Abstract
Laparoscopic surgery has generated a revolution in operative medicine during the past few decades. Although strongly criticized during its early years, minimization of surgical trauma and the benefits of minimization to the patient have been brought to our attention through the efforts and vision of a few pioneers in the recent history of medicine. The German gynecologist Kurt Semm (1927–2003) transformed the use of laparoscopy for diagnostic purposes into a modern therapeutic surgical concept, having performed the first laparoscopic appendectomy, inspiring Erich Mühe and many other surgeons around the world to perform a wide spectrum of procedures by minimally invasive means. Laparoscopic cholecystectomy soon became the gold standard, and various laparoscopic procedures are now preferred over open approaches, in the light of emerging evidence that demonstrates less operative stress, reduced pain, and shorter convalescence. Natural orifice transluminal endoscopic surgery (NOTES) and single-incision laparoscopic surgery (SILS) may be considered further steps toward minimization of surgical trauma, although these methods have not yet been standardized. Laparoscopic surgery with the use of a robotic platform constitutes a promising field of investigation. New technologies are to be considered under the prism of the history of surgery; they seem to be a step toward further minimization of surgical trauma, but not definite therapeutic modalities. Patient safety and medical ethics must be the cornerstone of future investigation and implementation of new techniques.
Keywords: Minimally invasive surgery, Laparoscopic surgery, NOTES, Robotic surgery, SILS
INTRODUCTION
A wide spectrum of gastroenterological diseases require surgical therapy. As early as the 4th century before the Common Era, Hippocrates stated:  οκόσα ϕάρμακα ου'κ ι'η̃ται, σίδηρος ι'η̃ται….,” meaning “What medicines do not heal, the lance will….”1 The history of abdominal surgery demonstrates a magnificent evolution from ancient years to the present. The drastic progress during the past centuries was initiated by the development of anesthetic techniques.2 Another landmark was the recognition of antisepsis and antimicrobial therapy as key components of favorable operative outcomes.3,4 Safe and effective analgesic regimens have largely completed the sum of conditions essential for the operative treatment of surgical diseases.5
οκόσα ϕάρμακα ου'κ ι'η̃ται, σίδηρος ι'η̃ται….,” meaning “What medicines do not heal, the lance will….”1 The history of abdominal surgery demonstrates a magnificent evolution from ancient years to the present. The drastic progress during the past centuries was initiated by the development of anesthetic techniques.2 Another landmark was the recognition of antisepsis and antimicrobial therapy as key components of favorable operative outcomes.3,4 Safe and effective analgesic regimens have largely completed the sum of conditions essential for the operative treatment of surgical diseases.5
