Abstract
Lumbar zygapophyseal joints act as primary pain generators in at least 10–15% of patients with chronic low back pain.
Diagnostic nerve blocks are the most reliable way to diagnose lumbar zygapophyseal joint pain.
IASP recommends either controlled or comparative blocks for diagnosis of zygapophyseal joint pain as there is a significant incidence of false positives with single blocks.
Management should be multimodal comprising education, exercises, analgesics and procedural interventions to achieve functional restoration.
There is a need for further RCTs with standardised diagnostic criteria and outcome measures as well as long-term data to determine the efficacy of radiofrequency denervation.
Introduction
The ‘Pain in Europe’ survey reported that nearly half of their respondents suffered back pain (1). Lumbar Zygapophyseal Joints (LZJ) are one among the various structures of spine that can be a source of back pain. Though LZJ were proposed as a source of pain as early as 1910, their legitimacy remained controversial until the 1970s. Bogduk identified four factors necessary for any structure to be deemed as a cause of back pain. They include nerve supply of the structure; its susceptibility to diseases or injuries; availability of diagnostic techniques of known reliability and validity; and the ability to simulate pain in normal volunteers (2). LZJ fulfil all four criteria. With mounting evidence for legitimacy of pain generation from zygapophyseal joints, it has been accepted that they can either contribute to or even be the primary source of low back pain. This review will summarise existing literature on epidemiology, aetiology, clinical presentation, diagnosis, and multimodal management of LZJ pain.
Applied anatomy
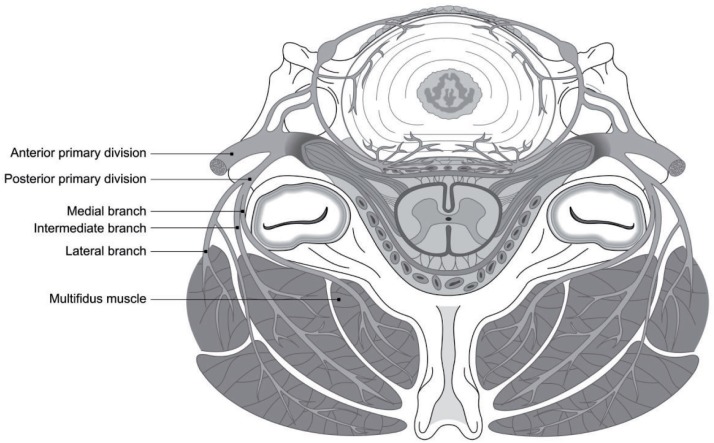
Zygapophyseal joints are the only synovial joints in the spine, with hyaline cartilage overlying subchondral bone, a synovial membrane and a joint capsule; they comprise the postero-lateral articulation between vertebral levels (Figure 1). The joint space has a potential capacity of 1 to 2 ml. Existence of menisci has also been highlighted in numerous publications.
Figure 1.
Facet joints forming the postero-lateral articulation of a spinal segment.
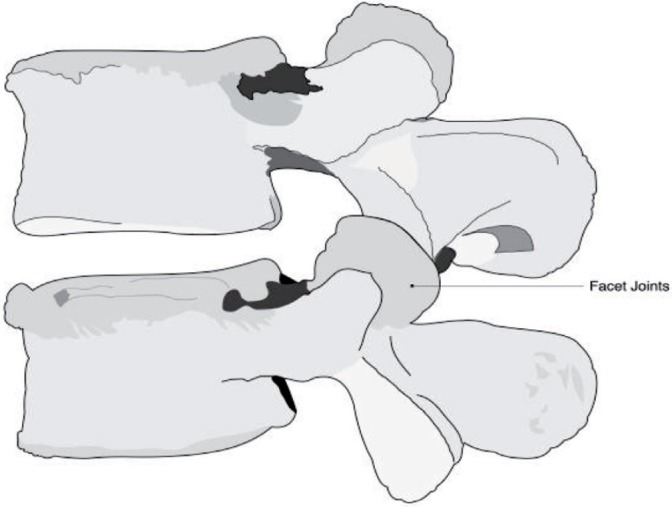
The joint capsule and adjoining structures are richly innervated. Each joint receives a dual nerve supply. The articular branches arise from the medial branch of the posterior primary rami. Thus the L4/L5 zygapophyseal joint receives supply from the L4 medial branch (corresponding segment) and the L3 medial branch (one level above). As articular branches are too small to be accurately targeted, their parent medial branches are commonly targeted for neurotomy as they course across the neck of superior articular process in the groove formed between the transverse process and superior articular process of the vertebrae. The medial branches also innervate the multifidus muscle, the interspinous muscle and ligament, and the periosteum of the neural arch (Figure 2) (3).
