Abstract
Background
An early provision of the Affordable Care Act (ACA) eliminated cost-sharing for a range of recommended preventive services. This provision took effect in September 2010, but little is known about its effect on preventive service use.
Methods
We evaluated changes in the use of recommended preventive services from 2009 (before the implementation of ACA cost-sharing provision) to 2011/2012 (after the implementation) in the Medical Expenditure Panel Survey, a nationally representative household interview survey in the US. Specifically, we examined: blood pressure check, cholesterol check, flu vaccination, and cervical, breast, and colorectal cancer screening, controlling for demographic characteristics and stratifying by insurance type.
Results
There were 64,280 (21,310 before and 42,970 after the implementation of ACA cost-sharing provision) adults included in the analyses. Receipt of recent blood pressure check, cholesterol check and flu vaccination increased significantly from 2009 to 2011/2012, primarily in the privately insured population aged 18–64 years, with adjusted prevalence ratios (95% confidence intervals) 1.03 (1.01–1.05) for blood pressure check, 1.13 (1.09–1.18) for cholesterol check and 1.04 (1.00–1.08) for flu vaccination (all p-values < 0.05). However, few changes were observed for cancer screening. We observed little change in the uninsured population.
Conclusions
These early observations suggest positive benefits from the ACA policy of eliminating cost-sharing for some preventive services. Future research is warranted to monitor and evaluate longer term effects of the ACA on access to care and health outcomes.
Keywords: Affordable Care Act, Preventive services, Cancer screening, Cost-sharing, Insurance
Introduction
Out-of-pocket payments can be a barrier to the use of recommended preventive services (Rezayatmand et al., 2013; Trivedi et al., 2008). Previous studies have shown that reductions in cost-sharing were associated with increased use of preventive services (Goodwin and Anderson, 2012; Guy, 2010; Meeker et al., 2011; Sabatino et al., 2012; Solanki and Schauffler, 1999; Solanki et al., 2000), although these studies were limited by older data or selected study participants with certain insurance types or employers. Few studies evaluated the effects of cost-sharing on use of preventive services in national population-based samples (Rezayatmand et al., 2013). Further, many of these studies only evaluated a few types of preventive services, mostly cancer screening (Rezayatmand et al., 2013).
With a strong emphasis on disease prevention, the Affordable Care Act (ACA) requires non-grandfathered private health plans (i.e. plans effective after the ACA was signed on March 23, 2010 or plans that existed before the ACA but lost its grandfathered status at renewal (Washington State Office of the Insurance Commissioner, 2014)) to provide coverage without cost-sharing for preventive services rated as `A' (strongly recommended) or `B' (recommended) by the US Preventive Services Task Force (USPSTF), for vaccinations recommended by the Advisory Committee on Immunization Practices (ACIP), and services for infants, women, and children recognized by the Health Resources and Services Administration (Fox and Shaw, 2015). This provision took effect for non-grandfathered private health plans starting with plan years beginning after September 23, 2010. Medicare was also required to eliminate cost-sharing starting January 1, 2011 for preventive services recommended by the USPSTF (Fox and Shaw, 2015). By definition, elimination of cost-sharing for recommended preventive services did not affect the uninsured. Thus, the implementation of this ACA provision provides an opportunity to evaluate the association between cost-sharing elimination and utilization of recommended preventive services by type of health insurance, at a national population-based level.
To fill research gaps on the relationship between cost-sharing and preventive service use and to evaluate the early impact of ACA elimination of cost-sharing provision, we analyzed nationally representative survey data and examined changes in use of multiple preventive services and cancer screening services before and after the implementation of the ACA provision. Furthermore, we also examined the heterogeneity in the effects of cost-sharing: if the low income and the sickest population were more likely to adjust health care utilization in response to changes in cost-sharing, as suggested by previous studies (Baicker and Goldman, 2011).
Methods
Study sample
The study sample included adults aged ≥18 years in the pooled data from 2009 (before the implementation of ACA elimination of cost-sharing for recommended preventive services) and from 2011/12 (after the implementation) Medical Expenditure Panel Survey (MEPS) Household Component. The MEPS is a nationally representative survey of the US civilian non-institutionalized population sponsored by the Agency for Healthcare Research and Quality. The MEPS collects data on health insurance, access to care, utilization, and cost of specific health services in addition to demographic characteristics and health history. The combined average annual response rate for 2009, 2011 and 2012 was approximately 56% (57%, 55% and 56% for 2009, 2011 and 2012, respectively). More information about the survey design and content is available from http://meps.ahrq.gov/mepsweb/. All data used were publicly available and deidentified, thus Institutional Review Board approval was not required for this study.
In our analysis, we included privately insured individuals aged 18–64 years, Medicare insured individuals aged ≥65 years, and uninsured individuals aged 18–64 years. The ACA provision eliminating cost-sharing applies to the first two groups, but not the last one. Those aged 18–64 years with public insurance were excluded because of mixed requirements regarding cost-sharing and different responses to the ACA provision in various public insurances (e.g. TRICARE, Medicaid of different states) (Office of the Secretary, Department of Defense, 2011; Wilensky and Gray, 2013). Those younger than 65 with Medicare only and those aged ≥65 without Medicare were excluded because of low frequencies.