Nonetheless, surgery is invasive, per se, subjecting the human body to significant stress, with an impact on a variety of systems, the most important of which are the cardiovascular, respiratory, excretory, and immune systems.6 Consequently, surgical stress affects organ homeostasis, which may be well tolerated by fit subjects, but poses significant risks to frail patients.7 Irrespective of physical status, surgery causes pain, which may deeply affect the human psyche in combination with the patient's perspectives and fears about the invasive nature of the procedure.8–10
It soon became clear that small incisions induced less operative stress. While anesthesia, analgesia, and antisepsis have provided a stable foundation for general surgery, for many years, investigators have struggled to reduce the size of incisions for diagnostic purposes and, from the 1980s to the present, with therapeutic intent. Efforts to explore human body cavities commenced in the early classical period of ancient Greece.11 Georg Kelling was the first to perform a laparoscopy with a cystoscope, but Hans Christian Jacobaeus, an internist from Stockholm, performed extensive research on laparoscopy and popularized the method. His work included primarily patients with ascites, which was evacuated to allow air insufflation and direct visualization with a cystoscope.12
EVOLUTION OF MINIMALLY INVASIVE SURGERY
During the first decades of the 20th century, laparoscopy was a diagnostic tool for abdominal pathologies. The laparoscopic concept crossed the borderline between diagnostic medicine and therapeutic surgery, thanks to a pioneer surgeon, the gynecologist Professor Kurt Semm (1927–2003).13 Semm received an abundance of criticism for his laparoscopic techniques, even from his fellow gynecologists, and was insulted both personally and scientifically.14,15 Sporadic cases of bowel injury were the impetus for the criticism and have constituted an impediment for the dissemination of his techniques. Nevertheless, Semm had some aces up his sleeve for the defense of surgical laparoscopy. His family owned a manufacturing company and implemented Semm's ideas in a short time, constructing surgical equipment for laparoscopic purposes.16 Furthermore, he had been performing research on operative laparoscopy for many years,17 and he stood up for what he believed, despite the onslaught of criticism. Holding lectures around the world, he found supporters, mainly across the Atlantic, and the advantages of laparoscopic surgery started to be acknowledged. Professor Erich Mühe performed the first laparoscopic cholecystectomy in 1985, although Philippe Mouret has frequently been cited as having performed the first procedure.18,19 Mühe had worked as an assistant in Erlangen, a university center in Germany with wide experience in endoscopic procedures, and had practiced rectosigmoid polypectomy with endoscopic instruments since 1977.20 Fascinated by laparoscopy and the work of Semm, he developed a direct visualization endoscope (Figure 1), which he used for laparoscopic cholecystectomy. His pioneering work was rejected by the German Surgical Society, and it was recognized by the Society only after widespread use of laparoscopic cholecystectomy by his French colleagues. It was not until 1997 that he was acknowledged for his pioneering method of cholecystectomy.18 The vision of a few surgeons, although opposed by most of the medical community, paved the way to minimally invasive surgery.
Figure 1.
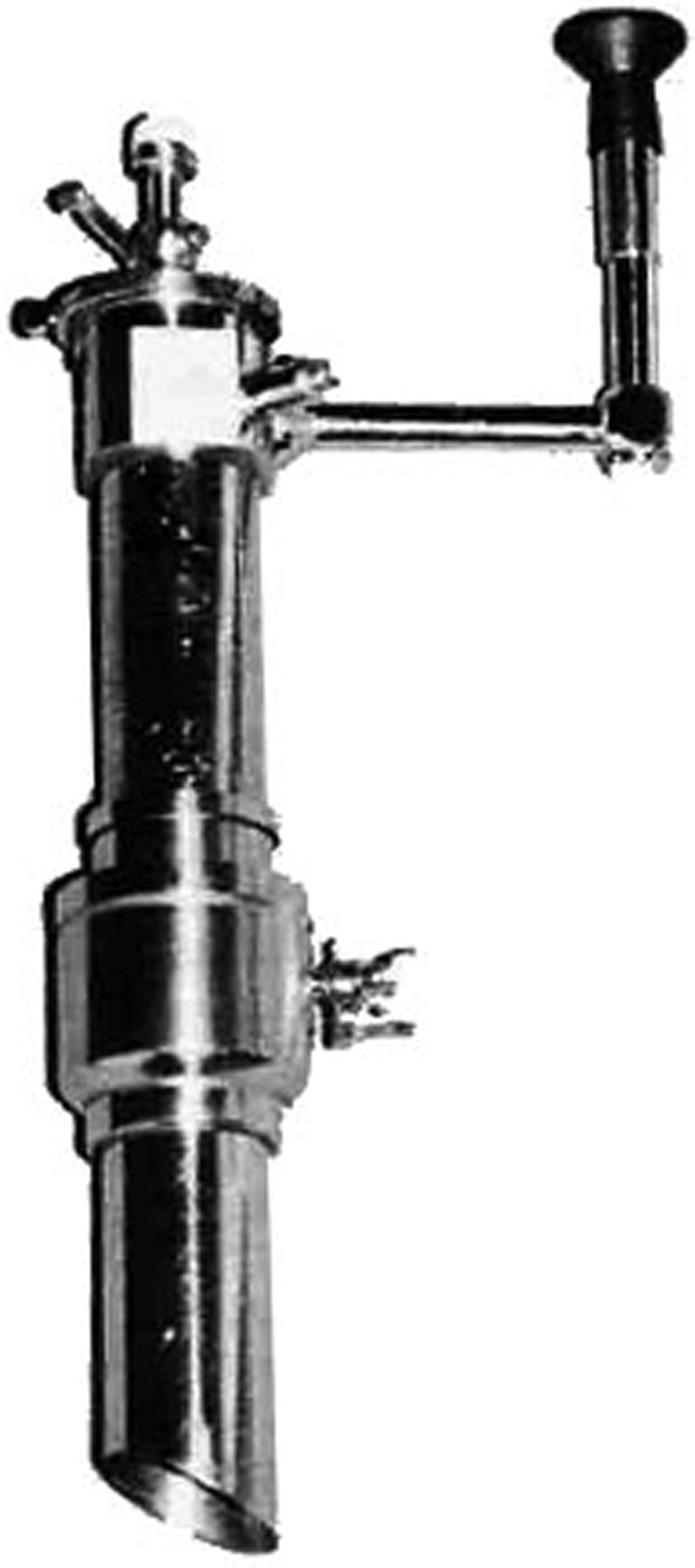
Mühe's endoscope for laparoscopic cholecystectomy.
