Abstract
Labour is an emotional experience and involves both physiological and psychological mechanisms.
The pain of labour is severe but despite this its memory diminishes with time.
Labour pain has two components: visceral pain which occurs during the early first stage and the second stage of childbirth, and somatic pain which occurs during the late first stage and the second stage.
The pain of labour in the first stage is mediated by T10 to L1 spinal segments, whereas that in the second stage is carried by T12 to L1, and S2 to S4 spinal segments.
Pain relief in labour is complex and often challenging without regional analgesia.
Effective management of labour pain plays a relatively minor role in a woman's satisfaction with childbirth.
Introduction
The experience of labour is complex and subjective. Several factors affect a woman's perception of labour making each experience unique. However as a consistent finding, labour pain is ranked high on the pain rating scale when compared to other painful life experiences1. The memory of this pain however is short lived and of parturients who experienced severe pain in labour, 90% found the experience satisfactory three months later2. This short term memory may be related to the positive outcome that often occurs at the end of labour.
The pattern of labour pain differs between nulliparous and multiparous women and it is well documented that pain scores are higher in the nulliparous compared to the multiparous woman especially if there has been no antenatal education. Consistent findings also indicate that nulliparous women on average experience greater sensory pain during early labour compared to multiparous women3 who seem to experience more intense pain during the pelvic phase of labour as a result of sudden stimulation of nociceptors surrounding the vaginal vault, vulva and perineum4 and rapid descent of the foetus5,6.
Labour pain as well as being unpleasant for the mother, can have deleterious effects on the foetus (figure 1).
Figure 1.
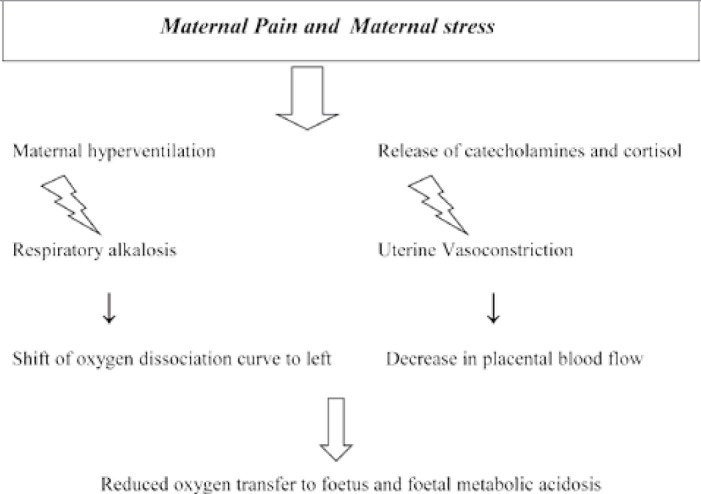
Figure 2a.
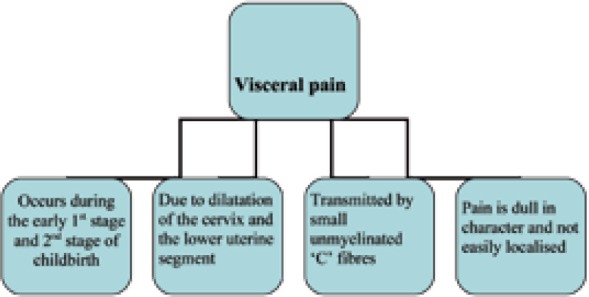
– Visceral Pain
Figure 2b.
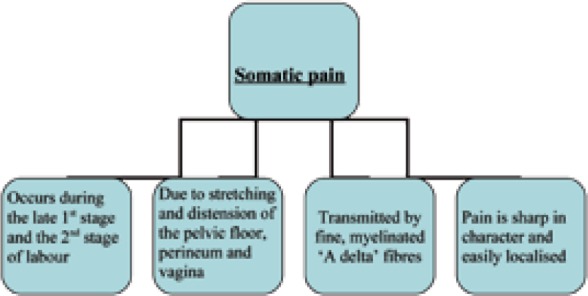
– Somatic pain
Mechanisms of Labour Pain
Labour is the active process of delivering a foetus and is characterised by regular, painful uterine contractions which increase in frequency and intensity.
The pain of labour has two components: visceral and somatic, and its anatomy is well documented. The cervix has a central role in both the first and second stage of labour.