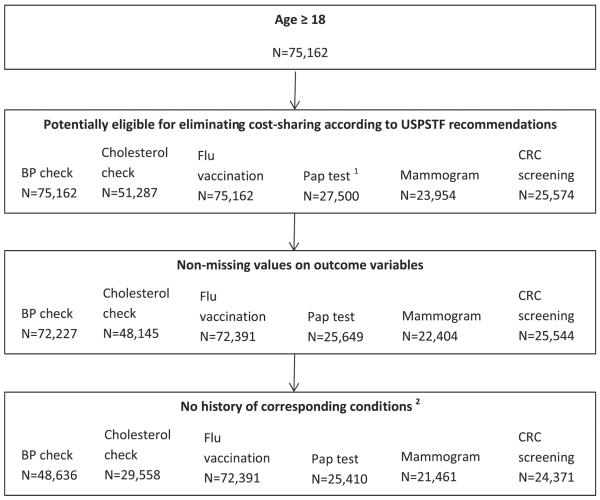
Our study population for each preventive service was defined separately to be consistent with the recommendation from the USPSTF and ACIP, and thus potentially covered by the ACA-preventive care provision. The specific recommendations (the specific year of the USPSTF recommendation used is provided in parentheses), level of evidence (grade), and participants in analysis are listed in the Appendix Table for the preventive services: blood pressure screening (2007), cholesterol screening (2008), influenza (flu) vaccinations (2009), and cancer screening services for breast cancer (2002), cervical cancer (2012) and colorectal cancer (2008). We used the age range 21–65 years for cervical cancer screening according to the USPSTF recommendation released in 2012 because this age range is applicable to all three study years while the previous recommendations are not. Women who had hysterectomy were excluded from the analyses for cervical cancer screening. Survey respondents were also excluded if time since last preventive service was missing or they had a history of the condition related to the preventive service in question (no exclusion was made based on history of condition for flu vaccination). A detailed inclusion/exclusion diagram and sample sizes for analyses of each of the preventive services is presented in Fig. 1.
Fig. 1.
Inclusion/exclusion diagram for the study participants in the Medical Expenditure Panel Survey, 2009 and 2011/2012. USPSTF = US Preventive Services Task Force; ACIP = Advisory Committee on Immunization Practices; BP = blood pressure; Pap = Papanicolaou; CRC = colorectal cancer. 1Women who had hysterectomy were excluded. 2High blood pressure for BP check; high cholesterol for cholesterol check; cervical cancer for Pap test; breast cancer for mammograms; colorectal cancer for CRC screening.
Measures
Outcomes
Receipt of preventive services, including cancer screening, recommended by the USPSTF and ACIP was measured by a series of related questions. Our outcome variables include self-reported receipt of the following services within the past year: blood pressure check, cholesterol check, flu vaccination, cervical cancer screening [Papanicolaou (Pap) test] and breast cancer screening (mammogram) for females, and any colorectal cancer screening (home blood stool testing, colonoscopy, or sigmoidoscopy). These variables were available in MEPS and recommended by the USPSTF. The exact wordings of the MEPS questionnaire items for these preventive services are listed in the Appendix Table.
Covariates
Survey year (2009 as the pre-ACA year vs. 2011/2012 as the post-ACA years) was the main covariate of interest in this study. Demographic characteristics in the multivariable analyses include: age (18–25, 26–29, 30–39, 40–49, 50–65, 65–74, 75+), gender, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other), education (less than high school, high school graduate, some college, college graduate or more), marital status (yes, no), region (Northeast, Midwest, South, West), residence in a metropolitan statistical area (MSA) (yes, no) and number of chronic conditions (0, 1, 2+). The number of chronic conditions was ascertained from a series of questions about whether a doctor or other health professional ever told the person they had high blood pressure, heart disease (including coronary heart disease, angina, myocardial infarction, and other unspecified heart disease), stroke, emphysema, high cholesterol, cancer (including cancer type), diabetes, arthritis, or asthma. Conditions were categorized by the absolute number of chronic conditions for each participant. We measured insurance type for each participant as: 1) aged 18–64 years with any private insurance, 2) aged ≥65 years with Medicare, and 3) aged 18–64 years with no insurance. Family income was classified into three categories according to the poverty line: low income (less than 200%), middle income (200% to <400%) and high income (≥400%); missing income was imputed using logical editing and weighted, sequential hot-decks (Agency for Healthcare Research and Quality, 2014a).
Statistical analysis
Descriptive statistics were calculated by survey year, and distributions were compared with chi-square tests (two-sided, significance level=0.05). Missing values for education and number of chronic conditions were treated as not missing completely at random in the weighted frequency calculation. To evaluate the association between survey year and receipt of preventive services, adjusted prevalence of receipt and marginal prevalence ratio (PR) and the 95% confidence intervals (CI) (Bieler et al., 2010) were calculated for each insurance type using multivariable logistic regression controlling for age, gender, race/ethnicity, education, marital status, region, residence, and number of chronic conditions. In order to assess if the association varied by socioeconomic status (Damiani et al., 2011; Hoeck et al., 2014; Sambamoorthi and McAlpine, 2003) and health status, we further conducted stratified analyses by family income and the number of chronic conditions, particularly for adults aged 18–64 years with any private insurance. Family income was chosen for the stratified analysis instead of education because of data completeness. The interaction effect between survey year and family income or number of chronic conditions was tested at a significance level of 0.05 in separate models with an interaction term added.