Laparoscopic cholecystectomy rapidly became the procedure of choice throughout the world.21 Fundoplication, adrenalectomy, groin and abdominal wall hernia repair, and colon surgery were introduced in the 1990s, and case reports of splenectomy, pancreatectomy, gastrectomy, and hepatectomy were sporadically published. Most of these operations were performed for benign conditions, because they had not been technically validated, and their oncological effectiveness was poorly defined. After 2000, initial observations claiming higher abdominal wall recurrence rates of colon adenocarcinomas were disproved.22 At the same time, the first long-term results of randomized trials on laparoscopic colon resection for cancer became available,23–25 which provided a further impetus for minimally invasive techniques. The establishment of laparoscopic centers throughout the world and the development of minimally invasive training curricula signaled the laparoscopic era. The procedures are now performed in operating rooms specifically designed for laparoscopy (Figure 2).
Figure 2.
A modern operating room for laparoscopic surgery.
ROBOTICS, NOTES, AND SILS
Although the use of basic laparoscopic techniques was spreading throughout the world, the laparoscopic scientific community kept seeking ways to obviate the limitations associated with the procedures, such as the lack of tactile feedback, the 2-dimensional view, and the limited degrees of freedom of the laparoscopic instruments. Robotic surgical platforms have been available since the late 1990s, and today these are represented by the only commercially available platform, the da Vinci System (Intuitive Surgical, Sunnyvale, California). Robotic platforms are manipulated by a surgeon situated distant from the surgical field, who uses a 3-dimensional laparoscopic view and special “chopstick” instruments (Figure 3). The hardware filters the surgeon's hand motions and is thought to provide increased precision and enhanced dexterity, allowing for multiple degrees of freedom, similar to the human wrist.24 Nevertheless, robotic platforms remain extremely costly, and their advantages currently seem to be clinically significant only in a subset of surgical procedures, such as rectal resection.26
Figure 3.
The da Vinci robotic platform.
Thanks to the works of Buess and colleagues,27 as well as that of others across the world, transanal microsurgery has provided an incentive for the so-called natural orifice transluminal endoscopic surgery (NOTES). The first case of transoral cholecystectomy in a human was published in 2007.28 Since then, cases and patient series of appendectomy, sleeve gastrectomy, splenectomy, and other procedures performed using the NOTES concept have been published. More important, transesophageal sphincterotomy for esophageal achalasia seems to provide clinically acceptable outcomes.29 It is clear that these techniques have not been standardized yet and are being performed in specialized centers.