Figure 2.
Diagrammatic illustration of medial branches and its course.
Biomechanics
Zygapophyseal joints form part of the posterior element of the spinal segment during load transmission. The percentage of load transferred through posterior elements is dependent on posture, and increases during extension. In normal healthy spinal segments, between 3 and 25 % of segmental load is transmitted via the LZJ while this can increase up to 47% in degenerative joints (4,5). In addition, they stabilise the motion segment during flexion and extension, and are involved in the mechanism of rotational kinematics by restricting axial rotation. Due to their high level of mobility and the large forces influencing them, LZJ can develop significant degenerative changes (5).
Aetiology
While the aetiology of LZJ pain can be identified in a few patients, the majority suffer pain due to repetitive strain and low-grade trauma accumulated during their lifetime (6). Zygapophyseal joints develop osteoarthritis similar to that of all diarthrodial joints. In a cadaveric study of 647 lumbar spines, Eubanks et al found evidence of degenerative changes in LZJ beginning in the third decade, with 60% of adults showing some signs of degeneration by the time they reach age 30 years. Moreover, degeneration appears to steadily increase until the seventh decade when it becomes ubiquitous. They also found the prevalence and degree of degeneration to be greatest at L4-L5 (7). The degenerative changes range from local and diffuse erosions, sclerosis of subchondral bone, facet hypertrophy and apophyseal malalignment to osteophyte formation. There is a paucity of evidence in correlating degenerative changes to the pain experienced (5). Other conditions such as inflammatory arthritides, synovial impingement, meniscoid entrapment, pseudogout and intrafacetal cysts may also affect zygapophyseal joints and cause pain.
Epidemiology
The National Omnibus survey in 1998 reported that 40% of adults in Great Britain suffered from back pain lasting for more than one-day (8). Among the back pain sufferers, there are wide discrepancies in the reported prevalence of LZJ pain. Several reviews highlight the flaws in diagnosing the condition based on history, clinical examination and radiological findings and recommend diagnostic blocks as a reliable and valid way to diagnose LZJ pain.
Using a single set of intra-articular injections or medial branch blocks, the reported prevalence varies from 8 to 94% (9,11). The prevalence rate narrows down from 15 to 45% (12,14) with controlled blocks using saline or comparative blocks with two different local anaesthetics. In addition to false positive rates of single blocks and the positive effects of saline, most of the published prevalence studies exclude patients with neurological signs and symptoms as well as post surgical patients, further confounding the issue. Furthermore, prevalence differs between different age groups. In a North American study with median age of 38 years, Schwarzer reported the prevalence rates as 15%, while his Australian sample with median age of 58 years found a prevalence rate of 40% (12,15). In post surgical patients alone, Manchikanti et al reported a prevalence of 16% using comparative local anaesthetic diagnostic blocks (16). Overall, reviews in this area implicate the LZJ as primary pain generator in 10–15 % of young adult patients with chronic low back pain (LBP) and probably higher in older populations.
Clinical Presentation
Clinicians around the world have put forward various symptoms and signs as predictors of LZJ pain and have attempted to validate them. These include localised low back pain unilateral and/or bilateral, tenderness upon palpation of LZJ or transverse processes, lack of radicular features, pain eased by flexion, pain on lateral flexion, extension and rotation and low back pain associated with groin or thigh pain (17,19). In a study by Revel et al, a cluster of seven items were shown to be of value in predicting the response to initial screening block (18): pain relieved by recumbency, age over 65 years, pain not exaggerated with: coughing and sneezing, extension, forward flexion, rising from flexion and extension-rotation test. Larger studies and studies using comparative local anaesthetic blocks have failed to demonstrate such correlation of clinical symptomatology. Hence, none of these features including Revel's criteria can reliably predict the positive response to diagnostic blocks (19,20). Similarly, radiologic imaging studies are also conflicting.
Pain referral patterns following stimulation of zygapophyseal joints have been studied in both symptomatic and asymptomatic volunteers. L1/2 to L5/S1 zygapophyseal joints could refer pain to the low back region, greater trochanter, posterolateral thigh, and groin region, and occasionally, to leg and foot (21,22). The referral zones were found to be more localised and smaller after electrical stimulation of medial branches of L1 to L4 posterior primary rami and L5 dorsal ramus in asymptomatic volunteers (23). Radicular symptoms may be evident in the presence of facetal hypertrophy, synovial cysts and osteophytes. In spite of a consistent referral pattern in the experimental setting, the use of pain maps to identify the origin of LZJ pain in a clinical setting is conflicting and yet to be proven.