All analyses were conducted using SAS 9.3 and SAS-Callable SUDAAN (SAS Institute Inc, Cary, NC). Survey procedures were used to account for the MEPS complex survey design and survey nonresponse (Agency for Healthcare Research and Quality, 2014a).
Results
We identified 64,280 (21,310 before and 42,970 after the implementation of ACA cost-sharing provision) adults eligible in the study. The majority of the participants were younger than 65 years old, non-Hispanic white, living in an MSA and privately insured (Table 1). Participants were similar before and after the ACA implementation, except that those from 2009 were slightly younger (56.5% vs. 54.5% less than 50 years old) and had a lower educational level (45.9% vs. 41% did not go to college) (Table 1).
Table 1.
Demographic characteristics, Medical Expenditure Panel Survey 2009, 2011 and 2012.
| Characteristic | 2009 (N = 21,310) |
2011/2012 (N = 42,970) |
p 1 | ||
|---|---|---|---|---|---|
| Sample N | Weighted % | Sample N | Weighted % | ||
| Age | 0.0081 | ||||
| 18–25 | 2967 | 13.5 | 5952 | 13.6 | |
| 26–29 | 1464 | 7.3 | 3169 | 6.9 | |
| 30–39 | 3959 | 17.1 | 7920 | 17.0 | |
| 40–49 | 4128 | 18.6 | 7713 | 17.0 | |
| 50–64 | 5099 | 25.0 | 10,270 | 25.4 | |
| 65–74 | 2037 | 9.9 | 4554 | 11.3 | |
| 75+ | 1656 | 8.6 | 3392 | 8.9 | |
| Gender | 0.4605 | ||||
| Male | 10,195 | 49.3 | 20,651 | 49.1 | |
| Female | 11,115 | 50.7 | 22,319 | 50.9 | |
| Race/Ethnicity | 0.1241 | ||||
| Non-Hispanic white | 10,178 | 69.9 | 19,691 | 68.6 | |
| Non-Hispanic black | 3743 | 10.3 | 7698 | 10.2 | |
| Hispanic | 5364 | 13.2 | 11,248 | 14.0 | |
| Other | 2025 | 6.6 | 4333 | 7.2 | |
| Family income | 0.6893 | ||||
| Low income | 7155 | 25.4 | 15,404 | 25.9 | |
| Middle income | 7095 | 31.9 | 13,783 | 31.6 | |
| High income | 7060 | 42.8 | 13,783 | 42.5 | |
| Education2 | <.0001 | ||||
| Less than high school | 4600 | 15.4 | 6060 | 13.2 | |
| High school graduate | 6472 | 30.5 | 9606 | 27.8 | |
| Some college | 4849 | 24.5 | 7313 | 26.1 | |
| College graduate or more | 5189 | 29.7 | 8328 | 32.9 | |
| Marital status | 0.2028 | ||||
| Not married | 9631 | 44.1 | 20,411 | 44.8 | |
| Married | 11,679 | 55.9 | 22,559 | 55.2 | |
| Region | 0.8311 | ||||
| Northeast | 3085 | 18.1 | 6530 | 17.7 | |
| Midwest | 4208 | 22.0 | 8243 | 21.6 | |
| South | 8255 | 37.0 | 16,662 | 37.7 | |
| West | 5762 | 23.0 | 11,535 | 23.0 | |
| Residence | 0.0604 | ||||
| Non-MSA | 2989 | 15.7 | 5375 | 14.5 | |
| MSA | 18,321 | 84.3 | 37,595 | 85.5 | |
| Health insurance | 0.0141 | ||||
| Aged <65, any private | 12,548 | 64.0 | 24,235 | 63.3 | |
| Aged <65, uninsured | 5069 | 17.5 | 10,789 | 16.6 | |
| Aged ≥65, any Medicare | 3693 | 18.5 | 7946 | 20.1 | |
| Number of chronic conditions2,3 | 0.8833 | ||||
| 0 | 9432 | 41.8 | 19,512 | 41.7 | |
| 1 | 4552 | 21.9 | 9190 | 22.2 | |
| 2+ | 7323 | 36.3 | 14,261 | 36.1 | |
MSA = metropolitan statistical area.
Wald chi-square test.
Sum to less than total N because of missing values.
Chronic conditions include: high blood pressure, stroke, heart disease, emphysema, high cholesterol, cancer, diabetes, arthritis and asthma.
As shown in Table 2, adults aged ≥65 years had higher rates of almost every preventive service within the past year than adults aged 18–64 years except Pap test, for which the highest rate (65% over the study period) was seen in the younger population with private insurance. Uninsured adults aged 18–64 years had the lowest rate of every service compared to insured adults. Among the preventive services studied, blood pressure check had the highest receipt rate with around 80% in privately insured adults 18–64 years, over 90% among those with Medicare and around 50% in uninsured younger population. Flu vaccination was low in the younger population, while relatively high (around 70%) in the elderly.
Table 2.