Visceral pain
Visceral labour pain occurs during the early first stage and the second stage of childbirth. With each uterine contraction, pressure is transmitted to the cervix causing stretching and distension and activating excitatory nocioceptive afferents. These afferents innervate the endocervix and lower segment from T10 – L1.
Somatic pain
This occurs in addition to the visceral pain described above, in the late first stage of labour and also in the second stage. It arises due to afferents that innervate the vaginal surface of the cervix, perineum and vagina and occurs as a result of stretching, distension, ischaemia and injury (tearing or iatrogenic) of the pelvic floor, perineum and vagina. It manifests during descent of the foetus and during this active stage, the uterus contracts more intensely in a rhythmic and regular manner.
The intensity of labour pain increases with greater cervical dilatation and correlates well with the intensity, duration and frequency of uterine contractions.
Pathways of labour pain
Well documented physiological knowledge provides the basis for explaining the two components of labour pain:
Visceral pain
Visceral pain is transmitted by small unmyelinated ‘C’ fibres which travel with sympathetic fibres and pass through the uterine, cervical and hypogastric nerve plexuses into the main sympathetic chain. The pain fibres from the sympathetic chain enter the white rami communicantes associated with T10 to L1 spinal nerves and pass via their posterior nerve roots to synapse in the dorsal horn of the spinal cord. Some fibres cross over at the level of the dorsal horn with extensive rostral and caudal extension resulting in poorly localised pain. Chemical mediators involved include bradykinin, leukotrienes, prostaglandins, serotonin, substance P and lactic acid.
The pain of early labour is referred to T10-T12 dermatomes such that pain is felt in the lower abdomen, sacrum and back. This pain is dull in character and is not always sensitive to opioid drugs; the response to opioids depends on the route of administration.
Somatic pain
Somatic pain is transmitted by fine, myelinated rapidly transmitting ‘A delta’ fibres. Transmission occurs via the pudendal nerves and perineal branches of the posterior cutaneous nerve of the thigh to S2 - S4 nerve roots. Somatic fibres from the cutaneous branches of the ilioinguinal and genitofemoral nerves also carry afferent fibres to L1 and L2.
Somatic pain occurs closer to delivery, is sharp in character and easily localised to the vagina, rectum and perineum. It radiates to the adjacent dermatomes T10 and L1 and compared to visceral pain, is more resistant to opioid drugs.
All resulting nerve impulses (visceral and somatic) pass to dorsal horn cells where they are processed and transmitted to the brain via the spino-thalamic tract. Transmission to the hypothalamic and limbic systems accounts for the emotional and autonomic responses associated with pain.
Psychology of labour pain
Labour pain is an emotional experience and presents a psychological challenge for many parturients. Indeed a recent Cochrane review concluded that women who had continuous intra-partum support were less likely to have intra-partum analgesia or to report dissatisfaction. Other groups have suggested that an underlying anxiety trait can both result in a higher uptake of epidural analgesia as well as influence the analgesic effect of the epidural block. There is current interest in determining whether the Pain Catastrophizing Score has any influence on either labour outcome or analgesic uptake.
Table 1.
Stages of Labour
| 1st stage | From the establishment of labour (progressive cervical dilatation associated with regular uterine contraction) to full cervical dilatation |
| 2nd stage | From full cervical dilatation to delivery of the infant |
| 3rd stage | From delivery of the infant to delivery of the placenta |
Table 2.
Management of labour pain
| Complementary and alternative therapies for labour pain | Pharmacological analgesia for labour pain |
|---|---|
| Psychological e.g. hypnosis | Inhalational analgesia e.g. entonox, isoflurane, desflurane, sevoflurane (reduce pain perception) |
| Physical e.g. transcutaneous electrical nerve stimulation (TENS), acupuncture | Parenteral opioids e.g. pethidine, morphine, diamorphine, fentanyl, remifentanil (reduce pain perception) |
| Other complimentary e.g. aromatherapy, water immersion | Regional analgesia e.g. epidural, combined spinal epidural, continuous spinal analgesia (reduce pain transmission) |
Interestingly there appears to be a circadian variation in labour pain perception and one group have demonstrated lower mean daytime visual analogue pain score compared to nocturnal scores.
Evidence also suggests that attitudes to pain relief in labour depend on personal aspirations, cultural factors and peer group influences. The ability to cope with pain may be rated as more important than the level of pain experienced. In one survey, only 9% of women wanted ‘the most pain free labour that drugs can give me’. The majority, 67%, wanted ‘the minimum quantity of drugs to keep the pain manageable’7. What seems to be important is that women are more likely to be satisfied with pain relief if they felt they had been in control during their labour.