Laparoscopic surgery through a single incision (SILS) has drawn the attention of the surgical community as an alternative to NOTES. Because single-incision procedures may also be performed with conventional laparoscopic instrumentation, their use has increased rapidly. Cholecystectomy, appendectomy, sleeve gastrectomy, splenectomy, and other procedures may be performed with the SILS method in selected patients.30–33 The clinical advantages of SILS have not been well established, and there is speculation about an increased incidence of biliary complications and incisional hernias.34–36
FUTURE PERSPECTIVES
In reviewing the history of minimally invasive surgery from its early years, it becomes evident that it is an evolving, vital field of operative medicine. NOTES, SILS, and robotic surgery do not constitute techniques, rather they are concepts. They are thus to be regarded as transitions from laparoscopic surgery to as yet unknown fields of minimally invasive therapeutic modalities. Current research projects seek to enhance surgical motion features through laparoscopic ports. A recently developed robotic platform combines the single-incision concept with robotic surgery, allowing for independent traction, manipulation, and dissection through a single polycerated tool (Figure 4).37 The STIFF-FLOP (STIFFness controllable Flexible and Learnable Manipulator for surgical OPerations) project, a European initiative funded by public, scientific, and private sectors, is seeking to create an articulating cognitive robotic arm that can stiffen its parts, depending on the situation, similar to the octopus arm.38 Further research projects around the world are focusing on the development of robotic platforms with controlled independence that can be applied in various surgical situations.
Figure 4.
Single-incision robotic platform.
As a scientific community, we have the obligation to learn from the past. From the history of laparoscopic surgery, the following must be considered when approaching a new technology or technique:
Pioneers of laparoscopic surgery were not only surgeons, but also internists and gastroenterologists. An interdisciplinary approach must therefore be implemented to the extent possible, disregarding specialty frontiers, to enhance productive creativity and technical innovation.39
Surgeons who developed and improved laparoscopic surgery were not accepted in their home countries and within their own disciplines. This rejection reminds one of the biblical saying “no prophet is accepted in his own country” (Luke 4:22). Laparoscopic techniques still have not been completely embraced by general surgeons, despite the established advantages in a wide spectrum of these procedures. Minimally invasive techniques must be incorporated further into surgical practice; otherwise, a new surgical specialty may arise.
Laparoscopic techniques emerged from gastroenterologic procedures performed with endoscopic instruments. With the introduction of NOTES, the paths of surgery and gastroenterology have met again, one hopes in a productive way.
Biliary injuries occurred at a higher incidence in the early years of laparoscopic cholecystectomy, as compared to those that occurred in open surgery.40 Semm's bowel injuries have been a drawback for the acceptance of the laparoscopic concept by the surgical community. At that time, laparoscopic surgery was considered an unethical dangerous practice. Today, the advantages of laparoscopic surgery are indisputable. Future research should be founded on patient safety and ethical principles. It would not be prudent to consider novel surgical developments as techniques that provide optimal cosmetic outcomes or improve the surgeon's comfort, rather than as a step in the evolution of minimally invasive surgery. In this context, it is essential to ensure patient safety and to “first, do no harm.”
Contributor Information
Stavros A. Antoniou, Center for Minimally Invasive Surgery, Hospital Neuwerk, Mönchengladbach, Germany..
George A. Antoniou, Liverpool Vascular and Endovascular Service, Royal Liverpool University Hospital, Liverpool, United Kingdom..
Athanasios I. Antoniou, Department of History and Ethnology, University of Thrace, Komotini, Greece..
Frank-Alexander Granderath, Center for Minimally Invasive Surgery, Hospital Neuwerk, Mönchengladbach, Germany..
References:
- 1. Hippocrates: Aphorisms. 400 BCE. Section 7 No. 87.