Association between survey year and receipt of preventive care, Medical Expenditure Panel Survey 2009, 2011 and 2012.
| Preventive services within the past year | Adjusted prevalence |
Prevalence ratio1 | |
|---|---|---|---|
| 2009 | 2011/2012 | ||
| Any private insurance, aged 18–64 years | |||
| Blood pressure check | 0.79 (0.78–0.80) | 0.81 (0.80–0.82) | 1.03 (1.01–1.05) |
| Cholesterol check | 0.52 (0.50–0.53) | 0.58 (0.57–0.60) | 1.13 (1.09–1.18) |
| Flu vaccination | 0.38 (0.36–0.39) | 0.39 (0.38–0.41) | 1.04 (1.00–1.08) |
| Pap test | 0.67 (0.65–0.69) | 0.65 (0.64–0.67) | 0.98 (0.95–1.01) |
| Mammogram | 0.60 (0.58–0.62) | 0.60 (0.58–0.62) | 1.00 (0.95–1.04) |
| Any colorectal cancer screening | 0.22 (0.20–0.24) | 0.21 (0.19–0.22) | 0.93 (0.83–1.04) |
| Any Medicare, aged 65+ years | |||
| Blood pressure check | 0.90 (0.87–0.92) | 0.92 (0.90–0.93) | 1.02 (0.99–1.05) |
| Cholesterol check | 0.79 (0.76–0.82) | 0.84 (0.81–0.86) | 1.06 (1.01–1.11) |
| Flu vaccination | 0.69 (0.67–0.71) | 0.71 (0.69–0.73) | 1.02 (0.99–1.06) |
| Pap test | 0.55 (0.44–0.66) | 0.50 (0.39–0.60) | 0.89 (0.68–1.18) |
| Mammogram | 0.56 (0.53–0.58) | 0.55 (0.52–0.57) | 0.99 (0.93–1.04) |
| Any colorectal cancer screening | 0.28 (0.25–0.31) | 0.26 (0.24–0.28) | 0.92 (0.81–1.03) |
| No insurance, aged 18–64 years | |||
| Blood pressure check | 0.47 (0.44–0.49) | 0.49 (0.47–0.51) | 1.05 (0.98–1.12) |
| Cholesterol check | 0.24 (0.22–0.26) | 0.26 (0.24–0.28) | 1.10 (0.97–1.24) |
| Flu vaccination | 0.16 (0.14–0.17) | 0.16 (0.14–0.17) | 1.01 (0.90–1.14) |
| Pap test | 0.42 (0.39–0.44) | 0.41 (0.38–0.44) | 0.99 (0.90–1.09) |
| Mammogram | 0.29 (0.25–0.32) | 0.30 (0.27–0.34) | 1.05 (0.91–1.21) |
| Any colorectal cancer screening | 0.08 (0.06–0.10) | 0.09 (0.08–0.12) | 1.16 (0.85–1.59) |
For each service, only populations with age range consistent with USPSTF recommended age range were included.
Models were adjusted for age, sex, race/ethnicity, education, marriage status, region, residence and number of chronic diseases.
Year 2009 was the reference group.
The majority of the changes in preventive services use between pre and post-ACA (2009 vs. 2011/2012) occurred among adults aged 18–64 years with private insurance, where the rate increased for blood pressure check (PR = 1.03, CI = 1.01–1.05), cholesterol check (PR = 1.13, CI=1.09–1.18) and flu vaccination (PR=1.04, CI=1.00–1.08). An increase in the use of cholesterol check was also seen among adults aged ≥65 years with Medicare (PR=1.06, CI=1.01–1.11). No change in preventive services use was observed for the uninsured younger population.
Because the changes in preventive services use were primarily seen in privately insured adults aged 18–64 years, we examined family income and the number of chronic conditions further in this group only. A statistically significant interaction between survey year and family income was identified for flu vaccination, with the increase (PR = 1.09, CI = 1.03–1.15) only seen in high income population (Table 3). The number of chronic conditions was also found to be a modifier for the relationship of survey year and receipt of flu vaccination: the receipt increased in individuals with chronic conditions, but did not change in those without chronic conditions (Table 3). Although we did not observe a change in receipt of mammogram overall, in the stratified analysis we found that use of mammography increased in individuals without chronic conditions (PR = 1.10, CI = 1.00–1.20). Among individuals with 2 or more chronic conditions, use of mammography declined (PR = 0.94, CI = 0.88–1.00), although the association was of borderline statistical significance.
Table 3.
Association between survey year and receipt of preventive care by family income or number of chronic conditions, adults aged 18–64 years with any private insurance, Medical Expenditure Panel Survey 2009, 2011 and 2012.
| Preventive services within the past year | ||||
|---|---|---|---|---|
| Family income | Low income | Middle income | High income | p interaction |
|
| ||||
| Blood pressure check | 1.06 (1.01–1.11) | 1.03 (1.00–1.07) | 1.02 (0.99–1.04) | 0.3910 |
| Cholesterol check | 1.14 (1.01–1.28) | 1.14 (1.07–1.23) | 1.13 (1.07–1.20) | 0.9219 |
| Flu vaccination | 0.94 (0.84–1.05) | 0.99 (0.91–1.06) | 1.09 (1.03–1.15) | 0.0085 |
| Pap test | 1.02 (0.95–1.10) | 1.00 (0.94–1.07) | 0.95 (0.91–1.00) | 0.1717 |
| Mammogram | 0.95 (0.82–1.09) | 1.08 (0.99–1.17) | 0.98 (0.93–1.04) | 0.1217 |
| Any colorectal cancer screening | 0.86 (0.63–1.19) | 1.07 (0.88–1.30) | 0.89 (0.77–1.02) | 0.2032 |
| Number of chronic conditions | None | One | Two or more | p interaction |
|
| ||||
| Blood pressure check | 1.03 (1.01–1.06) | 1.00 (0.98–1.03) | 1.03 (1.00–1.06) | 0.3270 |
| Cholesterol check | 1.12 (1.04–1.21) | 1.14 (1.06–1.22) | 1.14 (1.07–1.20) | 0.0855 |
| Flu vaccination | 0.98 (0.91–1.05) | 1.08 (1.00–1.17) | 1.07 (1.01–1.12) | 0.0307 |
| Pap test | 1.00 (0.96–1.05) | 0.94 (0.88–1.00) | 0.97 (0.91–1.03) | 0.2551 |
| Mammogram | 1.10 (1.00–1.20) | 1.00 (0.92–1.09) | 0.94 (0.88–1.00) | 0.0215 |
| Any colorectal cancer screening | 0.95 (0.71–1.28) | 0.95 (0.78–1.17) | 0.90 (0.79–1.02) | 0.7178 |
For each service, only populations with age range consistent with USPSTF recommended age range were included.