Antenatal education
No studies have shown that effective management of labour pain plays a major role in a woman's satisfaction with childbirth. Antenatal childbirth preparation however has a role in increasing maternal satisfaction and may reduce pain scores to some extent.
It is important that anaesthetists are involved with patients antenatally, and in educating midwives and obstetricians. Antenatal education is also essential when obtaining informed consent from the mother8; the aim is to provide good information to facilitate mothers to form realistic expectations and appreciate the limitations of certain methods of analgesia.
Management of labour pain
The aim of pain relief in labour is to render parturients relatively pain free whilst still able to participate in the birth experience. Ideally there should be no associated side effects or risks to both mother and baby. In reality, there are several methods of pain relief available but none are ideal.
Complementary and alternative therapies for pain management in labour
It is not surprising that many mothers try to avoid invasive and pharmacological methods of pain relief in labour and seek complementary therapies which have minimal side effects and are easy to administer. Few complementary therapies however are easily available or have been subject to proper scientific study. The majority provide pain relief which is incomplete, unpredictable and inconsistent (TENS, acupuncture), and some simply increase the ability to cope with labour pain (hypnosis).
A systematic review of randomised controlled trials comparing water immersion during labour with no immersion concluded that labouring in water in the first stage reduces the use of analgesia and reported maternal pain, without adverse outcomes on labour duration, operative delivery or neonatal outcomes9. These conclusions however can only be accepted with caution because the study sample sizes were small and blinding to the intervention was impossible. Water immersion may be associated with increased uterine perfusion, shorter labours and a decreased need for augmentation; the associated feeling of weightlessness also adds to comfort and allows for easy change of position during labour. Warm water, as well as inducing muscle relaxation and reducing anxiety may also decrease the release of catecholamines and stimulate the release of endorphins.
There is conflicting evidence to support the efficacy of TENS in labour. The majority of trials report it as being ineffective but the evidence for this is not strong, and in practice many parturients still utilise TENS in labour. The Cochrane collaboration are currently reviewing all randomised controlled trials involving the use of TENS in labour to determine its effectiveness and safety.
Pharmacological analgesia for labour pain
Inhalational
Entonox
A 50:50 mixture of oxygen and nitrous oxide is the most widely available inhalational analgesia in the United Kingdom. Despite its widespread use, studies have shown that when used in labour for short periods, it is not a potent analgesic but does provide some analgesia and is safe for labouring women and their babies10.
Isoflurane, Desflurane, Sevoflurane
These inhalational gases can be used with or without nitrous oxide to improve analgesic efficacy during labour at sub anaesthetic concentrations. Compared to entonox, most women prefer sevoflurane, and at a concentration of 0.8%, sevoflurane gives significantly better pain relief scores but is associated with more sedation11.
In practice, inhalational gases are not commonly utilised in labour due to technical difficulties in their safe administration, scavenging, requirement of specific vaporisers and concerns about atmospheric pollution.
Parenteral opioids
Pethidine
Like entonox, pethidine is readily available and easy to administer.
In a survey by the UK National Birthday Trust (NBT), 16% of women receiving pethidine rated it as ‘helpful’ whereas 25% rated it as ‘unhelpful’. Interestingly, midwives rated pethidine higher than parturients, interpreting sedation as analgesia12. The optimal opioid for labour analgesia remains unknown and a systematic review of the available choices concluded that no other opioid appeared to be better than pethidine in providing pain relief in labour13. In practice, pethidine is still the most commonly utilised opioid as it can be easily administered by midwives. The effects of systemic opioids in labour are predominantly sedative rather than analgesic14; other opioids when used in labour are usually administered as patient controlled analgesia.
Remifentanil
This is increasingly being used due to its fast onset and short duration of action. A typical bolus dose of 0.25 – 0.5 μg/kg with a lockout period of 1 – 2 minutes is currently being used. A small double blind crossover study has suggested than intravenous remifentanil when compared to entonox provides better pain relief15.
The efficacy of systemic opioids for labour analgesia is limited and undoubtedly inferior to regional analgesia, however there are often times when regional analgesia is not appropriate and alternative analgesia is essential.