- 2. Robinson DH, Toledo AH. Historical development of modern anesthesia. J Invest Surg. 2012;25:141–149. [DOI] [PubMed] [Google Scholar]
- 3. Gariepy TP. The introduction and acceptance of Listerian antisepsis in the United States. J Hist Med Allied Sci. 1994;49:167–206. [DOI] [PubMed] [Google Scholar]
- 4. Nichols RL. Preventing surgical site infections. Clin Med Res. 2004;2:115–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sabatowski R, Schäfer D, Kasper SM, Brunsch H, Radbruch L. Pain treatment: a historical overview. Curr Pharm Des. 2004;10:701–716. [DOI] [PubMed] [Google Scholar]
- 6. Mullins RJ: Shock, electrolytes and fluid. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 18th ed Philadelphia: Saunders Elsevier; 2007:69–112. [Google Scholar]
- 7. Scandrett KG, Zuckerbraun BS, Peitzman AB. Operative risk stratification in the older adult. Surg Clin North Am. 2015;95:149–172. [DOI] [PubMed] [Google Scholar]
- 8. Gan TJ, Habib AS, Miller TE, White W, Apfelbaum JL. Incidence, patient satisfaction, and perceptions of post-surgical pain: results from a US national survey. Curr Med Res Opin. 2014;30:149–160. [DOI] [PubMed] [Google Scholar]
- 9. Waljee J, McGlinn EP, Sears ED, Chung KC. Patient expectations and patient-reported outcomes in surgery: a systematic review. Surgery. 2014;155:799–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Theunissen M, Peters ML, Bruce J, Gramke HF, Marcus MA. Preoperative anxiety and catastrophizing: a systematic review and meta-analysis of the association with chronic postsurgical pain. Clin J Pain. 2012;28:819–841. [DOI] [PubMed] [Google Scholar]
- 11. Antoniou SA, Antoniou GA, Koutras C, Antoniou AI. Endoscopy and laparoscopy: a historical aspect of medical terminology. Surg Endosc. 2012;26:3650–3654. [DOI] [PubMed] [Google Scholar]
- 12. Litynski GS. Laparoscopy: the early attempts: spotlighting Georg Kelling and Hans Christian Jacobaeus. JSLS. 1997;1:83–85. [PMC free article] [PubMed] [Google Scholar]
- 13. Semm K. Pelviscopic appendectomy (in German). Dtsch Med Wochenschr. 1988;113:3–5. [DOI] [PubMed] [Google Scholar]
- 14. Semm K. Robotics and the future of laparoscopy. JSLS. 1999;3:87–88. [PMC free article] [PubMed] [Google Scholar]
- 15. Litynski GS. Kurt Semm and the fight against skepticism: endoscopic hemostasis, laparoscopic appendectomy, and Semm's impact on the “laparoscopic revolution.” JSLS. 1998;2:309–313. [PMC free article] [PubMed] [Google Scholar]
- 16. Mettler L. Historical profile of Kurt Karl Stephan Semm, born March 23, 1927 in Munich, Germany, resident of Tucson, AZ, USA since 1996. JSLS 2003;7:185–188. [PMC free article] [PubMed] [Google Scholar]
- 17. Semm K. Operative pelviscopy. Br Med Bull. 1986;42:284–295. [DOI] [PubMed] [Google Scholar]
- 18. Litynski GS. Erich Mühe and the rejection of laparoscopic cholecystectomy (1985): a surgeon ahead of his time. JSLS. 1998;2:341–346. [PMC free article] [PubMed] [Google Scholar]
- 19. Blum CA, Adams DB. Who did the first laparoscopic cholecystectomy? J Minim Access Surg. 2011;7:165–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Reynolds W., Jr The first laparoscopic cholecystectomy. JSLS. 2001;5:89–94. [PMC free article] [PubMed] [Google Scholar]
- 21. Begos DG, Modlin IM. Laparoscopic cholecystectomy: from gimmick to gold standard. J Clin Gastroenterol. 1994;19:325–330. [DOI] [PubMed] [Google Scholar]
- 22. Kuhry E, Schwenk WF, Gaupset R, Romild U, Bonjer HJ. Long-term results of laparoscopic colorectal cancer resection. Cochrane Database Syst Rev. 2008;16:CD003432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hazebroek EJ; Color Study Group. COLOR: a randomized clinical trial comparing laparoscopic and open resection for colon cancer. Surg Endosc. 2002;16:949–953. [DOI] [PubMed] [Google Scholar]
- 24. Jayne DG, Guillou PJ, Thorpe H, et al. and the Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007;20;:3061–3068. [DOI] [PubMed] [Google Scholar]
- 25. Lacy AM, Delgado S, Castells A, et al. The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann Surg. 2008;248:1–7. [DOI] [PubMed] [Google Scholar]
- 26. Yang Y, Wang F, Zhang P, et al. Robot-assisted versus conventional laparoscopic surgery for colorectal disease, focusing on rectal cancer: a meta-analysis. Ann Surg Oncol. 2012;19:3727–3736. [DOI] [PubMed] [Google Scholar]
- 27. Buess G, Kipfmüller K, Naruhn M, Braunstein S, Junginger T. Endoscopic microsurgery of rectal tumors. Endoscopy. 1987;19(suppl 1):38–42. [DOI] [PubMed] [Google Scholar]
- 28. USGI. USGI announces first NOTES transgastric cholecystectomy procedures, using the USGI Endosurgical Operating System, performed by Dr. Lee Swanstrom at Legacy Hospital in Portland, OR. June 25, 2007. http://web.archive.org/web/20071110233147/http://www.usgimedical.com/pr_transgastric_cholecystectomy.html Accessed January 20, 2015.