Diagnosis
IASP recommends that LZJ pain should be diagnosed only on the basis of radiologically guided, controlled (using a placebo) or comparative (two different local anaesthetics) intra-articular joint injections or medial branch blocks (24). Factors such as the relative risk for another false positive block, complication rate of the second diagnostic block versus definitive procedure (denervation), false negatives, and the cost-effectiveness dictate the clinical practice. Moreover, these blocks, alone, form a part of the therapeutic armamentarium.
Both medial branch blocks (MBB) and intra-articular injections have been used in prevalence studies and are equally effective in diagnosing LZJ pain. Comparative studies of MBBs and intra-articular injections using local anaesthetic and steroid found no difference in immediate pain relief (25). The false positive rates of single diagnostic block using lidocaine either intraarticular or medial branch block have been reported to range from 17 to 41% while the placebo with saline had a false positive rate of 18 to 32% (6).
Management
Management is usually multimodal comprising of education, exercises, analgesics, behavioural therapy and procedural interventions to achieve functional restoration. Numerous studies evaluating non-interventional management of low back pain (LBP) are available (26). Exercises, back schools and behavioural therapy have been to shown to improve functional status and behavioural outcomes as well as a reduction in pain scores among the heterogeneous population of LBP patients.
Pathoanatomical diagnosis may not be essential for acute and subacute back pain as its natural history is so favourable. However, the pursuit of pathoanatomical diagnosis for target-specific therapies is advocated for a sub-group of chronic LBP patients who fail conservative therapy (27). The various targeted therapeutic options available for LZJ pain include medial branch blocks, intra-articular injections and neurotomy. The following discussion focuses mainly on the evidence base for these procedures.
Medial Branch blocks
Medial branch blocks using local anaesthetic and/or steroids are commonly used for therapeutic purposes. In the preliminary report of an ongoing double blind, randomised controlled trial, Manchikanti et al reported pain relief of 12–14 weeks. Interestingly, they did not find any advantage of adding steroids (28). Boswell et al (29) reports moderate evidence for both short (< 3 months) and long-term (> 3 months) pain relief in their systematic review, based on the available case series and the above-mentioned preliminary report.
Intra-articular injections
There is considerable debate about the evidence base for the intraarticular instillation of local anaesthetic and/or steroids into the facet joint under fluoroscopic guidance. European guidelines for management of chronic non-specific low back pain do not recommend the use of intraarticular steroids (30). Experts question the validity of the diagnosis of LZJ pain in the majority of published studies, as they lack pre-screening and advocate the procedure for a heterogeneous population with LBP. In one such study where patients were identified after diagnostic blocks, Carette et al found the intraarticular steroid group to have less pain and disability at 6 months compared to their saline controls. However, the steroid group had numerous co-interventions reducing the statistical validity (31).
Medial branch Neurotomy
The rationale for medial branch neurotomy is that patients with LZJ pain should obtain pain relief if the nerve supply to the corresponding joint is interrupted.
In the commonly practised thermal radiofrequency (RF) denervation, radiofrequency energy is channelled through a needle to create a controlled burn (temperature up to 90 C over 60 – 120 seconds) to coagulate the target nerves. Using this treatment, Dreyfuss et al reported 60% pain relief lasting for one year in 87% of their patients. This prospective study is widely acclaimed for its selection of patients using comparative local anaesthetic blocks and using electromyography of the multifidus muscle for objective evaluation of denervation as well as the technical aspects of the procedure (32). Thermal RF denervation is associated with only minor complications and the incidence is reported as 0.3 to 1.7% per lesion. Kornick et al reported only 6 minor complications such as 3 cases of localised pain lasting more than 2 weeks and 3 cases of neuritic pain lasting less than 2 weeks (33).