Models were adjusted for age, sex, race/ethnicity, education, marriage status, region, residence and number of chronic diseases.
Prevalence ratios and 95% confidence intervals using year 2009 as the reference group were presented.
Family income levels were defined as: low income = less than 200% poverty line; middle income = 200% to less than 400% poverty line; high income = greater than or equal to 400% poverty line.
Discussion
Our findings suggest that the rate of uptake increased for some, but not all, recommended preventive services in which cost-sharing had been eliminated for many health plans during the first 2 years after implementation of the ACA provision. Specifically, we found that after the elimination of cost-sharing requirements began in 2010, the receipt of blood pressure checks, cholesterol checks and flu vaccination significantly increased from 2009 to 2011/2012, primarily among privately insured populations aged 18–64 years. Few changes were observed for breast, cervical, and colorectal cancer screening services.
Although some health plans already covered certain preventive services without any cost-sharing before the ACA, the majority of Americans were enrolled in the plans that did not (Burke and Simmons, 2014). Assuming that insurance beneficiaries are aware of the ACA provisions of eliminating cost-sharing for preventive services, our hypothesis was that they would be more likely to seek or consent to these services because of the removal of the financial barrier. Our findings for blood pressure check, cholesterol check, and flu vaccination are consistent with the hypothesis. The increase in these services was confined to insured people, suggesting a positive effect of the ACA provision. Lack of change in preventive services use in the uninsured population would be expected because changes in cost-sharing would not remove any financial barriers to care.
Among the insured, the increase in receipt of these three services was primarily seen among privately insured adults younger than 65 years, suggesting that younger adults benefit the most from eliminating the cost-sharing requirement for these services. Adults ages ≥65 years are more likely to be regular users of health care, compared with the younger adults (Agency for Healthcare Research and Quality, 2014b). In fact, the receipt rate of these three preventive services among those aged ≥65 years old was much higher than those aged 18–64 years at baseline (90% vs. 72% for blood pressure check; 79% vs. 45% for cholesterol check; and 69% vs. 33% for flu vaccination in 2009, respectively), leaving less room for improvements or possibly creating a ceiling effect for evaluating the impact of the ACA provisions. Our generally null findings among the elderly were consistent with results from a recently study in Medicare population (Jensen et al., 2015).
In the stratified analysis, we found that the increase in flu vaccination occurred in only people with chronic conditions. The promotion of flu vaccination has been challenged by the misconceptions of the vaccines (e.g. a flu shot can give you the flu) (Centers for Disease Control and Prevention, 2014) and concerns about side-effects (Canning et al., 2005) in the general population. However, as a high-risk population, those with chronic conditions may be more willing to receive the vaccine and their care providers may recommend it more strongly to avoid severe complications from flu. We found that the increase in flu vaccination was specifically seen in the high income group, which may be related to better health literacy in those with higher socioeconomic status (Bennett et al., 2009).
Blood pressure check, cholesterol check, and flu vaccination are mainly provided in physicians' offices especially during primary care office visit. They are also increasingly provided outside of medical care settings such as drug stores, grocery stores and work sites. Unfortunately we do not have information on where the respondents received these services. However we examined the number of physician visits (office-based visits and outpatient visits) and found no change during the study period among our study population (data not shown), suggesting that the increased uptake of these services likely happened at non-medical care settings or as an additional service during the physician's office visit.