- 29. Rieder E, Swanström LL, Perretta S, Lenglinger J, Riegler M, Dunst CM. Intraoperative assessment of esophagogastric junction distensibility during per oral endoscopic myotomy (POEM) for esophageal motility disorders. Surg Endosc. 2013;27:400–405. [DOI] [PubMed] [Google Scholar]
- 30. Arezzo A, Scozzari G, Famiglietti F, Passera R, Morino M. Is single-incision laparoscopic cholecystectomy safe? Results of a systematic review and meta-analysis. Surg Endosc. 2013;27:2293–2304. [DOI] [PubMed] [Google Scholar]
- 31. Antoniou SA, Koch OO, Antoniou GA, et al. Meta-analysis of randomized trials on single-incision laparoscopic versus conventional laparoscopic appendectomy. Am J Surg. 2014;207:613–622. [DOI] [PubMed] [Google Scholar]
- 32. Moreno-Sanz C, Morandeira-Rivas A, Sedano-Vizcaino C, Tenías-Burillo JM, Román-Ortíz C, de la Espada JB. Single-incision laparoscopic bariatric surgery: a systematic review. Surg Obes Relat Dis. 2013;pii:S1550-7289(13)00390-0 [DOI] [PubMed] [Google Scholar]
- 33. Fan Y, Wu SD, Kong J, Su Y, Tian Y, Yu H. Feasibility and safety of single-incision laparoscopic splenectomy: a systematic review. J Surg Res. 2014;186:354–362. [DOI] [PubMed] [Google Scholar]
- 34. Joseph M, Phillips MR, Farrell TM, Rupp CC. Single incision laparoscopic cholecystectomy is associated with a higher bile duct injury rate: a review and a word of caution. Ann Surg. 2012;256:1–6. [DOI] [PubMed] [Google Scholar]
- 35. Garg P, Thakur JD, Singh I, Nain N, Mittal G, Gupta V. A prospective controlled trial comparing single-incision and conventional laparoscopic cholecystectomy: caution before damage control. Surg Laparosc Endosc Percutan Tech. 2012;22:220–225. [DOI] [PubMed] [Google Scholar]
- 36. Milas M, Deve|fgija S, Trkulja V. Single incision versus standard multiport laparoscopic cholecystectomy: up-dated systematic review and meta-analysis of randomized trials. Surgeon. 2014;12:271–289. [DOI] [PubMed] [Google Scholar]
- 37. Tucson Bariatric. Da Vinci Robotic Surgical System. Tucson, AZ: 2015. Available at http://tucsonbariatric.com/procedures/davinci-robotic-surgical-system/ Accessed January 20, 2015.
- 38. STIFF-FLOP. Project Overview. Available at http://www.stiff-flop.eu/the-project/overview Accessed January 20, 2015.
- 39. Antoniou GA, Georgakarakos EI, Antoniou SA, Georgiadis GS. Multidisciplinary care as a holistic approach to the management of vascular disease. Int Angiol. 2014; 33:494–496. [PubMed] [Google Scholar]
- 40. Shea JA, Healey MJ, Berlin JA, Clarke JR, Malet PF, Staroscik RN, Schwartz JS, Williams SV. Mortality and complications associated with laparoscopic cholecystectomy. A meta-analysis. Ann Surg. 1996;224:609–620. [DOI] [PMC free article] [PubMed] [Google Scholar]