Regional analgesia
Epidural
Epidural analgesia is thought to be the most effective method of providing pain relief in labour and involves injecting local anaesthetic close to the nerves that transmit pain. It also gives the option of providing regional anaesthesia for obstetric interventions such as forceps delivery and caesarean sections, and obese and other parturients who are at risk of obstetric interventions particularly benefit from an early epidural.
Low –dose local anaesthetic and opioid mixtures; typically 10–15 mls 0.1% bupivacaine with 2mcg/ml fentanyl are currently in use in most delivery units, however some units still use higher concentrations of bupivacaine for labour analgesia. Low-dose mixtures are thought to provide excellent analgesia while preserving motor function with the mother more likely to mobilise during labour or deliver without assistance16. In practice the majority of women do not mobilise in labour.
A synergistic effect has been demonstrated between neuraxial opioids and local anaesthetics and the addition of opioids such as fentanyl to epidural local anaesthetic is associated with improved maternal analgesia. The low-dose mixture can be used as a test dose by careful titration; typically 10 mls 0.1% bupivacaine with 2 mcg/ml fentanyl, contributing to early analgesia in a correctly placed catheter and allowing early identification of accidental intrathecal injection manifested by rapid onset of analgesia, motor block (especially sacral) and sympathetic block.
Maintenance of analgesia in labour is provided by intermittent top-up by midwives, by continuous infusion or by use of patient-controlled epidural analgesia (PCEA). Continuous epidural infusions are associated with more motor block than either top-ups or PCEA. PCEA in labour is set up with a small background infusion and tops up that are smaller in volume than those usually administered by midwives or anaesthetists, but which can be administered more often. It results in satisfactory analgesia with reduced overall dose of bupivacaine and fentanyl.
Labour epidurals are associated with an increase in the duration of the second stage and an increased risk of instrumental vaginal delivery. They are also associated with an increased need for stimulation of labour contractions and may cause reduction in maternal blood pressure, and fever. They are the commonest cause of intrapartum pyrexia which is strongly associated with poor neonatal outcome in the form of neonatal encephalopathy and cerebral palsy. The exact mechanism is unknown but it is thought that an increased temperature of tissues increases their metabolic rate and therefore their oxygen requirements, resulting in cerebral palsy.
The sympathetic blockade accompanying low-dose epidural top-ups is slow in onset and seldom extensive. Maternal hypotension in these circumstances is usually associated with aorto-caval compression.
Immediate serious complications of epidural analgesia include: massive misplaced injection intravascularly, intrathecally, or subdurally, high or total spinal block (rare), hypotension, and local anaesthetic induced convulsions and cardiac arrest (rare). Delayed complications include post dural puncture headache, transient backache, urinary retention, epidural haematoma, abscess or meningitis (rare) and permanent neurological deficit (rare). The majority of neurological injuries in this setting are not as a result of neuraxial analgesia but are intrinsic to labour and delivery.
The amide local anaesthetic, levobupivacaine, is less cardiotoxic than racemic bupivacaine when given intravenously. However, cardiotoxic doses of bupivacaine are unlikely to be reached if low-dose infusions or top-ups are used. 20% lipid emulsion is now widely available as treatment for cardiac arrest secondary to overdose of these long acting local anaesthetics17.
Combined Spinal Epidural (CSE)
This involves an initial injection of a low dose of local anaesthetic and opioid (e.g. bupivacaine 2.5mg + fentanyl 15 – 25mcg) into the subarachnoid space followed by an epidural top-up. This method is thought to provide more rapid and complete analgesia with less motor block compared with the conventional epidural method18. In practice, traditional epidurals are performed far more frequently for labour analgesia than CSEs. There appears to be little basis for offering CSEs over epidurals in labour and it is debatable whether breaching the dura can ever be justified.
Evidence shows no difference in retrospective maternal satisfaction, ability to mobilise and obstetric and neonatal outcome. Many units reserve this technique for those in rapidly advancing labour when analgesia, particularly sacral is needed in the second stage of labour and for the multiparous parturient who had an ineffective epidural on a previous occasion. Perceived risks of the CSE technique include increased incidence of post-dural puncture headache, meningitis and epidural catheter migration through the dural hole.
Continuous spinal analgesia (CSA)
This is typically provided by either intermittent bolus or continuous infusion techniques and may be preferred in cases of accidental dural puncture.
It is used when other methods of pain relief are not available or in a mother in the very advanced first stage of labour or for high risk maternities. CSA with microcatheters offers some advantages over the single shot spinal or the continuous epidural techniques but it is associated with complications such as cauda equina syndrome and may be inherently more dangerous than the other two techniques.