Thermal RF denervation has been evaluated in at least 4 randomised controlled studies. Gallagher et al reported a statistically significant difference in VAS scores at 1 and 6 months after RF denervation in patients who had good response to diagnostic blocks (34). Van Kleef et al showed RF denervation could be effective in terms of VAS, global perceived effect and Oswestry disability scales up to 12 months (35). Leclaire et al did not find any difference between study and sham group in terms of pain scores and functional disability evaluated by Oswestry and Roland-Morris scales after 4 weeks of treatment (36). Though the methodology of the trial was commendable, their patient selection was very controversial (37). In another multicentre, randomised, double blind, sham-lesion controlled trial from Netherlands (11), there was a difference between sham and RF lesion at 3 months in VAS scores. However, there was no difference when it was combined with other outcomes such as changes in daily physical activity and use of analgesics. While the low VAS scores were reported to be maintained at 12 months, long-term analysis was not reported because blinding ended at 3 months. The global perceived effect was significantly different favouring RF denervation at 3 months. All of the above RCTs used a single diagnostic block and other criticisms include patient selection, methodological issues, and technical aspects of RF denervation. Hence, Hooten et al attempted to produce evidence based guidelines for the diagnostic and procedural aspects of RF denervation that could be used for future RCTs. Their recommendations include Revel's criteria for patient selection, comparative diagnostic blocks for diagnosis, and the various procedural aspects of RF denervation (Table. 1) (38). Bogduk argues that Revel's criteria can potentially miss a proportion of patients with LZJ pain (39).
Table 1.
Technical aspects of radio frequency denervation recommended by Hooten et al (38).
| Needle | 18 G, 1-cm exposed tip |
| Site | L1-L4: tip of the needle in the superior aspect of groove formed between transverse process and superior articular process. |
| L5: in the groove between the ala of sacrum and superior articular process. | |
| Lesion | 120 seconds at 80°C |
Of the available 4 systematic reviews, three did find moderate evidence for thermal RF denervation to be more effective than placebo for relief of LZJ pain (29,40,41), while the Cochrane review found conflicting (level C) evidence (37). There remains a need for further high quality, adequately powered RCTs with standardised selection, diagnostic criteria and outcome measures as well as long-term data.
Pulsed RF (application of RF energy with pulsed time cycles at temperatures not exceeding 42 C) has also been used to treat LZJ pain. The rationale for use of pulsed RF is the elimination of any potential inadvertent damage to adjacent nerve roots as well as the possible spinal instability secondary to multifidus muscle denervation from multilevel neurotomies. Mikeladze et al reported only 4 months of pain relief in 59% of patients with pulsed RF for LZJ pain in their retrospective case series (42).
Laser energy has also been used for denervation of LZJs. Iwatsuki et al performed laser irradiation to superior, middle and inferior portions of the dorsal surface of the facet capsule in 21 patients and reported greater than 70% pain relief for at least 1 year in 17 of their patients (43).
In summary, sources of chronic low backache can be established in selected patients. Lumbar zygapophyseal joints are one among the sources, diagnosed by controlled or comparative local anaesthetic blocks. Management should be multimodal therapy comprising of exercises, education, analgesics, behavioural therapy and procedural interventions to achieve functional restoration. The evidence suggests that radiofrequency denervation is not a placebo.
Acknowledgement
Graphics: Mr Ben Mason, Medical Illustration, Aberdeen Royal Infirmary
References
- 1.Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. Eur J Pain 2006; 10:287–333. [DOI] [PubMed] [Google Scholar]
- 2.Bogduk N: Low Back Pain. In clinical anatomy of the lumbar spine and sacrum 3rd edition. Edited by: Bogduk N. New York: Churchill Livingstone; 1997:187–214. [Google Scholar]
- 3.Bogduk N. The innervation of the lumbar spine. Spine 1983;8: 286–293. [DOI] [PubMed] [Google Scholar]
- 4.Cavanaugh JM, Ozaktay AC, Yamashita HT, King AI. Lumbar facet pain: biomechanics, neuroanatomy and neurophysiology. J Biomech 1996;29:1117–29. [DOI] [PubMed] [Google Scholar]
- 5.Kalichman L, Hunter DJ. Lumbar facet joint osteoarthritis: A review. Semin Arthritis Rheum 2007;37:69–80. [DOI] [PubMed] [Google Scholar]
- 6.Cohen SP, Raja SN. Pathogenesis, diagnosis, and treatment of lumbar zygapophyseal (facet) joint pain. Anesthesiology 2007; 106: 591–614. [DOI] [PubMed] [Google Scholar]
- 7.Eubanks JD, Lee MJ, Cassinelli E, Ahn NU. Prevalence of lumbar facet arthrosis and its relationship to age, sex and race: An anatomical study of cadaveric specimens. Spine 2007;32:2058–62. [DOI] [PubMed] [Google Scholar]
- 8.http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsStatistics/DH_4006687. Accessed on 29th September 2007.