Generally, we did not observe an increase in the utilization of cancer screening services after adjusting for potential confounding variables. This null finding is somewhat inconsistent with prior studies (Goodwin and Anderson, 2012; Meeker et al., 2011; Solanki et al., 2000; Trivedi et al., 2008) and likely due to multiple factors. First, we only have data for 2 years post-ACA implementation while a longer time may be required for changes in cancer screening; recommendations for screening intervals are longer than 1 year for most tests. Second, the change of guideline recommendations to less frequent screening and later starting age for cervical cancer (US Preventive Services Task Force, 2014; Saslow et al., 2012; Sawaya, 2009) and breast cancer (US Preventive Services Task Force, 2009) around the same time period may have in part offset any impact of the ACA provision. Third, cancer screening services are typically more complicated, more invasive, time-consuming, require more resources, and generally performed by specialists rather than primary care providers. Therefore, receipt of cancer screening may be more influenced by other non-financial barriers such as geographic isolation, difficulty taking time off from work, limited health literacy, availability of specialty services and cultural attitudes, than other preventive services. Last, although the ACA provision eliminates cost-sharing for cancer screening, many asymptomatic adults may still face unexpected expenses when a pre-cancerous lesion or early stage tumor is identified and follow-up procedures are required (Pollitz et al., 2013). For example, a deductible or co-payment could be charged for polyp removal during colonoscopies and colonoscopies following a positive fecal occult blood test (Green et al., 2014). A clarification issued by the federal government in 2013 partly addressed this issue for private insurance (Centers for Medicare & Medicaid Services, 2013), but this mainly is still an unresolved issue for Medicare (Green et al., 2014). Despite the primarily null findings for cancer screenings, in the stratified analysis, we observed that the receipt of mammogram increased in adults without chronic conditions, suggesting a potentially beneficial effect from the elimination of cost-sharing among certain subpopulations. Nevertheless, evaluation of the receipt of cancer screening services in relation to the implementation of the ACA will be an important area for further monitoring and investigation.
Despite the strengths of using nationally representative data in a large sample to assess the impact of elimination of cost-sharing requirements under the ACA on preventive services use for multiple services in age appropriate populations by type of health insurance, there were some limitations with our study. The frequencies of our outcome variables do not necessarily match the recommended frequency in all available guidelines, in part, because guidelines vary among different organizations. However, we chose to use the frequency of ≤1 year in our analysis to detect changes associated with the ACA using the most recently available MEPS data only 2 years after the implementation of the new policy. We were not able to evaluate changes in receipt of some preventive services covered by the ACA provisions, such as healthy diet counseling, screening for HIV, depression screening and tobacco-use screening, because these data were not available in the MEPS for all study years.
Information about receipt of preventive services in this study was based on self-reported survey responses and subject to recall error (Rauscher et al., 2008), although any recall errors would be similar over our study period, and not affect our analysis of changes over time. For the privately insured, we did not know if their health plans were grandfathered (grandfathered plans were not subject to the ACA provision). Because the elimination of cost-sharing is not universal for the privately insured, any associations are likely understated in this population. In addition, we were unable to consider factors other than cancer history to identify adults for whom screening within the past year would not have been recommended. Lastly, given our use of cross-sectional data, our analysis could not capture changes in preventive service utilization as a direct result of the ACA. Although the economic recovery during the same period may have also contributed to the observed increase in receipt of preventive services in the privately insured, we did not observe significant increases in receipt of preventive services in the uninsured.
In summary, we observed that the receipt of multiple preventive services, but not cancer screening services, significantly increased after the implementation of the ACA requirements eliminating cost-sharing for preventive services, with the increase largely confined to privately insured persons aged 18–64 years. These early observations, along with findings from other recent studies on the dependent coverage expansion provision (Han et al., 2014; Lau et al., 2014), suggest some positive benefits of the provisions despite limited overall awareness and understanding of the ACA during the early days (The Henry J. Kaiser Family Foundation, 2013; Gross et al., 2012; Long et al., 2014). Moving forward, research is needed to continue to monitor access to preventive services covered by the ACA provisions. If and to what extent the changes in access to care due to the ACA lead to changes in health outcomes and cost of care merit future investigation. Additional research could also examine the impact of cost-sharing elimination among vulnerable populations, such as individuals with low socioeconomic status and cancer survivors or other individuals with chronic conditions.
Appendix A
Appendix Table.
Guideline recommendations and questionnaire items for preventive services.
| Preventive service | Recommendation (year) 1 | Grade | Participants in analysis | Questionnaire item |
|---|---|---|---|---|
| Blood pressure screening | The USPSTF recommends screening for high blood pressure in adults age 18 years and older. (2007) | A | Adults aged ≥ 18 years | About how long has it been since (PERSON) had (PERSON)'s blood pressure checked by a doctor, nurse or other health professional? 2 |
| Cholesterol screening | The USPSTF strongly recommends screening men age 35 years and older for lipid disorders. (2008) | A | All men aged ≥ 35 years; Men aged 20–24 years and women aged ≥ 20 years if with history of heart disease or its known risk factors (i.e. smoking, diabetes, high blood pressure and obesity) | About how long has it been since (PERSON) had (PERSON)'s blood cholesterol checked by a doctor or other health professional? 2 |
| The USPSTF recommends screening men ages 20 to 35 years for lipid disorders if they are at increased risk for coronary heart disease. (2008) | B | |||
| The USPSTF strongly recommends screening women age 45 years and older for lipid disorders if they are at increased risk for coronary heart disease. (2008) | A | |||
| The USPSTF recommends screening women ages 20 to 45 years for lipid disorders if they are at increased risk for coronary heart disease. (2008) | B | |||
| Influenza Vaccine | ACIP recommends routine annual influenza vaccination for all persons aged ≥6 months who do not have contraindications. (2009) | Adults aged ≥ 18 years | About how long has it been since (PERSON) had a flu vaccination (shot or nasal spray)? 2 | |
| Cervical cancer screening | The USPSTF recommends screening for cervical cancer in women ages 21 to 65 years with cytology (Pap smear) every 3 years or, for women ages 30 to 65 years who want to lengthen the screening interval, screening with a combination of cytology and human papillomavirus (HPV) testing every 5 years. (2012) | A | Women aged 21–65 years | When did (PERSON) have (PERSON)'s most recent Pap test? 2 |
| Breast cancer screening 3 | The USPSTF recommends screening mammography for women, with or without clinical breast examination, every 1 to 2 years for women age 40 years and older. (2002) | B | Women aged ≥ 40 years | When did (PERSON) have (PERSON)'s most recent mammogram? 2 |
| Colorectal cancer screening | The USPSTF recommends screening for colorectal cancer using fecal occult blood testing, sigmoidoscopy, or colonoscopy in adults beginning at age 50 years and continuing until age 75 years. (2008) | A | Adults aged 50–75 years | When did (PERSON) do (PERSON)'s most recent blood stool test using a home kit? 4 |
| When did (PERSON) have (PERSON)'s most recent colonoscopy? 4 | ||||
| When did (PERSON) have (PERSON)'s most recent sigmoidoscopy? 4 |
USPSTF = US Preventive Services Task Force; ACIP = Advisory Committee on Immunization Practices;
Cited from: USPSTF A and B Recommendations at http://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-a-and-b-recommendations/#dag and Influenza ACIP Vaccine Recommendations at http://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/flu.html.