Contributor Information
Simona Labor, Specialist Registrar in Anaesthesia.
Simon Maguire, Consultant Anaesthetist, Wythenshawe Hospital, Manchester.
References
- 1.Melzack R. The myth of painless childbirth. Pain 1984; 321–337. [DOI] [PubMed]
- 2.Morgan BM, Bullpitt CJ, Clifton P, Lewis PJ. Analgesia and satisfaction in childbirth (the Queen Charlotte's 1000 mother survey). Lancet 1982a; ii: 808–810. [DOI] [PubMed] [Google Scholar]
- 3.Sheiner E, Sheiner EK, Shoham-Vardi I. The relationship between parity and labour pain. Int J Gynaecol Obstet 1998; 63: 287–8. [DOI] [PubMed] [Google Scholar]
- 4.Lowe NK. Pain and discomfort of labour and birth. J Obstet Gynaecol Neonatal Nurs 1996; 25: 82–92. [DOI] [PubMed] [Google Scholar]
- 5.Lowe NK. Differences in first and second stage labour pain between nulliparous and multiparous women. J Psychosom Obstet Gynecol 1992; 13: 243–53. [Google Scholar]
- 6.Ranta P, Jouppila R. The intensity of labour pain in grand multiparas. Acta Obstet Gynecol Scand 1996; 75: 250–4. [DOI] [PubMed] [Google Scholar]
- 7.Green JM, Coupland V, Kitzinger JV. Expectations, Experiences, and Psychological Outcomes of Childbirth: A Prospective Study of 825 Women Birth 2007; 17: 15. [DOI] [PubMed] [Google Scholar]
- 8.The Association of Anaesthetists of Great Britain and Ireland. Guidelines on Consent for Anaesthesia. Revised Edition 2006.
- 9.Cluett ER, Nikodem VC, McCandlish RE, Burns EE. Immersion in water in pregnancy, labour and birth. Cochrane Database of Systematic Reviews 2002, Issue 2. Art. No.: CD00011. DOI:10.1002/14651858.CD000111.pub2. [DOI] [PubMed]
- 10.Rosen M. Nitrous oxide for pain relief of labor pain: a systematic review. Am J Obstet Gynecol 2002; 186: S110–26. [DOI] [PubMed] [Google Scholar]
- 11.Yeo ST, Holdcroft A, Yentis SM, et al. Sevoflurane compared with Entonox for labour analgesia. Br J Anaesth 2007; 98: 110–15. [DOI] [PubMed] [Google Scholar]
- 12.Chamberlain G, Wraight A, Steer P, eds. Pain and its relief in childbirth: the results of a national survey conducted by the National Birthday Trust. Edinburgh: Churchill Livingstone, 1993. [Google Scholar]
- 13.Bricker L, Lavender T. Parenteral opioids for labor pain relief: a systematic review. Am J Obstet Gynecol 2002; 186: S94–109. [DOI] [PubMed] [Google Scholar]
- 14.Olofsson C, Ekblom G, Ekman-Ordeberg L. Granström L, Irestedt. Analgesic efficacy of intravenous morphine in labour pain: A reappraisal. Int J Obstet Anesth 1996; 5: 176–80. [DOI] [PubMed] [Google Scholar]
- 15.Volmanen P, Akural E, Raudaskoski T, Ohtonen P. Alahuhta, S. Comparison of remifentanil and nitrous oxide in labour analgesia. Acta Anaesthesiol Scand 2005; 49: 453–8. [DOI] [PubMed] [Google Scholar]
- 16.Collis RE, Davies DWL, Aveling W. Randomised comparison of combined spinal-epidural and standard epidural analgesia in labour. Lancet 1995; 345: 1413–16. [DOI] [PubMed] [Google Scholar]
- 17.Weinberg G. Reply to Drs. Goor, Groban, and Butterworth—lipid rescue: caveats and recommendations for the “Silver Bullet”. Regional Anaesthesia and Pain Medicine 2004; 29 (1): 74. [DOI] [PubMed] [Google Scholar]
- 18.Comparative Obstetric Mobile Epidural Trial (COMET) Study Group UK. Effect of low dose mobile versus traditional epidural techniques on mode of delivery: a randomised control trial. Lancet 2001; 358: 19–23. [DOI] [PubMed] [Google Scholar]