- 9.Jackson RP, Jacobs RR, Montesano PX. Facet joint injection in low-back pain: A prospective statistical study. Spine 1988;13: 966–71. [DOI] [PubMed] [Google Scholar]
- 10.Murtagh FR. Computed tomography and fluoroscopy guided anesthesia and steroid injection in facet syndrome. Spine 1988; 13:686–9. [PubMed] [Google Scholar]
- 11.Geurts J, van Wiik R, Wynne H, Hammink E, Buskens E, Lousberg R, Knape J, Groen G. Radiofrequency denervation of lumbar facet joints in the treatment of chronic low back pain: A randomised, double-blind, sham lesion-controlled trial. Clin J Pain 2005;21:335–44. [DOI] [PubMed] [Google Scholar]
- 12.Schwarzer A C, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. Clinical features of patients with pain stemming from the lumbar zygapophyseal joints. Is the lumbar facet syndrome a clinical entity? Spine 1994;199:1132–7. [DOI] [PubMed] [Google Scholar]
- 13.Manchikanti L, Boswell MV, Singh V, Pampati V, Damron KS, Beyer CD. Prevalence of facet joint pain in chronic spinal pain of cervical, thoracic and lumbar regions. BMC Musculoskelet Disord 2004;5:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manchikanti L, Pampati V, Fellows B, Bakhit CE. Prevalence of lumbar facet joint pain in chronic low back pain. Pain Physician 1999;2:59–64. [PubMed] [Google Scholar]
- 15.Schwarzer AC, Wang SC, Bogduk N, McNaught PJ, Laurent R. Prevalence and clinical features of lumbar zygapophyseal joint pain: a study in an Australian population with chronic low back pain. Ann Rheum Dis 1995;54:100–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manchikanti L, Manchukonda R, Pampati V, Damron KS, McManus CD. Prevalence of facet joint pain in chronic low back pain in post surgical patients by controlled comparative local anesthetic blocks. Arch Phys Med Rehabil 2007;88:449–55. [DOI] [PubMed] [Google Scholar]
- 17.Wilde VE, Ford JJ, McMeeken JM. Indicators of lumbar zygapophyseal joint pain: Survey of an expert panel with the Delphi technique. Phys Ther. 2007;87:1348–61. [DOI] [PubMed] [Google Scholar]
- 18.Revel M, Poiraudeau S, Payan SGR, Denke C, Afiwa N, Chevrot M, Jacques AF. Capacity of the clinical picture to characterize low back pain relieved by facet joint anesthesia. Proposed criteria to identify patients with painful facet joints. Spine 1998;23:1972–6. [DOI] [PubMed] [Google Scholar]
- 19.Manchikanti L, Pampati, Fellows MA, Baha AG. The inability of the clinical picture to characterise pain from facet joints. Pain Physician 2000;3:158–66. [PubMed] [Google Scholar]
- 20.Laslett M, Oberg B, Aprill CN, McDonald B. Zygapophysial joint blocks in chronic low back pain: a test of Revel's model as a screening test. BMC Musculoskelet Disord 2004;5:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fukui S, Ohseto K, Shiotani M, Ohno K, Karasawa H, Naganuma Y, Yuda Y. Distribution of referred pain from the lumbar zygapophyseal joints and dorsal rami. Clin J Pain 1997;13: 303–7. [DOI] [PubMed] [Google Scholar]
- 22.McCall IW, Park WM, O'Brien JP. Induced pain referral from posterior lumbar elements in normal subjects. Spine 1979;4:441–6. [DOI] [PubMed] [Google Scholar]
- 23.Windsor RE, King FJ, Roman SJ, Tata NS, Cone-Sullivan LA, Thampi S, Acebey M, Gilhool JJ, Rao R, Sugar R. Electrical stimulation induced lumbar medial branch referral patterns. Pain Physician 2002;5:347–53. [PubMed] [Google Scholar]
- 24.Lumbar spinal or radicular pain syndromes. In Classification of chronic pain 2nd Edition. Edited by: Merskey H. & Bogduk N. Seattle: IASP Press; 1994: p181. [Google Scholar]
- 25.Marks RC, Houston T, Thulbourne T. Facet joint injection and facet nerve block: A randomised comparison in 86 patients with chronic low back pain. Pain 1992;49:325–8. [DOI] [PubMed] [Google Scholar]