The answer options are: within past year; within past 2 years; within past 3 years; within past 5 years; more than 5 years; never; refuse; do not know.
The Department of Health and Human Services, in implementing the Affordable Care Act under the standard it sets out in revised Section 2713(a)(5) of the Public Health Service Act, utilizes the 2002 recommendation on breast cancer screening of the USPSTF.
The answer options are: within past year; within past 2 years; within past 3 years; within past 5 years; within past 10 years; more than 10 years; never; refuse; do not know.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institutes of Health or the Centers for Disease Control and Prevention.
Conflict of interest statement The authors declare that there are no conflicts of interests.
References
- Agency for Healthcare Research and Quality . MEPS-HC-155 2012 Full Year Consolidate Data File Documentation. Rockville, MD: 2014a. pp. C111–C122. [Google Scholar]
- Agency for Healthcare Research and Quality Table 1: Usual Source of Health Care and Selected Population Characteristics, United States, 2011. Medical Expenditure Panel Survey Household Component Data. Generated Interactively (September 30, 2014) 2014b [Google Scholar]
- Baicker K, Goldman D. Patient cost-sharing and healthcare spending growth. J. Econ. Perspect. 2011;25:47–68. doi: 10.1257/jep.25.2.47. [DOI] [PubMed] [Google Scholar]
- Bennett IM, Chen J, Soroui JS, White S. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann. Fam. Med. 2009;7:204–211. doi: 10.1370/afm.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am. J. Epidemiol. 2010;171:618–623. doi: 10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- Burke A, Simmons A. ASPE Issue Brief: Increased Coverage of Preventive Services With Zero Cost Sharing Under the Affordable Care Act. 2014. [Google Scholar]
- Canning HS, Phillips J, Allsup S. Health care worker beliefs about influenza vaccine and reasons for non-vaccination–a cross-sectional survey. J. Clin. Nurs. 2005;14:922–925. doi: 10.1111/j.1365-2702.2005.01190.x. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . Misconceptions About Seasonal Flu and Flu Vaccines. 2014. [Google Scholar]
- Centers for Medicare, Medicaid Services . Affordable Care Act Implementation FAQs–Set 12. 2013. The Center for Consumer Information & Insurance Oversight. [Google Scholar]
- Damiani G, Federico B, Bianchi CB, Ronconi A, Basso D, Fiorenza S, Sassi F. Socio-economic status and prevention of cardiovascular disease in Italy: evidence from a national health survey. Eur. J. Pub. Health. 2011;21:591–596. doi: 10.1093/eurpub/ckq075. [DOI] [PubMed] [Google Scholar]
- Fox JB, Shaw FE. Clinical preventive services coverage and the Affordable Care Act. Am. J. Public Health. 2015;105:e7–e10. doi: 10.2105/AJPH.2014.302289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin SM, Anderson GF. Effect of cost-sharing reductions on preventive service use among Medicare fee-for-service beneficiaries. Medicare Medicaid Res. Rev. 2012;2 doi: 10.5600/mmrr.002.01.a03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green BB, Coronado GD, Devoe JE, Allison J. Navigating the murky waters of colorectal cancer screening and health reform. Am. J. Public Health. 2014;104:982–986. doi: 10.2105/AJPH.2014.301877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross W, Stark T, Krosnick J, Pasek J, Sood G, Tompson T, Agiesta J, Junius D. Americans' Attitudes Toward the Affordable Care Act: Would Better Public Understanding Increase or Decrease Favorability? Robert Wood Johnson Foundation Inc; Princeton, NJ: 2012. [Google Scholar]
- Guy GP., Jr. The effects of cost sharing on access to care among childless adults. Health Serv. Res. 2010;45:1720–1739. doi: 10.1111/j.1475-6773.2010.01162.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han X, Yabroff KR, Robbins AS, Zheng Z, Jemal A. Dependent coverage and use of preventive care under the Affordable Care Act. N. Engl. J. Med. 2014;371:2341–2342. doi: 10.1056/NEJMc1406586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoeck S, van der Heyden J, Geerts J, Van Hal G. Preventive care use among the Belgian elderly population: does socio-economic status matter? Int. J. Environ. Res. Public Health. 2014;11:355–372. doi: 10.3390/ijerph110100355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen GA, Salloum RG, Hu J, Ferdows NB, Tarraf W. A slow start: use of preventive services among seniors following the Affordable Care Act's enhancement of Medicare benefits in the U.S. Prev. Med. 2015;76:37–42. doi: 10.1016/j.ypmed.2015.03.023. [DOI] [PubMed] [Google Scholar]
