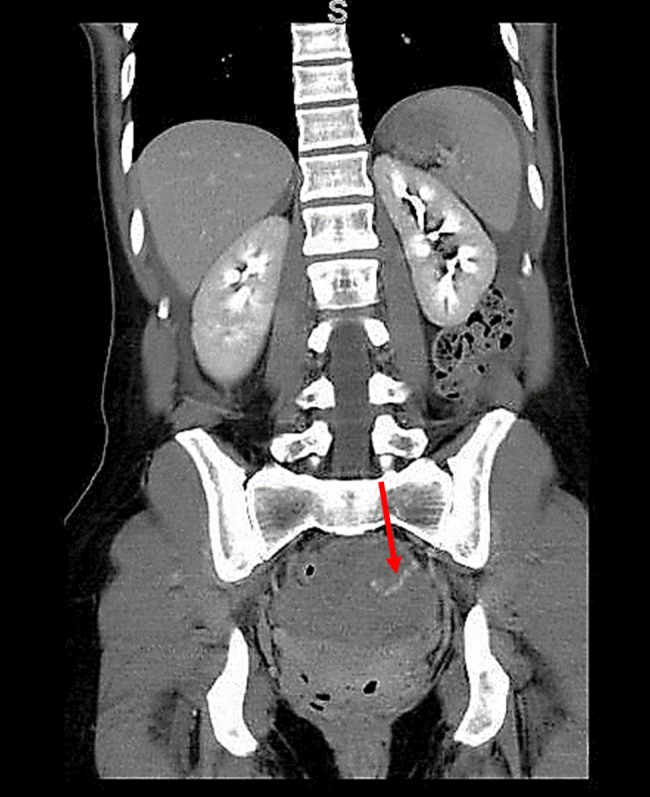
CT (coronal view) of the abdomen and pelvis showing extravasation of contrast material into the left pelvis (red arrow).
Figure 2:
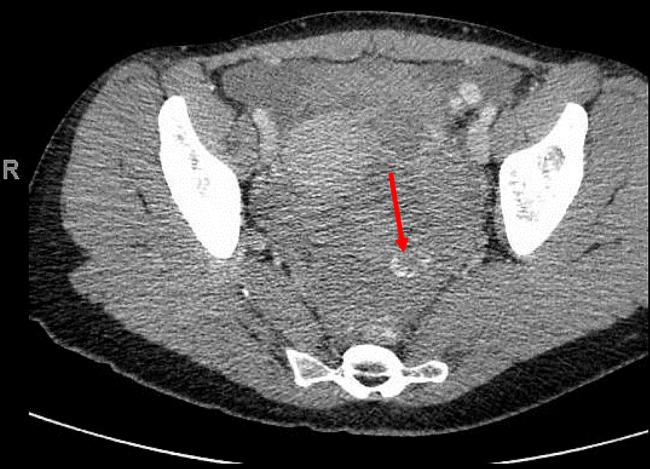
CT (axial view) of the pelvis showing extravasation of contrast material into the left pelvis (red arrow).
On examination, the patient was in painful distress. Vital signs were stable. Abdominal examination revealed bilateral lower quadrant and suprapubic tenderness with guarding. Perineal and genital examination revealed no evidence of trauma. Laboratory investigations revealed a white cell count of 12 200/mm3 and hemoglobin of 9.5 g/dl. Basic metabolic panel, partial thromboplastin time, international normalized ratio, lipase, ethyl alcohol level and urinalysis were normal. β-hCG was negative for pregnancy.
Based on the CT scan findings, interventional radiology was consulted and selective left internal iliac artery angiogram was performed and identified no active extravasation or pseudoaneurysm. Exploratory laparotomy was then performed to identify the source of bleeding. Preoperatively, blood pressure was 97/47 and the heart rate was 76 bpm. Upon entry to the peritoneal cavity, 900 ml of hemoperitoneum was observed and washed out. Active bleeding was identified from a ruptured area on the left ovary and control of bleeding followed by primary repair of the ovary was performed. Except for the ruptured area, no other signs of anatomical abnormalities, tumors or cysts were observed in the ovary. Four portions of the hemorrhagic soft tissue from the ovary were sent for histopathological examination that revealed a hemorrhagic corpus luteal cyst. Postoperatively, the patient was vitally stable, but received blood products for a low hemoglobin of 7.8 g/dl. The remaining postoperative course was uneventful. The patient was discharged on postoperative day 3 and is doing well.
DISCUSSION
In women of reproductive age presenting with acute abdomen, the differential diagnosis includes a number of gynecologic conditions. Rupture of a corpus luteal cyst wall is a rare complication and may lead to hemoperitoneum [3]. Postcoital hemoperitoneum without evident vaginal injury has infrequently been reported in the literature [2].
The features of corpus luteum hemorrhage have been similar in previous studies [5, 6] and include: (i) patient age range within reproductive years, (ii) sharp and sudden-onset pain more often on the right than the left side, (iii) history of recent sexual intercourse or strenuous physical activity, (iv) a tendency of onset during the secretory phase of the menstrual cycle and (v) an increased incidence in pregnant females.