- 26.van Tulder M, Koes B. Low Back Pain. In: McMahon SB, Koltzenburg M. eds. Wall and Melzack's Textbook of Pain. Philadelphia: Elsevier Churchill Livingstone, 2006:699–708. [Google Scholar]
- 27.Bogduk N. Management of chronic low back pain. Med J Aust 2004;180:79–83. [DOI] [PubMed] [Google Scholar]
- 28.Laxmaiah M, Kavita N M, Rajeev M, Cash KA, Damron KS, Pampati V, McManus CD. Evaluation of lumbar facet joint nerve blocks in the management of chronic low back pain: preliminary report of a randomised, double-blind controlled trial: clinical trail NCT00355914 Pain Physician 2007;10:425–40. [PubMed] [Google Scholar]
- 29.Boswell MV, Colson JD, Sehgal N, Dunbar EE, Epter R. A systematic review of therapeutic facet joint interventions in chronic spinal pain. Pain Physician 2007;10:229–53. [PubMed] [Google Scholar]
- 30.Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, Mannion AF, Reis S, Staal JB, Ursin H, Zanoli G. Chapter 4. European guidelines for the management of chronic non-specific low back pain. Eur Spine J 2006;15:S192–S300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carette S, Marcoux S, Truchon R, Grondin C, Gagnon J, Allard Y, Latulippe M. A controlled trial of corticosteroid injections into facet joints for chronic low back pain. N Eng J Med 1991;325:1002–7. [DOI] [PubMed] [Google Scholar]
- 32.Dreyfuss P, Halbrook B, Pauza K, Anand J, McLarty J, Bogduk N. Efficacy and validity of radiofrequency neurotomy for chronic lumbar zygapophyseal joint pain. Spine 2000;25:1270–77. [DOI] [PubMed] [Google Scholar]
- 33.Kornick C, Kramarich S, Lamer TJ, Sitzman BT. Complications of lumbar facet radiofrequency denervation Spine 2004;29:1352–1354. [DOI] [PubMed] [Google Scholar]
- 34.Buijs E, van Wijk R, Geurts J, Weeseman R, Stolker R, Groen G. Radiofrequency facet joint denervation in the treatment of low back pain: A prospective controlled double-blind study to assess its efficacy. Pain Clinic 1994;7:193–8. [Google Scholar]
- 35.van Kleef M, Barendse GA, Kessels A, Voets HM, Weber WE, de Lange S. Randomised trial of radiofrequency lumbar facet denervation for chronic low back pain. Spine 1999;24:1937–42. [DOI] [PubMed] [Google Scholar]
- 36.Leclaire R, Fortin L, Lambert R, Bergeron YM, Rossignol M. Radiofrequency facet joint denervation in the treatment of low back pain: A placebo-controlled clinical trial to assess efficacy. Spine 2001;26:1411–7. [DOI] [PubMed] [Google Scholar]
- 37.Niemisto L, Kalso E, Malmivaara A, Seitsalo S, Hurri H. Radiofrequency denervation for neck and back pain. The Cochrane Database of Systematic Reviews 2003, Issue 1. Art. No.: CD004058.DOI:10.1002/14651858.CD004058. [DOI] [PubMed]
- 38.Hooten WM, Martin DP, Huntoon MA. Radiofrequency neurotomy for low back pain: evidence-based procedural guidelines. Pain Med 2005;6:129–38. [DOI] [PubMed] [Google Scholar]
- 39.Bogduk N. Diagnosing lumbar zygapophyseal joint pain (commentary) Pain Med 2005;6:139–42. [DOI] [PubMed] [Google Scholar]
- 40.Geurts JW, van Wijk RM, Stolker RJ, Groen GJ. Efficacy of radiofrequency procedures for the treatment of spinal pain: A systematic review of randomised clinical trials. Reg Anesth Pain Med 2001;26:394–400. [DOI] [PubMed] [Google Scholar]
- 41.Slipman CW, Bhat AL, Gilchrist RV, Isaac Z, Chou L, Lenrow DA. A critical review of the evidence for the use of zygapophyseal injections and radiofrequency denervation in the treatment of low back pain. Spine J 2003;3:310–6. [DOI] [PubMed] [Google Scholar]
- 42.Mikeladze G, Espinal R, Finnegan R, Routon J, Martin D. Pulsed radiofrequency application in the treatment of chronic zygapophyseal joint pain. Spine J 2003;3:360–2. [DOI] [PubMed] [Google Scholar]
- 43.Iwatsuki K, Yoshimine T, Awazu K. Alternative denervation using laser irradiation in lumbar facet syndrome. Lasers Surg Med 2007;39:225–9. [DOI] [PubMed] [Google Scholar]