- Lau JS, Adams SH, Park MJ, Boscardin WJ, Irwin CE., Jr. Improvement in preventive care of young adults after the Affordable Care Act: the Affordable Care Act is helping. JAMA Pediatr. 2014;168:1101–1106. doi: 10.1001/jamapediatrics.2014.1691. [DOI] [PubMed] [Google Scholar]
- Long SK, Kenney GM, Zuckerman S, Goin DE, Wissoker D, Blavin F, Blumberg LJ, Clemans-Cope L, Holahan J, et al. The health reform monitoring survey: addressing data gaps to provide timely insights into the affordable care act. Health Aff. (Millwood) 2014;33:161–167. doi: 10.1377/hlthaff.2013.0934. [DOI] [PubMed] [Google Scholar]
- Meeker D, Joyce GF, Malkin J, Teutsch SM, Haddix AC, Goldman DP. Coverage and preventive screening. Health Serv. Res. 2011;46:173–184. doi: 10.1111/j.1475-6773.2010.01188.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the Secretary, Department of Defense TRICARE: elimination of co-payments for authorized preventive services for certain TRICARE Standard beneficiaries. Final rule. Fed. Regist. 2011;76:81368–81370. [PubMed] [Google Scholar]
- Pollitz K, Lucia K, Keith K, Smith R, Doroshenk M, Wolf H, Weber T. Coverage of Colonoscopies Under the Affordable Care Act's Prevention Benefit, The Henry J. Kaiser Family Foundation, American Cancer Society, and National Colorectal Cancer Roundtable (September 2012) 2013. [Google Scholar]
- Rauscher GH, Johnson TP, Cho YI, Walk JA. Accuracy of self-reported cancer-screening histories: a meta-analysis. Cancer Epidemiol. Biomarkers Prev. 2008;17:748–757. doi: 10.1158/1055-9965.EPI-07-2629. [DOI] [PubMed] [Google Scholar]
- Rezayatmand R, Pavlova M, Groot W. The impact of out-of-pocket payments on prevention and health-related lifestyle: a systematic literature review. Eur. J. Pub. Health. 2013;23:74–79. doi: 10.1093/eurpub/cks034. [DOI] [PubMed] [Google Scholar]
- Sabatino SA, Lawrence B, Elder R, Mercer SL, Wilson KM, DeVinney B, Melillo S, Carvalho M, Taplin S, et al. Effectiveness of interventions to increase screening for breast, cervical, and colorectal cancers: nine updated systematic reviews for the guide to community preventive services. Am. J. Prev. Med. 2012;43:97–118. doi: 10.1016/j.amepre.2012.04.009. [DOI] [PubMed] [Google Scholar]
- Sambamoorthi U, McAlpine DD. Racial, ethnic, socioeconomic, and access disparities in the use of preventive services among women. Prev. Med. 2003;37:475–484. doi: 10.1016/s0091-7435(03)00172-5. [DOI] [PubMed] [Google Scholar]
- Saslow D, Solomon D, Lawson HW, Killackey M, Kulasingam SL, Cain J, Garcia FA, Moriarty AT, Waxman AG, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J. Clin. 2012;62:147–172. doi: 10.3322/caac.21139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawaya GF. Cervical-cancer screening–new guidelines and the balance between benefits and harms. N. Engl. J. Med. 2009;361:2503–2505. doi: 10.1056/NEJMp0911380. [DOI] [PubMed] [Google Scholar]
- Solanki G, Schauffler HH. Cost-sharing and the utilization of clinical preventive services. Am. J. Prev. Med. 1999;17:127–133. doi: 10.1016/s0749-3797(99)00057-4. [DOI] [PubMed] [Google Scholar]
- Solanki G, Schauffler HH, Miller LS. The direct and indirect effects of cost-sharing on the use of preventive services. Health Serv. Res. 2000;34:1331–1350. [PMC free article] [PubMed] [Google Scholar]
- The Henry J. Kaiser Family Foundation . Kaiser Health Tracking Poll (March 2013) 2013. [Google Scholar]
- Trivedi AN, Rakowski W, Ayanian JZ. Effect of cost sharing on screening mammography in Medicare health plans. N. Engl. J. Med. 2008;358:375–383. doi: 10.1056/NEJMsa070929. [DOI] [PubMed] [Google Scholar]
- US Preventive Services Task Force Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 2009;151:716–726. doi: 10.7326/0003-4819-151-10-200911170-00008. W-236. [DOI] [PubMed] [Google Scholar]
- US Preventive Services Task Force . Screening for Cervical Cancer. 2014. [Google Scholar]
- Washington State Office of the Insurance Commissioner . What is a Non-Grandfathered Plan? 2014. [Google Scholar]
- Wilensky SE, Gray EA. Existing Medicaid beneficiaries left off the Affordable Care Act's prevention bandwagon. Health Aff. (Millwood) 2013;32:1188–1195. doi: 10.1377/hlthaff.2013.0224. [DOI] [PubMed] [Google Scholar]