Postcoital hemoperitoneum can be caused by forces occurring during intercourse that can result in acceleration–deceleration injuries [2]. Postcoital pain can vary in localization, radiation, time of onset since injury and progression [1, 7, 8]. Hemoglobin level is usually normal, and blood transfusion is rarely required. However, reports of postcoital hemoperitoneum volume range from 150 to >2000 ml [2]. Multiple sources of bleeding have been identified including a lacerated round ligament, a lacerated ovary, ruptured serous cystadenoma and ruptured corpus luteum cysts [8]. Ho et al. described 91 women diagnosed with ruptured corpus luteum cysts and hemoperitoneum, most of which reported recent sexual intercourse prior to the onset of pain [4].
The diagnosis of ruptured corpus luteal cyst begins with clinical suspicion from history, with patients usually being in the luteal phase of the ovarian cycle and may present after recent sexual intercourse or pelvic trauma. Patients may present with no apparent clinical signs to severe peritoneal irritation. β-hCG level is necessary to differentiate ruptured corpus luteal cyst from ruptured ectopic pregnancy, which may have a similar presentation [3]. Other features may include anemia, elevated CRP and mild leukocytosis [3]. Ultrasound is usually the first imaging modality due to its high sensitivity and ease of access, and can effectively diagnose corpus luteal hemorrhage [3, 4]. Although CT scanning is more sensitive than ultrasonography, it is less specific in detecting ovarian cysts. However, CT is considered the best option for imaging hemorrhagic ovarian cysts or hemoperitoneum due to cyst rupture and can be used to differentiate other intra-abdominal causes of acute hemorrhage [9]. On CT scan, corpus luteal cysts usually appear as a well-circumscribed unilocular adnexal lesion, rarely bilocular. The cyst walls appear slightly thickened (<3 mm) and show a characteristic inhomogeneous contrast enhancement after administration of contrast medium due to increased vascularity [3].
Historically, management of hemoperitoneum due to corpus luteal rupture was exclusively surgical. More recently, conservative management is possible and considered the first treatment of choice in patients with clear-cut ultrasound diagnosis, hemodynamic stability (systolic BP >90) and stable hemoglobin values over 4–6 h of monitoring [3, 4]. In addition to the use of intravenous fluids and blood transfusion, administration of tranexamic acid (500 mg intravenous loading dose and 250 mg intravenous maintenance dose every 6 h) has also been suggested [4]. According to the literature, laparoscopy seems to be the preferred surgical diagnostic modality for those with hemodynamic instability, with conversion to laparotomy in case of failure, or a decrease in hemoglobin of ∼2 g/dl over 4–6 h with increasing hemoperitoneum on follow-up imaging studies [4].
Postcoital hemoperitoneum without evidence of genital trauma is rare. Corpus luteal rupture is a well-known cause for hemoperitoneum with recent sexual intercourse frequently being reported. Corpus luteal rupture as a cause of postcoital hemoperitoneum should be suspected despite a paucity of CT or intraoperative evidence of cysts. A histopathological examination serves as the definitive modality to identify the underlying etiology of hemorrhage. Surgical management provides excellent results.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.Goswami A, Raghavan SS, Ghotekar LH. Postcoital haemoperitoneum: a cause for shock. Emerg Med Australas 2004;16:170–1. [DOI] [PubMed] [Google Scholar]
- 2.Mandato VD, Pirillo D, Ciarlini G, Comitini G, La Sala GB. Postcoital haemperitoneum without vaginal injury: a clinical challenge. Aust N Z J Obstet Gynaecol 2010;50:580–1. [DOI] [PubMed] [Google Scholar]
- 3.Fiaschetti V, Ricci A, Scarano AL, Liberto V, Citraro D, Arduini S et al. Hemoperitoneum from corpus luteal cyst rupture: a practical approach in emergency room. Case Rep Emerg Med 2014;2014:252657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ho WK, Wang YF, Wu HH, Tsai HD, Chen TH, Chen M. Ruptured corpus luteum with hemoperitoneum: case characteristics and demographic changes over time. Taiwan J Obstet Gynecol 2009;48:108–12. [DOI] [PubMed] [Google Scholar]
- 5.Hallatt JG, Steele CH, Snyder M. Ruptured corpus luteum with hemoperitoneum: a study of 173 surgical cases. Am J Obstet Gynecol 1984;149:5–9. [DOI] [PubMed] [Google Scholar]
- 6.Sivanesaratnam V, Singh A, Rachagan SP, Raman S. Intraperitoneal haemorrhage from a ruptured corpus luteum. A cause of ‘acute abdomen’ in women. Med J Aust 1986;144:411, 413–4. [PubMed] [Google Scholar]
- 7.Yian MT, Chen HJ, Chu TY, Yin CS. Postcoital hemoperitoneum without identifiable bleeding source: a case report. Zhonghua Yi Xue Za Zhi 1996;58:291–3. [PubMed] [Google Scholar]
- 8.McColgin SW, Williams LM, Sorrells TL, Morrison JC. Hemoperitoneum as a result of coital injury without associated vaginal injury. Am J Obstet Gynecol 1990;163:1503–5. [DOI] [PubMed] [Google Scholar]
- 9.Vandermeer FQ, Wong-You-Cheong JJ. Imaging of acute pelvic pain. Clin Obstet Gynecol 2009;52:2–20. [DOI] [PubMed] [Google Scholar]


